Abstract
Objectives
This study examines the main and moderating effects of childhood abuse or neglect severity, income, and family social support on the presence of postpartum depressive symptoms (PDS).
Methods
Participants included 183 postpartum mothers who endorsed a history of childhood maltreatment (CM) and enrolled in a longitudinal study of mother and child outcomes. Participants completed questionnaires to assess CM severity, associated societal and maternal characteristics, and depressive symptom severity.
Results
The results confirm previously identified links between CM severity and PDS. Further, hierarchical linear regression analyses indicate the interaction of household income and interpersonal support from the family attenuates the relationship between CM severity and PDS. The final model accounted for 29% of the variance of PDS scores, a large effect size.
Conclusions
This study is the first to demonstrate interrelationships between income and social support on resilience to postpartum psychopathology in childhood trauma-surviving women. Social support appeared to protect against PDS for all mothers in this study while income only conferred a protective effect when accompanied by family support. For clinicians, this implies the need to focus on improving family and other relationships, especially for at-risk mothers.
Significance
A history of CM has demonstrated deleterious effects in general and postpartum populations. Given the potential negative impact on mothers and their children, investigators have examined the potential for income and social support to protect against adverse outcomes. Our study adds to this literature by examining the variance explained by CM severity and the interaction of family support and income on depression following childbirth. Our unique findings identify specific contexts in which family support and income buffer against CM-PDS associations for women with compound risks. As such, particular policies and clinical interventions may be more strategically tailored for this population.
Keywords: postpartum depression, childhood maltreatment, women, social support, income
Introduction
A recent national survey found 37% of youths acknowledged past year physical assault with 5% of young girls describing sexual abuse during childhood, and 15% indicating maltreatment was perpetrated by a caregiver (Finkelhor, Turner, Shattuck, & Hamby 2015). There is extensive literature supporting a link between childhood maltreatment (CM) exposure and adverse mental health outcomes in adulthood. In particular, major depressive disorder (MDD), Posttraumatic Stress Disorder, anxiety, interpersonal aggression, and suicide attempts are frequently noted sequelae in adults reporting abuse and neglect in early development (Hamilton, Micol-Foster, & Muzik 2015; Harford & Grant 2014; Kaplow & Widom 2007; Sexton, Hamilton, McGinnis, Rosenblum, & Muzik 2015). Compounding these threats to public health, a history of CM increases risk of recurrent depressive episodes throughout the lifespan and is associated with more treatment refractory responses to evidence based interventions for postpartum depressive symptoms (PDS) (Cort et al. 2012; Nanni, Uher, & Danese 2012).
Within the context of childbearing, postpartum depression is a common condition that has demonstrated adverse effects on both maternal and child wellbeing (O'Hara & McCabe 2013). A recent systematic review confirmed robust relationships between CM and perinatal mood disorders (Choi & Sikkema 2015; Buist & Janson, 2001). Further, studies have identified associations between CM, maternal psychopathology, and mother-infant bonding and child development, thus increasing the probability of intergenerational transmission of risk (e.g., Martinez-Torteya et al. 2014; Muzik et al. 2013; Sexton et al. 2015).
Despite the elevated likelihood of deleterious lifespan trajectories secondary to CM, negative outcomes are preventable. In the past two decades, empirical investigations have expanded their scope to improve our understanding of factors that may attenuate CM-adult MDD associations. In non-postpartum populations, several constellations of risk and resilience have been identified following CM exposure. Some of the most robust findings concern the function of socioeconomic status (SES) as a moderating factor. Several studies have demonstrated strong correlations between CM and poverty (Sansone, Leung, & Weiderman 2012; Covey, Menard & Franzese 2013). Importantly, Zielinski (2009) demonstrated that a history of CM adversely affected employment status, income, and healthcare coverage in adults even after controlling for race, sex, age, and indicators of economic status in childhood. In turn, poverty in adulthood is one of the most consistent predictors of depression symptom severity (e.g., Kosidou et al. 2011), as well as of depression specifically in postpartum (Patel et al., 2002). Women with CM histories, especially those with demographic risk (e.g., low income), and with preexisting mental illness, are at greatest risk for postpartum symptom relapse (Muzik et al., 2016). Several investigations of CM survivors also find social support mediates the relationship between childhood maltreatment and later adjustment, particularly for women (e.g. McGloin & Widom 2001).
