Abstract
Understanding illness costs associated with diarrhea and acute respiratory infections (ARI) could guide prevention and treatment strategies. This study aimed to determine incidence of childhood diarrhea and ARI and costs of homecare, hospitalization, and outpatient treatment by practitioner type in rural Bangladesh. From each of 100 randomly selected population clusters we sampled 17 households with at least one child < 5 years of age. Childhood diarrhea incidence was 3,451 and ARI incidence was 5,849/1,000 child-years. For diarrhea and ARI outpatient care per 1,000 child-years, parents spent more on unqualified ($2,361 and $4,822) than qualified health-care practitioners ($113 and $947). For outpatient care, visits to unqualified health-care practitioners were at least five times more common than visits to qualified practitioners. Costs for outpatient care treatment by unqualified health-care practitioners per episode of illness were similar to those for qualified health-care practitioners. Homecare costs were similar for diarrhea and ARI ($0.16 and $0.24) as were similar hospitalization costs per episode of diarrhea and ARI ($35.40 and $37.76). On average, rural Bangladeshi households with children < 5 years of age spent 1.3% ($12 of $915) of their annual income managing diarrhea and ARI for those children. The majority of childhood illness management cost comprised visits to unqualified health-care practitioners. Policy makers should consider strategies to increase the skills of unqualified health-care practitioners, use community health workers to provide referral, and promote homecare for diarrhea and ARI. Incentives to motivate existing qualified physicians who are interested to work in rural Bangladesh could also be considered.
Introduction
Respiratory infections and diarrhea are leading causes of global childhood mortality.1 Approximately one-third (32%) of deaths among children < 5 years of age occur in south Asian countries.2 The cost of childhood illness places considerable economic burden on affected households. A study in rural India concluded that 10% of household income was spent on treatment of acute childhood morbidities.3 A study in urban Bangladesh conducted in 2011 calculated that the average cost of diarrhea illness per hospitalization episode was US$30,4 but little is known about other costs associated with childhood diarrhea and acute respiratory infections (ARI) in rural communities in Bangladesh.
Parents in Bangladesh can take their sick child to qualified health-care practitioners who hold an MBBS degree or to unqualified health-care practitioners, including paramedics, shopkeepers at pharmacies, and traditional and spiritual healers who have not received formal biomedical training and certification. Rural Bangladeshi and Indian parents have frequently sought care from unqualified health-care practitioners.5–8 Little information is available on costs associated with homecare and visits to unqualified and qualified practitioners. Understanding costs associated with diarrhea and ARI across practitioner type could guide policies and practices, especially for low-income families. This study aimed to measure the incidence of diarrhea and ARI, the costs of homecare, outpatient treatment by unqualified and qualified health-care practitioners, and hospitalization for children < 5 years of age in rural Bangladesh across wealth categories.
Methods
Study area.
The Government of Bangladesh and the United Nations Children's Fund (UNICEF) Sanitation, Hygiene Education, and Water Supply in Bangladesh (SHEWA-B) intervention commenced in 2007, targeting 24 million people in 76 rural subdistricts in 19 (of 64) districts. The program aimed to improve health by improving standards of hygiene practices. We leveraged the 2007 baseline survey among 100 random population clusters included in an evaluation of the impact of the SHEWA-B intervention to estimate the incidence of illness and cost of care seeking.
Sample size and study participants.
