Abstract
Background and Purpose
The detection of aquaporin 4-IgG (AQP4-IgG) is now a critical diagnostic criterion for neuromyelitis optica spectrum disorder (NMOSD). To evaluate the serostatus of NMOSD patients based on the 2015 new diagnostic criteria using a new in-house cell-based assay (CBA).
Methods
We generated a stable cell line using internal ribosome entry site-containing bicistronic vectors, which allow the simultaneous expression of two proteins (AQP4 and green fluorescent protein) separately from the same RNA transcript. We performed in-house CBA using serum from 386 patients: 178 NMOSD patients diagnosed according to the new diagnostic criteria without AQP4-IgG, 63 high risk NMOSD patients presenting 1 of the 6 core clinical characteristics of NMOSD but not fulfilling dissemination in space, and 145 patients with other neurological diseases, including 66 with multiple sclerosis. The serostatus of 111 definite and high risk NMOSD patients were also tested using a commercial CBA kit with identical serum to evaluate the correlation between the 2 methods. All assays were performed by two independent and blinded investigators.
Results
Our in-house assay yielded a specificity of 100% and sensitivities of 80% (142 of 178) and 76% (48 of 63) when detecting definite- and high risk NMOSD patients, respectively. The comparison with the commercial CBA kit revealed a correlation for 102 of the 111 patients: no correlation was present in 7 patients who were seronegative using the commercial method but seropositive using the in-house method, and in 2 patients who were seropositive using the commercial method but seronegative using the in-house method.
Conclusions
These results demonstrate that our in-house CBA is a highly specific and sensitive method for detecting AQP4-IgG in NMOSD patients.
Keywords: neuromyelitis optica spectrum disorder, aquaporin 4, aquaporin 4-IgG, cell-based immunofluorescence assay
INTRODUCTION
Neuromyelitis optica (NMO) is a relapsing autoimmune disease of the central nervous system that predominantly affects the optic nerves and spinal cord. The discovery of an autoantibody targeting water channel aquaporin 4 (AQP4), termed AQP4-IgG,1,2 has led to major advances in the understanding of NMO as a distinct disease entity with a fundamentally different etiology from that of multiple sclerosis (MS).3 Several studies have yielded evidence of an involvement of AQP4 in the pathogenesis of NMO.4,5,6 Based on determination of the highly specific AQP4-IgG, NMO has been recognized as a spectrum disease with a more-diverse clinical presentation that is not limited to optic neuritis or myelitis, and the new nomenclature of neuromyelitis optica spectrum disorder (NMOSD) is now widely used. The detection of AQP4-IgG allows the early diagnosis of NMOSD even in patients who experience a single attack with the core clinical characteristics of NMOSD,7 and thus assaying AQP4-IgG is now considered an integral step in the diagnosis of NMOSD.
Considering devastating impact of NMOSD relapses, early accurate diagnosis of NMOSD is crucial, and thus there is an increased demand for an assay that has high sensitivity and specificity in detecting AQP4-IgG in patients. Several assays with varying sensitivities and specificities have been developed over the years, such as the following types of cell-based assays (CBAs) involving live or fixed cells: cell-based indirect immunofluorescence assay and cell-based flow cytometry, enzyme-linked immunosorbent assay, and tissue-based indirect immunofluorescence and fluorescence im-munoprecipitation assays. Among these assays, those based on AQP4-transfected cell lines have yielded the highest sensitivity and specificity.8
We built an in-house CBA using the M23-AQP4-transfected human embryonic kidney 293 (HEK293) cell line, generated by an internal ribosome entry site (IRES) vector. We aimed to evaluate the sensitivity and specificity of this assay for detecting AQP4-IgG in NMOSD patients based on the 2015 new diagnostic criteria and in patients with other neurological diseases including MS. We also aimed to confirm the reliability of the procedure by comparing results with those obtained using a commercial anti-AQP4 indirect immunofluorescence assay (referred to as the commercial CBA henceforth).
