Abstract
Background
Necrotizing enterocolitis (NEC) is a severe multifactorial disease in preterm neonates associated with high morbidity and mortality. Better insight into prognostic values of the many reported factors associated with NEC is needed to enable identification of neonates at risk for NEC. The aim was to systematically review the literature to identify independent risk factors for NEC from the literature.
Methods
Medline, Cochrane, Embase, Pubmed and Google Scholar were searched systematically for cohort studies reporting prognostic factors for NEC in neonates using multivariable analysis. Studies were scored with the Quality In Prognosis Studies tool (QUIPS).
Results
From 5154 initial hits, 14 prognostic studies were included, with various designs. Study quality was rated high in three studies, moderate or low in the 11 others. Significant prognostic factors for NEC reported in at least two studies were: low birth weight, small for gestational age, low gestational age, assisted ventilation, premature rupture of membranes, black ethnicity, sepsis, outborn, hypotension (all increased risk), surfactant therapy (conflicting results) and cesarean section (lower risk). Meta-analysis was considered not feasible.
Conclusion
High quality studies on prognostic factors for NEC are rare. Several prognostic factors, that are not necessarily causal, are associated with NEC. High quality prognostic research is necessary to establish the predictive values of these factors.
Electronic supplementary material
The online version of this article (doi:10.1186/s12887-017-0847-3) contains supplementary material, which is available to authorized users.
Keywords: necrotizing enterocolitis, intestinal perforation, preterm, neonatal intensive care unit, risk factors, prognosis, epidemiology
Background
Necrotizing enterocolitis (NEC) is one of the most severe complications of preterm birth occurring in 5–10% of very low birth weight infants [1, 2]. Although more and more (extremely) preterm infants survive, the number of deaths attributed to NEC has been increasing [3]. Mortality rates ranging from 15% to 30% have been reported [4]. Surgical treatment is often needed, and survivors are at increased risk for poor long-term growth and neurodevelopmental impairment [5]. Despite preventive strategies such as prenatal glucocorticoid administration, breast feeding, use of donor milk and probiotic supplementation, NEC is still relatively common in most neonatal intensive care units (NICUs) [6–10].
NEC is difficult to predict in individual cases. The etiology is complex and multifactorial, including genetic predisposition, intestinal immaturity, imbalance in microvascular tone, abnormal microbial colonization and highly immune-reactive intestinal mucosa [1]. A common inflammatory pathway leads to intestinal ischemia, pneumatosis, necrosis and eventually perforation [11].
Many observational studies have reported clinical and non-clinical risk factors associated with NEC, but the prognostic value usually is unclear. Most of these studies were not designed to answer prognostic questions properly [12]. To identify independent risk factors for a complex disease as NEC, a (preferably prospective) prognostic cohort design with multivariable analysis including multiple co-variates is considered most appropriate [12–14]. The aim of this study was to provide a systematic review of the literature on prognostic studies reporting on independent risk factors for NEC in neonates.
Methods
Study selection
This systematic review was guided by the PRISMA Statement, a 27 item checklist to improve the reporting of systematic reviews [15]. A search strategy was developed in collaboration with a clinical librarian to search PubMed, Embase, Medline, Web-of-science, Cochrane and Google Scholar. An initial search was conducted in January 2014 and updated in August 2016, using terms related to necrotizing enterocolitis, intestinal perforation, neonates, birth weight, gestation, prediction, prognosis, epidemiology and risk factors. The complete search strategy is reported as supplemental material (Additional file 1). References of included studies were checked for additional eligible studies.
Studies were included for analysis if satisfying all following criteria: (1) full English written publications, (2) with a prospective or retrospective cohort study or nested case-control design (3) identifying (neonatal or non-neonatal) prognostic factors for NEC (primary or secondary outcome), (4) using multivariable data analysis including more than 2 co-variates, (5) in a study population of neonates/newborns, preterm infants, very low birth weight (VLBW) or extremely low birth weight (ELBW) infants. No explicit use of the term prognostic was required for inclusion.
Excluded were studies (1) only reporting on associative models of one or two variables with NEC (also if adjustment for potential confounders was performed), or (2) focusing only on risk factors for other abdominal problems than NEC such as spontaneous focal intestinal perforation, viral enteritis and allergic colitis.
After duplicates had been removed, two independent reviewers (NS, RG) screened titles and abstracts on both inclusion and exclusion criteria. Articles identified as potentially eligible underwent a full text review. Any disagreements between the two reviewers concerning study selection, quality assessment and interpretation of results were discussed and resolved in consensus meetings with all authors.
Quality assessment
The methodological quality of full text reports was independently assessed by the same researchers using the Quality In Prognosis Studies (QUIPS) tool [16]. The QUIPS tool assesses risk of bias in prognostic studies by rating each individual article in six domains: study participation, study attrition, measurement of prognostic factors, measurement of outcomes, measurement of confounding, and statistical analysis and reporting. As prognostic studies are designed to predict a specific outcome based on a combination of possible prognostic factors of equal interest, the domain of confounding was considered irrelevant. Therefore, an adapted QUIPS without items addressing confounding was used [17]. As NEC was assumed to be a short-term outcome in the included studies, items on long-term follow-up in the quality assessment were not included.
