Abstract
Objectives
Childhood obesity prevention and treatment depends, in part, on parents acting as agents of change for their children. Our objective was to measure the associations between parenting self-efficacy, parent depressive symptoms, and preschool child behaviors that support healthy growth.
Methods
We performed a cross-sectional analysis of baseline data from a randomized controlled trial. Parenting self-efficacy was measured using a 5-item version of the Parenting Sense of Competence (PSOC-5) scale (α=0.8). Parent depressive symptoms were measured using the Center for Epidemiological Studies-Depression (CESD) scale. Child outcomes included diet (24 hour diet recall), physical activity (accelerometry), sleep (parent-report), and media use during meals (parent-report). We performed separate multiple linear regressions for each outcome controlling for other covariates.
Results
The sample consisted of 601 parent-child pairs. Median child age was 4.3 (IQR 3.6–5.1) years; median child Body Mass Index (BMI) percentile was 79.1%(IQR 66.8–88.5%); 90% of children were Hispanic/Latino, and 6% of children were non-Hispanic Black. Median parent age was 31.5 (IQR 27.6–36.0) years; 22% of parents met criteria for depression. Parenting self-efficacy (median PSOC-5 25; IQR 24–28) was negatively correlated with depressive symptoms (ρ=−0.16; p<0.001). In adjusted models, higher parenting self-efficacy was associated with duration of child’s sleep and fewer meals eaten in front of a TV (p<0.001). There was a significant interaction of parenting self-efficacy and parental depressive symptoms on child sleep duration (p<0.001). Parenting self-efficacy and depressive symptoms were not significantly associated with child physical activity or child diet.
Conclusions
In this minority population, higher parenting self-efficacy was associated with longer child sleep and fewer meals in front the TV, but parent depressive symptoms mitigated that protective effect for child sleep duration.
Keywords: Pediatric Obesity, Self-Efficacy, Parenting, Depression
Introduction
The burden of obesity is particularly high among underserved minorities in the United States. Obesity prevalence is 47.8% among non-Hispanic black adults, 42.0% among Hispanic adults, 20.2% among non-Hispanic black children, and 22.4% among Hispanic children.(1) Thus, developing sustainable and measureable approaches to childhood obesity treatment and prevention, particularly for underserved populations, is of critical public health importance.
Childhood obesity is a complex chronic disease that has a wide range of causative factors. The determinants of childhood obesity shape childhood growth through a child’s energy balance, interacting in a cumulative way throughout a person’s life across a range of both micro-level (e.g., genetics, satiety, etc.) and macro-level (e.g., built environment, cultural norms, etc.) factors.(2) A child’s diet and physical activity directly influence energy balance while factors like adequate sleep, and limited media exposure influence childhood obesity indirectly, particularly in low-income households.(3, 4) Because these four components of child behavior have been previously identified as central contributors to childhood obesity, they were the primary outcomes for the present study.
The extant research provides clear evidence for the importance of the family environment in determining childhood obesity. (5–7) For example, when an obese parent and child are targeted concurrently in behavioral treatment trials, parental BMI change is a significant predictor of child BMI change, with lasting positive effects in both child and adult weight.(8, 9) Yet, except for a handful of factors (e.g. high parental stress, food insecurity, high parental BMI, maternal depressive symptoms, etc.), the specific ways in which parents influence the behaviors that contribute to childhood obesity have yet to be fully explored.(10–12) Recognizing parents as agents of changes means that parents are both role models and facilitators of effective behavior change for their children. Therefore, understanding how parenting is associated with childhood behaviors provides foundational information for developing obesity interventions.
One possible way that parenting can influence child obesity risk is through parenting self-efficacy. Self-efficacy is defined as “the conviction that one can successfully execute the behavior required to produce the outcomes.”(13) As a central-tenet of social cognitive theory (14) self-efficacy is an important and mutable mediator of behavior change. In the context of the family environment, parenting self-efficacy is a parent’s confidence to make good decisions for their children. A parent’s self-efficacy to carry out the parental role is a central construct for childhood obesity treatment and prevention, as improving a parent’s ability to act as an agent of change, despite perceived barriers, is an important component of successful behavior change.(15) Some initial work has been done to understand a parent’s self-efficacy in the context of specific behaviors that support healthy childhood growth.(16, 17) However, the ways in which the more general concept of parenting self-efficacy (i.e., a parent’s self-efficacy to carry out the parental role) relates to behaviors that support healthy childhood weight gain remains unstudied. Furthermore, data are lacking to understand how affective and cognitive aspects of parenting (i.e., depressive symptoms and self-efficacy) relate to each other in the setting of these healthy childhood behaviors, particularly in traditionally underserved communities.
Depression is a mood disorder that has been associated with worse parent and child health.(6, 18–20) Given the high prevalence of depression in under-served communities,(21, 22) the association between depressive symptoms and other mental and physical illness,(23) and its contribution to childhood obesity,(24) understanding how depressive symptoms is related to a parent’s self-efficacy is important for understanding the multi-factorial contributors to childhood obesity.(25)
The purpose of this study was to investigate the associations between general parenting self-efficacy with behaviors that support healthy childhood weight gain, including diet, physical activity, sleep, and media exposure in a traditionally under-represented racial and ethnic minority population. Given the additional challenges faced by traditionally underserved communities it is important to examine how parenting characteristics are related to important health behaviors that contribute to childhood obesity in these communities. We hypothesized that a parent’s self-efficacy to carry out the parental role would be positively associated with child diet, physical activity, and sleep time, and negatively associated with the amount of time the child is exposed to TV during meals. We also hypothesized that parent depressive symptoms would be negatively associated with child diet, physical activity and sleep time, and positively associated with the amount of time the child is exposed to TV during meals. Finally, we sought to understand the association between parenting self-efficacy and parent depressive symptoms, and whether a potential interaction between parenting self-efficacy and depressive symptoms would affect the association between parenting self-efficacy and the above behaviors affecting children’s health.
