Abstract
Context
The optimal lower extremity venous ultrasound (US) protocol to diagnose deep venous thrombosis of the popliteal and more proximal veins is unclear.
Objective
To determine the three-month rate of symptomatic venous thromboembolism (VTE) and clinical outcomes of inpatients and ambulatory patients with normal findings on single venous ultrasound of the popliteal and more proximal veins (single proximal US).
Design
Single proximal US results and clinical data of all inpatient and ambulatory patients with suspected acute deep venous thrombosis were retrospectively reviewed during a 12-month period between January and December 2014. Three-month follow-up data were reviewed for all these patients, who received all their care from a single geographically isolated health maintenance organization.
Main Outcome Measures
Three-month rate of symptomatic VTE and clinical outcomes after an initially normal single proximal US result.
Results
Of 1295 patients, 111 (8.6%) were found to have acute deep venous thrombosis on the initial proximal US. Of the remaining 1184 patients with initially normal results on proximal US who were sampled at 3-month follow-up, 1075 patients (90.8%) had no venous thromboembolic event. Among the others, 11 (0.9%) had a subsequent imaging-confirmed venous thromboembolic event, 53 (4.5%) died (none owing to venous thromboembolism), and 45 (3.8%) did not complete follow-up.
Conclusion
Symptomatic VTE after an initially normal single proximal US result occurred in less than 1% of this cohort. Therefore, serial proximal US is unnecessary for most of our patients, and its elimination will save time and out-of-pocket expenses.
INTRODUCTION
Venous thromboembolism (VTE), presenting as pulmonary embolism (PE) or deep venous thrombosis (DVT), affects approximately 100 persons per 100,000 in the USA annually. The incidence of VTE rises exponentially from fewer than 5 cases per 100,000 persons in those younger than age 15 years to 500 cases (0.5%) per 100,000 persons in those older than age 80 years. Even with anticoagulation treatment, VTE has a 7% recurrence rate at 6 months, with death occurring in 6% of DVT cases and 12% of PE cases within 1 month.1
Contrast venography remains the gold standard for the diagnosis of DVT.2 However, compression venous ultrasound (US) is currently the initial modality of choice in terms of cost, availability, and safety profile in diagnosing thrombosis of the femoral and popliteal veins. There is ongoing discussion regarding the optimal scanning protocol. One protocol is imaging of the proximal femoral and popliteal veins with one additional proximal US one week after the initial scan. This protocol will be referred to as serial proximal US.2,3 The second protocol is one-time whole-leg, extended US (single complete US), evaluating both the proximal and distal calf infrapopliteal veins.4,5
Serial proximal US requires repeated scanning in one week in a large number of patients with initially normal US results, most of whom will not have evidence of DVT on their repeated US.6 Single complete US is a time-consuming examination and requires greater expertise on the part of the ultrasonographer. Additionally, single complete US examinations detect a large percentage of calf DVTs, thereby exposing patients to the risks of anticoagulation therapy with questionable benefit.6 At our institution, we have performed only a single, one-time proximal US without a serial examination.
This study aimed to determine the three-month rate of symptomatic VTE and clinical outcomes of inpatients and ambulatory patients after an initially normal single proximal US result.
METHODS
Study Population
The Kaiser Permanente Hawaii institutional review board approved this study with a waiver of patient consent. All patients were part of a single geographically isolated health maintenance organization (HMO) and received all their care in the HMO; all clinical encounters, including inpatient and outpatient visits, were recorded in a common electronic medical record. Our single proximal US protocol included visualization of the iliofemoral junction and saphenofemoral junction, as well as the entire common femoral, superficial femoral, and popliteal veins. Compression, augmentation, and color Doppler US of the femoral and popliteal veins were included.
We retrospectively reviewed all proximal US studies performed because of suspected acute DVT during a 12-month period between January and December 2014 in the HMO. For each patient, we collected the following data: age, sex, clinical indication, result of the single proximal US examination, D-dimer results if obtained by the clinician, all additional imaging studies related to symptomatic venous thromboembolic disease (subsequent US, computed tomography angiography for evaluation of PE, radionuclide ventilation-perfusion scans), and clinical follow-up for 3 months. Patients were followed for symptoms of VTE for at least 3 months, permitting an assessment for VTE not detected on initial single proximal US. All quantitative serum rapid D-dimer assays were performed with use of the latex agglutination technique (STA D-Di, Diagnostica Stago, Parsippany, NJ). The manufacturer reports that a serum D-dimer level less than 0.5 μg/mL fibrinogen-equivalent units should be considered within normal limits.
