Abstract
Objective
Diversity in the physician workforce is essential to providing culturally effective care. In critical care, despite the high stakes and frequency with which cultural concerns arise, it is unknown whether physician diversity reflects that of critically ill patients. We sought to characterize demographic trends in critical care fellows, who represent the emerging intensivist workforce.
Design
We used published data to create logistic regression models comparing annual trends in the representation of women and racial/ethnic groups across critical care fellowship types.
Setting
United States Accreditation Council on Graduate Medical Education (ACGME)-approved residency and fellowship training programs.
Participants
Residents and fellows employed by ACGME-accredited training programs from 2004 to 2014.
Interventions
None.
Measurements and Main Results
From 2004–14, the number of critical care (CC) fellows increased annually, up 54.1% from 1,606 in 2004–05 to 2,475 in 2013–14. The proportion of female CC fellows increased from 29.5% (2004–05) to 38.3% (2013–14) (p<0.001). The absolute number of black fellows increased each year but the percentage change was not statistically significantly different (5.1% in 2004–05 vs. 3.9% in 2013–14 (p=0.92)). Hispanic fellows increased in number from 124 (7.7%) in 2004–05 to 216 (8.4%) in 2013–14 (p=0.015). The number of American Indian/Alaskan Native/Native Hawaiian/Pacific Islander fellows decreased from 15 (1.0%) to 7 (0.3%) (p<0.001). When compared to population estimates, female CC fellows and those from racial/ethnic minorities were under-represented in all years.
Conclusions
The demographics of the emerging critical care physician workforce reflect under-representation of women and racial/ethnic minorities. Trends highlight increases in women and Hispanics and stable or decreasing representation of non-Hispanic underrepresented minority CC fellows. Further research is needed to elucidate the reasons underlying persistent under-representation of racial and ethnic minorities in critical care fellowship programs.
Key words for indexing: critical care, medical staff, hospital, health personnel, cultural diversity, physicians, women
Introduction
American society is becoming increasingly diverse, with projections estimating that there will be no racial majority group by the year 2035.(1) Despite this demographic change, it is clear that the American health professional workforce is less diverse than the population as a whole.(2) Diversity of identity is important for several reasons. First, there is evidence that patient-provider demographic concordance may facilitate communication(3) and improve patient satisfaction with care.(4) Second, providers from backgrounds traditionally underrepresented in medicine may be more likely to practice in underserved areas.(5) Third, in academic settings, the scholarship produced by diverse research teams may be of higher quality and more impactful than the work generated by less diverse teams.(6–8)
The Association of American Medical Colleges, which tracks physician diversity, has shown increasing representation of women in the physician workforce, with women currently comprising 36.7% of physicians.(9) In contrast, there is stagnating representation of black and Hispanic/Latino physicians, who in 2013 made up 4.2% and 4.6% of physicians but 13% and 17% of the general population, respectively.(9)
In critical care, knowledge about provider demographic diversity and representation is lacking. Why is intensivist diversity important? In addition to the reasons cited above, ICU physicians make critical decisions about life and death, including withdrawal of life-sustaining therapy and organ allocation. There is also evidence of racial/ethnic disparities in the care of critically ill patients.(10, 11) The Institute of Medicine (now the National Academy of Medicine) details two key theories why such disparities in treatment occur despite well intentioned providers.(12)
For these reasons, there is an ethical imperative to ensure that diverse backgrounds and values are represented in the critical care workforce. Fostering diversity may enhance our ability to engage and communicate with patients of all backgrounds and may improve the quality of scholarship relating to the care of the critically ill patient. The goal of the present study was to characterize racial, ethnic and gender diversity among critical care fellows to determine whether population-level trends in demographic change are also reflected in the emerging intensivist workforce that will feed into the larger group of critical care physicians.
Materials and Methods
This is a retrospective cross-sectional analysis of data reported by the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC). This study was deemed exempt by the University of Pennsylvania institutional review board.