Quality points for a total of 17 items in five domains were assigned to each study, adding up to a total score of 75 points maximum. Domain items were scored as high when sufficient information concerning the risk of bias was present and the estimated risk of bias was considered low. Items were scored as moderate when the article provided insufficient information about this domain and low quality when an item was not reported or was not reported clearly or the estimated risk of bias was considered high. The quality of the studies was ranked high if ≥60 points (≥80% of the maximum score); moderate if 45–59 points (≥60% and <80% of the maximum score); and low if <45 points (<60% of maximum score) were given as described previously [17].
Data extraction and reporting
A standardized form was used to guide and document data extraction systematically. The following data were extracted: study characteristics (publication characteristics, study design, method of analysis, number of subjects, type and number of prognostic factors, outcomes of interest); patient characteristics (gestational age, birth weight, gender); and strength of association (relative risks (RR) and odds ratios (OR)). To restrict the data to those of most clinical interest, we only present details on statistically significant prognostic factors (p < 0.05) that were reported in at least two studies.
Results
Search and inclusion
The literature search yielded a total of 11,335 studies (Fig. 1). After removing duplicates 5154 articles remained of which titles and abstracts were screened. Full texts of 78 articles were retrieved after assessment for eligibility. A total of 14 articles met the selection criteria and were included in the study. No additional eligible studies were identified through bibliographic review of the included studies.
Fig. 1.
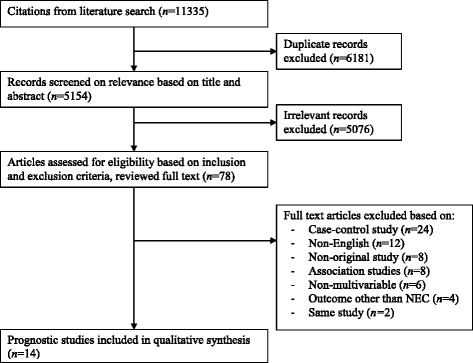
Flow chart of the systematic literature search
Study characteristics
The quality assessment results are listed in Table 1. Three of the included studies were of high quality, 11 were of moderate quality and none of low quality. Details of the included studies are presented in Table 2. Definitions of study population and outcome varied. Ten studies had a retrospective study design and four studies a prospective study design. In seven studies the study population consisted of VLBW infants, defined by birth weight below 1500 g. One study included neonates with intrauterine growth retardation (IUGR) and two studies neonates admitted to the NICU. In four studies the population was defined by gestational age: below 33 weeks, 23–34, 23–32 and 23–36 weeks. The outcome measure was often not clearly described and included NEC Bell stages I and II in one study, and stages II and III in all others.
Table 1.
Results of quality assessment of studies on NEC related prognostic factors according to the QUIPS tool [17]
| Study | Study participation (max. 15) |
Study attrition (max. 15) |
Prognostic factor measurement (max. 15) |
Outcome measurement (max. 15) |
Statistical analysis and reporting (max. 15) |
Quality score (max. 75) |
|---|---|---|---|---|---|---|
| Gephart et al. (2014) [18] | 15 | 5 | 12.5 | 15 | 15 | 62.5 |
| Lee et al. (2016) [38] | 15 | 5 | 12.5 | 12.5 | 15 | 60 |
| Youn et al. (2015) [30] | 15 | 5 | 12.5 | 12.5 | 15 | 60 |
| Boo et al. (2012) [21] | 15 | 5 | 12.5 | 10 | 15 | 57.5 |
| Drenckpohl et al. (2010) [36] | 15 | 5 | 10 | 12.5 | 15 | 57.5 |
| Guthrie et al. (2003) [23] | 15 | 5 | 10 | 12.5 | 15 | 57.5 |
| Yee et al. (2012) [27] | 15 | 5 | 12.5 | 10 | 15 | 57.5 |
| Gagliardi et al. (2008) [28] | 15 | 5 | 12.5 | 7.5 | 15 | 55 |
| Manogura et al. (2008) [39] | 15 | 5 | 10 | 10 | 15 | 55 |
| Yamoto et al. (2016) [26] | 15 | 5 | 10 | 10 | 15 | 55 |
| Faustini et al. (2003) [37] | 13.5 | 5 | 10 | 12.5 | 12.5 | 53.5 |
| Carter et al. (2008) [22] | 15 | 5 | 10 | 10 | 12.5 | 52.5 |
| Luig et al. (2004) [25] | 15 | 5 | 10 | 7.5 | 15 | 52.5 |
| Uauy et al. (1991) [24] | 12 | 5 | 10 | 10 | 12.5 | 49.5 |
NEC necrotizing enterocolitis, QUIPS quality in prognosis studies
Table 2.