A number of findings implicate low income as a salient factor affecting the mental health and wellbeing of postpartum women. A growing body of research suggests new mothers who report low-income or financial stress (Bener, Gerber, & Sheikh 2012; Gjerdingen, McGovern, Attanasio, Johnson & Kozkimannil 2014) show higher rates of depressive symptoms. More specifically, a longitudinal examination of women 0-3 years following childbirth found that decreases in income were associated with worsening depression, while increases in income were associated with symptom recovery (Dearing, Taylor, & McCartney 2004). Application of the social stress process model (Pearlin 1989) provides a possible explanation for the relationship between low income and PDS. Based on the model, increased stress associated with new motherhood is compounded by both financial insecurity and limited access to coping resources that results in increased vulnerability for depression. Of particular concern, low-income mothers with PDS are also less likely to have access to resources such as healthcare, a good education for their older children, and basic necessities. This makes it especially difficult to engage in treatment or improve their financial situation, making recovery a unique challenge in this population (Segre, O'Hara, Arndt, & Stuart 2007). It should also be emphasized that income-PDS associations have been less well replicated in developed countries (Norhayati, Hazlina, Asrenee, & Emilin 2015), suggesting continued research in this area is important.
Social support may confer unique postpartum benefits. For instance, Stuart and O'Hara (1995) extended Sullivan's (1953) interpersonal theory to conceptualizing and treating PDS. They note this vulnerable period is often complicated by disturbances in partner and personal relationships, such as discrepancies between desired and received social support for childcare (Stuart & O'Hara 1995). Notably, lacking social support from friends, and family has also been shown to play a particularly significant role in the onset and maintenance of PDS (Gjerdingen et al., 2014; Leahy-Warren, McCarthy, & Corcoran 2012). In addition to general interpersonal supports, a recent review also specifically identified poor marital relationships as contributors to increased PDS risk (Norhayati et al., 2015). However, the interactive influences of income and interpersonal support on depressive symptom outcomes have not yet been investigated in postpartum women with CM exposure. Identification of factors which protect against the heightened risk of PDS in women with low income and histories of CM (e.g.family support) is necessary to prevent and address maternal and child adversity.
The present study aims to fill this existing gap in the literature by extending prior research on CM and subsequent maternal depressive symptoms through investigating the effects of income and social support on postpartum depressive symptom outcomes. Similar to previous research, we hypothesize main effects will occur such that greater CM severity and lower income and social support will be associated with more severe PDS. We then extend our investigation to examine interaction effects and anticipate mothers with high incomes and social support to be significantly less symptomatic than their peers with less income and support.
Methods
Procedures and Participants
Participants in this study were recruited for a longitudinal study with the overall aim to study the impact of maternal childhood maltreatment exposure on the entry to motherhood, on maternal mental well-being and parenting, and ultimately also offspring outcomes. Participants for the [blind for review] Study (N=268) were recruited from community obstetric clinics, childbirth classes, newspaper advertisements, and other peripartum research projects. Inclusion criteria were: aged 18 or older, within 8 weeks postpartum, no past or recent (< 3months) history of psychosis or substance abuse, delivered child without significant developmental delay or medical illness and not premature (>34 weeks gestation). Participants enrolled in a longitudinal investigation spannig from 4- to 18-months postpartum, and includes phone, home, and office-based data collection. For the purposes of this report, we restricted our analyses to include only women with histories of CM exposure (n = 183).
At four months postpartum, mothers completed a self-report questionnaire (CTQ; Bernstein and Fink 1998) to assess CM exposure. In addition to the CTQ, women also provided information on postpartum mental health, sociodemographic characteristics (including income) and satisfaction with family support at the 4-months phone call.
All participants provided written informed consent and the study has been approved by the University Institutional Review Board. Women received an honorarium of $10 for the 4 months phone interview and a maximum honorarium of $130 for their participation in the overall longitudinal research.