Methods
We performed a cross-sectional analysis of baseline data collected from parent-child pairs enrolled in the Growing Right Onto Wellness (GROW) Trial (clinicaltrials.gov identifier NCT01316653). GROW is a 3-year family-centered behavioral intervention to prevent childhood obesity that was delivered in local community centers. The full methods of GROW have been previously published. (26)
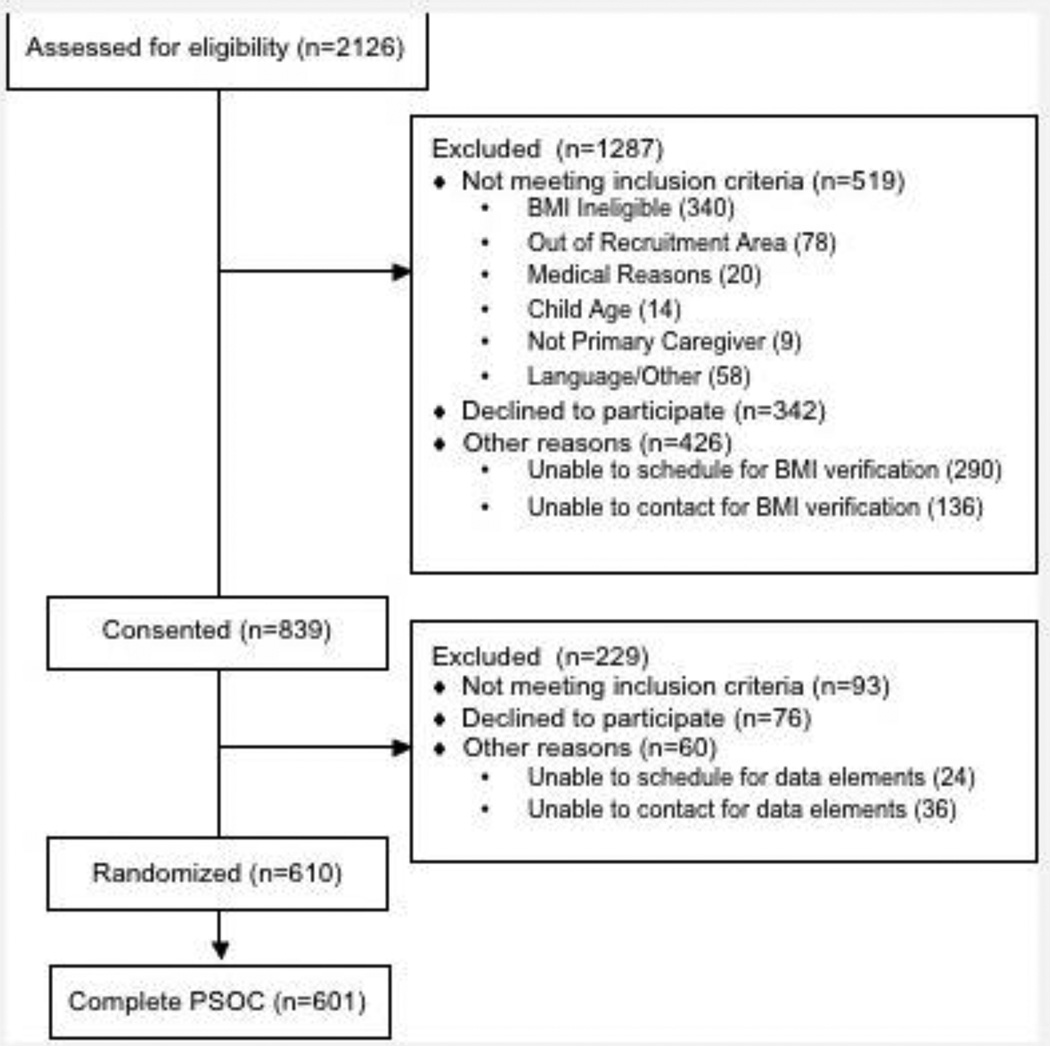
GROW enrolled 610 parent-child pairs from under-represented Latino and African American communities in Nashville, TN from January 2013 to June 2014 (Figure 1). Eligibility criteria for parent-child pairs were: 1) 3–5 year old child; 2) child’s Body Mass Index (BMI) >50th percentile and <95th percentile on standardized CDC growth curves; 3) parent self-identified preferred language of English or Spanish; 4) parent age ≥ 18 years; 5) consistent phone access; 6) parent commitment to participate in the duration of the three year study; 7) parent and child must be able to participate in moderate physical activity; 8) parent and child completion of baseline data collection; and 9) family must reside or frequently pass through one of two geographic regions in Nashville that is contiguous with a community center designated for the intervention.
Figure 1.
Consort Diagram for Growing Right Onto Wellness (GROW) Trial. PSOC-5=Parenting Sense of Competence Scale, 5 item version.
Baseline demographics and other self-reported measures were collected by guided verbal administration of a survey at baseline data collection. The survey was administered in a guided fashion because of the low literacy of the population. Bilingual research assistants administered the surveys in the parent’s language of choice (English or Spanish). All survey items were translated and back-translated by native Spanish speakers. Certified data collectors prospectively measured baseline height and weight for both parents and children. All Latino participants elected to have the survey administered in Spanish.