Methodologic characteristics of the included prognostic studies on risk factors for NEC
| Author | Country (year) | Design | Type of analysis | N included | Male (%) | Study population | Outcome | NEC type | Significant prognostic factors from multivariable analysis with p < 0.05 |
|---|---|---|---|---|---|---|---|---|---|
| Boo et al. (2012) [21] | Malaysia (2007) | Retrospective | Multivariable | 3601 | 52% | VLBW (≤1500 g) | NEC | II, III | Maternal age, BW, surfactant, intrapartum antibiotics, indomethacin, surfactant, congenital pneumonia |
| Carter et al. (2008) [22] | United States (unknown) | Retrospective | Multivariable | 134 | 54% | GA <35 weeks, BW <1500 g or requiring mechanical ventilation at birth | NEC | II, III | Number of infections, ventilation |
| Drenckpohl et al. (2010) [36] | United States (2002–2008) | Retrospective | Multivariable | 324 | 54% | GA 23–36 weeks | NEC | II, III | Ethnicity, PROM, sepsis, H2 blockers in TPN |
| Faustini et al. (2003) [37] | Italy (1999) | Retrospective | Multivariable | 221 | 49% | Live births of the university hospital in Rome | NEC | I, II | Any neonatal pathological condition, first time feeding with formula, any invasive procedure |
| Gagliardi et al. (2008) [28] | Italy (1999–2002) | Prospective | Multivariable | 2035 | 51% | VLBW (<1500 g), GA 23–37 weeks | NEC-medical, NEC-surgical |
II, III | Assisted ventilation, PDA, surfactant, Late-onset sepsis |
| Gephart et al. (2014) [18] | United States (2007–2011) | Retrospective | Multivariable (Prediction model) |
35,013 | 50% | BW <1500 g and GA < 36 weeks | NEC-surgical, NEC-medical |
II, III | GA, outborn, ethnicity, dopamine, dobutamine or milrinone combined with hypotension, metabolic acidosis, probiotics, late sepsis, PRBC transfusion, 2 or more positive cultures (blood, urine, other), human milk at day 7 and 14 of life, unit NEC rate |
| Guthrie et al. (2003) [23] | United States (1998–2000) | Retrospective | Multivariable | 15,072 | 53% | GA 23–34 weeks | NEC-surgical, NEC-medical |
II, III | BW, antenatal glucocorticoids, umbilical vessel catheterization, assisted ventilation, type of delivery, exposed both glucocorticoids and indomethacin during first week of life, Apgar score 5 min. |
| Lee et al. (2016) [38] | South Korea (2003–2014) | Retrospective | Multivariable | 354 | 53% | GA 23–31(+6) weeks | NEC | II, III | Maternal blood NLR, multiparity, BW, GA |
| Luig et al. (2004) [25] | Australia (1994–1999) | Retrospective | Multivariable | 4649 | 55% | All NICU admissions | NEC | II, III | Placental abruption, GA (weeks), SGA, year of birth, hyaline membrane disease, hypertensive disease of pregnancy |
| Manogura et al. (2008) [39] | United States (1997–2006) | Prospective | Multivariable | 404 | a | Neonates with suspected IUGR | NEC | II, III | BW, base deficit |
| Uauy et al. (1991) [24] | United States (1988–1989) | Prospective | Multivariable | 2681 | a | Infants admitted to one of the network centers <1500 g | NEC | II, III | Center of birth, ethnicity/gender, BW, maternal haemorrhage, duration of ROM, cesarean section |
| Yamoto et al. (2016) [26] | Japan (2006–2015) | Retrospective | Multivariable | 323 | 53% | BW <1000 g | NEC, FIP, MRI | II, III | Gestational age of <26 weeks, severe cardiac malformations, not received EAP |
| Yee et al. (2012) [27] | Canada (2003–2008) | Retrospective | Multivariable | 16,669 | 54% | GA <33 weeks | Early-Onset NEC, Late-Onset NEC |
II, III | GA, SGA, outborn/inborn, congenital anomalies, narcotic use in <3 days, postnatal glucocorticoids |
| Youn et al. (2015) [30] | Korea (2013–2014) | Prospective | Multivariable | 2326 | 50% | VLBW (<1500 g) | NEC | II, III | hypotension ≤1 week |
BW birth weight, EPO erythropoietin, FIP focal intestinal perforation, GA gestational age, IVH intraventricular hemorrhage, MRI meconium-related ileus, NCPAP nasal continuous positive airway pressure, NEC necrotizing enterocolitis, NICU neonatal intensive care unit, NLR neutrophil-lymphocyte ratio, PDA patent ductus arteriosus, PRBC packed red blood cell, (P)ROM (premature) rupture of membranes, RDS respiratory distress syndrome, SGA small for gestational age, SNAP score for neonatal acute physiology, TPN total parental nutrition, VLBW very low birth weight
Footnotes: a not available
Prognostic factors
The 14 included studies described 43 statistically significant risk factors for NEC identified by multivariable analysis. Eleven of these factors were significantly associated with NEC in at least two studies (Table 3). None of the prognostic factors were assessed in all studies. Of the 11 reproducible factors, the following were associated with an increased risk of NEC: small for gestational age, low gestational age, assisted ventilation, sepsis, hypotension, PROM, black ethnicity and outborn status (Table 4). The factor low birth weight was associated differently with NEC in 5 studies. The association with surfactant therapy also showed contrasting directions. Birth by cesarean section was associated with a decreased risk of NEC.
Table 3.
Summary of significant prognostic factors for NEC by high, moderate and low quality studies
| Prognostic factor | High quality | Moderate quality | Low quality |
|---|---|---|---|
| Birth weight | 1× | 4× | - |
| Gestational age (weeks) | 1× | 3× | - |
| Sepsis | 1× | 2× | - |
| Ethnicity | 1× | 2× | - |
| Hypotension | 1× | 1× | - |
| Outborn | 1× | 1× | - |
| Assisted ventilation | - | 3× | - |
| Cesarean section | - | 2× | - |
| PROM | - | 2× | - |
| Small for gestational age | - | 2× | - |
| Surfactant | - | 2× | - |
The table shows the statistically significant prognostic factors reported in at least two studies. The quality of the studies was ranked high if ≥60 points (≥80% of the maximum score), moderate if 45–59 points (≥60% and <80% of the maximum score) and low if <45 points (<60% of maximum score) were given. Using the QUIPS tool
NEC necrotizing enterocolitis, PDA patent ductus arteriosus, PROM premature rupture of membranes, RDS respiratory distress syndrome, QUIPS quality in prognosis studies
Table 4.