Measures
Sociodemographic Characteristics
Participants completed a 28-item assessment of cohabitation status, race/ethnicity, employment, income, and educational history, maternal and child health concerns, and perinatal medication use.
Assessment of Childhood Trauma
The Childhood Trauma Questionnaire (CTQ; Bernstein & Fink 1998) is a 28-item self- report questionnaire, with each item being rated on a 5-point Likert scale ranging from “Never True” to “Very Often True”. The questionnaire is then scored to create five domain scales: Emotional Abuse, Physical Abuse, Sexual Abuse, Physical Neglect, and Emotional Neglect. The CTQ also yields a total abuse severity score by summing across all scale scores. The CTQ total score was used in all analyses.
Postpartum Depressive Symptoms
PDS were measured on the Postpartum Depression Screening Scale (PPDS; Beck & Gable 2002). The PPDS is a 35-item questionnaire that is a rated on a 5-point Likert scale, ranging from “Strongly Disagree” to “Strongly Agree”. The sum for the PPDS yields psychopathology symptom scores for depression (range 35-175). Scores above 80 are suggestive of a likely MDD diagnosis. In all analyses, PPDS total sum score was used.
Family Support
Current level of family social support was measured with a 5-item scale, the Family Adaptation, Partnership, Growth, Affection, and Resolve scale (FAPGAR; Smilkstein 1978). This measure has been validly used with different populations to assess the level of family functioning and support (Chaves et al., 2013; Chen et al., 2015). Adaptation is characterized by one's use of familial resources for the purpose of problem solving during a stressful moment or crisis. Partnership is characterized by the sense that one is an integral part of the family network, with members sharing and discussing problems and feelings with the individual. Growth is characterized by one's belief that the family is maturing physically and emotionally through reciprocal support and guidance. Affection is thought to represent the compassionate or loving relationship among members of the family. Resolve is defined as one's commitment to supporting other members of the family emotionally and physically. Items are rated on a 4-point Likert scale, with responses ranging from “Never” to “Always”. Scores range from 0 to 20, with higher scores indicating a higher level of support. Sample items include, “I am satisfied that I can turn to my family to help when something is troubling me”.
Data Analysis
Demographic variables were evaluated with descriptive means and percentages as appropriate. A correlation matrix was used to analyze initial assessments of interrelationships between PDS and our predictive variables using Pearson r and Spearman Rho correlations as warranted for scale and ordinal data. To test our hypotheses, a regression model was computed to assess capacity to account for PDS. Using hierarchical linear regression (HLR), we tested the influence of distal CM followed by a second step incorporating our proximal variables of interest (income, family support, and their interaction) to ascertain their capacity to explain PDS variance beyond CM.
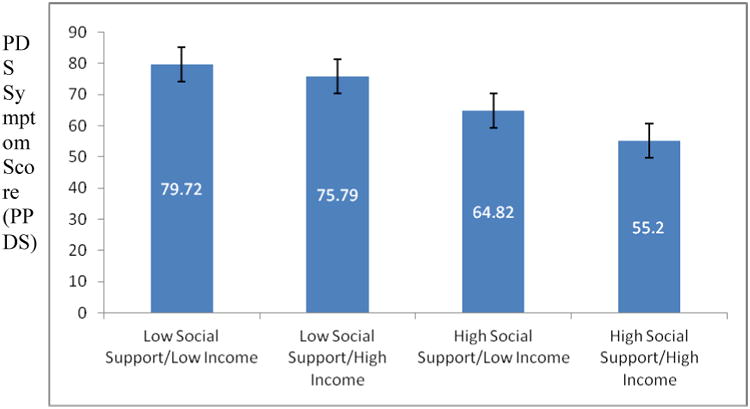
Following the HLR analysis, we conducted post-hoc analyses to assess the interactive pattern of social support and income. Participants were divided into high and low risk groups using the median split on the continuous social support variable and the household income variables. The high-social support risk group consisted of all participants who had an FAPGAR score greater than 17, and the low-social support risk group was all participants who had an FAGPAR score less than 17. The high-income and low-income groups consisted of mothers with an annual household income above or below $50,000. The four resulting groups (high income/low social support, low income/low social support, high income/high social support, and low income/high social support) were used to compare group differences on PDS using ANOVA and Tukey post-hoc processes.