Parenting self-efficacy was the main independent variable and was collected by self-report of a 5-item version of the Parenting Sense of Competence Scale (PSOC-5). The Parenting Sense of Competence Scale is a 17-item instrument designed to measure personal competence in the parenting role as a function of both parenting satisfaction (i.e., valuing/comfort) and parenting self-efficacy (i.e., skills/knowledge).(27, 28) The scale consistently demonstrates high internal consistency and temporal stability.(29–32) We included five items from the parenting self-efficacy sub-scale based on previous factor loading (Table 1).(29) Each item is scored on a 6-point Likert scale from strongly disagree to strongly agree, and the items are summed to create a total score with higher values representing higher parenting self-efficacy. Parent-child pairs were excluded from the analyses (n=9) if the parent did not complete the parenting sense of competence measure for an analytic sample size of 601.
Table 1.
| Item | Mean (SD) Response; N=601 |
|---|---|
| 1. I would make a fine model for a new parent to follow in order to learn what she/he would need to know in order to be a good parent. |
4.9 (1.0) |
| 2. I meet my own personal expectations for expertise in caring for my children. |
5.1 (0.8) |
| 3. If anyone can find the answer to what is troubling my children, I am the one. |
5.3 (0.7) |
| 4. Considering how long I’ve been a parent, I feel thoroughly familiar with this role. |
5.1 (0.9) |
| 5. I honestly believe I have all the skills necessary to be a good parent to my children. |
5.1 (0.9) |
Scored on a 6 point Likert scale: 1-Strongly Disagree to 6-Strongly Agree
Parent depressive symptoms was measured by the Center for Epidemiological Studies-Depression (CESD) scale. (33) The CESD is a well-validated scale consisting of 20 items that assess how often in the last week a person experienced symptoms associated with depression. Each item is scored on a 4-point Likert scale (0–3), and the responses are summed to create the final score (possible range 0–60) with higher scores representing more depressive symptoms. Scores of 16 or higher are indicative of possible clinical depression.(33)
There were four main outcomes reported in this analysis: 1) Child physical activity as measured by accelerometry; 2) Child diet as measured by three 24-hour diet recalls; 3) Child sleep as measured by parent report; and 4) Child meal-time media exposure as measured by parent report.
Accelerometry data were collected using the GT3X+ monitor (manufactured by ActiLife). The child and parent each wore the monitor on the right hip for seven complete days, including sleeping and during water activity. Accelerometry data are reported as the average number of minutes spent in moderate or vigorous physical activity (MVPA) for both weekend and weekday, from 7:00 am to 8:59 pm, using previously defined cut-points.(34)
Dietary intake was measured using 24-hour recall conducted on two weekdays and one weekend day using NDS-R software. Dietary recalls were collected over the telephone in English or Spanish. To avoid collecting days with similar foods, recalls were not conducted on consecutive days. In addition, in order to capture variability of food supplies in the home, the third recall was collected more than one week after the first recall. The adult responsible for child feeding (e.g., parents, daycare providers) reported the child’s intake on a food record form. Full quality assurance checks were conducted on at least 10% of the dietary recalls according to NDS-R standard protocols. The data from diet recalls were then coded using the 2010 Healthy Eating Index (HEI).(35) The HEI is a validated measure of diet quality that references nutritional intake against the 2010 USDA dietary recommendations. The HEI is made up of 12 components and is scored on a scale from 0 to 100, with 100 representing total adherence to USDA recommendations.
Child sleep and meal-time media exposure were measured by parent report. Child sleep was calculated as a continuous variable by subtracting a parent’s response to “What is the child’s usual wake time?” from “What is the child’s usual bedtime?” Meal-time media exposure (scored from 0 to 7 days) was measured by asking, “In the past 7 days, how many days did your child eat in front of a television?” We also asked parents about the total amount of time their child watched television, which we report as the average child daily TV use in hours. The study team developed the sleep and media items for the purposes of the larger study.
Statistical Analysis
Descriptive statistics (median and interquartile range for continuous variables; percentages for categorical variables) were used to summarize baseline characteristics. When creating scale scores for the CESD, the individual’s own median value on scale items was imputed for missing items, but only when those missing items comprised <10% of the scale (note that we did not do this type of substitution for the PSOC-5 as it had only five items; any missing value would have comprised > 10% of the scale). For all variables, group means were substituted for missing continuous variables and the most frequent category was substituted for missing categorical variables. As the amount of missing data was minimal (1.5% or less for each variable), this type of simple substitution is acceptable.(36)
Cronbach’s alpha was computed to estimate the internal consistency of the PSOC-5 in this sample. Because the distribution of PSOC-5 and CESD scores were both non-normal, Spearman correlations (ρ) were calculated to estimate the unadjusted, bi-variate relationships between these two variables as well as the relationships between these variables and the four behavioral outcomes.
We examined three hierarchical multiple regression models for each behavioral outcome: Model 1 examined PSOC-5 as a main effect without parent depressive symptoms (CESD scores) included. Model 2 added CESD scores along with the PSOC-5, and Model 3 contained the two main effects plus the interaction of CESD and PSOC-5. CESD and PSOC-5 scores were mean-centered before being multiplied to construct the interaction terms for Model 3. Based on a priori considerations, all of these models controlled for the following set of covariates: parent age, child age, child gender, parent education, parent BMI, Supplemental Nutrition Assistance Program (SNAP) participation, and child race/ethnicity (coded into two dichotomous dummy variables: non-Hispanic, Black vs. Hispanic; and other race/ethnicity vs. Hispanic). Parent gender was not included as a covariate because 98% of index parents were women. To address the potential role of acculturation, we conducted a secondary analysis of the sub-set of Latino participants including acculturation as a covariate in the above models. In this study acculturation was measured using the Brief Acculturation Scale for Hispanics (BASH) (range 4–20).(37) To address whether the potential association between PSOC-5 and meal-time media was meal-specific or due to TV time more generally we conducted another secondary analysis evaluating the relationship between PSOC-5 and average daily TV time using the same models as above.