Prognostic factors associated with NEC reported in at least two studies
| First author: | Boo | Carter | Drenckpohl | Faustini | Gagliardi | Gephart | Guthrie | Lee | Luig | Manogura | Uauy | Yamoto | Yee | Youn |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Low) birth weightb | OR 0.999 [0.998,0.999]c |
OR 1.001 [p = 0.164]d,e |
OR 1 [1.000,1.001] |
. | . | . | p < 0.001f | OR 0.07 [0.01,0.53]g |
. | p < 0.001f | OR 0.999 [p < 0.001]c,d,h |
. | . | . |
| Gestational age (weeks)b | . | . | . | . | . | OR 2.37 [1.78,3.16]i |
. | OR 1.14 [0.85,1.54]g |
OR 0.82 [0.77,0.89]g |
. | . | OR 19.32 [3.27,370.43]j |
OR 0.84 [0.81,0.87]g |
. |
| Sepsis | . | . | OR 4.98 [2.2,11.27]a |
. | OR 5.38 [2.86,10.14]k |
OR 1.49 [1.30,1.72]k |
. | OR 1.41 [0.42,4.67]a |
. | . | . | . | . | OR 1.75 [0.71,2.86]l |
| Ethnicity | . | OR 0.571 [p = 0.317]d,m |
OR 0.36 [0.17,0.78]n |
. | . | OR 1.22 [1.09,1.35]m |
. | . | . | . | OR 1.68 [p < 0.001]d,h,m |
. | . | . |
| Hypotension | . | . | . | . | . | OR 1.51 [1.36,1.69]o |
. | . | . | . | . | . | . | OR 2.00 [1.001,3.999]o |
| Outborn | . | . | . | . | . | OR 1.31 [1.17,1.46] |
. | . | . | . | . | . | OR 1.55 [1.31,1.83] |
. |
| Assisted ventilation | . | OR 1.053 [p = 0.047]d,a |
. | . | OR 2.71 [1.03,7.15]a |
. | OR 3.5 [2.5,4.7]p |
. | . | . | . | . | . | . |
| Cesarean section | . | . | . | . | . | . | OR 0.60 [0.50,0.80] |
. | . | . | OR 0.60 [p < 0.001]d,h |
. | . | . |
| PROM | . | . | OR 2.06 [1.02,4.16] |
. | . | . | . | . | . | . | OR 1.10 [p < 0.009]d,h |
. | . | . |
| Small for gestational ageb | . | . | . | . | . | . | . | . | OR 1.97 [1.19,3.26]a |
. | . | . | OR 1.35 [1.08,1.69]q |
. |
| Surfactant | OR 1.59 [1.17,2.16] |
. | . | . | OR 0.41 [0.19,0.90] |
. | . | . | . | . | . | . | . | . |
This table shows the strength and the direction of association of prognostic factors, with concomitant confidence intervals if available
NEC necrotizing enterocolitis, OR odds ratio, PROM premature rupture of membranes
Footnotes: a exact definition was lacking; b cutt-off values differs between studies; c < 1500 g; d no CI was given or could be calculated; e < 1500 g or requiring mechanical ventilation at birth; f OR increased with decreasing weight, no exact ratio was given; g calculated for increase of one unit of the continuous variable; h calculated by results presented in article; i < 28 weeks; j < 26 weeks; k late-onset sepsis; l combination of early- and late-onset sepsis; m black ethnicity; n white ethnicity; o inotropics requirement; p mechanical ventilation first day of life; q < 10th percentile for the given GA
Because of the diversity in study population, definition and incidence of outcome and type of analysis, the measures of associations need to be interpreted in the context of the study characteristics as reported in Table 2. Because of substantial heterogeneity in design, population, prognostic factors and outcomes of the included prognostic studies, it was not feasible to perform a meta-analysis.
Discussion
This is the first systematic review of prognostic studies on risk factors for NEC in neonates. Only three of the 14 included studies scored high for methodological quality; all others scored moderate. This was mostly because of limited information on definition and measurement of the prognostic factor and on the outcome of NEC. Only one report was found on the development of a prediction model for the outcome of NEC [18].
We defined a prognostic study design based on several specific criteria suggested in the literature. Aiming to estimate the risk of developing a future clinical outcome (NEC) based on more than one (independent) characteristic, is considered the key feature of a prognostic study design [12–14]. Therefore we only included studies with a defined study population and multivariable analysis of variables of potential equal importance. We did not include trials or studies that focused on the association between NEC and a single risk factor. Although these studies may generate relevant hypotheses, these do not address prognostic questions from a clear prognostic research perspective [12].
Risk factors for NEC
Low birth weight is the most commonly reported significant prognostic factor for NEC among neonates in the current literature, which is in line with large cohort studies describing the highest incidence of NEC among the infants with the lowest birth weights [19, 20]. Interestingly, the clinical relevance of birth weight as an independent prognostic factor for NEC is questionable with odds ratios (ORs) ranging between 0.999–1.001 [21–24]. Presumably, low gestational age or being small for gestational age are clinically more important. However, associations between NEC and these factors were only confirmed by multivariable analysis in four and two of the studies respectively [18, 25–27].