Results
Participants were generally young, as would be expected in a study investigating childbearing women. Mothers were primarily Non-Hispanic White and married. The average PDS score was elevated but below the clinical cutoff suggestive of MDD diagnoses; 22.4% of women were above the clinical cutoff for diagnosis. No significant differences between the demographics characterizing those with a history of CM and mothers enrolled in the larger MACY study were observed. See Table 1 for descriptive statistics specific to demographic and mental health assessments.
Table 1. Characteristics of population of abuse survivors.
| Characteristics | Frequency/Mean | Value/Standard Deviation |
|---|---|---|
| Mother's Age | 29.15 | 6.15 |
| Race (Non-Hispanic White) | 67 | 58.8% |
| Marital Status (Married) | 75 | 41% |
| Annual Household Income | ||
| < $15,000/year | 47 | 30.9% |
| $15,000-25,000 | 19 | 12.5% |
| $25,000-50,000 | 27 | 17.8% |
| $50,000-75,000 | 57 | 37.5% |
| >$75,000/year | 2 | 1.3% |
| Educational Level (some college or higher) | 98 | 53.5% |
| PPDS Scale Score | 69.19 | 23.34 |
| Probable MDD Diagnosis (PPDS) | 41 | 22.4% |
| FAPGAR Score | 14.98 | 4.28 |
| CTQ Score | 51.51 | 17.18 |
Notes: CTQ = Childhood Trauma Questionnaire, PPDS = Postpartum Depression Screening Scale, FAPGAR = Family Adaptation, Partnership, Growth, Affection, and Resolve scale; MDD= Major Depressive Disorder.
Initial relationships between PDS, CM severity, income, and family social support are provided in Table 2. As expected, PDS evidenced a significant positive correlation with CM severity and negative relationships with family social support and income. CM exposure was negatively correlated with current social support and household income. However, income and family social support were not significantly related.
Table 2. Correlation matrix between Childhood Maltreatment, Associated Factors, and Postpartum Depression Symptom Scores.
| Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. CTQ | - | -0.163* | -0.242** | 0.336** |
| 2. Household Income | -0.163* | - | 0.123 | -0.216** |
| 3. FAPGAR | -0.242** | 0.123 | - | -0.440** |
| 4. PPDS | 0.336** | -0.216** | -0.440** | - |
The HLR investigating predictors of PDS severity demonstrated several significant findings (Table 3). In the first step, CM severity was confirmed as a significant predictor of depressive symptoms, accounting for 11.9% of the variance in the model. Cohen's f2 suggests a small-to-moderate effect size for this relationship. In the second step, CM severity and the interaction of social support and income emerged as significant predictors of PDS while support and income did not evidence significant relationships beyond their interaction. The second step yielded a statistically significant improvement over consideration of CM severity alone. The final model accounted for 29% of the overall variance in PDS scores with a strong effect size.
Table 3. Multiple Linear Regression for Factors Predicting PDS.
| Step | Predictor | β | SE | p | R2 (R2Δ) | F2 | Δp | R2 | f2 | p |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | CTQ | .345 | .102 | <.001** | .119 | .135 | <.000** | |||
|
| ||||||||||
| 2 | CTQ | .214 | .097 | .004** | ||||||
| FAPGAR | -.085 | .783 | .561 | |||||||
| Household Income | .402 | 4.375 | .101 | |||||||
| FAPGAR* Household Income | -.648 | .286 | .028* | |||||||
| .170 | .2 | <.001** | .289 | .406 | .028* | |||||
Notes: PDS = Postpartum depressive symptoms, CTQ = Childhood Trauma Questionnaire, FAPGAR = Family Adaptation, Partnership, Growth, Affection, and Resolve scale. Numbers in matrix for ß represent standardized ß coefficients.
p <.05,
p <.01
Given the significant interaction of social support and income in our regression model, we investigated group differences based on low and high family support and income and PDS outcomes. The ANOVA demonstrated significant between-group differences on depression scores, F(3, 147) = 10.18, p <.001. As illustrated in Figure 1, Tukey post-hoc analyses yielded significant differences (p=0.002) between the low social support/high income group (M=75.79, SD=22.88) and high social support/high income group (M=55.20, SD=17.36). In addition, there were significant differences (p=.006) between the low social support/low income group (M=79.72, SD=24.41) and the high social support/low income group (M=64.82, SD=19.95). Finally, significant differences (p<.001) were found between the low social support/low income group and the high social support/high income group.