Standardized β-coefficients are presented to facilitate interpretation of effect size across multiple outcome variables. To reduce its negative skewness (skewness =−0.84, SE skewness = 0.10), parenting sense of competence was reflected and a square root transformation was performed. To reduce the positive skewness of maternal depressive symptoms, (skewness = 1.41, SE skewness = 0.10), a square root transformation was performed. We ran analyses with these variables transformed and without transformation. Because the pattern of results was identical between the two sets of models, for ease of interpretation we present analyses with untransformed variables, allowing us to interpret effects in their original scale. Data were analyzed using SPSS version 22. For all analyses, a 2-tailed p-value <0.05 was considered statistically significant
Results
Participant Characteristics
Full baseline characteristics of the population are listed in Table 2. Among the 601 caregivers with complete PSOC-5 data, 96% were mothers, 2% were fathers, and the remaining 2% were a mix of other extended family members including aunts, sisters, and grandparents. Most families self-identified as Latino (90.2%); the remaining families self-identified as African American, non-Hispanic (6.5%) or Other, non-Hispanic (3.3%). Most parents (69%) had at least some high school education, although 145 (24%) had less than a 6th grade education. The majority (75%) of families received governmental support for purchasing food (i.e., food stamps) through the Supplemental Nutritional Assistance Program.
Table 2.
Baseline characteristics of the population
| Parent Characteristics | Median (Inter-quartile range) or Percentage |
Correlation with PSOC-5 | |
|---|---|---|---|
| Age (years) | 31.45 (27.65–35.96) | −.01 | |
| Gender (female) | 97.8% | .01 | |
| Highest Education | |||
| Less than High School | 31.3% | ||
| Some High School | 30.1% | ||
| High School Graduate or Higher | 38.6% | ||
| Body Mass Index (kg/m2) | 28.75 (25.62–32.58) | .01 | |
| Household SNAP participation | |||
| Yes | 75.5% | ||
| No | 24.5% | ||
| Child Characteristics | |||
| Age (years) | 4.32 (3.60–5.11) | .09* | |
| Gender (female) | 51.4% | .02 | |
| Body Mass Index Percentile (%)1 | 79.10 (66.80–88.50) | .03 | |
| Race/Ethnicity | |||
| Hispanic/Latino | 90.2% | ||
| African American | 6.5% | ||
| Other | 3.3% | . | |
| Child Outcomes of Interest | |||
| Diet (24 hour diet recall; HEI) | 65.46 (56.55−73.16) | .06 | |
| Physical Activity (Accelerometry, minutes of MPVA) |
98.00 (74.61−118.96) | −.02 | |
| Sleep (mins) | 630 (600 – 690) | .17** | |
| Meal-time Media Exposure: (Meals/week eaten in front of TV) |
2 (0–3) | −.17** | |
Spearman’s ρ shown for correlations between Parenting Sense of Competence Scale (PSOC-5) and each variable.
Study inclusion criteria were limited to Body Mass Index percentile >50th and <95th.
p < 0.05;
p < 0.01
SNAP=Supplemental Nutrition Assistance Program. HEI=Healthy Eating Index. MVPA=Moderate or vigorous physical activity
The median age of the index child was 4.3 years (IQR 3.6–5.1). Because of the inclusion criteria of the parent study (obesity prevention), only two children met criteria for obesity based on standardized CDC growth curves. The majority of children (65%) in this sample were in the normal weight category (<85th percentile), while the remaining 34% were overweight (BMI between the 85th and 95th percentile).
The median PSOC-5 score was 25 (IQR 24,28; Range 16–30). No established cut points exist for the shortened version of the PSOC-5 used in this study, but the majority (68%) of parents responded “agree” or “strongly agree” to each of the 5 questions (see Table 1 for PSOC-5 item wording and mean scores). The internal consistency (Cronbach’s alpha) of the PSOC-5 was 0.80. The median CESD score was 7 (IQR 3, 14; Range 0–51). Twenty-two percent of parents met criteria for depression using well-established cut-points on the CESD.(33)
Bi-variate Relationships between Parenting Self-Efficacy and Childhood Healthy Behaviors
More than 25% of children participated in an average of 75–98 minutes of MVPA per day, while over half of the sample had >98 minutes of MVPA per day. Only 10% of children had <58 minutes of MVPA per day. The correlation between MVPA/day and parenting self-efficacy was not statistically significant (ρ=−0.02; p=0.6).
The median score on the healthy eating index was 65 (range 0–100), indicating that most children are not meeting daily dietary recommendations. The correlation between the healthy eating index and parenting self-efficacy was not statistically significant (ρ=0.06; p=0.13).
The median parent-reported sleep duration for children in this sample was 10.5 hours. Higher parenting self-efficacy was associated with longer child sleep (ρ=0.17; p < 0.001).
The median number of days that a child ate in front of the TV per week was 2 (IQR 0–3), with 235 children (39%) never eating in front of the TV. Thirteen percent of children ate in front of the TV every day. There was a significant negative correlation between higher parenting self-efficacy and eating fewer meals in front of the TV (ρ=−0.17; p<0.001).
Bi-variate Relationships Between Parent Depressive Symptoms and Childhood Healthy Behaviors
The correlations between parent CESD scores and the child HEI as well as the child MVPA were negative, but not significant (ρ = −0.07; p = 0.07, for HEI; ρ = −0.02; p = 0.7 for MVPA). However, parental depressive symptoms were significantly, negatively related to duration of child’s sleep (ρ = −0.08; p = 0.05) and significantly, positively related to the number of days per week the child was exposed to TV during meals (ρ =0.09; p = 0.03).
