Abstract
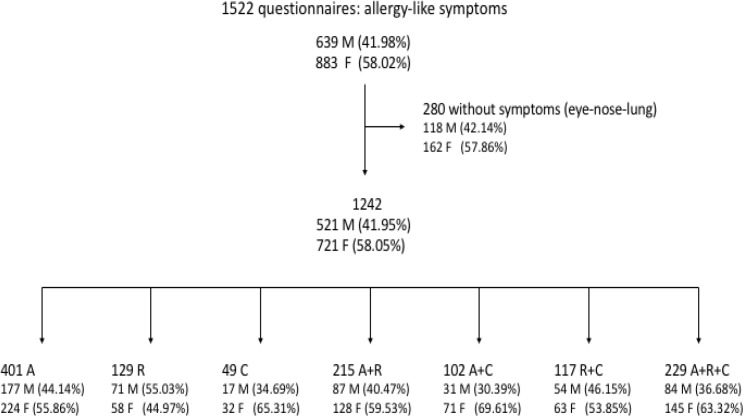
Here, we report on the prevalence of allergic conjunctivitis and positive skin prick test (SPT) results in relation to respiratory allergic conditions among patients with symptoms of allergies at a respiratory outpatient clinic. A questionnaire survey of symptoms (i.e., asthma-like, rhinitis, and conjunctivitis symptoms) involving 1522 patients was carried out. The responses of 1242 patients indicated that they had allergic conjunctivitis, asthma, rhinitis, or a combination of these conditions, and 869 of these patients underwent SPTs that assessed responses to 40 allergens.
Allergic conjunctivitis was found to be very common (40%, 497 out of 1242 patients) among those with symptoms of allergies. Conjunctivitis was slightly more common among women, while rhinitis was more common among men. Patients with both conjunctivitis and rhinitis were more likely to undergo SPTs, and they had a higher rate of positive SPTs. The coexistence of two or more comorbidities increased the risk of having an immunoglobulin E (IgE)-mediated allergy (based on the SPT results) compared to having each of the conditions alone. In conclusion, allergic conjunctivitis can occur either alone or with asthma and/or rhinitis. It is not always accompanied by rhinitis, but the coexistence of these conditions was the strongest indicator of IgE-mediated allergies.
Key Words: Allergic Conjunctivitis, Asthma, Allergic Rhinitis, Skin Prick Tests, Allergic Comorbidities
INTRODUCTION
In the past decade, guidelines regarding the management of asthma (1) and allergic rhinitis (2) have been published separately. However, the “one airway, one disease” idea and the similar mechanisms of allergic inflammation that exists between asthma and allergic rhinitis resulted in the creation of a new set of guidelines concerning both comorbidities. These guidelines were prepared by an initiative called Allergic Rhinitis and its Impact on Asthma (ARIA), which works with the World Health Organization. Nevertheless, these guidelines do not include allergic conjunctivitis as an allergic comorbidity. Allergic conjunctivitis with allergic rhinitis is often referred to as “allergic rhino-conjunctivitis” because of the extremely frequent coexistence of these conditions. Moreover, multicenter studies such as the International Study of Asthma and Allergies in Childhood (ISAAC) (3,4) and the National Health And Nutrition Examination Survey (NHANES) (5) refer to concurrent allergic conditions of the nose and eyes as “allergic rhino-conjunctivitis.” The term “hay fever” is also commonly used, and it refers to a group of symptoms that occur in sensitized individuals due to seasonal pollen exposure, such as sneezing and nasal itchiness, discharge, and congestion, which can be accompanied by allergic ocular symptoms.
The extent to which allergic conjunctivitis is a part of the “asthma–allergic rhinitis” entity has not been evaluated rigorously and, consequently, this issue has not been sufficiently addressed by the relevant guidelines.
The eyes are rarely the only organs that exhibit immediate allergic-type responses (almost 10% of patients with allergies have solely ocular symptoms). Often, patients with ocular allergies have coexisting atopic manifestations such as rhinitis, asthma, urticaria, or eczema. Despite this, ocular signs and symptoms can sometimes be the first and most obvious feature of a broader allergic response that prompts patients to visit their physicians (6).
It is estimated that, in the USA, allergies involving the eyes, nose, and throat affect 18.3% of the general population (7). Moreover, a study in Sweden reported that the prevalence of allergic conjunctivitis was 19% among 12–13-year-old schoolchildren, with 92% of those with allergic conjunctivitis having allergic rhinitis (8). In general practice, about 6% of consultations are for inflamed or red eyes, 35% of which are caused by allergies, according to a survey of ophthalmologists and general practitioners in nine countries in Eastern Europe and the Middle East (9). Ocular allergies account for 10% of the ophthalmology outpatient visits in the Asia Pacific region, and although red eye is a very uncommon primary symptom for allergists, it commonly accompanies other allergy symptoms, occurring in around 25% of allergists’ patients (10). Among patients with seasonal and perennial allergic conjunctivitis, ocular allergy symptoms are twice as common as nasal symptoms alone (11).