METHODS
Patients
Serum samples from 386 patients were tested in duplicate, comprising 178 samples from patients who fulfilled the 2015 diagnostic criteria for NMOSD without the AQP4 serostatus (referred to as definite NMOSD here), 63 samples from patients with 1 of the 6 core clinical characteristics of NMOSD but not fulfilling dissemination in space (referred to as a high risk NMOSD here), and 145 samples from patients with other neurological diseases, including 68 samples from MS patients who the fulfilled 2010 McDonald's criteria.9 The demographic and clinical characteristics of the NMOSD and MS patients are summarized in Table 1. The patients with other neurological diseases are grouped and summarized in Table 2. All patients provided written informed consent, and this study was approved by our institutional review board.
Table 1. Demographic characteristics of the NMOSD and MS patients.
| Demographic | Definite NMOSD (n=178) | High risk NMOSD (n=63) | MS (n=68) |
|---|---|---|---|
| Men:women (n:n) | 20:158 | 13:50 | 20:48 |
| Onset age (years, mean±SD) | 31.8±11.5 | 40.4±11.0 | 27.7±9.2 |
| Disease duration (years, mean±SD) | 22.0±5.6 | 6.7±5.7 | 5.9±4.7 |
| EDSS score (median) | 3.0 | 2.5 | 1.5 |
EDSS: Kurtzke's Expanded Disability Status Scale, MS: multiple sclerosis, NMOSD: neuromyelitis optica spectrum disorder, SD: standard deviation.
Table 2. Patients with other neurological diseases (ONDs) (n=145).
| Disease | n |
|---|---|
| Multiple sclerosis | 68 |
| Idiopathic isolated myelitis | 29 |
| Optic neuritis | 5 |
| Isolated brain demyelination | 19 |
| Unknown central nervous system inflammation (DIS+) | 5 |
| Non inflammatory neurological disease | 19 |
DIS: dissemination in space.
Generation of M23-AQP4-HEK293 cells
M23-AQP4 cDNA was PCR-amplified from pET15b-M23-AQP4 plasmid and cloned into the NheI and SacI sites of the pIRES2-EGFP vector (Clontech, Mountain View, CA, USA). The cloned M23-AQP4 plasmid or the empty vector plasmid was transfected into HEK293 cells (ATCC, Manassas, VA, USA) using Lipofectamine 2000 reagent (Invitrogen, Waltham, MA, USA). After 48 hours, the cells were split into the medium containing 2 mg/mL G418 (Invitrogen). The G418-resistant cells were isolated after 2 weeks and then further cloned by limiting dilution. The individual stable transfectant clones were screened for green fluorescent protein (GFP) expression using flow cytometry. M23-AQP4 protein expression in GFP-positive cells was confirmed by Western blotting with anti-AQP4 antibody (Abcam, Cambridge, UK). The following primer sequences were used for the PCR: forward, 5′-GGT ACC GCT AGC GCC ACC ATG GTG GCT TTC AAA GGG-3′; reverse, 5′-TCT AGA GAG CTC TCA TAC TGA AGA CAA TAC-3′. All of the sequences were confirmed by automatic sequencing.
Cell-based indirect immunofluorescence assay
Stably transfected HEK293 cells expressing GFP-M23-AQP4 fusion protein or HEK293 cells stably transfected with empty vector were seeded into eight-well chamber slides (SPL Life Science, Pocheon, Korea), and incubated in 5% CO2 at 37℃ overnight. Culture medium was removed by gentle suction and the cells were washed three times with phosphate-buffered saline (PBS). Cells were blocked with blocking buffer (PBS containing 5% bovine serum albumin) at room temperature (RT) for 1 hour. Sera were diluted 1:20 using blocking buffer. Diluted serum (100 µL) was added to each well and incubated at RT for 2 hours. The cells were washed three times with PBS as described above, and then fixed with 2% paraformaldehyde at RT for 45 min. After washing with PBS, the cells were incubated with goat anti-human IgG conjugated with Alexa-594 (Jackson Immunoresearch, West Grove, PA, USA; diluted 1:2,000 with PBS) for 1 hour at RT in the dark. The cells were then washed three times before being mounted with VECTASHIELD® antifade reagent with DAPI (Vector Laboratories, Burlingame, CA, USA) and covered with coverslips. Each experiment was performed in duplicate, and the green and red fluorescence on the cell membranes was examined by two investigators (K.G.Y. and K.Y.S.) who were blinded to the clinical and laboratory information of the studied patients, under a fluorescence microscope (Zeiss, Oberkochen, Germany). The presence of only green fluorescence was considered to indicate negativity for AQP4 antibodies and the presence of red fluorescence that was not colocalized with green fluorescence was considered to indicate nonspecific binding, and hence negative for AQP4 antibodies. The presence of red fluorescence on cell membranes and green fluorescence in the cytosol was considered to indicate positivity for AQP4-IgG.