Bi-variate Relationship Between Parenting Self-Efficacy and Depressive Symptoms
There was a significant negative correlation between higher parenting self-efficacy and lower parent depressive symptoms (ρ =−0.16, p<0.001).
Multivariable Results with Parenting Self-Efficacy, Depressive Symptoms, and their Interaction on Child Health Behaviors
Table 3 presents the results of the four sets of multivariable regression analyses adjusting for all of the covariates. For child diet and child physical activity, neither the PSOC-5 nor the CESD main effects were significant on any of the steps of the regression model, nor was the interaction of those variables significant on step 3. For meal-time media exposure, the PSOC-5 effect was significant on all three steps, but the CESD and interaction effects were not significant on either step 2 or step 3.
Table 3.
Parenting self-efficacy, depression, and healthy childhood behaviors.
| Child Diet (24 hour diet recall) |
Child Physical Activity (accelerometry) |
Child Sleep (Total Time) | Meal-time Media Exposure: Child Meals/Week Eaten in Front of TV |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | Step 1 | Step 2 | Step 3 | Step 1 | Step 2 | Step 3 | Step 1 | Step 2 | Step 3 | |
| PSOC-5 | .07 | .06 | .06 | −.01 | −.01 | −.01 | .23** | .22** | .22** | −.15** | −.14** | −.14** |
| Depressio N |
−.06 | −.05 | −.04 | −.02 | −.05 | −.08 | .07 | .07 | ||||
| PSOC-5 x depression |
.04 | .08 | −.13** | .02 | ||||||||
Standardized beta weights from regression models are presented.
All models are adjusted for parent age, child age, child gender, parent education, parent Body Mass Index, Supplemental Nutrition Assistance Program (SNAP) participation, and child race/ethnicity
p < 0.05;
p < 0.01
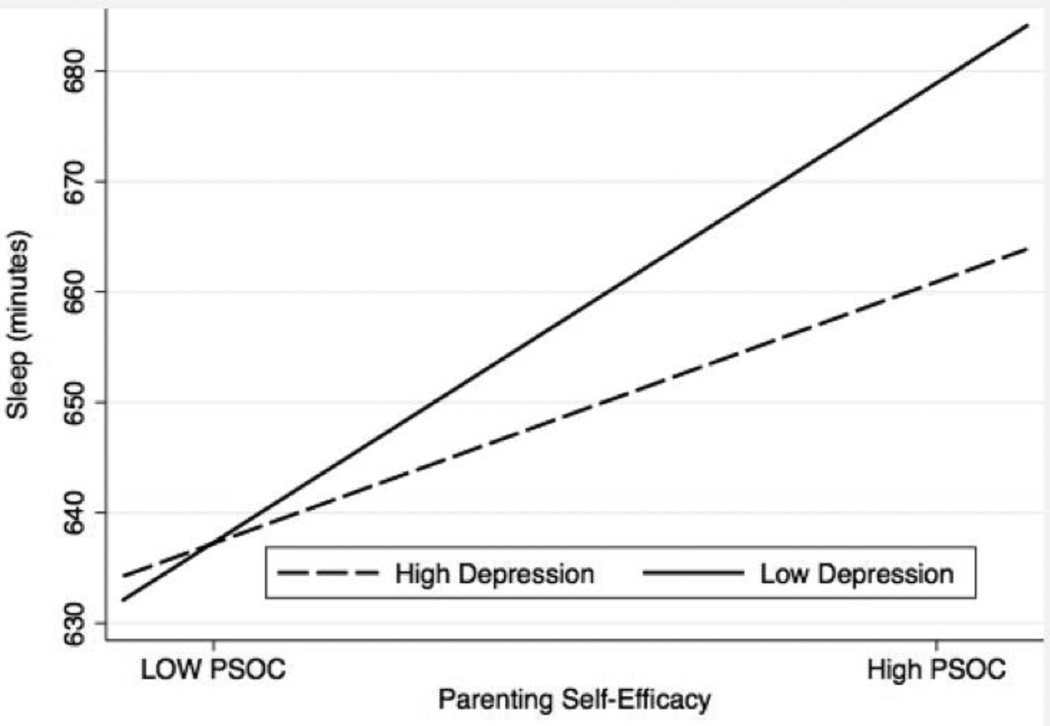
For duration of child’s sleep, however, the results were different. Not only was the PSOC-5 effect significant on all three models, there was also a significant interaction between PSOC-5 and CESD scores on step 3. This interaction is depicted in Figure 2. For parents with low PSOC-5 scores, parent depressive symptoms were not associated with child sleep. But, for parents with higher PSOC-5 scores, higher depressive symptoms were associated with shorter child sleep times.
Figure 2.
The interaction between parenting self-efficacy and parent depression on child sleep (minutes). To illustrate the effect of the interaction from the multivariable regression, representative lines are shown. “Low PSOC” and “low depression” represent scores at the 25th percentile. “High PSOC” and “high depression” represent scores at the 75th percentile. PSOC=Parenting Sense of Competence Scale.
Follow-up Analyses
Two secondary analyses were conducted to further characterize the results. Given the significant finding between PSOC-5 and meal-time media exposure we examined the association between PSOC-5 and total TV time. The median hours of TV watched per day was 2 (IQR 3–5 hours). There was no association between PSOC-5, CESD or their interaction on average daily TV time in multivariable models. We also conducted a secondary analysis among the sub-set of Latino participants, including acculturation as an additional covariate in the multivariable models. Among Latino participants, the median BASH score was 5.4 (IQR 4–6). Inclusion of acculturation in the multivariable models did not change the results.