Also of interest, two studies showed a protective effect of cesarean section for developing NEC (OR both 0.60) [23, 24]. The authors suggest that this is due to less stress during delivery, although they point out that selection bias may have occurred. Surfactant therapy proved a positive predictor for NEC in one study but a negative predictor in another [21, 28]. The authors of the latter study explained this by improvement of pulmonary function leading to less gut ischemia. Boo et al. reported that surfactant was administered only to infants with severe respiratory distress syndrome (RDS), suggesting that not surfactant but severe RDS was a significant risk factor for NEC [21]. Kliegman et al. studied RDS and NEC and concluded that neonatal hypoxia is not etiologically related to NEC [29]. They found that mild or no RDS was associated with an increased risk of NEC in contrast to severe RDS, however by performing only univariable analysis. It is unclear whether this can be explained by a protective effect of surfactant in the severe cases or by other factors such as different nutritional or antibiotic treatment. Assisted ventilation was also associated with an increased risk of NEC [22, 23, 28]. The question arises whether this reflects disease severity - as the sickest patients (with the highest risk for NEC) will need ventilation - or the mechanical ventilation itself, as disease severity (other than by birth weight and gestation age) was not adjusted for in all of these studies.
Gephart et al. were the only authors who described the development of a prediction model. Their model (GutCheckNEC) included 10 clinical risk factors based on a large neonatal dataset [18]. They found that hypotension requiring inotropic treatment was associated with an increased risk of NEC. Also, Youn et al. considered hypotension within a week of life, as an independent risk factor for NEC [30]. They suggest that the circulatory collapse in the first week of life may assault the gastrointestinal blood flow resulting in higher NEC incidence. Two studies showed neonates who were born outside of the hospital were at greater risk for developing NEC compared to inborn neonates, which was also included in the model of Gephart et al. [18, 27].
The only maternal or perinatal prognostic factors for which evidence in the prognostic literature was found were PROM, cesarean section and being inborn. Interestingly, for commonly assumed clinical neonatal risk factors for NEC such as umbilical lines, red cell transfusions, H2 blockers, and (high osmolar) formula feeding no prognostic evidence was found [20, 31–35]. These factors showed no significant associations in prognostic studies, or have only been reported in studies without a prognostic design.
White ethnicity was associated with a lower risk for NEC compared to black ethnicity in multivariable analyses [18, 24, 36]. However, one study could not confirm these findings, probably due to the overwhelming effects of other factors in the multivariable model [22]. Another finding from two multivariable analyses is an association between diagnosis and treatment of sepsis and NEC, which was defined as blood culture proven late onset sepsis in one study and undefined sepsis prior to NEC in the other [28, 36].
Interpretation of results
When interpreting the results, the following considerations should be taken into account. Firstly, most included studies were of limited quality and heterogeneous. The incidence of NEC stages II-III varied widely, probably due to differences in the selection of the study population and in NEC classification [18, 21–28, 30, 36–39].
Secondly, predictability is not synonymous to causality, although this is often inferred. This is most striking in studies that are unclear on or even ignore the temporality between exposure and onset of outcome. This was nicely pointed out by Patel et al., who studied the association between red blood cell (RBC) transfusions and NEC. They showed that severe anemia but not red blood cell (RBC) transfusion was associated with an increased risk of NEC and suggested that prevention of anemia may be more beneficial than minimizing RBC transfusions [40].
Discriminating etiologic and prognostic study designs is complex, especially because the methodological approaches overlap to some extent. Prognostic research focuses on the probability of a particular state of health whereas etiological research aims to assess the causal relationship between risk factors and outcome. Therefore every causal factor is a predictor but not every predictor is causally related to the outcome [12, 41].
Lastly, the problem of unreported negative findings even within a published report is worth mentioning. Not all studies described the total set of baseline variables included in the multivariable model. Univariable significant factors may have tested non-significant in multivariable models and left out of the final model. By not reporting non-significant factors, it remains impossible to rule out factors that are often assumed to be predictors for NEC. Also, the prognostic factors reported in this review, may have been non-significant in other reports.
Strengths and limitations
Strengths of this review are the broad search strategy, the systematic rating of risk of bias using QUIPS and reporting of data according to PRISMA. Dretzke’s key points for the methodological approach for systematic review of prognostic factors were followed [42].
Nevertheless, several limitations may have influenced our study selection and results. Reliable identification of prognostic studies can be difficult especially in case of incomplete reporting and diversity of terminology [42]. Language bias may have occurred by excluding non-English articles. Earlier reported but arbitrarily set cut-off points for low, moderate and high quality in the QUIPS rating were used. Prognostic factors studied once were not summarized in this review but can also be relevant predictors of NEC. This concerned, for example, the only report on multivessel fetal Doppler imaging, by Manogura et al., which still may be relevant [39].
Future perspectives
Well-designed prospective prognostic studies are needed with detailed reporting on definitions, methods and measurement of the prognostic factor and outcome. Special attention should be given to timing of the exposures in relation to the diagnosis of NEC. It would be interesting not only to focus on patient factors but also on maternal factors. Maternal lifestyle factors (such as smoking and obesity), morbidity (such as diabetes, preeclampsia, and chorioamnionitis) and prenatal medication (such as antibiotics and corticosteroids) may also be relevant risk factors for NEC [43–48]. A second step is the development and validation of a prediction model to quantify individual risk profiles and identify patients at risk. Until now this has only been performed by Gephart et al. who developed a model based on a large set of retrospective data. Their model still needs external validation in other neonatal populations to evaluate its general clinical usefulness. In our opinion development and validation of prospective prediction models are still necessary for preventive strategies and future reduction of the incidence of NEC.