Three-Month Follow-up
Objective confirmation of VTE was required for all patients returning with suspected VTE. Cause of death was obtained for patients who died within the three-month follow-up period from initial US. Patients without subsequent clinic visits or electronic medical record notes within the three-month follow-up period were considered “lost” to follow-up.
Statistical Analysis
The prevalence rate of acute DVT on US was calculated and compared with previous studies’ prevalence rates. Similarly, the rate of patients lost to follow-up was compared with that of other studies. Nominal variables were evaluated with χ2 tests, and numeric variables were evaluated with t statistics, with significance defined as p < 0.05.
RESULTS
Characteristics of the Study Population
There were 1295 patients who underwent single proximal US in the 12-month interval between January 1 and December 31, 2014. Patient characteristics are presented in Table 1. There were 576 men and 719 women. The mean age of all patients was 64.10 years. There was no significant difference in the ages between men and women (p = 0.78).
Table 1.
Patient characteristics
| Characteristic | DVT on initial US, n = 111 | No DVT on initial US, n = 1184 |
|---|---|---|
| Patient age, mean ± SD (range), years | 64.94 ± 16.79 (28.53–97.54) | 64.03 ± 16.66 (11.17–100.32) |
| D-dimer testing, no. (%) | 15 (14) | 234 (20) |
| Men, no. (%) | 57 (51) | 519 (44) |
| Indications for US, no. (%)a | ||
| Pain or swelling | 94 (85) | 1079 (91) |
| History of DVT/PE | 12 (11) | 75 (6) |
| Miscellaneous (cellulitis, tachycardia, shortness of breath) | 5 (5) | 30 (3) |
| Location of US, no. (%) | ||
| Right proximal leg | 40 (36) | 442 (37) |
| Left proximal leg | 40 (36) | 449 (38) |
| Bilateral proximal legs | 31 (28) | 293 (25) |
Percentages do not total to 100% because of rounding.
DVT = deep venous thrombosis; PE = pulmonary embolism; SD = standard deviation; US = ultrasound.
Initial Ultrasound
Overall, 249 of 1295 patients (19.2%) had D-dimer testing at the time of initial single proximal US. Forty-two of 249 patients (16.9%) had D-dimer values below 0.5 μg/mL, and they all had initially normal single proximal US results. Of 249 patients, 207 (83.1%) had D-dimer values of greater than 0.5 μg/mL. Fifteen of the 207 patients had DVT on initial US, and the remaining 192 of 207 patients had normal initial US results. One of the 192 patients with initially normal single proximal US findings and an elevated D-dimer (D-dimer of 2.29 μg/mL) was found to have PE on subsequent imaging 7 weeks later. (This case will be described subsequently in further detail.) The remaining 191 patients with initially normal US results and D-dimer values greater than 0.5 μg/mL had no clinical symptoms of VTE during the 3-month follow-up period.
Nearly all patients, 1173 (90.6%) of 1295, who underwent US evaluation for DVT presented with lower extremity pain or swelling. A history of DVT or PE was present in 87 of these 1295 patients (6.7%). The remaining 35 (2.7%) of 1295 patients presented with a variety of symptoms, including cellulitis, tachycardia, and/or shortness of breath. An approximately even proportion of patients underwent evaluation for right or left lower extremity DVT: 482 (37.2%) of 1295 patients underwent unilateral right lower extremity proximal US, whereas 489 (37.8%) of 1295 patients underwent unilateral left lower extremity proximal US. The other 324 patients (25.0%) underwent bilateral lower extremity proximal US examinations.
A total of 111 patients (8.6%) demonstrated acute DVT on single proximal US. These 57 men and 54 women who presented with acute DVT did not differ from the patients who did not by any of the following characteristics: age (p = 0.59), sex proportion (p = 0.13), or whether D-dimer level was obtained (p = 0.13). There was an even distribution in the laterality of DVT, with 40 thromboses (36.0%) occurring in the right lower extremity, 40 (36.0%) in the left lower extremity, and 31 (27.9%) occurring bilaterally. There was no difference in the laterality or bilaterality of DVT compared with the distribution of proximal US studies performed (p = 0.76).