Data sources
Demographic data about college graduates and medical school applicants, acceptees, matriculants, and graduates were obtained from AAMC published reports(13) and online data tables (https://www.aamc.org/initiatives/diversity/179816/facts_and_figures.html). Demographic data (race, ethnicity, and male or female gender) for U.S. critical care fellows was obtained from a joint report from the AMA and AAMC published annually in the Journal of the American Medical Association.(14–23)
Population of interest
"Critical care fellow" was defined as trainees in programs with any of the following designations: anesthesiology - critical care medicine; internal medicine - critical care medicine; internal medicine - pulmonary disease and critical care medicine (“pulmonary critical care”); pediatrics - pediatric critical care medicine; general surgery- surgical critical care. Most of these training programs are one year in length, with the exception of pulmonary critical care, which is generally 2–3 years in length. For the purposes of this analysis, all training programs were considered together to create a picture of demographic diversity amongst critical care fellows in any given year. We excluded emergency medicine and obstetrics and gynecology residency programs given low numbers of critical care fellows originating from these programs.(24) We also excluded combined internal medicine/emergency medicine/critical care training programs due to low numbers (<15 fellows in each of the ten years examined). Finally, we did not include neuro-critical care fellows because these fellowships are not ACGME-accredited and we were not able to find published data on neurocritical care fellow demographics.
“Underrepresented minority” was defined as race or ethnicity historically underrepresented in medicine, which includes black, Hispanic, American Indian, Alaskan Native, Native Hawaiian, and Pacific Islander. Due to small numbers (fewer than 20 fellows total in each of ten analytic years, 0.14–1.2%), American Indian, Alaskan Native, Native Hawaiian and Pacific Islander were grouped together (“AI/AN/NH/PI”). Given the lack of information about Asian subgroups (e.g. East Asian, Southeast Asian), we did not include Asian fellows in the definition of underrepresented minority. Housestaff whose race was designated as “Other” were excluded from analysis; these individuals were a mix of “other” and unknown, and largely included individuals identified as having Hispanic ethnicity but no racial designation.(25)
Annual demographic data for the United States population were obtained from United States Census Bureau. Population estimates from 2000 to 2010 were downloaded from the Population and Housing Estimates page of the Census Bureau (http://www.census.gov/popest/data/historical/2000s/vintage_2009/index.html). Population estimates for 2011 to 2014 were downloaded from the Census Bureau’s searchable American Fact Finder utility (American Community Survey searchable online databases, which are publicly available (http://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml).
Inclusion and exclusion criteria
For each demographic group, we determined trends in representation for both critical care fellowship programs and critical care pipeline specialties (anesthesiology, internal medicine, pediatrics, and surgery). We excluded emergency medicine and obstetrics and gynecology residency programs given low numbers of critical care fellows originating from these programs.(24) We excluded combined internal medicine/emergency medicine/critical care training programs due to low numbers (<15 fellows in each of the ten years examined).
Statistical analysis
To test whether changes in demographic parameters were statistically significant, two procedures were undertaken. First, logistic regression models were developed to examine the change in gender and ethnicity over time and across program types. Second, to account for the multiple categories in the race outcome, we employed a multinomial logistic regression model to examine changes in race over time and across program type. The race outcome variable was specified as: Asian, black, white, and AI/AN/NH/PI. An interaction term was introduced into models to examine whether temporal changes varied by fellowship program type; a second interaction term was introduced to examine whether temporal changes varied for critical care vs. non-critical care programs. The linearity assumption for time was evaluated with fractional polynomial analysis, which showed a linear model to be the best fitting model. The demographic trends of critical care fellows were compared qualitatively to United States population estimates via graphical representation. All statistical procedures were conducted with the software program Stata (version 13.0, StataCorp LC, College Station, Texas).