Figure 1. PDS symptoms at 4 months by Income/Social Support Status.
Discussion
Consistent with extant literature and supporting our initial hypothesis, CM severity was a moderate predictor of PDS. Given consistent and overwhelming evidence that the toxic effects of distal adverse events such as CM are associated with adversity in adulthood (e.g. Hamilton et al. 2015), and that risk is increased further among new mothers (Gjerdingen et al. 2014), continued prevention and early intervention efforts are imperative.
The fact that many postpartum women in our study with a history of CM did not evidence elevated postpartum mood symptoms is encouraging and suggests developmental or proximal factors may engender a ‘plasticity’ to long-term responses to early injury. In our investigation of current factors that may promote resilience to perinatal depression in the context of CM, we did note, as has previously been reported (e.g. Norhayati et al. 2015), greater social and family support is associated with improved postpartum outcomes, whereas, as expected, low income is negatively associated with positive outcomes.
However, when taking into account main and interactive effects of family support and income on PDS, the benefits appear less direct. Our findings suggest a more complex view of the roles these factors are associated with pathology. As noted, social support and low income have traditionally been treated as risk and protective factors that may independently confer or defer risk (e.g. Milgrom et al., 2008). Contrary to hypotheses, we did not observe significant main effects for either family support or income within the HLR analysis. Instead, the most noteworthy and clinically relevant findings concerning these factors were rooted in their interactive relationships as illustrated in Figure 1. Women with the lowest reported family social support were at highest risk for PDS, generally irrespective of income. Consistent with prior research (e.g. Leahy-Warren et al., 2012), our results suggest interpersonal relationships are vital to most mothers with CM during the postpartum period. Further, the co-occurrence of relatively high income and high family social support evidenced the best outcomes with respect to PDS, whereas high family social support predicted a powerful protective effect on PDS in the context of low income. By contrast, high income in the absence of social support was not associated with lower levels of PDS. To summarize in lay terms, “Relationships help. Money by itself does not, but surely helps when relationships are good”, at least for mothers with CM histories.
Policy Implications
Recognizing the link between social support and economics and risk or resilience to perinatal depression, both have been targets for prevention or intervention. From a policy prevention perspective, there is a recent call for paid maternity leave in the United States, as the U.S. is the only country among advanced economies that doesn't mandate paid maternity leave in contrast to Europe or Canada (The Organization for Economic Co-operation and Development 2015); paid maternity leave would promote economic security and allow for socialization of new mothers on maternity leave.
Individual Intervention Implications
From a clinical perspective, social support, especially from partner and/or family, is recognized as a key ingredient to lower postpartum risk for mood disorders, and has been the centerpiece of the most evidence-based psychotherapy for perinatal depression, that is Interpersonal Psychotherapy (O'Hara, M. W., Stuart, S., Gorman, L.L., Wenzel, A. (2000). Furthermore, in clinical practice the awareness that financial strain counteracts wellness and jeopardizes treatment engagement (Muzik et al., 2014) is known, and therefore many therapy programs offer referrals to financial resources along with more traditional psychotherapy (e.g., Grote et al. 2015; Muzik et al. 2015).
Applied to clinical practice, these findings have the potential to further risk assessment and treatment optimization for PDS in individuals with CM history in a number of ways. First, enhancing social and family support, either directly by improving family relationships or indirectly by working to augment a patients' network of supportive relationships, should be a salient goal when treating mothers with a CM history, irrespective of income. Thus, screening for the quality of social support and provision of or referral to relationship-based, social support enhancing therapies seem critical from a public health perspective. Such efforts are now underway with the integration of behavioral health consultants into primary care (e.g., obstetrics, family medicine, pediatrics), who perform screening for social networks and adversity, as well as delivery of interpersonal therapy or referrals (Grote et al. 2015).