Statistical analysis
The following calculations were performed as part of the statistical analysis in this study:
1) Sensitivity was calculated as [true positives/(true positives+ false negatives)].
2) Specificity was calculated at [true negatives/(true negatives+ false positives)].
3) Accuracy was calculated as [(true positives+true negatives)/total samples]×100.
4) The 95% confidence interval (CI) for sensitivity was calculated as √[(1-sensitivity)×sensitivity/(number of tests)]× 1.96.
5) The 95% CI for specificity was calculated as √[(1-specificity)× specificity/(number of tests)]×1.96.
RESULTS
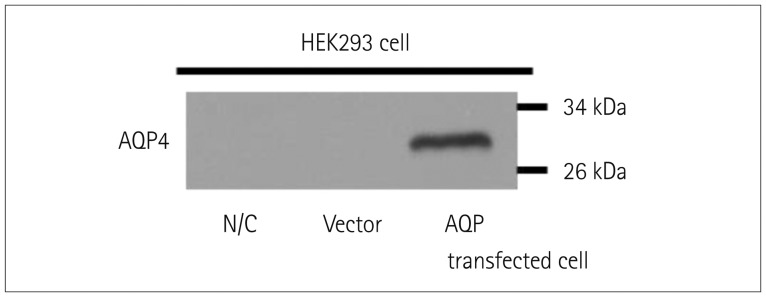
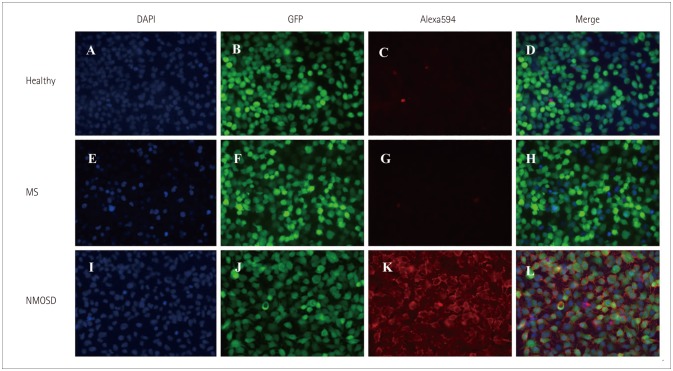
HEK293 cells transfected with M23-AQP4 were used in the in-house CBA, with successful transfection confirmed using Western blotting (Fig. 1). The widely used CBA method was adopted, and fluorescence levels were measured using fluorescence microscopy. Green fluorescence in the cytosol was observed in AQP4-transfected cells, and when patient serum that contained AQP4-IgG was added, red fluorescence was observed through the cell membranes (Fig. 2). If the patient serum did not contain AQP4-IgG, no red fluorescence was observed (Fig. 2).
Fig. 1. AQP4 overexpression in HEK293 cells using the AQP4-IRES2-EGFP vector. Western blot data confirming the successful transfection of AQP4. Lanes containing either untransfected HEK293 cells or HEK293 cells transfected with the IRES2-EGFP vector only do not show any bands. The lane containing lysate of HEK293 cells transfected with the M23-AQP4 gene shows a band at ~30 kDa. AQP4: aquaporin 4, EGFP: enhanced green fluorescent protein, HEK293: human embryonic kidney 293, IRES: internal ribosome entry site, N/C: untransfected cells, Vector: transfected IRES2-eGFP vector only.