Results
Over the period from 2004 to 2014, there was an annual increase in the number of critical care fellows in training, with an overall 54.8% increase from 1,606 in 2004–05 to 2,475 in 2013–14. These fellows were in five different training programs: pulmonary critical care (60.4% of fellows in 2013–2014), pediatric critical care (17.2%), surgical critical care (8.6%), internal medicine/critical care (8.3%), and anesthesia critical care (5.6%).
Gender
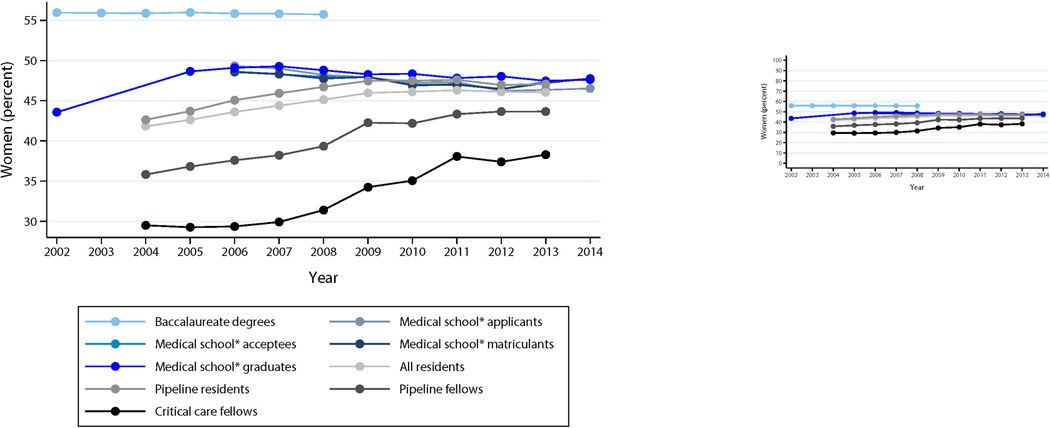
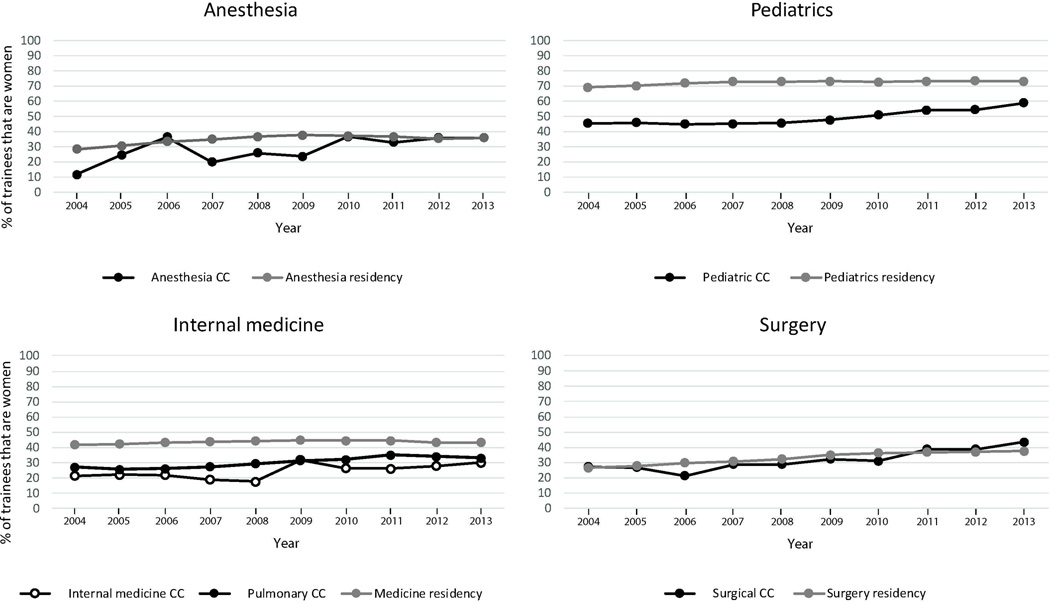
The number of women in critical care fellowship programs increased both in absolute number and in proportion every year from 2004–05 (29.5% of fellows) to 2013–14 (38.3% of fellows) (p<0.001) (Figure 1). This increase was seen in all fellowships and did not differ by program type (p=0.109 for interaction). At all time points, pediatric critical care fellowship programs had the highest proportion of female fellows (45.5% in 2004, 58.8% in 2013–14). The largest absolute increase in female fellows was seen in anesthesia critical care, with 11.6% (n=5) female fellows in 2004–05 and 36.0% (n=50) female fellows in 2013–14 (p<0.001). Comparison of the proportion of female critical care fellows in each program type with the proportion of female residents in each primary specialty showed that female representation reached parity in anesthesiology and surgery, but not in either of the internal medicine programs or in pediatrics (Figure 2). We observed the trend in female gender over time to differ when comparing critical care fellowships vs. non-critical training programs. Specifically, there was a greater increase in female gender in critical care fellowships vs. non-critical care training programs (p<0.001 for the interaction).