Second, women with multiple, cumulative risk factors (i.e., low income, low family support, greater CM severity history) may require more intensive acute interventions, and would likely benefit from treatments capable of concurrently addressing elevating personal income and specifically targeting enhancement of social support (e.g., Muzik et al. 2015). Postpartum women with higher incomes may benefit from PDS through IPT alone while mothers with economic concerns may find IPT augmented with a case management or liaison approach that addresses financial domains and access to available resources maximally beneficial (e.g., Grote et al. 2015).
This study also has important risk assessment and management implications. As stated, the explanatory power of CM severity on PDS severity was moderate and significant. However, the addition of income and family social support doubled the variance explained by our model providing strong evidence for their clinical significance. Through early assessment of these social and economic domains (i.e., prior to delivery) providers may detect cases at greater risk for negative mood postpartum and provide well-timed, tailored preventative care that protects against emotional, cognitive, and behavioral postpartum vulnerabilities for both mother and child.
Limitations
Several limitations of this investigation are notable. First, assessment of CM was retrospective, increasing the possibility of error introduced as a consequence of recall bias. As observed in other investigations using retrospective assessment, it may be that depressed or euthymic moods alter recall accuracy for abuse and neglect or perceptions of CM severity through processes such as mood-congruent recall of memories (Brewen et al. 1993). Second, our research focused only on depressive symptoms within the context of CM. As such, findings may not generalize to other mental health concerns often experienced postpartum or women without experiences of CM during early development. Third, household annual income is only one facet of the broader construct of SES. At present, it is unknown whether main and moderating effects would be demonstrated with other aspects of SES (e.g., education, occupation). Fourth, our attention to social support is restricted in this study to family support. We are not able to confirm whether non-family supports would be protective against PDS and whether the strength of this association would rival that demonstrated within the family. Fifth, household income may be associated with several additional risk factors. Given the absence of statistical controls and limited number of variables investigated, it may be the case that some of the variance identified in our study may be due to additional and unmeasured factors. Finally, the findings in this study may not be generalizable to other populations with unique risk factors, as this sample is largely Caucasian, educated, and married.
Conclusion
Despite these challenges, this study makes several novel contributions to the field. To our knowledge, this investigation is the first to examine the cumulative and interactive relationships between history of CM, social supports, and income in conferring risk for or protecting against PDS symptom severity. While, providers cannot “un-ring the bell” and modify maltreatment histories, this study highlights potential targets that may improve the ability to amend developmental trajectories to reduce postpartum psychopathology and promote resilience and recovery in at-risk mothers. Given the well-documented vulnerability of this population, and the potential for danger not only to mothers, but their children as well, amelioration of PDS should be a high public health priority. These results move the literature forward towards providing more targeted and efficacious responses for a population both deserving and requiring research and clinical scrutiny.
Several additional research questions arise in the face of our findings. Do postpartum mothers respond differently to psychotherapeutic interventions based on support-income interactions? Do mothers with chronic low income differ from those with temporarily reduced income such as employed women on bed rest or using maternity leave that expect to return to work? Are similar relationships between support and income found for other risks associated with CM such as PTSD, mother-infant interactions, or child development? Continued attention to postpartum mental health and wellness following adversity may augment our ability to identify individual, clinical, and community strategies to bolster adaptation and reduce intergenerational transmission of risk. Taken together, our results underscore the importance of continuing to investigate observed risk and resilience factors in the context of childbearing as well as their potential interactive effects.
Acknowledgments
Support for this research was provided by grants from the National Institute of Mental Health and Eunice Kennedy Shriver National Institute of Child Health and Human Development (MH080147; PI: Muzik) and the Michigan Institute for Clinical and Health Research at the University of Michigan (UL1RR024986; PI: Muzik). The Mental Health Service at VA Ann Arbor Healthcare System also supported this research. The authors wish to thank the mothers and children who made this research possible and gratefully acknowledge the contributions to the project of Amanda Ellis, Heather Cameron, Rena Menke, Kelsie Rodriguez, Ellen Waxler McGinnis.
References
- The Organisation for Economic Co-operation and Development (OECD) (n.d.). Retrieved from http://www.oecd.org/social/family/database.htm.