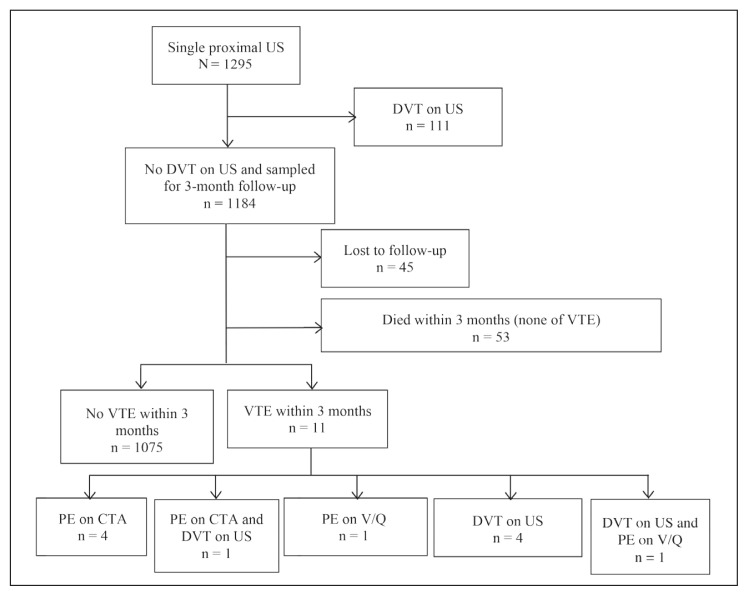
Of the remaining 1184 patients whose initial US showed no evidence of DVT, 45 (3.8%) were lost to follow-up within 3 months of their initial US (Figure 1). An additional 53 patients (4.5%)—35 women and 18 men—died within 3 months of their initial US. However, none of these patients were suspected to have died from VTE, according to their death note. The reported cause of death for these patients included atherosclerotic heart disease in 17 patients (32.1%), underlying malignancy in 20 (37.7%), and other causes, including polytrauma and sepsis, in 16 (30.2%). The mean age at death of these 53 patients was 72.7 years (standard deviation = 13.7 years), with a range of 43.6 to 97.0 years.
Figure 1.
Flow analysis of patients who underwent single proximal US for suspected DVT.
CTA = computed tomography angiography, DVT = deep venous thrombosis, PE = pulmonary embolism, US = ultrasound, V/Q = ventilation-perfusion scan, VTE = venous thromboembolism
Repeated Ultrasound
Among patients who had an initially normal proximal US result, 84 underwent repeated proximal US because of recurrent symptoms within 3 months whose findings remained normal. Eleven of 1184, or 0.9% (95% confidence interval [CI] = 0.4%–1.5%), who had an initially normal US result experienced a subsequent VTE (confirmed with an abnormal VTE imaging study result) within 3 months.
Venous Thromboembolism after an Initially Normal Proximal Venous Ultrasound
Eleven patients experienced VTE within three months after an initially normal proximal US result (Table 2). Within ten days of an initially normal US result, one patient was noted to have DVT on subsequent US and three patients were noted to have PE. Of the three patients with PE, one had DVT found on US, whereas the remaining two patients did not have US repeated. The remaining seven patients were noted to have PE and/or DVT three to eight weeks after the initially normal proximal US result.
Table 2.
