Abstract
Neurotransplantation as a treatment for Parkinson disease reached the stage of human trials over 15 years ago, but the field, which is still in its infancy, has encountered a number of roadblocks since then, both political and scientific. With hope that stem cells may be used as a new source of dopaminergic neurons to replace the degenerating nerve cells in Parkinson disease looming, it is critical that we learn from the past as we work toward achieving new milestones aimed at making this new therapeutic strategy a reality. One of those milestones, which is an important translational step in the development of stem cell technology and the subject of a report in this issue of the JCI, involves transplanting new dopaminergic cell lines to a primate model of Parkinson disease.
The possibility of repairing the damaged human brain has been a dream of physicians and scientists for decades. Over time it has become obvious that Parkinson disease is a natural first when it comes to tackling this ambitious feat, primarily because the majority of the signs and symptoms appear to result from the progressive loss of cells in a small area known as the substantia nigra, which sits atop the brain stem. These cells make dopamine, which is delivered to a part of the basal ganglia known as the striatum; when nigral neurons die and striatal dopamine diminishes, the signs and symptoms of Parkinson disease become manifest. Thus, replenishing missing neurons in a limited area of the brain should in theory reverse parkinsonism, making this an attractive approach. But the challenge of actually replacing injured and/or lost neurons in the adult human nervous system has proven to be a daunting task with far more bumps in the road, both political and scientific, than anyone would have anticipated.
Neurotransplantation: trials and tribulations
While stem cell therapy is very much in the forefront when approaches to brain repair and cell replacement therapy are being considered, there is already a substantial body of work in the Parkinson disease field involving neurotransplantation, including the use of both adult adrenomedullary tissue and human fetal mesencephalic tissue (which is rich in dopaminergic [DA] neurons); the lessons learned should not be ignored. While adrenomedullary transplantation proved to be something of a medical fiasco, with little efficacy and unacceptable morbidity and mortality, a number of the early open label trials with human fetal mesencephalic tissue appeared to be very promising. However, due to a ban on the use of federal funds for research utilizing human fetal tissue imposed by then-President Ronald Reagan, little work was done in this area until President Bill Clinton lifted this moratorium on his second day in office. Not long thereafter, 2 large controlled clinical trials aimed at using fetal human mesencephalic tissue transplanted to the striatum to treat Parkinson disease were launched with federal funding. However, to the surprise of many, both trials failed to show a significant clinical benefit based on their primary endpoint variables (1, 2) in spite of substantial evidence of graft survival based on both autopsy (3) and imaging studies. Unfortunately, a substantial subset of patients also developed persistent excessive movements known as dyskinesias (2). Dyskinesias are typically a consequence of long-term L-dopa therapy, but in the patients receiving transplants, these movements persisted even after L-dopa was discontinued, raising serious safety concerns.
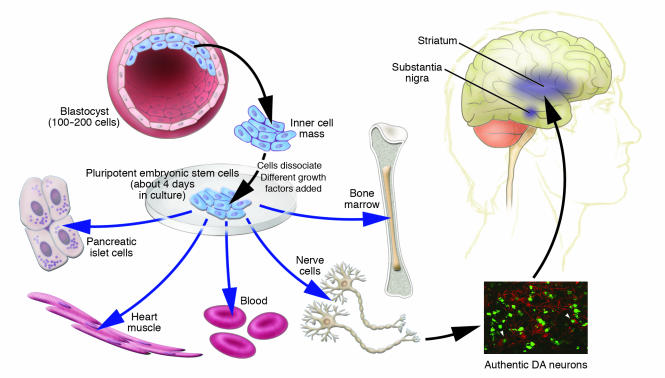
Why didn’t this approach work? Theories range from poor graft survival to the possibility that low-grade inflammation interfered with graft function. But the reality is that we still don’t know. Why is all this relevant to the use of stems cell to treat Parkinson disease? First, strategies used in fetal cell transplantation are essentially the same as those which will be applied with DA stem cells, but we are now in a quandary regarding this entire approach. A second hurdle relates to the vast technical barriers that are being encountered in the process of learning how to use stem cells to treat any human disease. With regard to Parkinson disease, the first task has been to create authentic DA cell lines that can be used to replace the missing neurons in the nigrostriatal system, and the second to get those cells to persist in vivo without forming tumors. While this has been an intensive area of research, there are only a limited number of successes so far, and these have been achieved primarily in rodents (4–7). For these reasons, the current report by Takagi and colleagues in this issue of the JCI is of great interest (8). These investigators have prepared what appear to be authentic DA neurons and used those cells to reverse parkinsonism in a primate model of the disease (Figure 1). This is important because treatment of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine–induced (MPTP-induced) parkinsonism in primates (the model used here) has proven highly predictive of new symptomatic approaches in the treatment of Parkinson disease. Yet we still have a long way to go.
Figure 1.
