Abstract
Background
We explored the application of 3-dimensional (3D) printing technology in treating giant cell tumors (GCT) of the proximal tibia. A tibia block was designed and produced through 3D printing technology. We expected that this 3D-printed block would fill the bone defect after en-bloc resection. Importantly, the block, combined with a standard knee joint prosthesis, provided attachments for collateral ligaments of the knee, which can maintain knee stability.
Material/Methods
A computed tomography (CT) scan was taken of both knee joints in 4 patients with GCT of the proximal tibia. We developed a novel technique – the real-size 3D-printed proximal tibia model – to design preoperative treatment plans. Hence, with the application of 3D printing technology, a customized proximal tibia block could be designed for each patient individually, which fixed the bone defect, combined with standard knee prosthesis.
Results
In all 4 cases, the 3D-printed block fitted the bone defect precisely. The motion range of the affected knee was 90 degrees on average, and the soft tissue balance and stability of the knee were good. After an average 7-month follow-up, the MSTS score was 19 on average. No sign of prosthesis fracture, loosening, or other relevant complications were detected.
Conclusions
This technique can be used to treat GCT of the proximal tibia when it is hard to achieve soft tissue balance after tumor resection. 3D printing technology simplified the design and manufacturing progress of custom-made orthopedic medical instruments. This new surgical technique could be much more widely applied because of 3D printing technology.
MeSH Keywords: Arthroplasty, Replacement, Knee; Giant Cell Tumor of Bone; Imaging, Three-Dimensional
Background
Giant cell tumor (GCT) of bone is a rare, benign, but locally invasive neoplasm, accounting for 3–5% of all primary bone tumors [1,2]. GCT mostly involves the distal femur, followed by proximal tibia and distal radius [3]. The choice of surgical treatments in patients with GCT of the proximal tibia include either intralesional curettage with a high-speed burr, cryotherapy or prenylation, cementation or bone grafting, or en-bloc resection and reconstruction. For primary cases, intralesional curettage with adjuvant methods is the main choice when the local recurrence rate is relatively high [4]. In local recurrence cases or elderly patients, en-bloc resection and reconstruction of the knee joint could be a good choice to reduce the risk of local recurrence and to achieve better quality of life [4].
Generally, we choose a customized rotating-hinge knee prosthesis to fill the bone defect left after en-bloc resection of the tibia. However, poor flexibility and stress concentration cause prosthesis fracture and loosening, which often lead to poor follow-up results [5–8]. Standard knee prosthesis, which can solve these problems, cannot fix large bone defects after the resection, so the joint stabilization remains a problem.
In recent years, clinicians have managed to integrate CT imaging and computer-aided design (CAD) into surgical planning and custom-made implants design. 3D printing technology has also been applied clinically in preoperative planning, and it has been shown that 3D-printed models can achieve accuracy in preoperative design and manufacturing internal fixation devices [9]. Moreover, studies on 3D-printed metallic implants in animal experiments have also been reported [10,11], but it has not been reported in design and production of tumor prostheses.
Recently, the China Food and Drug Administration (CFDA) approved the use of 3D-printed metallic implants clinically (registration number: 20153461311). In this paper, we explored the application of 3D printing technology in treating patients with giant cell tumors (GCT) of the proximal tibia through en-bloc resection and reconstruction of the knee joint. A tibia block was designed and produced using 3D printing technology. We expected this 3D-printed block, combined with a standard knee joint prosthesis, would fix the bone defect after en-bloc resection and maintain knee stability through providing attachments for collateral ligaments of the knee, achieving good results.
Material and Methods
Ethics approval and consent to participate
This study was conducted in accordance with the principles outlined in the Declaration of Helsinki and was approved by the Ethics Committee of the Second Hospital of Jilin University. Written informed consent to participate was obtained from all patients involved in the study. Patient data were kept anonymous to ensure confidentiality and privacy.