Taking into consideration all the above, it could easily be concluded that the prevalence of ocular allergies is underestimated and, hence, that ocular allergies are underdiagnosed and undertreated. This study is a continuation of a study that we published in 2013, which evaluated the prevalence of conjunctivitis and the most common allergens in Northern Greece (6). The objective of the present study was to retrospectively evaluate the prevalence of allergic conjunctivitis and positive skin prick test (SPT) results in relation to allergic respiratory conditions among patients with symptoms of allergies at a respiratory outpatient clinic. In addition, we determined the gender distribution in groups of patients categorized according to their symptoms (i.e., asthma-like symptoms, rhinitis, and conjunctivitis). Moreover, we determined which combination of conditions was the strongest indicator of immunoglobulin E (IgE)-mediated allergies (as indicated by positive SPTs).
Our objective was to encourage ophthalmologists, allergists, pulmonologists, and general practitioners to recognize conjunctivitis as a frequent comorbidity in patients with allergies.
METHODS
This study is a retrospective study that involved analyzing data from the electronic archives of an outpatient respiratory clinic in Northern Greece. None of the personal information was identifiable and no invasive procedures were conducted. The study was approved by the Ethics Committee of the Aristotle University of Thessaloniki, Greece.
The study was based on 10,000 patients with respiratory symptoms who had been referred during a 14-year period (1996–2010). Of these patients, 1522 who were suspected of having an allergic condition (such as asthma, rhinitis, or conjunctivitis, based on their clinical history and an examination) filled in a questionnaire that was designed for the evaluation of allergic symptoms and the subsequent diagnosis of allergic conditions. The questionnaire contains 200 questions and is used by the Pulmonary Department of the Aristotle University of Thessaloniki. It enables the collection of information on personal characteristics (such as age and profession), symptoms of the upper and lower respiratory systems and the eye (i.e., wheezing, dyspnea, cough, sputum, rhinorrhea, sneezing, and runny, itchy, and red eyes), and the time of year and time of the day during which these symptoms appear. There are also questions concerning symptoms caused by a variety of allergens (i.e., dust, pets, particular foods, drugs, cold air, and exercise) as well as the patient’s medical history and previous and current medication use. The screening question on asthma-like symptoms, rhinitis, and conjunctivitis was as follows: Do you have or have you had (during last year) any of the following symptoms: (A) dyspnea, wheezing, noisy breathing, or asthma; (B) a runny nose or allergic sneezing; and (C) watery, itchy, or red eyes?
Based on their responses, the patients were categorized into seven groups, as follows:
Group A: Patients with asthma only [A – R – C]
Group B: Patients with rhinitis only [R – A – C]
Group C: Patients with conjunctivitis only [C – A – R]
Group D: Patients with asthma and rhinitis but not conjunctivitis [A + R – C]
Group E: Patients with asthma and conjunctivitis but not rhinitis [A + C – R]
Group F: Patients with rhinitis and conjunctivitis but not asthma [R + C – A]
Group G: Patients with all three conditions [A + R + C]
The patients completed the questionnaires with the help of an experienced nurse. Subsequently, SPTs were recommended to all the patients and performed (by the same experienced doctor) after obtaining consent, as recommended by the European Academy of Allergology and Clinical Immunology (12) and the US Joint Council of Allergy Asthma and Immunology (13,14). It is important to note that undergoing an SPT was associated with a patient fee. Only 70% (869 out of 1242) of the patients consented to undergo SPTs. In our earlier study (6), positive reactions to any of the eight main allergens (cypress, Parietaria officinalis, European olive, dust mite mix, Alternaria spp., pet dander [dog and cat], and grass mix) were analyzed by patient group. The patients who underwent the SPTs had not been on any oral antihistamine and/or cortisone medications for at least a week prior to the SPTs.
The statistical analysis carried out using Statistical Package for the Social Sciences (SPSS) version 12 (SPSS Inc., Chicago, IL, USA). Chi-square tests used to determine whether the gender-related differences in the proportions of patients in each patient group were statistically significant. These tests also used to determine whether the gender-related and patient group-related differences in the proportions of patients who underwent SPTs and had positive SPTs results were significant. P values <0.05 were considered statistically significant.