Patients with venous thromboembolism after initially normal proximal venous ultrasound
| Age (years), sex | Risk factors | D-dimer at time of initial US (μg/mL) | D-dimer at time of VTE diagnosis (μg/mL) | Symptoms at time of VTE diagnosis | Time from initially normal US to VTE diagnosis (days) | Subsequent PE study | Results of repeated proximal US at time of VTE diagnosis |
|---|---|---|---|---|---|---|---|
| 88, M | History of DVT and PE | NP | 3.88 | Dyspnea and hypoxia | 3 | PE on V/Q | DVT |
| 44, F | History of PE after IVC filter placement, Factor V Leiden mutation, elevated homocysteine level | NP | NP | Dyspnea | 7 | PE on V/Q | NP |
| 64, F | Obesity, metastatic small-bowel carcinoid tumor, hospitalization for treatment of epidural abscess and osteomyelitis after decompression surgery | NP | 3.73 | Hypoxia and tachycardia | 9 | PE on CTA | NP |
| 70, M | Prostate cancer | NP | NP | Lower extremity pain and swelling | 9 | NP | DVT |
| 84, M | Type 2 diabetes | NP | NP | Lower extremity erythema, pain, and swelling | 21 | NP | DVT |
| 66, F | Immobilization because of cuboid fracture | NP | 1.63 | Chest pain | 28 | PE on CTA | NP |
| 61, M | History of DVT and PE | NP | 1.67 | Chest pain | 32 | PE on CTA | DVT |
| 63, F | History of DVT, hospitalization for treatment of acute diverticulitis | NP | 2.12 | Dyspnea and chest pain | 35 | PE on CTA | No DVT |
| 53, F | Metastatic breast cancer, recent lengthy plane ride | 2.29 | NP | Dyspnea and chest pain | 49 | PE on CTA | No DVT |
| 94, F | History of DVT and PE | NP | NP | Lower extremity erythema, pain, and swelling | 49 | NP | DVT |
| 68, M | Metastatic squamous cell of head and neck with recent robotic radiosurgery for pelvic node metastasis | NP | NP | Lower extremity swelling | 60 | NP | DVT |
CTA = computed tomography angiography; DVT = deep venous thrombosis; F = female; IVC = inferior vena cava; M = male; NP = not performed; PE = pulmonary embolism; US = ultrasound, V/Q = ventilation-perfusion scan; VTE = venous thromboembolism.
DISCUSSION
At a time of rising health care costs and increased scrutiny into appropriate utilization of imaging services, we have been reevaluating many of our imaging algorithms. There is some controversy as to the most appropriate method of evaluating patients with suspected lower extremity DVT. Prior studies have focused on the comparison between serial proximal US versus a single complete lower extremity venous US. However, the end points for these studies have been to compare the sensitivities of US for detecting lower extremity DVT, rather than patient-centered clinical outcomes. In this study, we evaluated the clinical outcomes of patients with initially normal proximal US results at a minimum of three-month follow-up.
We found an 8.6% (111 of 1295 patients) prevalence rate of acute proximal DVT on initial US. Our prevalence rate was within the range of previous reported rates of 7.4% to 18.0% for proximal DVT found on single complete US.4,5 We calculated an overall proximal DVT prevalence rate from multiple studies of single complete US.5,7–10 The prevalence rate of acute proximal DVT on single complete US was 9.5%, which was not significantly different from ours (χ2; p = 0.27).
In terms of overall prevalence rate of both proximal and distal DVT, 31% to 61% of all diagnosed cases of DVT in single complete US protocols are attributable to DVT of the distal calf. Consequently, previous studies using single complete US protocols have statistically significantly higher overall DVT prevalence rates than ours, ranging from 13.7%–32.7%.4,5,7–10
Single complete US has been shown to be equivalent to the serial proximal US diagnostic strategy regarding the 3-month incidence of symptomatic VTE among patients with initially normal results. In a prospective, randomized, multicenter trial of ambulatory patients in 2008, Bernardi et al11 reported an incidence of symptomatic VTE of 0.9% (95% CI = 0.3%–1.8%) in the serial proximal US group and in 1.2% (95% CI = 0.5%–2.2%) in the single complete US group, which met established equivalence criteria.
Overall, our 3-month cumulative rate of VTE after a single normal proximal US result was 11 of 1184, or 0.9% (95% CI = 0.4%–1.5%). Our CI overlaps with the reported CIs of serial proximal US protocols. Birdwell et al12 reported a 3-month rate of VTE of 0.6% (CI = 0.1%–2.1%), and Cogo et al13 reported a 0.7% (CI = 0.3%–1.2%) rate at 6-month follow-up after normal serial proximal US results. In these 2 studies, only 77% to 83% of all patients with initially normal results returned 1 week later for repeated US, impairing clinical efficiency.11,12 Moreover, the diagnostic yield of 1-week repeated US was low, with only 0.9% to 5.7% of the total number of DVTs detected on repeated US.11,12 Our data suggest that serial proximal US adds unnecessary cost and inconvenience to patients without improving their clinical outcome.