Patient characteristics
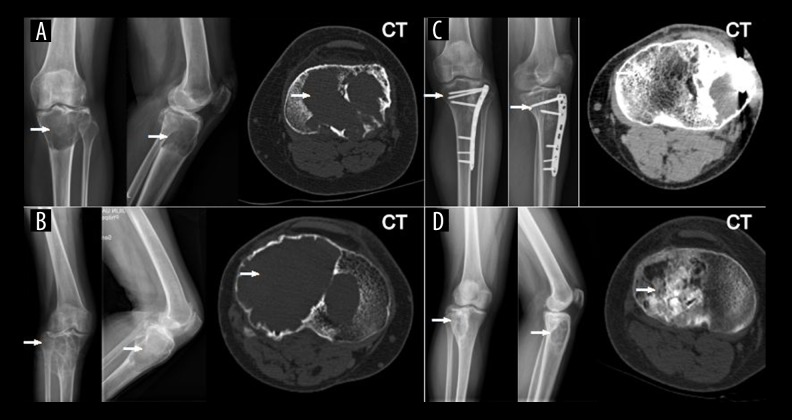
Between August 2015 and December 2015, 4 patients (1 male and 3 females, aged 35–68 years) with giant cell tumor of the proximal tibia underwent en-bloc resection of the tumor of the proximal tibia and reconstruction with prosthesis. All 4 cases were diagnosed pathologically with GCT. To reduce the possibility of local recurrence, the criteria for en-bloc resection were patients who had local recurrence and aged patients who could not tolerate another operation. One case was diagnosed by primary tumor. The other 3 underwent curettage in previous surgery and suffered a local recurrence. One of them (Case 3) underwent internal fixation after curettage (Figure 1). Antero-posterior and lateral radiographs, CT, and/or magnetic resonance imaging (MRI) were performed to locate the tumor. Chest X-ray was examined to exclude any pulmonary metastasis. Patient demographics are listed in Table 1.
Figure 1.
Antero-posterior and lateral radiographs showing GCT lesions in these 4 cases (A–D), and Case3 (B) had an internal fixation after curettage of the lesion (arrow shows the lesion).
Table 1.
Cases’ details.
| Case no. | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Age/sex | 40/F | 68/F | 53/M | 35/F |
| Site (L/R) | L | R | L | R |
| Primary/recurrence | R | P | R1 | R |
| First occurrence | 2006 | 2015 | 2014 | 2004 |
| Previous surgeries | CL in 2006 | – | CL in 2014 | CL in 2004 |
| Operation time (minute) | 210 | 130 | 170 | 180 |
| Length of incision (mm) | 300 | 300 | 4502 | 290 |
| Length of resection (cm) | 6.5 | 8.5 | 8.0 | 8.0 |
| Length of block (cm) | 5.4 | 7.7 | 7.1 | 7.1 |
| Hospital stays (days) | 19 | 19 | 15 | 15 |
| Range of motion | 0–90° | 0–70° | 0–110° | 0–90° |
| Bohler sign | N | N | N | N |
| Drawer test (anterior) | N | N | N | N |
| Drawer test (posterior) | N | N | N | N |
| MSTS score (pre-operation) | 13 | 11 | 14 | 14 |
| MSTS score (latest follow-up) | 13 | 19 | 19 | 24 |
| Duration of follow-up (monthes) | 8 | 6 | 6 | 8 |
CL is short for the Curettage of the Lesion. P for positive and N for negative. MSTS score (The Musculoskeletal Tumor Society) is 30 in total. 1. Operated earlier with curettage and internal fixation. 2 .The incision was extended distally in 150 mm in Case3 to remove the internal fixation.
Data acquisition and processing of images
Imaging data of the patient’s bilateral knee joints was obtained through 64-slice spiral CT scan (PHILIPS Corporation, Japan) (X-ray Tube Current 232 mA and KVP 120 kV, slice thickness 1 mm, reconstruction interval 1 mm).