RESULTS
Of the 1522 patients (636 men and 883 women) who completed the questionnaire, 280 reported that they had not experienced any of the assessed symptoms, so only the remaining 1242 (521 men and 721 women) were categorized into the patient groups described in the previous section.
Out of the 1242 patients with allergies, 497 (40%) were assessed as having conjunctivitis. There were more women with conjunctivitis than men (311 women and 186 men) (Figure 1). Among the patients with both asthma and conjunctivitis (group E), there were significantly more women than men (p=0.018). In addition, among the patients with conjunctivitis only (group C), there was a non-significant predominance of women (p=0.367), and among those with all three comorbidities (group G), there was also a non-significant preponderance of women (p=0.086). Men were significantly more common than women only among the patients with rhinitis only (group B) (p=0.002).
Figure 1.
Number of patients who completed the questionnaires and gender distribution by allergy-related symptoms. (M: men, W: women, A: asthma, R: rhinitis, C: conjunctivitis
Men underwent SPTs more often than women (75% vs. 67%), with a significant difference between the genders in all patient groups (p=0.003). The patients who had conjunctivitis only (group C) and those who had rhinitis and conjunctivitis but not asthma (group F) underwent SPTs at significantly higher rates than those in all the other patient groups (p=0.005 and p=0.001, respectively). As shown in Table 1, around 70% of all the patients who underwent SPTs were positive for at least one of the 40 allergens tested. The patients who had rhinitis and conjunctivitis (group F) and those who had all three comorbidities (group G) had significantly higher rates of positive SPTs compared to those in all the other patient groups (p=0.005 and p=0.001, respectively). With respect to gender distribution, for men, groups C, E, F and G (conjunctivitis alone or accompanied by other(s) comorbidities), had higher proportions of positive SPTs. Men were more likely to undergo SPTs than women in all groups (p=0.003) as well as had higher proportions of positive SPTs in all the patient groups compared to women (p=0.003).
Table 1.
Frequency of patients with positive or negative SPTs among all the patients with allergy-related symptoms (SPT: skin prick test
| Allergic symptoms groups | Total No. |
Performed SPTs
No/percentage (%) |
Positive SPTs
No/percentage (%) |
Negative SPTs
No/Percentage (%) |
|---|---|---|---|---|
| A | 401 | 242 (60.35%) | 149 (61.57%) | 93 (38.43%) |
| B | 129 | 97 (75.19%) | 65 (67.01%) | 32 (32.99%) |
| C | 49 | 41 (83.67%) | 23 (56.10%) | 18 (43.90%) |
| D | 215 | 160 (74.42%) | 108 (67.50%) | 52 (32.50%) |
| E | 102 | 60 (58.82%) | 43 (71.67%) | 17 (28.33%) |
| F | 117 | 98 (83.76%) | 81 (82.65%) | 17 (17.35%) |
| G | 229 | 171 (74.67%) | 137 (80.12%) | 34 (19.88%) |
| Total | 1242 | 869 (69.97%) | 606 (69.74%) | 263 (30.26%) |
DISCUSSION
As the study related conjunctivitis to respiratory allergies, it was rather surprising to note that 49 out of the 1242 patients who reported having allergic symptoms had conjunctivitis only (group C). This could be attributable to the patients’ perception that, for a minor case of conjunctivitis that is likely to be due to an allergy, the major problem could originate in the respiratory tract. A high percentage of patients (100% of the men and 75% of the women) with conjunctivitis only (group C) decided to proceed with the SPTs. These patients, along with those with rhinitis and conjunctivitis (group F) underwent SPTs at significantly higher rates than those in all the other patient groups (Group C, p=0.005; Group F, p=0.001). This may have occurred because these patients had particularly troublesome symptoms or the symptoms may have been more strongly indicative an allergy. The fact that 65% of the men and only 50% of the women had positive SPTs (in Group C) shows that the men may have had a better perception of their condition and/or that, in some cases the women’s ocular symptoms may have been related to mechanical irritation caused by the use of cosmetics.
Another important observation is that the proportion of patients with rhinitis and conjunctivitis (group F) who underwent SPTs (84%) was higher than those in the other patient groups, and these patients also had a higher rate of positive SPTs (83%) compared to those in the other groups. The percentages were also higher for the patients who had all three comorbidities (group G), at 75% and 80%, respectively, but the differences were not significant (p=0.98).