- Beck CT, Gable RK. Postpartum Depression Screening Scale. Vol. 1. Los Angeles, CA: Western Psychological Services; 2002. [Google Scholar]
- Bener A, Gerber LM, Sheikh J. Prevalence of psychiatric disorders and associated risk factors in women during their postpartum period: a major public health problem and global comparison. International journal of women's health. 2012;4:191. doi: 10.2147/IJWH.S29380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein D, Fink L. Childhood Trauma Questionnaire: A retrospective self-report. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience: A reappraisal of retrospective reports. Psychological bulletin. 1993;113(1):82. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- Buist A, Janson H. Childhood sexual abuse, parenting and postpartum depression—a 3-year follow-up study. Child Abuse & Neglect. 2001;25(7):909–921. doi: 10.1016/s0145-2134(01)00246-0. [DOI] [PubMed] [Google Scholar]
- Chaves CB, Amaral OP, Nelas PA, Coutinho EC, Dionisio RM. Assessment of family functionality among the elderly with chronic illness. The European Journal of Counselling Psychology. 2013;2(2):139–144. [Google Scholar]
- Chen JY, Chen HS, Liu MC, Chao MC. Relationship between Families Perception of Health and Support in the Care of Vulnerable Children. Clinics in Mother and Child Health. 2015;2015 [Google Scholar]
- Choi KW, Sikkema KJ. Childhood maltreatment and perinatal mood and anxiety disorders: A systematic review. Trauma, Violence, & Abuse. 2015:1–27. doi: 10.1177/1524838015584369. [DOI] [PubMed] [Google Scholar]
- Cort NA, Gamble SA, Smith PN, Chaudron LH, Lu N, He H, Talbot NL. Predictors of treatment outcomes among depressed women with childhood sexual abuse histories. Depression and anxiety. 2012;29(6):479–486. doi: 10.1002/da.21942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covey HC, Menard S, Franzese RJ. Effects of adolescent physical abuse, exposure to neighborhood violence, and witnessing parental violence on adult socioeconomic status. Child maltreatment. 2013 doi: 10.1177/1077559513477914. [DOI] [PubMed] [Google Scholar]
- Dearing E, Taylor BA, McCartney K. Implications of family income dynamics for women's depressive symptoms during the first 3 years after childbirth. Am J Public Health. 2004;94:1372–1377. doi: 10.2105/ajph.94.8.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, Hamby SL. Prevalence of Childhood Exposure to Violence, Crime, and Abuse: Results from the National Survey of Children's Exposure to Violence. JAMA Pediatrics. 2015;169(8):746–754. doi: 10.1001/jamapediatrics.2015.0676. [DOI] [PubMed] [Google Scholar]
- Gjerdingen D, McGovern P, Attanasio L, Johnson PJ, Kozhimannil KB. Maternal depressive symptoms, employment, and social support. The Journal of the American Board of Family Medicine. 2014;27(1):87–96. doi: 10.3122/jabfm.2014.01.130126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Katon WJ, Russo JE, Lohr MJ, Curran M, Galvin E, Carson K. Collaborative care for perinatal depression in socioeconomically disadvantaged women: a randomized trial. Depression and anxiety. 2015 doi: 10.1002/da.22405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton L, Micol-Foster V, Muzik M. Childhood Maltreatment Trauma: Relevance for Adult Physical and Emotional Health. A Review. Trauma Cases Rev. 2015;1:003. [Google Scholar]
- Harford TC, Yi HY, Grant BF. Associations between childhood abuse and interpersonal aggression and suicide attempt among US adults in a national study. Child Abuse & Neglect. 2014;38(8):1389–1398. doi: 10.1016/j.chiabu.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplow JB, W CS. Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology. 2007;116:176–187. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]
- Kosidou K, Dalman C, Lundberg M, Hallqvist J, Isacsson G, Magnusson C. Socioeconomic status and risk of psychological distress and depression in the Stockholm Public Health Cohort: A population-based study. Journal of affective disorders. 2011;134(1):160–167. doi: 10.1016/j.jad.2011.05.024. [DOI] [PubMed] [Google Scholar]