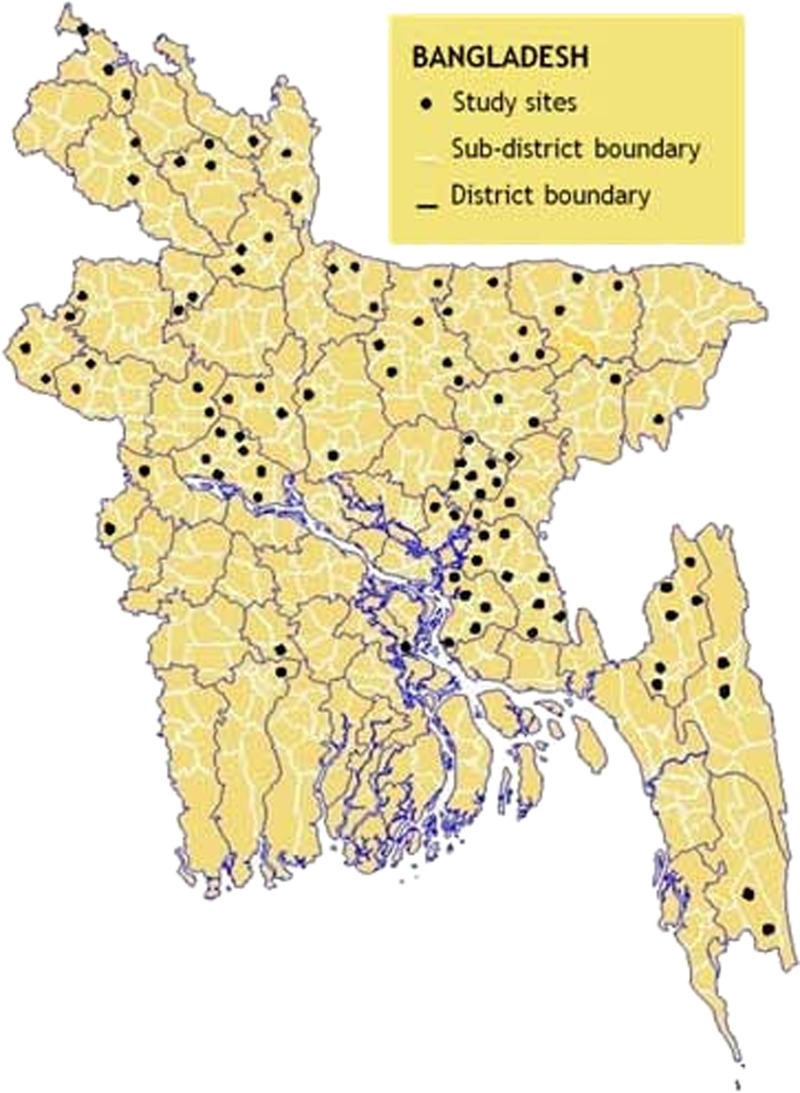
The cross-sectional survey sampled 1,700 households, as described elsewhere.9 In brief, to select the assessment population, we used cluster sampling. We selected clusters using probability proportional to size of population; therefore, the sampling units for this analysis were self-weighted. The study team sampled 50 clusters from the areas that would receive the SHEWA-B program, selected by UNICEF to have low water, sanitation, and hygiene (WASH) coverage. Fifty additional clusters were selected from those for subsequent use as control populations that were heuristically matched, in consultation with UNICEF staff based on similarity in geography, hydrogeology, infrastructure, agricultural productivity, and household construction and did not have similar intensive WASH programs in place.9 Clusters were selected using probability proportionate to the size of each union, the smallest administrative unit in rural Bangladesh, and 10% of the clusters were purposively located within the Chittagong Hill Tract (CHT) areas to ensure that this indigenous population would not be under-represented (Figure 1 ). Within clusters, 17 households were selected systematically from the house closest to the center point of the village with at least one child < 5 years of age. Then, the team skipped the two closest households and selected the next eligible household. The selection process continued until the field team reached the sample size for each cluster. The team administered the cross-sectional survey and collected hospitalization data from all 17 households. Based on attaining 80% power, an adequate sample size for assessing reported episodes of illness and outpatient care-seeking behavior, we collected these data from only the first seven households from each cluster. SHEWA-B intervention activities had not been initiated at the time of baseline data collection; thus, we included data from all selected clusters.
Figure 1.
Study sites of Sanitation, Hygiene Education and Water Supply in Bangladesh health impact study, rural Bangladesh, 2007.
Data collection.
From September to November 2007, the field team interviewed caregivers to collect data on diarrhea and ARI symptoms. They used a structured set of questions, conducted spot observations of household facilities, and collected data from available medical records related to health-care practitioner visits and treatment costs. The team interviewed participants using three recall times:14 days before interview (reported episodes of illness and homecare costs), 2 months before interview (outpatient treatment), and 12 months before interview (hospitalization). If a child had an episode of diarrhea or ARI that resulted in hospitalization in addition to an outpatient visit, they were included in the hospitalization category, not outpatient. These recall times were chosen based on studies demonstrating validity of self-reports for illness.10–12 A 2-month recall time for disease symptoms prompting a visit to a health-care provider has been used in previous studies.12 The field team collected data for all children aged < 5 years in sampled households. For outpatient treatment, the team inquired about costs of registration/visit fees, medicine, transportation, and wage loss. For hospitalization, the team inquired about costs of outpatient treatment before hospitalization, hospital registration and bed charges, medicine, diagnosis costs, transportation, and wage loss.