Discussion
Parenting self-efficacy for mothers from this low-income minority population was associated with important childhood behaviors for healthy childhood growth, including sleep and meal-time media exposure. The results also indicated a positive correlation between parenting self-efficacy and a healthy child diet, but that correlation did not reach statistical significance in adjusted models, warranting further investigation in future studies. There was no association between parenting self-efficacy and child physical activity. Although the effect sizes reported were small (between 0.1 and 0.3), these data suggest that parenting self-efficacy may be an important component of effective parenting by contributing to child behaviors over which parents have the most direct influence, but may not be as important for child behaviors, such as child diet and physical activity, that have a wide range of behavioral influences or a wide range of people who could potentially influence such behaviors.
The home environment for physical activity is an important contributor to childhood obesity. (38) Because child sleep and media exposure during meals are modifiable behaviors that have been associated with childhood obesity, the results from this study suggest that bolstering parenting self-efficacy may be an important approach to fostering a home environment supportive of healthy child growth. (3, 38–43) This is especially important among low-income participants, where the contribution of socioeconomic status to disparities in obesity is well described.(44)
The role of parent depressive symptoms was modest in these analyses. Notably, there was a significant interaction between parenting self-efficacy and parent depressive symptoms on duration of child sleep, with depressive symptoms lessening the protective effect of parenting self-efficacy. This is consistent with previous literature that has identified associations between higher maternal depressive symptoms and shorter sleep duration.(45, 46) These data also highlight the relatively high percentage (22%) of possibly depressed parents in a low-income, minority population such as the one we studied. These associations are of particular importance for the development of childhood obesity interventions both in clinical practice and in the research setting, as specifically targeting parenting self-efficacy and/or depression may be an important component of such interventions. The high rate of elevated depressive symptoms also has implications for a broader set of health outcomes, including both parent and child health.(6, 18, 19, 23) The solution to the problem of childhood obesity will certainly require a multi-faceted approach, and attending to the affective and cognitive aspects of parenting cannot be overlooked.
The results from this study help to address a gap in the existing literature on parenting self-efficacy by focusing on Latino and African American families and by focusing on how parenting-self-efficacy relates to child healthy behaviors. A recent systematic review by Grossklaus and Marvicsin highlighted an important gap in our understanding of how parenting self-efficacy is related to childhood obesity.(47) While their review identified 16 articles that used a measure of general parenting self-efficacy or confidence, only one article explicitly evaluated the association with child feeding behaviors. The previous literature has mainly highlighted the parental determinants of parenting self-efficacy as well as the link between parenting self-efficacy and other measures of child behavior (e.g., behavior problems). Taveras et al., developed a 6-item, context specific scale that investigated a parent’s self-efficacy to make healthy changes (e.g., remove TV from room, change family eating patterns, etc.). Their cross-sectional analysis identified associations between a parent’s context-specific self-efficacy with screen time exposure (β =−0.36 [95% CI:−0.55 to −0.18]), fast-food consumption (β =−0.73 [95% CI:−1.15 to −0.30]), and sugar-sweetened beverage consumption (β =−0.040 [95% CI: −0.080 to −0.002]).(16) Our results rely on a general measure of parenting self-efficacy, rather than a context specific measure. Although our findings indicate a similar magnitude of relationship between general parenting self-efficacy and meal-time media exposure as the one reported by Taveras et al., our associations do not hold for child diet or physical activity. Thus it may be important to include measures of both general parenting self-efficacy and context-specific parent self-efficacy for future behavior-change approaches.
One important potential contributor to the association between parent self-efficacy and child behaviors is culture, more specifically acculturation. The population studied in this analysis had homogenously low acculturation scores, limiting our ability to draw conclusions about a potential relationship. Consequently future research should focus on the intersection of culture and socioeconomic status, investigating how these two important constructs are related to parent self-efficacy and childhood healthy behaviors.
This study’s main limitation is that it is cross-sectional, so no causal inference can be drawn. This is particularly relevant for the association between parent self-efficacy and sleep, as worse childhood sleep patterns could certainly limit a parent’s sense of self-efficacy. In addition, mothers with depressive symptoms might have variable insight into their own self-efficacy. One of the strengths of the current study is the robust nature of the diet (24 hour diet recall) and physical activity (accelerometry) data. The main predictor (PSOC-5) and some of the outcomes are parent-reported, including child sleep, diet recall, and meal-time media exposure. These types of questions would be susceptible to both recall bias and social desirability bias (especially as the survey administration was guided by a research assistant); however, as the bias is likely non-differential, the effect would be to bias the results to the null. We also used a shortened version of the Parenting Sense of Competence scale, one which had not been previously validated either in its current version or in a similar low-income population. Our results demonstrate, however, that this 5-item scale had adequate internal consistency. Our results also provide preliminary evidence for construct validity for the shortened PSOC-5 given the association between the PSOC-5, parent depression, and childhood behaviors. Our sample consisted of 96% mothers, limiting the generalizability of the findings to other child caregivers such as fathers or grandparents. Parents in this analysis had enrolled in and committed to the 3-year RCT, which may have selected for a population of parents with higher self-efficacy than the general population. Finally, even though the sample included a high percentage of overweight children, the inclusion criteria of the parent study excluded obese children from the sample. This may have limited our ability to detect an association by limiting the variability in the behaviors because children who are obese likely have the unhealthiest behaviors. It will be important to evaluate the effect of parenting self-efficacy on healthy childhood behaviors in children who are obese to assess if there are differential effects.
Conclusions for Practice
By demonstrating associations between parenting self-efficacy and childhood behaviors that support healthy childhood growth (i.e., sleep and meal-time media exposure) in a low-income minority population, these data have identified potentially important targets for childhood obesity treatment and prevention programs. Future attempts to curb the childhood obesity epidemic should consider specifically measuring and addressing both the cognitive (parenting self-efficacy) and affective (parent depression) components of parenting to ameliorate this public health crisis.