Conclusion
It is concluded that high quality studies on prognostic factors for NEC are rare. Several prognostic factors are associated with NEC, of which not all are necessarily causal. Ruling out factors is hampered by incomplete reporting. Future high quality prognostic (and predictive) research is necessary to enable clinicians to identify patients at high risk for NEC.
Acknowledgements
We gratefully appreciate the support of our biomedical information specialist, Wichor M. Bramer, who contributed to the literature search.
Funding
Not applicable.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Authors’ contributions
All authors were involved in the concept and design of the study. NS and RG conducted independent literature searches, quality assessment, and data extraction and wrote the first draft of the manuscript. MJV and RCJ supervised the article selection, quality assessment and data presentation. MJV, RCJ and IKMR critically reviewed and revised the manuscript. All authors have read and approved the final manuscript and agree to be accountable for all aspects of the work. No form of payment was given to anyone to produce the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ELBW
Extremely low birth weight
- EPO
Erythropoietin
- IVH
Intraventricular hemorrhage
- NCPAP
Nasal continuous positive airway pressure
- NEC
Necrotizing enterocolitis
- NICU
Neonatal intensive care unit
- OR
Odds ratio
- PDA
Patent ductus arteriosus
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- PROM
Premature rupture of membranes
- QUIPS
Quality in prognosis studies
- RDS
Respiratory distress syndrome
- RR
Relative risk
- SNAP
Score for neonatal acute physiology
- TPN
Total parenteral nutrition
- VLBW
Very low birth weight
Additional file
Literature search strategy. (DOCX 118 kb)
References
- 1.Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364(3):255–264. doi: 10.1056/NEJMra1005408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson AM, Bizzarro MJ. Necrotizing enterocolitis in newborns: pathogenesis, prevention and management. Drugs. 2008;68(9):1227–1238. doi: 10.2165/00003495-200868090-00004. [DOI] [PubMed] [Google Scholar]
- 3.Patel RM, Kandefer S, Walsh MC, Bell EF, Carlo WA, Laptook AR, Sanchez PJ, Shankaran S, Van Meurs KP, Ball MB, et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med. 2015;372(4):331–340. doi: 10.1056/NEJMoa1403489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin PW, Stoll BJ. Necrotising enterocolitis. Lancet. 2006;368(9543):1271–1283. doi: 10.1016/S0140-6736(06)69525-1. [DOI] [PubMed] [Google Scholar]
- 5.Schulzke SM, Deshpande GC, Patole SK. Neurodevelopmental outcomes of very low-birth-weight infants with necrotizing enterocolitis: a systematic review of observational studies. Arch Pediatr Adolesc Med. 2007;161(6):583–590. doi: 10.1001/archpedi.161.6.583. [DOI] [PubMed] [Google Scholar]
- 6.AlFaleh K, Anabrees J. Probiotics for prevention of necrotizing enterocolitis in preterm infants. Cochrane Database Syst Rev. 2014;4:CD005496. doi: 10.1002/14651858.CD005496.pub4. [DOI] [PubMed] [Google Scholar]
- 7.Bury RG, Tudehope D. Enteral antibiotics for preventing necrotizing enterocolitis in low birthweight or preterm infants. Cochrane Database Syst Rev. 2001;1:CD000405. doi: 10.1002/14651858.CD000405. [DOI] [PubMed] [Google Scholar]
- 8.Good M, Sodhi CP, Hackam DJ. Evidence-based feeding strategies before and after the development of necrotizing enterocolitis. Expert Rev Clin Immunol. 2014;10(7):875–884. doi: 10.1586/1744666X.2014.913481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halac E, Halac J, Begue EF, Casanas JM, Indiveri DR, Petit JF, Figueroa MJ, Olmas JM, Rodriguez LA, Obregon RJ, et al. Prenatal and postnatal corticosteroid therapy to prevent neonatal necrotizing enterocolitis: a controlled trial. J Pediatr. 1990;117(1 Pt 1):132–138. doi: 10.1016/S0022-3476(05)72461-6. [DOI] [PubMed] [Google Scholar]
- 10.Deshpande G, Rao S, Patole S, Bulsara M. Updated meta-analysis of probiotics for preventing necrotizing enterocolitis in preterm neonates. Pediatrics. 2010;125(5):921–930. doi: 10.1542/peds.2009-1301. [DOI] [PubMed] [Google Scholar]
- 11.Markel TA, Crisostomo PR, Wairiuko GM, Pitcher J, Tsai BM, Meldrum DR. Cytokines in necrotizing enterocolitis. Shock. 2006;25(4):329–337. doi: 10.1097/01.shk.0000192126.33823.87. [DOI] [PubMed] [Google Scholar]
- 12.Moons KG, Royston P, Vergouwe Y, Grobbee DE, Altman DG. Prognosis and prognostic research: what, why, and how? BMJ. 2009;338:b375. doi: 10.1136/bmj.b375. [DOI] [PubMed] [Google Scholar]