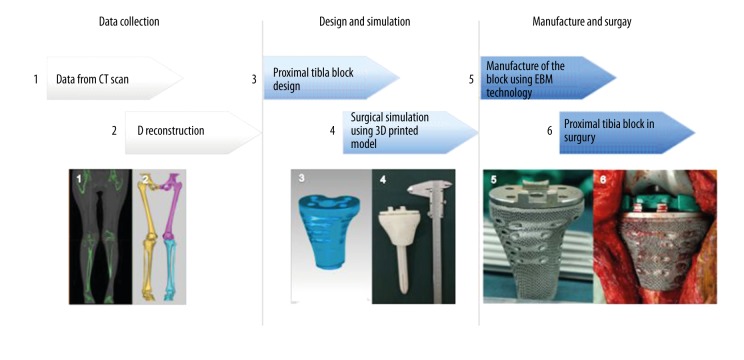
The DICOM file format obtained by each scan was input into the Materialise’s Mimics (version 14.0) software package for 3D reconstruction and editing to eliminate impurities. Results were then saved in the STL file format and imported into the IMAGEWARE software (Imageware V12.1, EDS Corporation, USA) to mimic surgery and design of custom-made proximal tibia block (Figure 2).
Figure 2.
A brief flow chart of this study (EBM: Electron Beam Melting).
Surgical procedure planning
Selection of tumor prosthesis
All patients underwent en-bloc resection of tumor of proximal tibia and reconstruction with prosthesis. Standard knee prosthesis combined with an extension stem were applied. With the help of the newly designed 3D-printed block during the procedure, the soft tissue balance was achieved.
Special techniques applied during the procedure
Special attention was given to preserve the collateral ligaments during the en-bloc of the lesion. The soft tissue of collateral ligaments was peeled off meticulously from proximal tibia like a sleevelet. After the resection, the ligaments were then sutured to the proximal tibia block, which provided a reticular porous-structured surface for ligaments to attach. The knee joint motion range was tested immediately after the operation. Postoperatively, systematic rehabilitation training plan was designed and carried out.
Design and manufacture of proximal tibia block
GCT lesion location and the range of resection
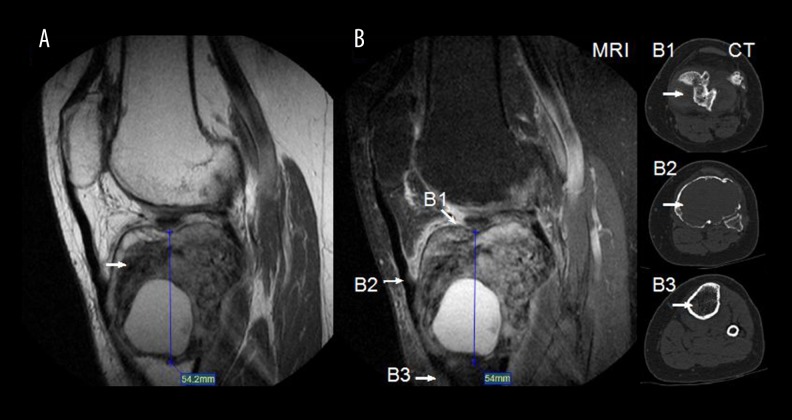
For all the patients, a CT scan was performed 1 week prior to surgery to obtain a 2-dimensional (2D) CT of the lesion. The tumor resection region was determined according to standard oncologic principles. The surgical excision, 2 cm longer than the tumor boundary, was made wide to reduce the risk of local recurrence [12]. In these 4 cases, the median resection length was 7.8 cm (range, 6.5–8.5 cm). In Case 1, an additional MRI was taken to inspect the bone cortex destruction. In Case 3, a 3D CT was taken to locate the internal plates of the previous surgery (Figure 3).
Figure 3.
GCT lesion located in the MRI and CT scan) The range of resection was recorded and then used as a parameter in design of the proximal tibia block. (A, B) Lesion and its boundary located in the MRI. (B1–B3) The lesion boundary located in CT.
Proximal tibia block design and surgical simulation through 3D-printed model
The proximal tibia block was designed through the mirror image of the 3D reconstruction (unaffected side) to ensure the same morphological characters. Then, the length of the block was designed through surgical simulation software according to resection region. The original anatomical model was then modified into a model with several geometric figures in details. Initially, in the first case, reticular porous structure was generated on all of its surface to connect soft tissue, but it was hard to suture through the limited space. Then, to maintain keen stability, horizontal cylinder holes were designed on the surface of the block to attach collateral ligaments according to previous studies [13].