Definitions.
Diarrhea was defined as passage of unusually loose or watery stools at least three times within 24 hours as reported by child caregivers.13 Respiratory disease was defined as the presence of fever with difficulty breathing and/or cough.14 We defined homecare as treatment received at home before visiting a practitioner. Accordingly, we defined homecare costs as costs for purchasing treatment before visiting a qualified or unqualified practitioner. We defined health-care practitioners as qualified if they possessed an MBBS degree or equivalent and unqualified if they did not possess an MBBS degree or equivalent, including traditional village doctors, religious and/or spiritual healers, paramedics, medical assistants/health workers, homeopaths, and drug sellers. Outpatient costs were defined as those associated with visiting practitioners/facilities before hospital admission, and costs of hospitalization as costs of any treatment before hospitalization (visiting fees and medicine costs for any outpatient care, from either unqualified or qualified practitioners, before hospitalization), costs during hospitalization (registration fees, bed rent, medicine, diagnosis, and transportation), and costs of working days lost by parents or caregivers because of the illness resulting in hospitalization. We defined direct cost as cost of registration fees, bed rent, medicine, diagnosis, and transportation and indirect cost as wage loss for patient caregivers.
Data analysis.
For 14-day illness recall, we estimated the total observed child-years by adding all individual observed durations. For children > 14 days of age, the observed period was 14 days per child and for children < 14 days of age, it was their age. We trained data collectors to report occasions when a child had symptoms of illness over multiple occasions within the recall period as one episode. For children with diarrhea or ARI, we deducted 33% of observed days from the total observed period. Based on discussions among data collectors and child caregivers on estimates of the number of days the sick child was sick, we estimated that sick children remained sick an average of 33% of the 14-day recall time. Similarly, we estimated the total observed child-years for the 2-month recall time data equal to the child's age if < 2 months of age. The observed time for children > 2 months of age was 2 months. We deducted the total days they were ill from the total observed period. For calculating total days a sick child was ill in last 2 months, we included all illness episodes individually. We estimated similarly for the 12-month hospitalization recall time.
We calculated wealth scores using principal component analysis of household assets, utilities, and services.15,16 To assess the relationship between disease incidence or costs and household wealth status, we used the continuous wealth scores from the first principal component. We compared risk ratios (RRs) for the outcome of interest from lower scores to higher scores.
We calculated disease incidence and cost of illness per 1,000 child-years and cost per household. We calculated disease incidence based on reported episodes of illness, care-seeking events, and hospitalizations: incidence = ([total episodes × 1,000]/total observed child-years).
We calculated the mean cost of each episode by dividing the total cost by the total number of episodes of illness. To calculate the costs per 1,000 child-years due to diarrhea and ARI, we used the following formula: mean cost per 1,000 child-years = ([total actual cost] × [incidences per 1,000 child-years]/total number of illness episodes). We converted the costs of illness from local currency (Bangladeshi taka) into U.S. dollars at the 2007 rate (US$1 = taka 69).
We calculated the mean annual cost of illness per household including mean homecare costs, mean costs of outpatient care, and mean costs of hospitalization in the year preceding the interview. For mean homecare costs per household in the year preceding the interview, we calculated total amount spent on homecare costs by the parents of sick children during a 14-day recall time, divided by the total number of survey households, and assumed the rate was typical of spending throughout the year thus the estimated annual spending. The formula used for mean homecare costs per household in the year preceding the interview was ([total amount spent for the treatment of sick children at home during a 14-day recall time before bringing to a practitioner × 365]/[total number of survey households × 14]). Similarly, for estimating the mean outpatient care cost per household in the year preceding the interview, we calculated total actual amount spent by the parents of sick children for the 2-month recall time, divided by the total number of survey households, and calculated annual spending. For calculating the mean cost for a hospitalized patient per household, we calculated total actual costs for the hospitalized cases for the 1-year recall time, divided by the total number of surveyed households.