- 13.Hemingway H, Croft P, Perel P, Hayden JA, Abrams K, Timmis A, Briggs A, Udumyan R, Moons KG, Steyerberg EW, et al. Prognosis research strategy (PROGRESS) 1: a framework for researching clinical outcomes. BMJ. 2013;346 doi: 10.1136/bmj.e5595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riley RD, Hayden JA, Steyerberg EW, Moons KG, Abrams K, Kyzas PA, Malats N, Briggs A, Schroter S, Altman DG, et al. Prognosis Research Strategy (PROGRESS) 2: prognostic factor research. PLoS Med. 2013;10(2):e1001380. doi: 10.1371/journal.pmed.1001380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 17.de Jonge RC, van Furth AM, Wassenaar M, Gemke RJ, Terwee CB. Predicting sequelae and death after bacterial meningitis in childhood: a systematic review of prognostic studies. BMC Infect Dis. 2010;10:232. doi: 10.1186/1471-2334-10-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gephart SM, Spitzer AR, Effken JA, Dodd E, Halpern M, McGrath JM. Discrimination of GutCheck(NEC): a clinical risk index for necrotizing enterocolitis. J Perinatol. 2014;34(6):468–475. doi: 10.1038/jp.2014.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark RH, Gordon P, Walker WM, Laughon M, Smith PB, Spitzer AR. Characteristics of patients who die of necrotizing enterocolitis. J Perinatol. 2012;32(3):199–204. doi: 10.1038/jp.2011.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Llanos AR, Moss ME, Pinzon MC, Dye T, Sinkin RA, Kendig JW. Epidemiology of neonatal necrotising enterocolitis: a population-based study. Paediatr Perinat Epidemiol. 2002;16(4):342–349. doi: 10.1046/j.1365-3016.2002.00445.x. [DOI] [PubMed] [Google Scholar]
- 21.Boo NY, Cheah IG. Risk factors associated with necrotising enterocolitis in very low birth weight infants in Malaysian neonatal intensive care units. Singap Med J. 2012;53(12):826–831. [PubMed] [Google Scholar]
- 22.Carter BM, Holditch-Davis D. Risk factors for necrotizing enterocolitis in preterm infants: how race, gender, and health status contribute. Adv Neonatal Care. 2008;8(5):285–290. doi: 10.1097/01.ANC.0000338019.56405.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guthrie SO, Gordon PV, Thomas V, Thorp JA, Peabody J, Clark RH. Necrotizing enterocolitis among neonates in the United States. J Perinatol. 2003;23(4):278–285. doi: 10.1038/sj.jp.7210892. [DOI] [PubMed] [Google Scholar]
- 24.Uauy RD, Fanaroff AA, Korones SB, Phillips EA, Phillips JB, Wright LL. Necrotizing enterocolitis in very low birth weight infants: biodemographic and clinical correlates. National Institute of Child Health and Human Development Neonatal Research Network. J Pediatr. 1991;119(4):630–638. doi: 10.1016/S0022-3476(05)82418-7. [DOI] [PubMed] [Google Scholar]
- 25.Luig M, Lui K. Nsw, Group AN: Epidemiology of necrotizing enterocolitis--Part II: Risks and susceptibility of premature infants during the surfactant era: a regional study. J Paediatr Child Health. 2005;41(4):174–179. doi: 10.1111/j.1440-1754.2005.00583.x. [DOI] [PubMed] [Google Scholar]
- 26.Yamoto M, Nakazawa Y, Fukumoto K, Miyake H, Nakajima H, Sekioka A, Nomura A, Ooyama K, Yamada Y, Nogami K, et al. Risk factors and prevention for surgical intestinal disorders in extremely low birth weight infants. Pediatr Surg Int. 2016;32(9):887–893. doi: 10.1007/s00383-016-3940-z. [DOI] [PubMed] [Google Scholar]
- 27.Yee WH, Soraisham AS, Shah VS, Aziz K, Yoon W, Lee SK, Canadian Neonatal N. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129(2):e298–e304. doi: 10.1542/peds.2011-2022. [DOI] [PubMed] [Google Scholar]
- 28.Gagliardi L, Bellu R, Cardilli V, De Curtis M, Network Neonatale L. Necrotising enterocolitis in very low birth weight infants in Italy: incidence and non-nutritional risk factors. J Pediatr Gastroenterol Nutr. 2008;47(2):206–210. doi: 10.1097/MPG.0b013e318174e855. [DOI] [PubMed] [Google Scholar]
- 29.Kliegman RM, Hack M, Jones P, Fanaroff AA. Epidemiologic study of necrotizing enterocolitis among low-birth-weight infants. Absence of identifiable risk factors. J Pediatr. 1982;100(3):440–444. doi: 10.1016/S0022-3476(82)80456-3. [DOI] [PubMed] [Google Scholar]
- 30.Youn YA, Kim EK, Kim SY. Necrotizing Enterocolitis among Very-Low-Birth-Weight Infants in Korea. J Korean Med Sci. 2015;30(Suppl 1):S75–S80. doi: 10.3346/jkms.2015.30.S1.S75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Been JV, Lievense S, Zimmermann LJ, Kramer BW, Wolfs TG. Chorioamnionitis as a risk factor for necrotizing enterocolitis: a systematic review and meta-analysis. J Pediatr. 2013;162(2):236–242. doi: 10.1016/j.jpeds.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 32.Holman RC, Stoll BJ, Curns AT, Yorita KL, Steiner CA, Schonberger LB. Necrotising enterocolitis hospitalisations among neonates in the United States. Paediatr Perinat Epidemiol. 2006;20(6):498–506. doi: 10.1111/j.1365-3016.2006.00756.x. [DOI] [PubMed] [Google Scholar]
- 33.Martinez-Tallo E, Claure N, Bancalari E. Necrotizing enterocolitis in full-term or near-term infants: risk factors. Biol Neonate. 1997;71(5):292–298. doi: 10.1159/000244428. [DOI] [PubMed] [Google Scholar]
- 34.Rand T, Weninger M, Kohlhauser C, Bischof S, Heinz-Peer G, Trattnig S, Popow C, Salzer HR. Effects of umbilical arterial catheterization on mesenteric hemodynamics. Pediatr Radiol. 1996;26(7):435–438. doi: 10.1007/BF01377197. [DOI] [PubMed] [Google Scholar]
- 35.Stout G, Lambert DK, Baer VL, Gordon PV, Henry E, Wiedmeier SE, Stoddard RA, Miner CA, Schmutz N, Burnett J, et al. Necrotizing enterocolitis during the first week of life: a multicentered case-control and cohort comparison study. J Perinatol. 2008;28(8):556–560. doi: 10.1038/jp.2008.36. [DOI] [PubMed] [Google Scholar]
- 36.Drenckpohl D, Knaub L, Schneider C. Risk factors that may predispose premature infants to increased incidence of necrotizing enterocolitis. ICAN: infant, Child, & Adolescent Nutrition 2010;2(1):37–44.