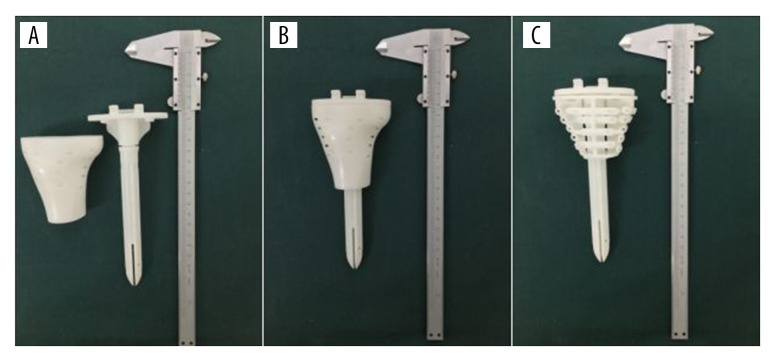
For all 4 cases, a cylinder hole was vertically built into the center of the block to let the extension stem of the tibia tray prosthesis precisely pass through into the medullary cavity (Figure 4).
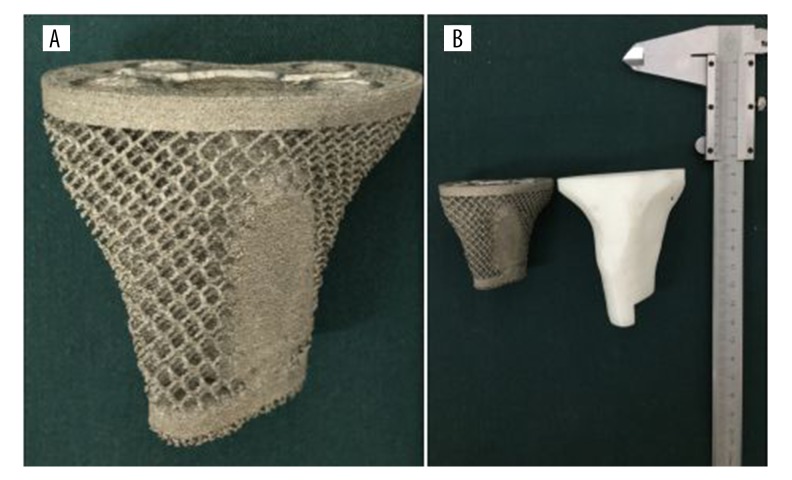
Figure 4.
Design of the block. (A) The modified proximal tibia block. (B) 3D-printed model for surgical simulation. (C) Difference between the original case (C1) and the modified one (C2).
After the design was completed, the model was saved as an STL file and then imported into a 3D printing machine. The designed block model, include tibia tray prosthesis with extension stem, was 3D-printed at 1: 1 scale. All these models were made of photosensitive resin. Preoperatively, surgical simulation based on the 3D-printed model was produced to check the accuracy of the model (Figure 5).
Figure 5.
Surgical simulation using 3D-printed model. (A, B) Models of the knee prosthesis and the block. (C) Internal structure of the block.
Manufacture of the block
The block combined with proximal tibia prosthesis fitted the tibia precisely during the preoperative surgical simulation through photosensitive resin models. The final product was fabricated by a commercial company (AK MEDICAL Ltd, China), which was certified by China Food and Drug Administration (CFDA). The 3D-printed product was made of titanium alloy (Ti6Al4V) through use of EBM technology [14]. Reticular porous structures were generated on the surface of the block during the process of rapid-prototyping. After post-processing, the block could be used (Figure 6).
Figure 6.
The final product made of titanium alloy. (A) The reticular porous structure on the surface. (B) Comparing with model made of photosensitive resin.
Surgery
All operations were performed under epidural anesthesia. The patient was placed on the operating table in a supine position. The conventional anterior medial incision for the knee was applied. En-bloc resection of the proximal tibia was strictly performed in accordance with the principles of tumor-free surgery. The length of osteotomy was determined based on preoperative design. Then, the prosthesis and the 3D-printed block were installed into the medulla of tibia with a bone cement technique. Special attention was given to preserve the patellar tendon and collateral ligaments during the en-bloc resection of the lesion. The soft tissue of collateral ligaments was peeled off meticulously from the proximal tibia like a sleevelet. Importantly, the ligaments were sutured to the proximal tibia block through the reticular porous structure. The motion range of knee joint was tested immediately after the reconstruction (Figures 7, 8). Tranexamic acid was used before the tourniquet was loosened to reduce transfusion rate and blood loss [15,16].