The United Kingdom National Institute for Health and Clinical Excellence and the American College of Chest Physicians recommend proximal venous US for patients in whom DVT is suspected and who score two or more (“DVT likely”) on the Wells scoring system.13,14 If the US result is normal, a D-dimer test should be ordered. Repeated proximal venous US should be performed six to eight days later in all patients with a positive D-dimer test and a normal initial proximal US result.15, 16
Bernardi et al3 used a serial proximal US protocol, repeating the US 1 week later only in patients with elevated D-dimer results. Their 3-month rate of VTE was 0.4% (CI = 0.0%–0.9%), and they reduced the volume of repeated US scans by 87%.3 Similarly, Wells et al14 reported that patients with low pretest probability and initially normal proximal US results (55% of patients) could forgo the repeated US at 1 week, because their 3-month rate of VTE was 0.6% (CI = 0.1%–1.8%).14 Although just 19.2% of our patients received D-dimer testing at the time of their initial US, only 1 patient with D-dimer value greater than 0.5 μg/mL was subsequently found to have PE 7 weeks after an initially normal US result. Because this was a retrospective study, it is unknown whether a repeated proximal US 1 week later would have diagnosed DVT in this patient. Our study results suggest that with close clinical follow-up, both the initial serum D-dimer testing and repeated US at 1 week can be avoided without compromising the established 3-month rate of VTE or adversely affecting clinical outcomes.
Complete US requires greater skill of vascular technologists, is more time-consuming than proximal US, and may not be readily available in many centers. A highly variable percentage (9.3%–82.7%) of studies with indeterminate findings has been reported in calf US studies.17 Given the low rate of missed DVT with single proximal US, our data suggest that complete US may not be necessary to achieve comparable clinical outcomes.
A review of the existing literature on proximal and complete US showed similar pooled estimates of 3-month thromboembolic rates: 0.6% (95% CI = 0.4%–0.9%) in patients in whom anticoagulation was withheld after normal serial proximal US results, and 0.4% (95% CI = 0.1%–0.6%) in patients undergoing single complete US. Among patients receiving anticoagulation therapy after undergoing single complete US, up to 50% of all DVTs were in the calf,18 and there was no decrease in the 3-month thromboembolic risk.6 Additionally, detecting cases of isolated DVTs of the calf on single complete US may expose patients to the harms of unnecessary anticoagulation, including a 1.1% annual risk of major bleeding.19
In our study, 11 patients experienced VTE within 3 months after a normal proximal US result. Of the 7 patients diagnosed with PE, 2 had DVT on US and 2 had no DVT on US at the time of PE diagnosis. Of the remaining 3 of 7 cases, it is unlikely that 1-week serial US would have changed the clinical outcome. All 11 patients with VTE occurring within 3 months after a normal proximal US result had major risk factors, including a history of VTE and/or an active malignancy, in combination with triggering events such as a recent hospitalization/major surgery and/or immobilization. This suggests that patients at high risk of VTE should be treated differently. Whether this management should be in the form of closer clinical follow-up, D-dimer testing, or serial US is unclear.
The primary limitation of this study is the absence of a direct comparison group that underwent serial proximal US or single complete US in whom clinical outcomes could be assessed. However, there was no mention of VTE as a cause of mortality in those patients who died during the 3-month follow-up period. A related limitation is the small group of patients (3.5%) who were lost to follow-up. However, this was a retrospective study, and we did not have the ability to perform telephone interviews with patients, as was the case in previous studies4,5,9,10,20 that reported a 0% to 1.8% loss to follow-up rate. However, we would expect that in a geographically isolated HMO such as ours, those patients with continued or worsening symptoms would have sought further care in the HMO.
At a time when utilization of resources is of concern to all health care providers, use of a streamlined approach to US evaluation of acute DVT is highly desirable. Given the high volume of US examinations and procedures performed at our institution, it has not been practical to perform routine serial proximal US. In addition, we lack an adequate number of certified vascular US technologists to perform complete US examinations, and there is likely to be a high rate of nondiagnostic studies when noncertified technologists are asked to perform complete US examinations.