Figure 1. Representation of women in the critical care pipeline, 2004–2014.
“Pipeline” specialties are those contributing the majority of US critical care fellows: anesthesiology, internal medicine, pediatrics, and surgery.
Y axis is scaled for readability. Inset graph is scaled from 0 to 100 percent. Incomplete line graphs represent unavailable data.
*allopathic United States medical schools
Figure 2. Representation of women in critical care fellowships versus pipeline residency programs, 2004–2014.
CC: critical care
Race/Ethnicity
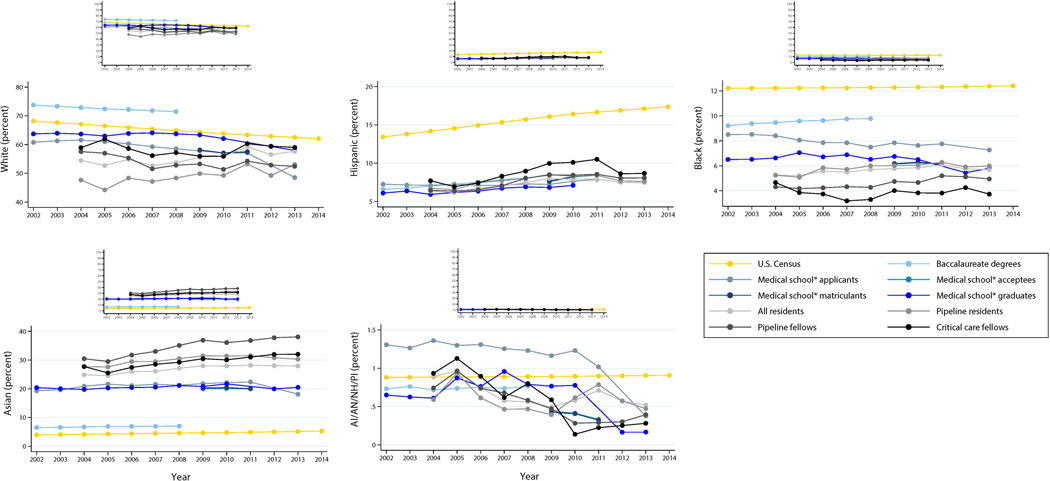
From 2004–05 to 2013–2014, the absolute number of black fellows increased each year while the percentage of black fellows decreased slightly from 5.1% (n=75) in 2004–05 to 3.9% (n=93) in 2013–14 (p=0.92 for change over time). The number of fellows from American Indian/Alaskan Native/Native Hawaiian/Pacific Islander groups decreased over the same period from 15 (1.0%) in 2004–05 to 7 (0.3%) in 2013–2014 (p<0.001). When compared to United States Census population estimates, the percentage of fellows from these two groups remained less than their representation in the population at large (Figure 3). Summing across all years of the study, underrepresented racial groups (black, American Indian, Alaskan Native, Native Hawaiian, or Pacific Islander) were somewhat less common in critical care fellowships (13.1%) versus non-critical care pipeline programs (15.1%) (p<0.001). The trend of these percentages was flat over time and did not differ for critical care vs. non-critical care programs.