- 37.Faustini A, Forastiere F, Giorgi Rossi P, Perucci CA. An epidemic of gastroenteritis and mild necrotizing enterocolitis in two neonatal units of a University Hospital in Rome. Italy Epidemiol Infect. 2004;132(3):455–465. doi: 10.1017/S0950268804002006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee JY, Park KH, Kim A, Yang HR, Jung EY, Cho SH. Maternal and Placental Risk Factors for Developing Necrotizing Enterocolitis in Very Preterm Infants. Pediatr. Neonatol 2016;58(1):57–62. [DOI] [PubMed]
- 39.Manogura AC, Turan O, Kush ML, Berg C, Bhide A, Turan S, Moyano D, Bower S, Nicolaides KH, Galan HL, et al. Predictors of necrotizing enterocolitis in preterm growth-restricted neonates. Am J Obstet Gynecol. 2008;198(6):638 e631–638 e635. doi: 10.1016/j.ajog.2007.11.048. [DOI] [PubMed] [Google Scholar]
- 40.Patel RM, Knezevic A, Shenvi N, Hinkes M, Keene S, Roback JD, Easley KA, Josephson CD. Association of Red Blood Cell Transfusion, Anemia, and Necrotizing Enterocolitis in Very Low-Birth-Weight Infants. JAMA. 2016;315(9):889–897. doi: 10.1001/jama.2016.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tripepi G, Jager KJ, Dekker FW, Zoccali C. Testing for causality and prognosis: etiological and prognostic models. Kidney Int. 2008;74(12):1512–1515. doi: 10.1038/ki.2008.416. [DOI] [PubMed] [Google Scholar]
- 42.Dretzke J, Ensor J, Bayliss S, Hodgkinson J, Lordkipanidze M, Riley RD, Fitzmaurice D, Moore D. Methodological issues and recommendations for systematic reviews of prognostic studies: an example from cardiovascular disease. Syst Rev. 2014;3:140. doi: 10.1186/2046-4053-3-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cetinkaya M, Ozkan H, Koksal N. Maternal preeclampsia is associated with increased risk of necrotizing enterocolitis in preterm infants. Early Hum Dev. 2012;88(11):893–898. doi: 10.1016/j.earlhumdev.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 44.Downard CD, Grant SN, Maki AC, Krupski MC, Matheson PJ, Bendon RW, Fallat ME, Garrison RN. Maternal cigarette smoking and the development of necrotizing enterocolitis. Pediatrics. 2012;130(1):78–82. doi: 10.1542/peds.2011-3808. [DOI] [PubMed] [Google Scholar]
- 45.Garcia-Munoz Rodrigo F, Galan Henriquez G, Figueras Aloy J, Garcia-Alix Perez A. Outcomes of very-low-birth-weight infants exposed to maternal clinical chorioamnionitis: a multicentre study. Neonatology. 2014;106(3):229–234. doi: 10.1159/000363127. [DOI] [PubMed] [Google Scholar]
- 46.Weintraub AS, Ferrara L, Deluca L, Moshier E, Green RS, Oakman E, Lee MJ, Rand L. Antenatal antibiotic exposure in preterm infants with necrotizing enterocolitis. J Perinatol. 2012;32(9):705–709. doi: 10.1038/jp.2011.180. [DOI] [PubMed] [Google Scholar]
- 47.Wong D, Abdel-Latif M, Kent A, Network N. Antenatal steroid exposure and outcomes of very premature infants: a regional cohort study. Arch Dis Child Fetal Neonatal Ed. 2014;99(1):F12–F20. doi: 10.1136/archdischild-2013-304705. [DOI] [PubMed] [Google Scholar]
- 48.Grandi C, Tapia JL, Cardoso VC. Impact of maternal diabetes mellitus on mortality and morbidity of very low birth weight infants: a multicenter Latin America study. J Pediatr. 2015;91(3):234–241. doi: 10.1016/j.jped.2014.08.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files.