To evaluate the relationships between disease proportion and household wealth, cost per episode of illness and household wealth, and cost of illness per household and household wealth, we calculated RRs for diarrhea and ARI using a cluster-adjusted random effects Poisson regression model. Similarly, to evaluate the relationships between disease incidence and household wealth and between cost per 1,000 child-years and household wealth, we calculated RRs using cluster-adjusted random effects Poisson regression models.17,18
We also estimated the percentage of annual household income spent on treatment of childhood diarrhea and ARI. Since we did not collect income data, we used 2007 rural monthly household income data from the Bangladesh household income and expenditure survey report, which was $99.60 per month.19
Ethical issues and informed consent.
Field workers sought formal written informed consent from each study participant. This study was part of a program evaluation conducted by the International Center for Diarrheal Disease Research, Bangladesh (icddr,b) for UNICEF and was judged not to be human subjects research.15 The evaluation plan was reviewed and approved by UNICEF and the Department of Public Health Engineering of the Government of Bangladesh.
Results
During the 3-month study period, the field team collected data from 1,692 (99%) of 1,700 study households selected (Figure 1) from 45 districts. The mean number of persons per household was 5.5. One-third of the parents had no formal education (Table 1). Fourteen days before survey, 13% of children had diarrhea and 21% had ARI. Two months before survey, 13% of children with diarrhea visited health-care practitioners (11% visited unqualified, 0.9% qualified, and 1.4% both) and 24% with ARI visited health-care practitioners (18% visited unqualified, 4.2% qualified, and 2.2% both). Two percent of children with diarrhea and/or ARI were admitted to hospitals in the previous year (Table 2).
Table 1.
Household characteristics, rural Bangladesh, 2007 (N = 1,692)
| Household characteristics | |
|---|---|
| Household members, mean (SD) | 5.5 (2.1) |
| Children < 5 years of age, mean (SD) | 1.3 (0.5) |
| Sleeping rooms, mean (SD) | 2.1 (1.3) |
| Female headed households, % | 6 |
| Mother had no formal education, % | 31 |
| Father had no formal education, % | 36 |
| Had a television, % | 26 |
| Used a functional cell phone set, % | 29 |
| Had electricity connection, % | 45 |
| Had hygienic latrine to use*, % | 23 |
| Owned household land, % | 94 |
| Self-declared poorest, % | 9 |
SD = standard deviation.
Government of Bangladesh definition of hygienic latrine is “sealing of the passage between the squat hole and the pit,” which could be either a water seal or a lid.
Table 2.
Occurrence and costs of diarrhea and ARI in rural Bangladesh, 2007
| Indicators | Diarrhea | ARI |
|---|---|---|
| % (95% CI) | % (95% CI) | |
| Frequency of illness* and care-seeking behavior | ||
| Illness in 14-day recall (N = 808) | 12.6 (10.3, 14.9) | 20.8 (18.0, 23.6) |
| Provide with homecare†:14-day recall (N = 808) | 4.1 (2.7, 5.5) | 3.2 (2.0, 4.4) |
| Visited health-care practitioners: 2-month recall (N = 808) | 13.1 (10.8, 15.5) | 24.6 (21.6, 27.6) |
| Visited only qualified health-care practitioners | 0.9 (0.2, 1.5) | 4.2 (2.8, 5.6) |
| Visited only unqualified health-care practitioners | 11 (8.7, 13.0) | 18.2 (15.5, 20.9) |