Figure 3. Racial and ethnic representation in the critical care pipeline, 2004–2014.
AI/AN/NH/PI: Alaskan Native, American Indian, Native Hawaiian, Pacific Islander; “Pipeline” specialties are those contributing the majority of US critical care fellows: anesthesiology, internal medicine, pediatrics, and surgery.
Y axes are scaled for readability. Inset graphs are scaled from 0 to 100 percent. Incomplete line graphs represent unavailable data.
* allopathic United States medical schools
Asian fellows increased from 30.1% (n=446) of critical care fellows in 2004–05 to 33.8% (n=797) in 2013–14 (p<0.001). White fellows comprised 63.8% (n=947) of critical care fellows in 2004–05 and decreased to 62.1% (n=1469) in 2013–14 (p<0.001).
For Hispanic fellows, both the number and percentage increased from 124 (7.7%) in 2004–05 to 216 (8.4%) in 2013–14 (p=0.015). When compared to non-critical care training programs, the percentage of fellows identified as Hispanic was slightly higher in critical care fellowships (p=0.02). However, the change over time in Hispanic ethnicity was similar for critical care vs. non-critical care (p=0.07 for the interaction). When compared to United States Census population estimates, the percentage of fellows identified as Hispanic was lower than the proportion of the United States population identified as Hispanic (Figure 3).
Depending on year, fellows in the “Other/Unknown” category made up 4.1 to 11.5% of fellows, but the percentage of fellows identified as Other decreased over the 10-year period we examined.
Discussion
The demographic makeup of critical care fellowships has changed substantially over the past 10 years. Women make up an increasing proportion of critical care fellows from all disciplines, comprising more than 38% of all critical care fellows, up from 29.5% in 2004–05. However, racial and ethnic representation has not kept pace with changing population demographics. The percentage of fellows identified as Hispanic is increasing but remains less than half that of the proportion in the United States population. The proportion of fellows who are black has remained flat and is less than 4%, compared to 13% in the population. American Indians, Alaskan Natives, Native Hawaiians, and Pacific Islanders have seen their representation in critical care fellowships decrease over time.
These findings suggest that, similar to changes seen in medical student and practicing physician demographics, representation of women in critical care is steadily increasing. All of the specialties we examined have shown an increase in the number and proportion of women, and in two of these specialties (anesthesia and surgery), the proportion of women in critical care training programs equals or exceeds that in the primary specialty.
In contrast, the trends in racial and ethnic representation are less reassuring. Demographic groups that have historically been underrepresented remained so over the 10 years that we examined, with just a slight increase in the proportion of fellows identified as Hispanic. Interestingly, the already low proportion of black and AI/AN/NH/PI housestaff was still lower in critical care, suggesting that residents from these groups are matching into critical care at lower rates than others. Non-white physicians tend to select primary care specialties more than white physicians, but this would not explain differential findings for black and Hispanic housestaff. More research is needed to understand the degree to racial and ethnic underrepresentation is due to specialty choice versus ability to successfully match into critical care.
Changing population demographics offer a compelling argument for promoting diversity in the critical care workforce, but there are at least two other reasons to consider representation. First, racial and ethnic minorities tend to prefer and use(26, 27) more aggressive care at the end of life, leading to overrepresentation in the intensive care unit. Second, race has been associated with health system distrust,(28, 29) which may impact engagement with the healthcare team. A diverse workforce may improve cultural sensitivity of critical care teams and improve our ability to address longstanding disparities in healthcare and outcomes. The physician is just part of the multidisciplinary team needed to deliver optimal critical care, but understanding physician diversity is one step toward understanding diversity in the critical care team.