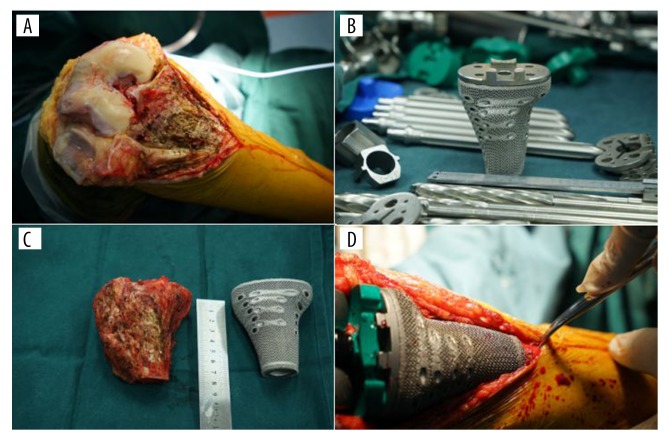
Figure 7.
(A–D) Intraoperatively, the proximal tibia prosthesis was highly consistent with the block.
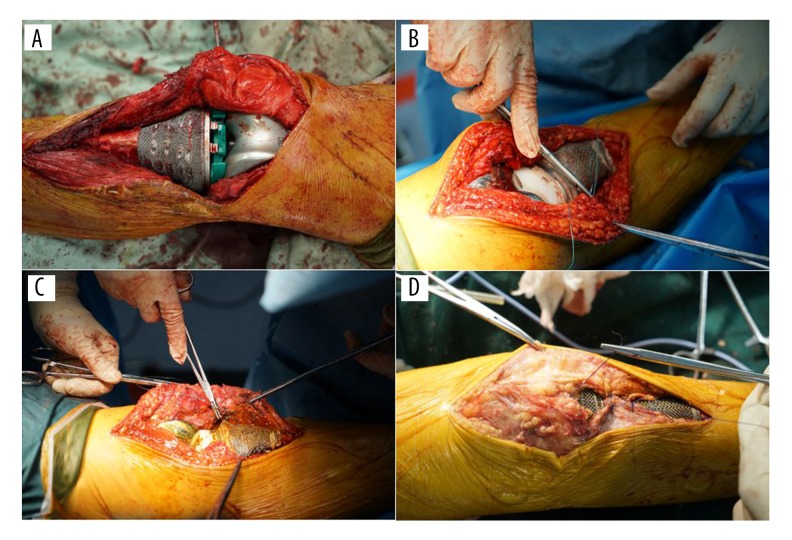
Figure 8.
(A–D) The ligaments were preserved and sutured to the proximal tibia space through reticular porous structure.
Follow-up
The patients were followed up at 1, 3, 6, and 12 months during the first year after the operation, every 6 months in the second year, and every year after the second year. Antero-posterior and lateral radiographs were taken to look for signs of prosthesis fracture and loosening. The Musculoskeletal Tumor Society (MSTS) score [17], image appearance, and videos of the motion of these patients were recorded.
Results
Surgery effect
The operation was completed successfully in all patients. The 3D-printed block fitted the bone defects precisely and connected ligaments and soft issues (Table 1). There were no signs of wound infection, skin necrosis, or other surgical complications (including peroneal nerve injury). The motion range and stability of the knee joint were examined and recorded in Table 1. Monitoring for prosthesis failure requires a long follow-up study.
Follow-up results
The patients were followed up for 5–8 months. The latest follow-up scores for these patients can be seen in Table 1. There were no signs of prosthesis fracture or loosening. No chronic infection or other prosthesis relevant complications were reported in these cases (Figure 9). Because most of the recurrences after treatment were reported within 2 years [12], a further follow-up study was needed.
Figure 9.