Fig. 2. In-house CBA to detect AQP4-IgG in patient sera. Sera from healthy subjects (A-D), MS patients (E-H), and NMOSD patients (I-L) were added to AQP4-GFP-transfected HEK293 cells. HEK293 cells transfected with AQP4-GFP show green fluorescence in the cytosol under fluorescence microscopy (B, F, and J). When the patient serum contained AQP4-IgG, red fluorescence was detected on the HEK293 cell membrane (K) due to binding of AQ4-IgG to AQP4, which is expressed on the membrane of HEK293 cells. AQP4-IgG: aquaporin 4-IgG, CBA: cell based assay, GFP: green fluorescent protein, HEK293: human embryonic kidney 293, MS: multiple sclerosis, NMOSD: neuromyelitis optica spectrum disorder.
Sera from 387 patients were assayed. The 178 definite-NMOSD patients comprised 142 true positives and 36 false negatives, yielding a sensitivity of 80% (95% CI=73.1–85.4%). The 63 high risk NMOSD patients comprised 48 true positives and 15 false negatives, yielding sensitivity of 76% (95% CI=63.8–86.0%). None of the 145 patients with other neurological diseases exhibited positivity, yielding specificity of 100% (95% CI=97.5–100%). The accuracy of the in-house CBA for detecting AQP4-IgG in definite NMOSD was 80% and in high risk NMOSD was 76%. This suggests that the in-house CBA is an accurate assay with high sensitivity and specificity (Table 3).
Table 3. Sensitivity, specificity, and accuracy of the in-house CBA.
| Assay | Definite NMOSD | Sensitivity (95% CI) | Accuracy (95% CI) | High risk NMOSD | Sensitivity (95% CI) | Accuracy (95% CI) | OND | Specificity (95% CI) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tested | + | Tested | + | Tested | + | ||||||
| In-house CBA | 178 | 142 | 80 (73.1–85.4) | 80 (73.1–85.4) | 63 | 48 | 76 (63.8–86.0) | 76 (63.8–86.0) | 145 | 0 | 100 (97.5–100) |
CBA: cell based assay, CI: confidence interval, NMOSD: neuromyelitis optica spectrum disorder, OND: other neurological diseases.
Sera from 90 definite-NMOSD and 21 high risk NMOSD patients were tested using both the in-house CBA and commercial CBA kit, and the results were compared (Table 4). The in-house CBA yielded sensitivity of 89% (95% CI=80.5–94.5%) and the commercial CBA yielded sensitivity of 87% (95% CI=77.9–92.9%) when sera from definite-NMOSD patients were assayed. The sensitivity for detecting AQP4-IgG in high risk NMOSD patients was higher for the in-house CBA was a more sensitive (sensitivity 91%, 95% CI=69.6–98.8%) method of detecting AQP4-IgG in high risk NMOSD patients than for the commercial CBA (sensitivity 76%, 95% CI=52.8–91.8%). The specificity of each assay could not be evaluated since only NMOSD patients were tested.
Table 4. Interassay concordance between the in-house CBA and the commercial CBA kit.
| Assay | Definite NMOSD | Sensitivity (95% CI) | Concordance | High risk NMOSD | Sensitivity (95% CI) | Concordance | ||
|---|---|---|---|---|---|---|---|---|
| Tested | + | Tested | + | |||||
| In-house CBA | 90 | 80 | 89 (80.5–94.5) | 84/90 93.3% |
21 | 19 | 91 (69.6–98.8) | 18/21 86% |
| Commercial CBA kit | 90 | 78 | 87 (77.9–92.9) | 21 | 16 | 76 (52.8–91.8) | ||
CI: confidence interval, CBA: cell based assay, NMOSD: neuromyelitis optica spectrum disorder.
The interassay concordance between the in-house CBA and the commercial CBA was determined for each patient group. The results of 84 samples (93%) from 90 definite-NMOSD patients correlated; in the other 6 samples, did not correlate as 4 were seropositive using the in-house CBA but seronegative using the commercial CBA, while 2 were seronegative using the in-house CBA but seropositive using the commercial CBA. The interassay concordance was determined to be 86% (18/21) when sera from high risk NMOSD patients were evaluated 3 samples did not correlate: 3 were seropositive using the in-house CBA but seronegative using the commercial CBA.