Further research is needed to explain the trends that we describe in this report. As the trends seen in female fellows suggest, demonstrable change in demographic trends is achievable over relatively short spans of time. The factors underpinning comparatively slower change in racial and ethnic representation in critical care fellows still need to be elucidated, but may include mentorship, access to critical care fellowship programs during residency, and representation in residency programs that tend to feed into critical care. It is important to note that lack of appreciable change in racial and ethnic physician demographics is not unique to critical care,(30) providing support for research in this area that transcends specialty type. Next steps include deepening our understanding of how prospective medical students, medical students, and residents make choices about their career path. This could involve interviews or surveys, ideally including people who remain in the pipeline to critical care and those who leave the pipeline. Additionally, it would be useful to characterize current residency program efforts to promote diversity and inclusion and to determine the effectiveness of different approaches.
The strengths of our analysis include examination of trends over time and inclusion of data from multiple specialties that feed into critical care. The multiple pathways to critical care, presence of multiple large, partially overlapping professional societies (including the American College of Chest Physicians, the American Thoracic Society, and the Society of Critical Care Medicine), and lack of a centralized data source about intensivists constitute a barrier to the compilation of comprehensive data about this field. Our approach circumvents these barriers and focuses on the newest members of the field, whose demographics are more amenable to change then are those of the established intensivist workforce.
Our study also has limitations. First, the data reported by the AMA and AAMC are based on fellowship program self-report, and may therefore contain inaccuracies. Second, there was a 90% program response rate, meaning that some trainees were missed. However, these programs contributed more than 96% of the trainees in ACGME-accredited training programs, which increases confidence in our findings. Third, a subset of fellows had a racial/ethnic designation of "Other/Unknown". These individuals may represent multiracial fellows or fellows opting not to disclose a racial or ethnic identity. Additional racial and ethnic categories may need to be added to AAMC reporting tools to enable adequate characterization of physicians in training. The number of fellows designated as “Other/Unknown” did decrease over time, which increases confidence that our findings are reflective of actual demographic trends. Fourth, there are many identity categories relevant to the practice of medicine, including socioeconomic class, family educational attainment, gender identity, sexual orientation, disability, and religion. We only examined male/female gender, race, and ethnicity, which have been consistently tracked demographic parameters. Fifth, not all critical care fellows go on to practice critical care medicine, and not all critical care is delivered by fellowship-trained intensivists, so our findings offer only a partial illustration of changes in the critical care workforce. However, given the evidence that intensivist-directed care may afford better outcomes,(31) it is important to understand the composition of this group of intensive care providers. Finally, optimal critical care is delivered by a multidisciplinary team; we did not address diversity in nurses, pharmacists and other critical care professionals who represent vital members of the critical care team. Additional research is needed to characterize diversity in these groups and to understand barriers to representation if they exist.
Conclusions
Women and racial/ethnic minorities underrepresented in medicine are also underrepresented in the emerging critical care physician workforce. The representation of women and Hispanics is increasing over time, while black, American Indian, Alaskan Native, Native Hawaiian and Pacific Islander representation is flat or decreasing. Further research is needed to explore the reasons underlying the persistent underrepresentation of certain racial and ethnic minorities in critical care fellowship programs.
Acknowledgments
Financial support: The work reported herein was unfunded. Meghan Lane-Fall receives research funding from the following groups: University of Pennsylvania Provost’s Office, University of Pennsylvania McCabe Fund, Anesthesia Patient Safety Foundation, and the Robert Wood Johnson Foundation.
Dr. Lane-Fall’s institution received funding from Anesthesia Patient Safety Foundation, Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program, and the National Institutes of Health Loan Repayment Program. She disclosed funding from honoraria for speaking as a visiting professor at the following institutions in the past 36 months: Vanderbilt University (February 2016), University of Alabama at Birmingham (November 2014), Cornell University (October 2014), Stanford University (September 2014), Massachusetts General Hospital (March 2014).