Pluripotent embryonic stem cells are obtained from the inner cell mass of the blastocyst stage of development. These cells have the potential to develop into any tissue type. A variety of different treatments or “cocktails” have been devised to coax these cells into developing into a neuronal lineage and then into authentic DA neurons. Green, BrdU; red, tyrosine hydroxylase–positive (TH-positive) DA neurons (8). These are then used for cell replacement therapy by transplantation into the area of the brain where DA nigrostriatal neurons have degenerated. To date, almost all fetal cell transplants have involved putting these cells into the striatum (which lies deep in the brain, below the shaded area in the figure) as have most experimental studies. However, it is still not clear that this is the best target area; it is also possible that it will be necessary to transplant the cells to multiple sites, including the substantia nigra. The major challenge at the current time appears to be getting transplanted DA embryonic stem cells to maintain their DA phenotype in large numbers and over a prolonged period of time.
Challenges for the future
While the observations in the current study (8) are encouraging, the number of surviving DA neurons was very low, with only 1% to 3% of the cells surviving — well below the estimated number of DA neurons that survived after fetal cell transplants, where figures hovered around 10%. The explanation may lie in species differences and/or simple volumetric issues; however, based on what we have learned to date in human fetal cell trials, it may be necessary for far more DA neurons to survive, and, of course, the survival must be long lasting, an aspect of therapy that was not assessed in the current study. It is also important to note that, as the authors point out, dyskinesias were not observed in their monkeys. However, the authors do not present evidence that this species develops L-dopa–induced dyskinesias, and much longer-term follow-up may be needed since dyskinesias were typically not seen during the first year in human studies. It is good news that tumors were not observed, but this could also be related to the small number of surviving cells.
Keeping in mind these caveats, clearly the study reported here will advance research aimed at validating the use of stem cells to treat neurodegenerative disease. And this is most welcome, particularly for investigators working on strategies for cell replacement the United States, who must be feeling something of a déjà vu in face of yet another presidential moratorium, this time limiting the number of human stem cell lines that can be used for research and treatment. Ironically, this frustration recently led California voters to approve a $3 billion initiative to fund stem cell research, which some have predicted will lead to a “gold rush” on stem cell research (9). Regardless of whether or not this proves to be the case, it can be hoped that this new initiative will serve as a beacon of hope for scientists and patients alike as we press ahead in this challenging area of science that appears to promise so much for the treatment of human diseases.
Footnotes
See the related article beginning on page 102.
Nonstandard abbreviations used: DA, dopaminergic.
Conflict of interest: The author has declared that no conflict of interest exists.
References
- 1.Freed CR, et al. Transplantation of embryonic dopamine neurons for severe Parkinson’s disease. N. Engl. J. Med. 2001;344:710–719. doi: 10.1056/NEJM200103083441002. [DOI] [PubMed] [Google Scholar]
- 2.Olanow CW, et al. A double-blind controlled trial of bilateral fetal nigral transplantation in Parkinson’s disease. Ann. Neurol. 2003;54:403–414. doi: 10.1002/ana.10720. [DOI] [PubMed] [Google Scholar]
- 3.Kordower JH, Sortwell CE. Neuro-pathology of fetal nigra transplants for Parkinson’s disease. Prog. Brain Res. 2000;127:333–344. doi: 10.1016/s0079-6123(00)27016-7. [DOI] [PubMed] [Google Scholar]
- 4.Studer L, Tabar V, McKay RD. Transplantation of expanded mesencephalic precursors leads to recovery in parkinsonian rats. Nat. Neurosci. 1998;1:290–295. doi: 10.1038/1105. [DOI] [PubMed] [Google Scholar]
- 5.Isacson O, et al. Cell implantation therapies for Parkinson’s disease using neural stem, transgenic or xenogeneic donor cells. Parkinsonism Relat. Disord. 2001;7:205–212. doi: 10.1016/s1353-8020(00)00059-6. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez-Pernaute R, Studer L, Bankiewicz KS, Major EO, McKay RD. In vitro generation and transplantation of precursor-derived human dopamine neurons. J. Neurosci. Res. 2001;65:284–288. doi: 10.1002/jnr.1152. [DOI] [PubMed] [Google Scholar]
- 7.Kim JH, et al. Dopamine neurons derived from embryonic stem cells function in an animal model of Parkinson’s disease. Nature. 2002;418:50–56. doi: 10.1038/nature00900. [DOI] [PubMed] [Google Scholar]
- 8.Takagi Y, et al. Dopaminergic neurons generated from monkey embryonic stem cells function in a Parkinson primate model. J. Clin. Invest. 2005;115:102–109. doi:10.1172/JCI200521137. doi: 10.1172/JCI21137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holden C. U.S. science policy. California’s Proposition 71 launches stem cell gold rush. Science. 2004;306:1111. doi: 10.1126/science.306.5699.1111. [DOI] [PubMed] [Google Scholar]