DISCUSSION
The importance of AQP4-IgG is now widely known, and different assays have been developed to detect this autoantibody in patient sera. However, these assays reportedly have varying sensitivities (33–90%).10 In the present fully blinded study, our in-house CBA detected AQP4-IgG in 80% of definite-NMOSD patients and 76% of high risk NMOSD patients, with 100% specificity. A systemic review on literatures reporting on different assays for detecting AQP4-IgG found that the CBA had the highest sensitivity (mean sensitivity=76.7%, range=55.6–96.7%),27 while the mean accuracy was also higher for the CBA (76.5%) than for other methods (range=48.5–62.3%).
The commercial CBA kit is based on using cells that have already been fixed, which makes it a simple and easy method. An international multicenter study found that the commercial CBA kit (EUROIMMUN, Luebeck, Germany) had a specificity of 100% and sensitivities of between 51.5% and 86.4%.10 A similar study found that the CBA using live cells expressing human M23-AQP4 was more sensitive than the CBA using fixed cells.8 We evaluated the interassay concordance between the in-house CBA and the commercial CBA kit using identical serum from 90 definite-NMOSD and 21 high risk NMOSD patients, and found a high interassay concordance. Moreover, the in-house CBA showed a higher sensitivity than the commercial CBA kit, and we suggest that this is due to our in-house CBA being based on live cells rather than fixed cells.
AQP4 is found on the astrocytic membrane in two isoforms: M23 and M1. The M1 isoform is the full-length protein while the M23 isoform is 22 amino acids shorter at the intracellular N-terminus.11 Some studies have found no differences between the M1 and M23 isoforms when detecting AQP4-IgG,8,12,13 while many other studies showed that the use of the M23 isoform provided a more sensitive substrate for AQP4-IgG assays than did the M1 isoform.14,15,16,17,18,19,20,21 A higher binding affinity of AQP4-IgG to the M23 isoform could be due to the formation of orthogonal arrays of particles (OAPs) at the cell surface by M23.22 In fact, when mutation was introduced to M23 protein and OAP formation was disrupted, the AQP4-IgG binding affinity was significantly reduced.23 Hence, in order to develop a more sensitive test, we used the M23 isoform of AQP4 when generating transfected HEK293 cells.
Live transiently transfected cells with fluorescently tagged AQP4 are often used due to the possibility that the expression of the gene of interest could decrease over time as the cell replicates,24 and the maintenance of cell lines and transfection prior to its use could limit the reproducibility of the assay.13 Moreover, CBAs with transiently transfected cells are based on the colocalization of AQP4-IgG in patient serum to cells that express fluorescently tagged AQP4. Tagging AQP4 with GFP and the expression of GFP can be used to confirm successful transfection and monitor AQP4 gene expression and protein localization.25 However, this method could restrict the binding between the antibody and antigen, since the addition of the 27-kDa GFP protein could change the structure of the AQP4 protein as well as the formation of OAP, leading to a reduced sensitivity. However, no difference in sensitivity between the M1 and M23 isoforms was found when N-terminal GFP tag was added.26 Mader et al.14 used GFP tagged at the C-terminus of M23-AQP4 and found that the M23 isoform maintained superior sensitivity; however, fluorescent tags still could be cytotoxic and so influence the assay.
The current study applied a new approach of the IRES-containing bicistronic vector to generate a stable HEK293 cell line. In contrast to transient transfection, stable transfection allows the gene of interest to be integrated into the host genome and the gene expression persists even as the cell replicates.24 Instead of a GFP tag, we used an IRES vector that is based on IRES controlling the downstream cistron expression without affecting the expression of upstream cistron, thereby allowing the simultaneous expression of both the protein of interest (M23-AQP4) and a selectable marker (GFP) without interfering with the expression of one another.27 We were therefore able to determine the serostatus without any interference in the fluorescence of each protein.
Despite our in-house CBA yielding high sensitivity and specificity, our method could not overcome the innate limitation of cell based immunofluorescence assay and it can only produce semiquantitative results.
In conclusion, we have refined a previous method by utilizing an IRES vector to generate stably transfected M23-AQP4-HEK293 cell lines. The high sensitivity and specificity of this assay reconfirms that the CBA is an accurate and reliable method for detecting both definite and high risk NMOSD patients.