Significance.
Self-efficacy is a central tenet of behavior change. Parenting self-efficacy may therefore be an important contributor to behavior change in children, which is an understudied contributor to pediatric obesity. This study demonstrates cross-sectional associations between parenting self-efficacy and healthy child behaviors, and describes an interaction with parent depression on child sleep. Targeting parenting self-efficacy and parent depression may be important components of behavioral interventions and clinical care designed to support healthy child growth.
Acknowledgments
Funding
This research was supported by grants U01 HL103620 and U01 Hl103561 with additional support from the remaining members of the COPTR Consortium (U01 HL103622, U01 HD068890, U01 HL103629) from the National Heart, Lung, and Blood Institute and the Eunice Kennedy Shriver National Institute of Child Health and Development and the Office of Behavioral and Social Sciences Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute, the National Institutes of Health, or the National Institute of Child Health and Development. Additional funding was from the following grants from the National Institute of Diabetes and Digestive and Kidney Diseases: P30DK050456 and P30DK092924. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute or the National Institutes of Health. Dr. Heerman’s time was supported by a T32 grant from the NICHD (5T32HD060554) and a K12 grant from the AHRQ (1K12HS022990). Data were managed through REDCap, which is supported from NCATS (UL1 TR000445). Collection of diet data was supported by NORC grant number NIH DK56350.
Footnotes
Conflict of Interests
None of the authors have any competing interests to declare.
Contributor Information
William J. Heerman, Vanderbilt University Medical Center, 2146 Belcourt Avenue, 2nd Floor, Nashville, TN 37212, bill.heerman@Vanderbilt.Edu.
Julie Lounds Taylor, Vanderbilt Kennedy Center, 110 Magnolia Circle, Nashville, TN 37203, julie.l.taylor@vanderbilt.edu.
Kenneth A. Wallston, Vanderbilt University Medical Center, School of Nursing, 461 21st Avenue South, Nashville, TN 37240, ken.wallston@vanderbilt.edu.
Shari L. Barkin, Vanderbilt University Medical Center, Division of General Pediatrics 2200 Children’s Way, DOT 8246, Nashville, TN 37232 shari.barkin@vanderbilt.edu.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA : the journal of the American Medical Association. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang TT, Drewnowski Adam, Kumanyika Shiriki K, Glass Thomas A. A Systems-Oriented Multilevel Framework for Addressing Obesity in the 21st Century. Preventing chronic disease. 2009;6(3) [PMC free article] [PubMed] [Google Scholar]
- 3.Appelhans BM, Fitzpatrick SL, Li H, et al. The home environment and childhood obesity in low-income households: indirect effects via sleep duration and screen time. BMC public health. 2014;14:1160. doi: 10.1186/1471-2458-14-1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu JH, Jones SJ, Sun H, et al. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: an urban and rural comparison. Childhood obesity. 2012;8(5):440–448. doi: 10.1089/chi.2012.0090. [DOI] [PubMed] [Google Scholar]
- 5.Koch FS, Sepa A, Ludvigsson J. Psychological stress and obesity. The Journal of pediatrics. 2008;153(6):839–844. doi: 10.1016/j.jpeds.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Casey P, Goolsby S, Berkowitz C, et al. Maternal depression, changing public assistance, food security, and child health status. Pediatrics. 2004;113(2):298–304. doi: 10.1542/peds.113.2.298. [DOI] [PubMed] [Google Scholar]
- 7.Taveras EM, Gillman MW, Kleinman K, et al. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010;125(4):686–695. doi: 10.1542/peds.2009-2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wrotniak BH, Epstein LH, Paluch RA, et al. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Archives of pediatrics & adolescent medicine. 2004;158(4):342–347. doi: 10.1001/archpedi.158.4.342. [DOI] [PubMed] [Google Scholar]
- 9.Cousins JH, Rubovits DS, Dunn JK, et al. Family versus individually oriented intervention for weight loss in Mexican American women. Public Health Rep. 1992;107(5):549–555. [PMC free article] [PubMed] [Google Scholar]
- 10.Beydoun MA, Wang Y. Pathways linking socioeconomic status to obesity through depression and lifestyle factors among young US adults. J Affect Disord. 2010;123(1–3):52–63. doi: 10.1016/j.jad.2009.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hernandez-Valero MA, Wilkinson AV, Forman MR, et al. Maternal BMI and country of birth as indicators of childhood obesity in children of Mexican origin. Obesity (Silver Spring) 2007;15(10):2512–2519. doi: 10.1038/oby.2007.298. [DOI] [PubMed] [Google Scholar]
- 12.Gundersen C, Lohman BJ, Garasky S, et al. Food security, maternal stressors, and overweight among low-income US children: results from the National Health and Nutrition Examination Survey (1999–2002) Pediatrics. 2008;122(3):e529–e540. doi: 10.1542/peds.2008-0556. [DOI] [PubMed] [Google Scholar]
- 13.Bandura A. Self-efficacy : the exercise of control. New York: W.H. Freeman; 1997. [Google Scholar]
- 14.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 15.Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: a review. Clin Psychol Rev. 2005;25(3):341–363. doi: 10.1016/j.cpr.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Taveras EM, Mitchell K, Gortmaker SL. Parental confidence in making overweight-related behavior changes. Pediatrics. 2009;124(1):151–158. doi: 10.1542/peds.2008-2892. [DOI] [PubMed] [Google Scholar]
- 17.Bohman B, Nyberg G, Sundblom E, et al. Validity and Reliability of a Parental Self-Efficacy Instrument in the Healthy School Start Prevention Trial of Childhood Obesity. Health education & behavior : the official publication of the Society for Public Health Education. 2013;41(4):392–396. doi: 10.1177/1090198113515243. [DOI] [PubMed] [Google Scholar]