Our results show that clinical outcomes after single proximal US for evaluation of DVT are not significantly different from those reported by studies of serial proximal US or complete US. Therefore, single proximal US is sufficient to detect clinically relevant acute DVT, without the added time and cost to most patients. The strength of our study is the generalizability to routine clinical practice at other medical centers with similar DVT rates.
CONCLUSION
Symptomatic VTE after an initially normal single proximal US result occurred in less than 1% of this cohort. Therefore, serial proximal US is unnecessary for most of our patients, and single proximal US saves them both time and out-of-pocket expenses. Other institutions should evaluate their own clinical outcomes data to verify these results.
Acknowledgment
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.White RH. The epidemiology of venous thromboembolism. Circulation. 2003 Jun 17;107(23 Suppl 1):I4–8. doi: 10.1161/01.CIR.0000078468.11849.66. DOI: https://doi.org/10.1161/01.cir.0000078468.11849.66. [DOI] [PubMed] [Google Scholar]
- 2.Lensing AW, Prandoni P, Brandjes D, et al. Detection of deep-vein thrombosis by real-time B-mode ultrasonography. N Engl J Med. 1989 Feb 9;320(6):342–5. doi: 10.1056/NEJM198902093200602. DOI: https://doi.org/10.1056/nejm198902093200602. [DOI] [PubMed] [Google Scholar]
- 3.Bernardi E, Prandoni P, Lensing AW, et al. D-dimer testing as an adjunct to ultrasonography in patients with clinically suspected deep vein thrombosis: Prospective cohort study. The Multicentre Italian D-dimer Ultrasound Study Investigators Group. BMJ. 1998 Oct 17;317(7165):1037–40. doi: 10.1136/bmj.317.7165.1037. DOI: https://doi.org/10.1136/bmj.317.7165.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elias A, Mallard L, Elias M, et al. A single complete ultrasound investigation of the venous network for the diagnostic management of patients with a clinically suspected first episode of deep venous thrombosis of the lower limbs. Thromb Haemost. 2003 Feb;89(2):221–7. [PubMed] [Google Scholar]
- 5.Schellong SM, Schwarz T, Halbritter K, et al. Complete compression ultrasonography of the leg veins as a single test for the diagnosis of deep vein thrombosis. Thromb Haemost. 2003 Feb;89(2):228–34. [PubMed] [Google Scholar]
- 6.Guanella R, Righini M. Serial limited versus single complete compression ultrasonography for the diagnosis of lower extremity deep vein thrombosis. Semin Respir Crit Care Med. 2012 Apr;33(2):144–50. doi: 10.1055/s-0032-1311793. DOI: https://doi.org/10.1055/s-0032-1311793. [DOI] [PubMed] [Google Scholar]
- 7.Stevens SM, Elliott CG, Chan KJ, Egger MJ, Ahmed KM. Withholding anticoagulation after a negative result on duplex ultrasonography for suspected symptomatic deep venous thrombosis. Ann Intern Med. 2004 Jun 15;140(12):985–91. doi: 10.7326/0003-4819-140-12-200406150-00007. DOI: https://doi.org/10.7326/0003-4819-140-12-200406150-00007. [DOI] [PubMed] [Google Scholar]
- 8.Subramaniam RM, Heath R, Chou T, Cox K, Davis G, Swarbrick M. Deep venous thrombosis: Withholding anticoagulation therapy after negative complete lower limb US findings. Radiology. 2005 Oct;237(1):348–52. doi: 10.1148/radiol.2371041294. DOI: https://doi.org/10.1148/radiol.2371041294. [DOI] [PubMed] [Google Scholar]
- 9.Sevestre MA, Labarère J, Casez P, et al. Accuracy of complete compression ultrasound in ruling out suspected deep venous thrombosis in the ambulatory setting. A prospective cohort study. Thromb Haemost. 2009 Jul;102(1):166–72. doi: 10.1160/TH09-01-0048. DOI: https://doi.org/10.1160/th09-01-0048. [DOI] [PubMed] [Google Scholar]