Footnotes
Location where work performed: University of Pennsylvania Perelman School of Medicine
Copyright form disclosure: The remaining authors have disclosed that they do not have any potential conflicts of interest.
Contributor Information
Meghan B. Lane-Fall, Department of Anesthesiology and Critical Care, Perelman School of Medicine; Center for Perioperative Outcomes Research and Transformation; Center for Healthcare Improvement and Patient Safety, Perelman School of Medicine; Leonard Davis Institute of Health Economics, University of Pennsylvania; Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, USA; Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program; NIH PRIDE Research in Implementation Science for Equity.
Todd A. Miano, Center for Clinical Epidemiology and Biostatistics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA; Department of Anesthesiology and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
Jaya Aysola, Department of Medicine, Division of General Internal Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA; Office of Diversity and Inclusion, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
John G. T. Augoustides, Department of Anesthesiology and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
References
- 1.Minority Population Growth - The New Boom: An Analysis of America's Changing Demographics. 2012 [Google Scholar]
- 2.Xierali IM, Castillo-Page L, Zhang K, et al. AM last page: The urgency of physician workforce diversity. Academic Medicine. 2014;89(8):1192. doi: 10.1097/ACM.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 3.Cooper LA, Roter DL, Johnson RL, et al. Patient-Centered Communication, Ratings of Care, and Concordance of Patient and Physician Race. Annals of Internal Medicine. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 4.Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? Journal of Health and Social Behavior. 2002;43(3):296–306. [PubMed] [Google Scholar]
- 5.Walker KO, Moreno G, Grumbach K. The association among specialty, race, ethnicity, and practice location among California physicians in diverse specialties. Journal of the National Medical Association. 2012;104(1–2):46–52. doi: 10.1016/s0027-9684(15)30126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freeman RB, Huang W. Collaborating With People Like Me: Ethnic co-authorship within the US. National Bureau of Economic Research Working Paper Series 2014;No. 19905(published as Richard B. Freeman, Wei Huang "Collaborating With People Like Me: Ethnic Co-authorship within the US," in Sarah Turner and William Kerr, organizers, "High-Skill Immigration" (University of Chicago Press) Journal of Labor Economics. 2014 [Google Scholar]
- 7.Cohen JJ, Gabriel BA, Terrell C. The Case For Diversity In The Health Care Workforce. Health Affairs. 2002;21(5):90–102. doi: 10.1377/hlthaff.21.5.90. [DOI] [PubMed] [Google Scholar]
- 8.Valantine HA, Collins FS. National Institutes of Health addresses the science of diversity. Proceedings of the National Academy of Sciences. 2015;112(40):12240–12242. doi: 10.1073/pnas.1515612112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nivet MA, Castillo-Page L. Diversity in the Physician Workforce: Facts & Figures 2014. Washington, D.C.: 2014. [Google Scholar]
- 10.Shaw JJ, Santry HP. Who Gets Early Tracheostomy?: Evidence of Unequal Treatment at 185 Academic Medical Centers. Chest. 2015;148(5):1242–1250. doi: 10.1378/chest.15-0576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elliott AM, Alexander SC, Mescher CA, et al. Differences in Physicians' Verbal and Nonverbal Communication With Black and White Patients at the End of Life. Journal of pain and symptom management. 2016;51(1):1–8. doi: 10.1016/j.jpainsymman.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smedley BD, Stith AY, Nelson AR. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 13.Castillo-Page L. Diversity in Medical Education: Facts & Figures 2012. Washington, D.C.: 2012. [Google Scholar]