(A–F) A 40-year-old female (case 1) suffered a local recurrence in 2015. The MRI and CT scan showed that the lesion breached the bone cortex. Resection of tumor and reconstruction of the knee joint with prosthesis were applied. Antero-posterior and lateral radiographs taken postoperative, one month and 3 months after discharge shows no sign of prosthesis fracture and loosening. The flexion of the affected knee was 90 degrees at 6 months after surgery.
Discussion
En-bloc resection of tumors of the proximal tibia and reconstruction with customized rotating-hinged knee prosthesis has been demonstrated to provide acceptable function and a remarkably low recurrence risk in most cases [4,18]. However, poor flexibility and stress concentration cause prosthesis fracture and loosening, which lead to poor follow-up results [19]. It is desired that rotational and flexional stress affection can be reduced, while the stability is still ensured. Based on these principals, we turned to use of a standard knee prosthesis in this study, which can solve stress concentration and mechanical wear, and the soft tissue balance of the knee was ensured. With the help of the newly designed 3D-printed block based on the unaffected side of the proximal tibia, the bone defect after en-bloc resection was precisely filled. Ligament attachments of collateral ligaments were attached into this block, which can keep the soft tissue balance.
Various methods for surgical visualization have been implemented. 3D anatomical images reconstructed from CT or MRI have now become a commonly used tool for orthopedic surgery in the last 2 decades [20–22]. The advantage of observing the patient’s anatomy through 3D printing is obvious. In the present study, we introduced 3D printing technology into surgical visualization. Through use of a 3D-printed model made of photosensitive resin it is much easier and safer to design treatment plans. Intraoperatively, the personalized designed proximal tibia block makes it easier to apply innovate surgical techniques.
Benefit from the advantage of 3D printing technology, the block was modified to easily connect the soft tissue of collateral ligaments, which could help reconstruct the knee joint, and is useful in design and manufacture of custom-made orthopedic medical instruments. This new surgical technique could be more widely used because of 3D printing technology.
3D printing technology is a kind of additive manufacturing, in which no raw material is wasted, so the cost of 3D printing is lower than in tradition processes. The total cost was about 30% lower than the cost of traditional prosthesis. The time needed to produce a 3D-printed customized prosthesis was also shorter than that required for a traditional prosthesis. Taken together, these facts make this new technology attractive.
The material properties of 3D-printed Ti-alloy had been applied in several studies [23]. Liu et al. compared the mechanical characteristics of the EBM-printed Ti-6Al-4V orthopedic implants with the general implants of AO (Association for the Study of Internal Fixation) systems. In this study, it was shown that the stiffness, strength, and structure of EBM plate-bending were greater than the general implants clinically [14]. Facchini et al. worked on the microstructure and mechanical properties of Ti-alloy and found that The Ti-6Al-4V alloy produced by EBM had 99.4% of the theoretical density and a very fine microstructure, and, preserved tensile mechanical properties that fully satisfied the standard requirements [24].
In the operation, the interface between the tibial tray and 3D-printed Ti-alloy block was filled by bone cement to prevent any micromovement. This kind of technique has been safely applied in some prosthesis revision systems [25,26]. The interfaces between the tibial tray and 3D-printed Ti-alloy were filled by bone cement, reducing the chance of fatigue and corrosion.
In this study, patients with GCT were selected because it was benign with locally invasive neoplasm, and it had a high possibility of local recurrence. In addition, the possibility of metastasis of GCT was lower than with a malignant bone tumor, which could make the procedure relatively safe.
Postoperative fractures and implant loosening were taken into consideration during the design. In this study, we turned to use of cemented stems to acquire better stress distribution in the tibial bone [27]. The length of the stems was designed based on AAOS (American Academy of Orthopaedic Surgeons) principals [28]. A benefit of the new properties of our tibia block is that we were able to used standard knee prostheses, which has lower possibility of postoperative fractures and implant loosening than with the traditional modular rotating-hinge prosthesis [5]. By these means, we expected to avoid postoperative fractures and implant loosening. Moreover, there is no relevant complication reported (4 cases) by now.
This study introduced a new application of 3D printing technology in knee surgery. 3D printing technology is widely used in our center for preoperative planning and surgical visualization of complex trauma, correction of bony abnormalities, and custom-made internal fixation for fractures.