The patient group with the third highest rate of positive SPTs was the patients with conjunctivitis and asthma without rhinitis (group E). The results indicate that when conjunctivitis coexists with asthma without rhinitis (group E), there appears to be a stronger indication of IgE-mediated allergy than when asthma coexists with rhinitis without conjunctivitis (group D), especially in men. For men, the coexistence of conjunctivitis with either of the other conditions accompanied by a higher probability of IgE-mediated allergy. The presence of asthma alone or conjunctivitis alone (groups A and C, respectively) had the poorest prognostic value for positive SPTs for both men and women.
The very high proportions of patients with both rhinitis and conjunctivitis (group F) and those with all three comorbidities (group G) who underwent SPTs indicates that the patients’ perception that there was an allergic background to their disease was stronger in groups F and G compared to among those with every other combination of comorbidities investigated.
In addition, men were significantly more likely to undergo SPTs than women in all the patient groups (p=0.003). This may be attributable to socioeconomic factors, given that each patient incurred a fee when they underwent the SPT. As a result, only 70% of the patients (75% of the men and 67% of the women) underwent SPTs (despite the fact that the doctor recommended to each of them that they undergo the SPT). Lastly, men had considerably and statistically significantly higher proportions of positive SPTs in all the patient groups compared to women (p=0.003).
There are no data concerning the prevalence of allergic conjunctivitis in adults with asthma in previous studies such as the ARIA review (3,15). Besides our previous study (6), the only studies about allergic conjunctivitis alone were conducted in pediatric populations (16-18) except for one, which involved young Italian men (19). As a result, it is difficult to estimate the proportion of individuals who have both rhinitis and conjunctivitis. This is likely to be because conjunctivitis symptoms are rarely considered to be a major issue, and they are presumably not spontaneously reported by patients with rhinitis and/or asthma in medical consultations or in questionnaire-based epidemiologic studies such as the ISAAC (4) or the European Community Respiratory Health Survey (ECRHS) (5). In keeping with the above hypothesis, the ARIA review (3) highlighted that the association between rhinitis and conjunctivitis maybe underestimated in epidemiologic studies and, presumably, the same is true for asthma and conjunctivitis.
In daily clinical practice, diagnostic and therapeutic procedures generally focus on the most predominant condition. Hence, doctors usually neglect to ask patients about symptoms concerning organs that are not involved in the predominant condition (such as the eyes). This occurs despite the evidence that atopic conditions frequently occur together. Consequently, nose, lung, skin, and eye specialists often fail to treat patients holistically and, instead, treat only the system they specialize in. Our study clearly indicates that patients with respiratory symptoms usually have conjunctivitis, and among these patients, there is a greater proportion with positive SPTs (compared to those in other the patient groups). More studies on whether patients with conjunctivitis symptoms as their main allergy symptoms also have a high risk of other allergic conditions are required.
A potential limitation of the study is that it did not involve a sample from the general population, and instead focused on patients who were referred to an outpatient respiratory clinic (not to an allergist or an ophthalmologist). Furthermore, the screening questions referred to general asthma-like symptoms. Another consideration is that the questionnaire had a question on having watery, itchy, or red eyes and a separate question on rhinitis symptoms. As explained earlier in the Discussion, other studies have dealt with the symptoms of itchy and watery eyes and the symptoms of rhinitis together, as rhino-conjunctivitis. Finally, it is possible that some of the ocular symptoms could have been related to other causes of red eyes.
In conclusion, conjunctivitis is a very frequent comorbidity among patients with respiratory and allergy symptoms. Conjunctivitis can occur without other symptoms of allergies, and coexistence with rhinitis is certainly not a prerequisite. Conjunctivitis is a separate entity from rhinitis, and, according to our study, their coexistence appears to be less common than is indicated in previous studies, in which the term “rhino-conjunctivitis” has often been used (4,5). On the other hand, our results show that the coexistence of two or more potentially allergic comorbidities is associated with an increased probability of having positive SPTs (indicating IgE-mediated allergies) compared to each condition alone.
DISCLOSURE
Conflict of interest
None declared.
All the aforementioned authors met the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have provided approval for the revised manuscript to be published.
References
- 1.Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2015. Page 22-78.
- 2.Bousquet J, Reid J, van Weel C, Baena Cagnani C, Canonica GW, Demoly P, Denburg J, Fokkens WJ, Grouse L, Mullol K, Ohta K, Schermer T, Valovirta E, Zhong N, Zuberbier T. Allergic rhinitis management pocket reference 2008. Allergy. 2008 Aug;63(8):990–6. doi: 10.1111/j.1398-9995.2008.01642.x. PMID: 18691301. [DOI] [PubMed] [Google Scholar]
- 3.Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, van Wijk RG, Ohta K, Zuberbier T, Schünemann HJ Global Allergy and Asthma European Network; Grading of Recommendations Assessment Development and Evaluation Working Group. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010 Sep;126(3):466–76. doi: 10.1016/j.jaci.2010.06.047. PMID: 20816182. [DOI] [PubMed] [Google Scholar]
- 4.Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet. 1998 Apr ;351(9111):1225–32. PMID: 9643741. [PubMed] [Google Scholar]
- 5.[database on the Internet] [(2017, Jaunary 15)]. Retrieved from https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/documents.aspx?BeginYear=2005.