- 14.Brotherton SE, Etzel SI. Graduate medical education, 2005–2006. JAMA : the journal of the American Medical Association. 2006;296(9):1154–1169. doi: 10.1001/jama.296.9.1154. [DOI] [PubMed] [Google Scholar]
- 15.Brotherton SE, Etzel SI. Graduate medical education, 2006–2007. JAMA : the journal of the American Medical Association. 2007;298(9):1081–1096. doi: 10.1001/jama.298.9.1081. [DOI] [PubMed] [Google Scholar]
- 16.Brotherton SE, Etzel SI. Graduate medical education, 2007–2008. JAMA : the journal of the American Medical Association. 2008;300(10):1228–1243. doi: 10.1001/jama.300.10.1228. [DOI] [PubMed] [Google Scholar]
- 17.Brotherton SE, Etzel SI. Graduate medical education, 2008–2009. JAMA - Journal of the American Medical Association. 2009;302(12):1357–1372. doi: 10.1001/jama.2009.1221. [DOI] [PubMed] [Google Scholar]
- 18.Brotherton SE, Etzel SI. Graduate medical education, 2009–2010. JAMA : the journal of the American Medical Association. 2010;304(11):1255–1270. doi: 10.1001/jama.2010.1273. [DOI] [PubMed] [Google Scholar]
- 19.Brotherton SE, Etzel SI. Graduate medical education, 2010–2011. JAMA : the journal of the American Medical Association. 2011;306(9):1015–1030. doi: 10.1001/jama.2011.1236. [DOI] [PubMed] [Google Scholar]
- 20.Brotherton SE, Etzel SI. Graduate medical education, 2011–2012. JAMA : the journal of the American Medical Association. 2012;308(21):2264–2279. doi: 10.1001/jama.2012.7913. [DOI] [PubMed] [Google Scholar]
- 21.Brotherton SE, Etzel SI. Graduate medical education, 2012–2013. JAMA : the journal of the American Medical Association. 2013;310(21):2328–2346. doi: 10.1001/jama.2013.278364. [DOI] [PubMed] [Google Scholar]
- 22.Brotherton SE, Etzel SI. GRaduate medical education, 2013–2014. JAMA. 2014;312(22):2427–2445. doi: 10.1001/jama.2014.12575. [DOI] [PubMed] [Google Scholar]
- 23.II. graduate medical education. JAMA. 2005;294(9):1129–1143. [PubMed] [Google Scholar]
- 24.Siegal EM, Dressler DD, Dichter JR, et al. Training a hospitalist workforce to address the intensivist shortage in American hospitals: a position paper from the Society of Hospital Medicine and the Society of Critical Care Medicine. Crit Care Med. 2012;40(6):1952–1956. doi: 10.1097/CCM.0b013e318258eef7. [DOI] [PubMed] [Google Scholar]
- 25.Brotherton SE. Explanation of "Other" designation in ACGME/JAMA resident reports. 2015 [Google Scholar]
- 26.Barnato AE, Berhane Z, Weissfeld LA, et al. Racial Variation in End-of-Life Intensive Care Use: A Race or Hospital Effect? Health Services Research. 2006;41(6):2219–2237. doi: 10.1111/j.1475-6773.2006.00598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miesfeldt S, Murray K, Lucas L, et al. Association of Age, Gender, and Race with Intensity of End-of-Life Care for Medicare Beneficiaries with Cancer. Journal of Palliative Medicine. 2012;15(5):548–554. doi: 10.1089/jpm.2011.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson KS, Kuchibhatla M, Tulsky JA. What explains racial differences in the use of advance directives and attitudes toward hospice care? Journal of the American Geriatrics Society. 2008;56(10):1953–1958. doi: 10.1111/j.1532-5415.2008.01919.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Halbert C, Armstrong K, Gandy OH, et al. Racial differences in trust in health care providers. Archives of Internal Medicine. 2006;166(8):896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- 30.Chapman CH, Hwang WT, Deville C. Diversity based on race, ethnicity, and sex, of the US radiation oncology physician workforce. Int J Radiat Oncol Biol Phys. 2013;85(4):912–918. doi: 10.1016/j.ijrobp.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 31.Pronovost PJ, Angus DC, Dorman T, et al. Physician staffing patterns and clinical outcomes in critically ill patients: A systematic review. Journal of the American Medical Association. 2002;288(17):2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]