- 10.Sevestre MA, Labarère J, Casez P, et al. Outcomes for inpatients with normal findings on whole-leg ultrasonography: A prospective study. Am J Med. 2010 Feb;123(2):158–65. doi: 10.1016/j.amjmed.2009.05.034. DOI: https://doi.org/10.1016/j.amjmed.2009.05.034. [DOI] [PubMed] [Google Scholar]
- 11.Bernardi E, Camporese G, Büller HR, et al. Serial 2-point ultrasonography plus D-dimer vs whole-leg color-coded Doppler ultrasonography for diagnosing suspected symptomatic deep vein thrombosis: A randomized controlled trial. JAMA. 2008 Oct 8;300(14):1653–9. doi: 10.1001/jama.300.14.1653. DOI: https://doi.org/10.1001/jama.300.14.1653. [DOI] [PubMed] [Google Scholar]
- 12.Birdwell BG, Raskob GE, Whitsett TL, et al. The clinical validity of normal compression ultrasonography in outpatients suspected of having deep venous thrombosis. Ann Intern Med. 1998 Jan 1;128(1):1–7. doi: 10.7326/0003-4819-128-1-199801010-00001. DOI: https://doi.org/10.7326/0003-4819-128-1-199801010-00001. [DOI] [PubMed] [Google Scholar]
- 13.Cogo A, Lensing AW, Koopman MM, et al. Compression ultrasonography for diagnostic management of patients with clinically suspected deep vein thrombosis: Prospective cohort study. BMJ. 1998 Jan 3;316(7124):17–20. doi: 10.1136/bmj.316.7124.17. DOI: https://doi.org/10.1136/bmj.316.7124.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells PS, Hirsh J, Anderson DR, et al. Accuracy of clinical assessment of deep-vein thrombosis. Lancet. 1995 May 27;345(8961):1326–30. doi: 10.1016/s0140-6736(95)92535-x. DOI: https://doi.org/10.1016/S0140-6736(95)92535-X. Erratum in: Lancet 1995 Aug 19;346(8973):516. DOI: https://doi.org/10.1016/S0140-6736(95)91372-6. [DOI] [PubMed] [Google Scholar]
- 15.Wells PS, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997 Dec 20–27;350(9094):1795–8. doi: 10.1016/S0140-6736(97)08140-3. Doi: https://doi.org/10.1016/s0140-6736(97)08140-3. [DOI] [PubMed] [Google Scholar]
- 16.Chong LY, Fenu E, Stansby G, Hodgkinson S Guideline Development Group. Management of venous thromboembolic diseases and the role of thrombophilia testing: Summary of NICE guidance. BMJ. 2012 Jun 27;344:e3979. doi: 10.1136/bmj.e3979. DOI: https://doi.org/10.1136/bmj.e3979. [DOI] [PubMed] [Google Scholar]
- 17.Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuünemann HJ American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel. Executive summary: Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012 Feb;141(2 Suppl):7S–47S. doi: 10.1378/chest.1412S3. DOI: https://doi.org/10.1378/chest.1412S3. Erratum in: Chest 2012 Apr;141(4):1129. DOI: https://doi.org/10.1378/chest.141.4.1129a. Erratum in: Chest 2012 Dec;142(6):1698. DOI: https://doi.org/10.1378/chest.12-2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gottlieb RH, Widjaja J, Tian L, Rubens DJ, Voci SL. Calf sonography for detecting deep venous thrombosis in symptomatic patients: Experience and review of the literature. J Clin Ultrasound. 1999 Oct;27(8):415–20. doi: 10.1002/(sici)1097-0096(199910)27:8<415::aid-jcu1>3.0.co;2-6. DOI: https://doi.org/10.1002/(sici)1097-0096(199910)27:8<415::aid-jcu1>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 19.Righini M, Paris S, Le Gal G, Laroche JP, Perrier A, Bounameaux H. Clinical relevance of distal deep vein thrombosis. Review of literature data. Thromb Haemost. 2006 Jan;95(1):56–64. DOI: https://doi.org/10.1160/th05-08-0588. [PubMed] [Google Scholar]
- 20.Krakow E, Ortel TL. Continuing anticoagulation following venous thromboembolism. JAMA. 2005 Dec 28;294(24):3088. doi: 10.1001/jama.294.24.3088-a. author reply 3088–9. DOI: https://doi.org/10.1001/jama.294.24.3088-a. [DOI] [PubMed] [Google Scholar]