Acknowledgements
This study was supported by the Bio & Medical Technology Development Program (M3A9B6069339) thourough the Ministry of Science, ICT & Future Planning, Republic of Korea.
Footnotes
Conflicts of Interest: Kim YS, Kim GY, Kong BS, Lee JE, Oh YM, Hyun JW, Kim SH, Joung AR, Kim BJ and Choi KH report no conflicts of interest. Dr. Kim HJ has lectured, consulted, and received honoraria from Bayer Schering Pharma, Biogen, Genzyme, HanAll BioPharma, MedImmune, Merck Serono, Novartis, Teva-Handok, and UCB; received a grant from the Ministry of Science; and accepted research funding from ICT & Future Planning, Genzyme, Kael-GemVax, Merck Serono, Teva-Handok, and UCB. He serves on a steering committee for MedImmune and as a co-editor for the Multiple Sclerosis Journal-Experimental, Translational, and Clinical. He also serves as an associated editor for the Journal of Clinical Neurology.
References
- 1.Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364:2106–2112. doi: 10.1016/S0140-6736(04)17551-X. [DOI] [PubMed] [Google Scholar]
- 2.Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005;202:473–477. doi: 10.1084/jem.20050304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roemer SF, Parisi JE, Lennon VA, Benarroch EE, Lassmann H, Bruck W, et al. Pattern-specific loss of aquaporin-4 immunoreactivity distinguishes neuromyelitis optica from multiple sclerosis. Brain. 2007;130:1194–1205. doi: 10.1093/brain/awl371. [DOI] [PubMed] [Google Scholar]
- 4.Bradl M, Misu T, Takahashi T, Watanabe M, Mader S, Reindl M, et al. Neuromyelitis optica: pathogenicity of patient immunoglobulin in vivo. Ann Neurol. 2009;66:630–643. doi: 10.1002/ana.21837. [DOI] [PubMed] [Google Scholar]
- 5.Hinson SR, McKeon A, Lennon VA. Neurological autoimmunity targeting aquaporin-4. Neuroscience. 2010;168:1009–1018. doi: 10.1016/j.neuroscience.2009.08.032. [DOI] [PubMed] [Google Scholar]
- 6.Verkman AS, Phuan PW, Asavapanumas N, Tradtrantip L. Biology of AQP4 and anti-AQP4 antibody: therapeutic implications for NMO. Brain Pathol. 2013;23:684–695. doi: 10.1111/bpa.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85:177–189. doi: 10.1212/WNL.0000000000001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waters PJ, McKeon A, Leite MI, Rajasekharan S, Lennon VA, Villalobos A, et al. Serologic diagnosis of NMO: a multicenter comparison of aquaporin-4-IgG assays. Neurology. 2012;78:665–671. doi: 10.1212/WNL.0b013e318248dec1. discussion 669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waters P, Reindl M, Saiz A, Schanda K, Tuller F, Kral V, et al. Multicentre comparison of a diagnostic assay: aquaporin-4 antibodies in neuromyelitis optica. J Neurol Neurosurg Psychiatry. 2016;87:1005–1015. doi: 10.1136/jnnp-2015-312601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hinson SR, Romero MF, Popescu BF, Lucchinetti CF, Fryer JP, Wolburg H, et al. Molecular outcomes of neuromyelitis optica (NMO)-IgG binding to aquaporin-4 in astrocytes. Proc Natl Acad Sci U S A. 2012;109:1245–1250. doi: 10.1073/pnas.1109980108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalluri SR, Illes Z, Srivastava R, Cree B, Menge T, Bennett JL, et al. Quantification and functional characterization of antibodies to native aquaporin 4 in neuromyelitis optica. Arch Neurol. 2010;67:1201–1208. doi: 10.1001/archneurol.2010.269. [DOI] [PubMed] [Google Scholar]