In terms of the 3D-printed block, its clinical application still has limitation. The time spent on manufacturing was longer than in traditional methods, but this could be solved by cooperating closely with the multidisciplinary team.
Conclusions
In this study, the personalized 3D-printed proximal tibia block was successfully applied in treating patients with GCT, acquiring functional results. 3D printing technology makes the operation precise and safe, which is beneficial for the patients. This new surgical technique could be much more widely used because of 3D printing technology.
Acknowledgements
Finally, we would like to thank Prof. Wang and Prof. Qin, who provided friendly encouragement in writing this paper and give valuable advice. Thanks also go to Dr. Liu and Dr. Qu, who gave great help in writing and revising this paper. Sincere thanks to Beijing AKEC Medical Company and Jilin XuFeng Company for their cooperation.
Abbreviations
- GCT
giant cell tumor
- 3D
three-dimensional
- 2D
two-dimensional
- CT
computed tomography
- MRI
magnetic resonance imaging
- EBM
Electron Beam Melting
- CFDA
China Food and Drug Administration
Footnotes
Competing interests
The authors declare that they have no competing interests.
Source of support: Departmental sources
References
- 1.McDonald DJ, Sim FH, Leod RA, Dahlin DC. Giant cell tumour of bone. J Bone Joint Surg. 1986;68A:235–42. [PubMed] [Google Scholar]
- 2.Sung HW, Kuo DP, Shu WP, et al. Giant-cell tumour of bone: analisys of two hundred and eight cases in chinese patients. J Bone Joint Surg. 57A:167–73. 192. [PubMed] [Google Scholar]
- 3.Dahlin DC, Cupps RE, Johnson EW., Jr Giant cell tumor: A study of 195 cases. Cancer. 1970;25:1061–70. doi: 10.1002/1097-0142(197005)25:5<1061::aid-cncr2820250509>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 4.Moon MS, Kim SS, Moon JL, et al. Treating giant cell tumours with curettage, electrocautery, burring, phenol irrigation, and cementation. J Orthop Surg. 2013;21(2):209–12. doi: 10.1177/230949901302100219. [DOI] [PubMed] [Google Scholar]
- 5.Barrack RL, Lyons TR, Ingraham RQ, et al. The use of a modular rotating hinge block in salvage revision total knee arthroplasty. J Arthroplasty. 2000;15(7):858–66. doi: 10.1054/arth.2000.9056. [DOI] [PubMed] [Google Scholar]
- 6.Campanacci M, Baldini N, Boriani S, et al. Giant cell tumor of bone. J Bone Joint Surg Am. 1987;69(1):106–14. [PubMed] [Google Scholar]
- 7.Zylberberg A, Bayley G, Gala L, et al. Primary total knee arthroplasty twenty years after distal femoral cement augmentation of a giant cell tumor. Case Rep Orthop. 2015;2015:283294. doi: 10.1155/2015/283294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grimer RJ, Carter SR, Tillman RM, et al. Endoprosthetic replacement of the proximal tibia. J Bone Joint Surg Br. 1999;81(3):488–94. doi: 10.1302/0301-620x.81b3.9234. [DOI] [PubMed] [Google Scholar]
- 9.Kim HN, Liu XN, Noh KC. Use of a real-size 3D-printed model as a preoperative and intraoperative tool for minimally invasive plating of comminuted midshaft clavicle fractures. J Orthop Surg Res. 2015;10:91. doi: 10.1186/s13018-015-0233-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melican MC, Zimmerman MC, Dhillon MS, et al. Three-dimensional printing and porous metallic surfaces: A new orthopedic application. J Biomed Mater Res. 2001l;55(2):194–202. doi: 10.1002/1097-4636(200105)55:2<194::aid-jbm1006>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 11.El-Hajje A, Kolos EC, Wang JK, et al. Physical and mechanical characterisation of 3D-printed porous titanium for biomedical applications. J Mater Sci Mater Med. 2014;25(11):2471–80. doi: 10.1007/s10856-014-5277-2. [DOI] [PubMed] [Google Scholar]