- 18.Everson SA, Maty SC, Lynch JW, et al. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. Journal of psychosomatic research. 2002;53(4):891–895. doi: 10.1016/s0022-3999(02)00303-3. [DOI] [PubMed] [Google Scholar]
- 19.Stewart RC. Maternal depression and infant growth: a review of recent evidence. Maternal & child nutrition. 2007;3(2):94–107. doi: 10.1111/j.1740-8709.2007.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilbody S, Bower P, Fletcher J, et al. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives of internal medicine. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 21.Simpson SM, Krishnan LL, Kunik ME, et al. Racial disparities in diagnosis and treatment of depression: a literature review. Psychiatr Q. 2007;78(1):3–14. doi: 10.1007/s11126-006-9022-y. [DOI] [PubMed] [Google Scholar]
- 22.Wittayanukorn S, Qian J, Hansen RA. Prevalence of depressive symptoms and predictors of treatment among U.S. adults from 2005 to 2010. Gen Hosp Psychiatry. 2014;36(3):330–336. doi: 10.1016/j.genhosppsych.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 23.Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 24.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110(3):497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 25.Coleman PK, Karraker KH. Parenting self-efficacy among mothers of school-age children: Conceptualization, measurement, and correlates. Fam Relat. 2000;49(1):13–24. [Google Scholar]
- 26.Po’e EK, Heerman WJ, Mistry RS, et al. Growing Right Onto Wellness (GROW): A family-centered, community-based obesity prevention randomized controlled trial for preschool child-parent pairs. Contemporary clinical trials. 2013;36(2):436–449. doi: 10.1016/j.cct.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gibaud-Wallston J. Self-esteem and situational stress: Factors related to sense of competence in new parents. Dissertation Abstracts International. 1978;39(1-B) [Google Scholar]
- 28.Gibaud-Wallston J, Wandersman LP. Development and Utility of the Parenting Sense of Competence Scale. American Psychological Association; August; Toronto, Canada: 1978. [Google Scholar]
- 29.Gilmore L, Cuskelly M. Factor structure of the Parenting Sense of Competence scale using a normative sample. Child: care, health and development. 2009;35(1):48–55. doi: 10.1111/j.1365-2214.2008.00867.x. [DOI] [PubMed] [Google Scholar]
- 30.Johnston C, Mash EJ. A Measure of Parenting Satisfaction and Efficacy. Journal of Clinical Child Psychology. 1989;18(2):167–175. [Google Scholar]
- 31.Ohan JL, Leung DW, Johnston C. The Parenting Sense of Competence Scale: Evidence of a stable factor structure and validity. Canadian Journal of Behavioural Science. 2000;32(4):251–261. [Google Scholar]
- 32.Rogers HH, Matthews JJ. The Parenting Sense of Competence Scale: Investigation of the factor structure, reliability, and validity for an Australian Sample. Australian Psychologist. 2004;39(1):88–96. [Google Scholar]
- 33.Lewinsohn PM, Seeley JR, Roberts RE, et al. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and aging. 1997;12(2):277–287. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- 34.Pate RR, Almeida MJ, McIver KL, et al. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring) 2006;14(11):2000–2006. doi: 10.1038/oby.2006.234. [DOI] [PubMed] [Google Scholar]
- 35.Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. Journal of the Academy of Nutrition and Dietetics. 2013;113(4):569–580. doi: 10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harrell FE. Regression modeling strategies : with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- 37.Mills SD, Malcarne VL, Fox RS, et al. Psychometric Evaluation of the Brief Acculturation Scale for Hispanics. Hisp J Behav Sci. 2014;36(2):164–174. doi: 10.1177/0739986314526697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tandon PS, Zhou C, Sallis JF, et al. Home environment relationships with children’s physical activity, sedentary time, and screen time by socioeconomic status. The international journal of behavioral nutrition and physical activity. 2012;9:88. doi: 10.1186/1479-5868-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knutson KL. Does inadequate sleep play a role in vulnerability to obesity? Am J Hum Biol. 2012;24(3):361–371. doi: 10.1002/ajhb.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child development. 2007;78(1):309–323. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 41.Bell JF, Zimmerman FJ. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Archives of pediatrics & adolescent medicine. 2010;164(9):840–845. doi: 10.1001/archpediatrics.2010.143. [DOI] [PubMed] [Google Scholar]
- 42.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16(3):643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Falbe J, Rosner B, Willett WC, et al. Adiposity and different types of screen time. Pediatrics. 2013;132(6):e1497–e1505. doi: 10.1542/peds.2013-0887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shrewsbury V, Wardle J. Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990–2005. Obesity (Silver Spring) 2008;16(2):275–284. doi: 10.1038/oby.2007.35. [DOI] [PubMed] [Google Scholar]
- 45.El-Sheikh M, Kelly RJ, Bagley EJ, et al. Parental depressive symptoms and children’s sleep: the role of family conflict. J Child Psychol Psychiatry. 2012;53(7):806–814. doi: 10.1111/j.1469-7610.2012.02530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Keller PS, Kouros CD, Erath SA, et al. Longitudinal relations between maternal depressive symptoms and child sleep problems: the role of parasympathetic nervous system reactivity. J Child Psychol Psychiatry. 2014;55(2):172–179. doi: 10.1111/jcpp.12151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Grossklaus H, Marvicsin D. Parenting efficacy and its relationship to the prevention of childhood obesity. Pediatric nursing. 2014;40(2):69–86. [PubMed] [Google Scholar]