- Leahy-Warren P, McCarthy G, Corcoran P. First-time mothers: social support, maternal parental self-efficacy and postnatal depression. Journal of Clinical Nursing. 2012;21(3-4):388–397. doi: 10.1111/j.1365-2702.2011.03701.x. [DOI] [PubMed] [Google Scholar]
- Martinez-Torteya C, Dayton CJ, Beeghly M, Seng JS, McGinnis E, Broderick A, Rosenblum K, Muzik M. Maternal parenting predicts infant biobehavioral regulation among women with a history of childhood maltreatment. Development and psychopathology. 2014;26(2):379–392. doi: 10.1017/S0954579414000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGloin JM, W CS. Resilience among abused and neglected children grown up. Development and Psychopathology. 2001;13:1021–1038. doi: 10.1017/s095457940100414x. [DOI] [PubMed] [Google Scholar]
- Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, Thelen K, Seng JS. Mother-infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Arch Womens Ment Health. 2013;16(1):29–38. doi: 10.1007/s00737-012-0312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Schmicker M, Alfafara E, Dayton C, Schuster M, Rosenblum KL. Predictors of Treatment Engagement to a Parenting Intervention among Caucasian and African-American Mothers. Journal of Social Service Research. 2014;40(5):662–680. [Google Scholar]
- Muzik M, Rosenblum KL, Alfafara EA, Schuster MM, Miller NM, Waddell RM, Stanton Kohler E. Mom Power: preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Arch Womens Ment Health. 2015;18(3):507–521. doi: 10.1007/s00737-014-0490-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, McGinnis EW, Bocknek E, Morelen D, Rosenblum KL, Liberzon I, Abelson JL. Ptsd symptoms across pregnancy and early postpartum among women with lifetime ptsd diagnosis. Depress Anxiety. 2016 Jul;33(7):584–591. doi: 10.1002/da.22465. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. 2012;169:141–151. doi: 10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- Norhayati MN, Hazlina NN, Asrenee AR, Emilin WW. Magnitude and risk factors for postpartum symptoms: A literature review. Journal of affective disorders. 2015;175:34–52. doi: 10.1016/j.jad.2014.12.041. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry. 2000;57(11):1039–45. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annual review of clinical psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- Patel V, Rodrigues M, DeSouza n. Gender, Poverty, and Postnatal Depression: A Study of Mothers in Goa, India. Am J Psychiatry. 2002;159(1):43–47. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- Pearlin LI. The sociological study of stress. Journal of health and social behavior. 1989:241–256. [PubMed] [Google Scholar]
- Sansone RA, Leung JS, Wiederman MW. Five forms of childhood trauma: Relationships with employment in adulthood. Child abuse & neglect. 2012;36(9):676–679. doi: 10.1016/j.chiabu.2012.07.007. [DOI] [PubMed] [Google Scholar]
- Segre LS, O'Hara MW, Arndt S, Stuart S. The prevalence of postpartum depression. Social Psychiatry and Psychiatric Epidemiology. 2007;42(4):316–321. doi: 10.1007/s00127-007-0168-1. [DOI] [PubMed] [Google Scholar]
- Sexton MB, Hamilton L, McGinnis EW, Rosenblum KL, Muzik M. The roles of resilience and childhood trauma history: main and moderating effects on postpartum maternal mental health and functioning. Journal of affective disorders. 2015;174:562–568. doi: 10.1016/j.jad.2014.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smilkstein G. The family APGAR: A proposal for a family function test and its use by physicians. The Journal of Family Practice. 1978;6(8):1231–1239. [PubMed] [Google Scholar]
- Stuart S, O'Hara MW. Interpersonal psychotherapy for postpartum depression: A treatment program. Journal of Psychotherapy Practice and Research. 1995;4:18–29. [PMC free article] [PubMed] [Google Scholar]
- Sullivan HS. The interpersonal theory of psychiatry. New York: Norton; 1953. [Google Scholar]
- Zielinski DS. Child maltreatment and adult socioeconomic well-being. Child abuse & neglect. 2009;33:666–678. doi: 10.1016/j.chiabu.2009.09.001. [DOI] [PubMed] [Google Scholar]