- 12.Saikia KC, Bhattacharyya TD, Bhuyan SK, et al. Local recurrences after curettage and cementing in long bone giant cell tumor. Indian J Orthop. 2011;45(2):168–73. doi: 10.4103/0019-5413.77138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhalmi S, Odin M, Assad M, et al. Hard, soft tissue and in vitro cell response to porous nickel-titanium: A biocompatibility evaluation. Biomed Mater Eng. 1999;9(3):151–62. [PubMed] [Google Scholar]
- 14.Liu P, Yang Y, Liu R, et al. A study on the mechanical characteristics of the EBM-printed Ti-6Al-4V LCP plates in vitro. J Orthop Surg Res. 2014;9:106. doi: 10.1186/s13018-014-0106-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shen PF, Hou WL, Chen JB, et al. Effectiveness and safety of tranexamic acid for total knee arthroplasty: A prospective randomized controlled trial. Med Sci Monit. 2015;21:576–81. doi: 10.12659/MSM.892768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu X, Li W, Xu P, et al. Safety and efficacy of tranexamic acid in total knee arthroplasty. Med Sci Monit. 2015;21:3095–103. doi: 10.12659/MSM.895801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong KC, Kumta SM, Antonio GE, et al. Image fusion for computer-assisted bone tumor surgery. Clin Orthop Relat Res. 2008;466(10):2533–41. doi: 10.1007/s11999-008-0374-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones RE, Skedros JG, Chan AJ, et al. Total knee arthroplasty using the S-ROM mobile-bearing hinge prosthesis. J Arthroplasty. 2001;16(3):279–87. doi: 10.1054/arth.2001.21498. [DOI] [PubMed] [Google Scholar]
- 19.Pala E, Henderson ER, Calabrò T, et al. Survival of current production tumor endoprostheses: Complications, functional results, and a comparative statistical analysis. J Surg Oncol. 2013;108(6):403–8. doi: 10.1002/jso.23414. [DOI] [PubMed] [Google Scholar]
- 20.Dobbe J, Strackee S, Schreurs A, et al. Computer-assisted planning and navigation for corrective distal radius osteotomy, based on pre- and intraoperative imaging. IEEE Trans Biomed Eng. 2010;58(1):182–90. doi: 10.1109/TBME.2010.2084576. [DOI] [PubMed] [Google Scholar]
- 21.Oka K, Moritomo H, Goto A, et al. Corrective osteotomy for malunited intra-articular fracture of the distal radius using a custom-made surgical guide based on three-dimensional computer simulation: Case report. J Hand Surg Am. 2008;33(6):835–40. doi: 10.1016/j.jhsa.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 22.Murase T, Oka K, Moritomo H, et al. Three-dimensional corrective osteotomy of malunited fractures of the upper extremity with use of a computer simulation system. J Bone Joint Surg Am. 2008;90(11):2375–89. doi: 10.2106/JBJS.G.01299. [DOI] [PubMed] [Google Scholar]
- 23.Lewandowski JJ, Seifi M. Metal additive manufacturing: A review of mechanical properties. Annu Rev Mater Res. 2016;46:14.1–14.36. [Google Scholar]
- 24.Facchini L, Magalini E, Robotti P, et al. Microstructure and mechanical properties of Ti-6Al-4V produced by electron beam melting of pre-alloyed powders. Rapid Prototyping Journal. 2009;15(3):171–78. [Google Scholar]
- 25.Abolghasemian M, Tangsataporn S, Sternheim A, et al. Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss. Bone Joint J. 2013;95(2):166–72. doi: 10.1302/0301-620X.95B2.30608. [DOI] [PubMed] [Google Scholar]
- 26.Levine DL, Dharia MA, Siggelkow E, et al. Repair of periprosthetic pelvis defects with porous metal implants: A finite element study. J Biomech Eng. 2010;132(2):021006. doi: 10.1115/1.4000853. [DOI] [PubMed] [Google Scholar]
- 27.El-Zayat BF, Heyse TJ, Fanciullacci N, et al. Fixation techniques and stem dimensions in hinged total knee arthroplasty: A finite element study. Arch Orthop Trauma Surg. 2016 doi: 10.1007/s00402-016-2571-0. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Glassman AH, Lachiewicz PF, Tanzer M. Orthopaedic knowledge update: Hip and knee reconstruction 4. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2011. p. 172. [Google Scholar]