- 6.Almaliotis D, Michailopoulos P, Gioulekas D, Giouleka P, Papakosta D, Siempis T, Karampatakis V. Allergic conjunctivitis and the most common allergens in Northern Greece. World Allergy Organ J. 2013 Jul 16;6(1) doi: 10.1186/1939-4551-6-12. PMID: 23866689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nathan RA, Meltzer EO, Seiner JC, Storms W. Prevalence of allergic rhinitis in the United States. Journal of allergy and clinical immunology. 1997 Jun 1;99(6):S808–14. [PubMed] [Google Scholar]
- 8.Hesselmar B, Aberg B, Eriksson B, Aberg N. Allergic rhinoconjunctivitis, eczema, and sensitization in two areas with differing climates. Pediatr Allergy Immunol. 2001 Aug;12(4):208–15. doi: 10.1034/j.1399-3038.2001.012004208.x. PMID: 11555318. [DOI] [PubMed] [Google Scholar]
- 9.Petricek I, Prost M, Popova A. The differential diagnosis of red eye: a survey of medical practitioners from Eastern Europe and the Middle East. Ophthalmologica. 2006;220(4):229–37. doi: 10.1159/000093076. PubMed PMID: 16785753. [DOI] [PubMed] [Google Scholar]
- 10.Katelaris CH. Ocular allergy in the Asia Pacific region. Asia Pac Allergy. 2011 Oct;1(3):108–14. doi: 10.5415/apallergy.2011.1.3.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bielory L. Ocular allergy overview. Immunol Allergy Clin North Am. 2008 Feb;28(1):1–23. doi: 10.1016/j.iac.2007.12.011. PMID: 18282543. [DOI] [PubMed] [Google Scholar]
- 12.Position paper: Allergen standardization, skin tests. The European Academy of Allergology and Clinical Immunology. Allergy. 1993;48(14 Suppl):48–82. PMID: 8342740. [PubMed] [Google Scholar]
- 13.Bernstein IL, Storms WW. Practice parameters for allergy diagnostic testing Joint Task Force on Practice Parameters for the Diagnosis and Treatment of Asthma The American Academy of Allergy, Asthma and Immunology and the American College of Allergy, Asthma and Immunology. Ann Allergy Asthma Immunol. 1995 Dec;75(6 Pt 2):543–625. [PubMed] [Google Scholar]
- 14.Allergen skin testing; Board of Directors. American Academy of Allergy and Immunology. J Allergy Clin Immunol. 1993 Nov;92(5):636–7. PMID: 8227853. [PubMed] [Google Scholar]
- 15.Riedi CA, Rosario NA. Prevalence of allergic conjunctivitis: a missed opportunity? Allergy. 2010 Jan;65(1):131–2. doi: 10.1111/j.1398-9995.2009.02100.x. PMID: 20078506. [DOI] [PubMed] [Google Scholar]
- 16.Gradman J, Wolthers OD. Allergic conjunctivitis in children with asthma, rhinitis and eczema in a secondary outpatient clinic. Pediatr Allergy Immunol. 2006 Nov;17(7):524–6. doi: 10.1111/j.1399-3038.2006.00429.x. PMID: 17014628. [DOI] [PubMed] [Google Scholar]
- 17.Singla JP, Parashar Y. Prevalence of allergic rhinitis, allergic conjunctivitis and atopic dermatitis in children with recurrent wheeze. Indian Pediatr. 2009 Mar;46(3) PMID: 19346577. [PubMed] [Google Scholar]
- 18.Baig R, Ali AW, Ali T, Ali A, Shah MN, Sarfaraz A, Ahmad K. Prevalence of allergic conjunctivitis in school children of Karachi. J Pak Med Assoc. 2010 May;60(5):371–3. PMID: 20527610. [PubMed] [Google Scholar]
- 19.Ciprandi G, Vizzaccaro A, Cirillo I, Cerqueti P, Canonica GW. Prevalence of allergic conjunctivitis in Italian young men. Allergy. 1996 Jul;51(7):517–8. doi: 10.1111/j.1398-9995.1996.tb04662.x. PMID: 8863932. [DOI] [PubMed] [Google Scholar]