- 13.Jarius S, Wildemann B. Aquaporin-4 antibodies (NMO-IgG) as a serological marker of neuromyelitis optica: a critical review of the literature. Brain Pathol. 2013;23:661–683. doi: 10.1111/bpa.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mader S, Lutterotti A, Di Pauli F, Kuenz B, Schanda K, Aboul-Enein F, et al. Patterns of antibody binding to aquaporin-4 isoforms in neuromyelitis optica. PLoS One. 2010;5:e10455. doi: 10.1371/journal.pone.0010455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pisani F, Sparaneo A, Tortorella C, Ruggieri M, Trojano M, Mola MG, et al. Aquaporin-4 autoantibodies in neuromyelitis optica: AQP4 isoform-dependent sensitivity and specificity. PLoS One. 2013;8:e79185. doi: 10.1371/journal.pone.0079185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kitley J, Woodhall M, Leite MI, Palace J, Vincent A, Waters P. Aquaporin-4 antibody isoform binding specificities do not explain clinical variations in NMO. Neurol Neuroimmunol Neuroinflamm. 2015;2:e121. doi: 10.1212/NXI.0000000000000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crane JM, Lam C, Rossi A, Gupta T, Bennett JL, Verkman AS. Binding affinity and specificity of neuromyelitis optica autoantibodies to aquaporin-4 M1/M23 isoforms and orthogonal arrays. J Biol Chem. 2011;286:16516–16524. doi: 10.1074/jbc.M111.227298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iorio R, Fryer JP, Hinson SR, Fallier-Becker P, Wolburg H, Pittock SJ, et al. Astrocytic autoantibody of neuromyelitis optica (NMO-IgG) binds to aquaporin-4 extracellular loops, monomers, tetramers and high order arrays. J Autoimmun. 2013;40:21–27. doi: 10.1016/j.jaut.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sato DK, Nakashima I, Takahashi T, Misu T, Waters P, Kuroda H, et al. Aquaporin-4 antibody-positive cases beyond current diagnostic criteria for NMO spectrum disorders. Neurology. 2013;80:2210–2216. doi: 10.1212/WNL.0b013e318296ea08. [DOI] [PubMed] [Google Scholar]
- 20.Marignier R, Bernard-Valnet R, Giraudon P, Collongues N, Papeix C, Zéphir H, et al. Aquaporin-4 antibody-negative neuromyelitis optica: distinct assay sensitivity-dependent entity. Neurology. 2013;80:2194–2200. doi: 10.1212/WNL.0b013e318296e917. [DOI] [PubMed] [Google Scholar]
- 21.Rossi A, Ratelade J, Papadopoulos MC, Bennett JL, Verkman AS. Neuromyelitis optica IgG does not alter aquaporin-4 water permeability, plasma membrane M1/M23 isoform content, or supramolecular assembly. Glia. 2012;60:2027–2039. doi: 10.1002/glia.22417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nicchia GP, Mastrototaro M, Rossi A, Pisani F, Tortorella C, Ruggieri M, et al. Aquaporin-4 orthogonal arrays of particles are the target for neuromyelitis optica autoantibodies. Glia. 2009;57:1363–1373. doi: 10.1002/glia.20855. [DOI] [PubMed] [Google Scholar]
- 23.Tuller F, Holzer H, Schanda K, Aboulenein-Djamshidian F, Höftberger R, Khalil M, et al. Characterization of the binding pattern of human aquaporin-4 autoantibodies in patients with neuromyelitis optica spectrum disorders. J Neuroinflammation. 2016;13:176. doi: 10.1186/s12974-016-0642-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim TK, Eberwine JH. Mammalian cell transfection: the present and the future. Anal Bioanal Chem. 2010;397:3173–3178. doi: 10.1007/s00216-010-3821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chalfie M, Tu Y, Euskirchen G, Ward WW, Prasher DC. Green fluorescent protein as a marker for gene expression. Science. 1994;263:802–805. doi: 10.1126/science.8303295. [DOI] [PubMed] [Google Scholar]
- 26.Waters PJ, Pittock SJ, Bennett JL, Jarius S, Weinshenker BG, Wingerchuk DM. Evaluation of aquaporin-4 antibody assays. Clin Exp Neuroimmunol. 2014;5:290–303. doi: 10.1111/cen3.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gurtu V, Yan G, Zhang G. IRES bicistronic expression vectors for efficient creation of stable mammalian cell lines. Biochem Biophys Res Commun. 1996;229:295–298. doi: 10.1006/bbrc.1996.1795. [DOI] [PubMed] [Google Scholar]