| Visited both qualified and unqualified | 1.4 (0.6, 2.2) | 2.2 (1.2, 3.2) |
| Hospitalization: 1-year recall time (N = 2,126) | 1.5 (0.99, 2.06) | 1.0 (0.65, 1.56) |
| Incidences‡ per 1,000 child-years | Diarrhea | ARI |
| Disease incidence (N = 808) | 3,451 (2,824, 4,079) | 5,849 (5,060, 6,638) |
| Incidence of homecare† (N = 808) | 1,117 (743, 1,490) | 905 (562, 1,248) |
| Incidence of visiting any health-care practitioner (N = 808) | 1,103 (872, 1,334) | 2,059 (1,780, 2,339) |
| Only qualified | 60 (14, 107) | 361 (231, 491) |
| Only unqualified | 914 (700, 1,129) | 1,445 (1,211, 1,678) |
| Both qualified and unqualified | 128 (46, 211) | 253.5 (128, 379) |
| Hospitalization incidence (N = 2,126) | 18.6 (11.7, 25.6) | 14.5 (7.8, 21.2) |
| Cost per episode of illness (US$§) | Diarrhea | ARI |
| Homecare | 0.16 (0.11, 0.22) | 0.24 (0.13, 0.34) |
| Visited any health-care practitioner (in 2 months) | 2.66 (1.58, 3.74) | 3.43 (2.62, 4.23) |
| Visited qualified only (in 2 months) | 2.80 (−0.59, 6.18) | 2.62 (1.47, 3.77) |
| Visited unqualified only (in 2 months) | 2.58 (1.33, 3.83) | 3.34 (2.36, 4.31) |
| Visited both (in 2 months) | 3.16 (0.26, 6.05) | 5.66 (2.15, 9.17) |
| Hospitalization | 35.40 (25.46, 45.35) | 37.76 (28.81, 46.72) |
| Cost of illness per 1,000 child-years (in US$§) | Diarrhea | ARI |
| Total costs (homecare, outpatient, and hospitalization) per 1,000 child-years | 3,770 (2,879, 4,664) | 7,967 (6,578, 9,057) |
| Cost of outpatient care per 1,000 child-years (N = 808) | ||
| Homecare∥ | 175 (148, 213) | 214 (186, 243) |
| Visiting any health-care practitioner | ||
| Total | 2,935 (2,318, 3,543) | 7,205 (6,098, 8,013) |
| Direct | 1,400 (1,101, 1,683) | 3,981 (3,337, 4,385) |
| Indirect¶ | 1,535 (1,217, 1,860) | 3,224 (2,761, 3,628) |
| Visiting only qualified health-care practitioners | ||
| Total | 169 (39, 300) | 947 (606, 1,289) |
| Direct | 56 (13, 100) | 624 (399, 849) |
| Indirect | 113 (26, 200) | 323 (207, 440) |
| Visiting only unqualified health-care practitioners | ||
| Total | 2,361 (1,807, 2,915) | 4,822 (4,041, 5,603) |
| Direct | 1,142 (874, 1,410) | 2,472 (2,072, 2,872) |
| Indirect | 1,219 (934, 1,506) | 2,350 (1,970, 2,731) |
| Visiting both qualified and unqualified health-care practitioners | ||
| Total | 405 (146, 664) | 1,436 (723, 2,149) |
| Direct | 202 (73, 332) | 885 (445, 1,324) |
| Indirect | 203 (73, 333) | 551 (277, 825) |
| Hospitalization | 660.2 (412.5, 907.8) | 547.6 (294.2, 801.0) |
| Direct cost before hospitalization | 49.9 (31.2, 68.6) | 36.3 (19.5, 53.1) |
| Direct cost during hospitalization | 354.0 (221.2, 486.8) | 342.2 (183.8, 500.5) |
| Indirect cost | 256.2 (160.1, 352.4) | 169.1 (90.8, 247.3) |
| Outpatient care and hospitalization annual costs per household in the year preceding the interviews (in US$) | Diarrhea | ARI |
| Total annual costs per household (homecare, outpatient, and hospitalization) | 3.14 (1.76, 4.53) | 6.38 (4.54, 8.23) |
| Homecare∥ | 0.19 (0.11, 0.29) | 0.23 (0.10, 0.36) |
| Visited any health-care practitioner (N = 696) | 2.30 (1.29, 3.31) | 5.66 (4.18, 7.15) |
| Only qualified | 0.16 (−0.03, 0.35) | 0.74 (0.35, 1.14) |
| Only unqualified | 1.86 (0.90, 2.81) | 4.08 (2.76, 5.40) |
| Both qualified and unqualified | 0.28 (0.01, 0.56) | 0.85 (0.23, 1.46) |
| Hospitalization cost (N = 1,692) | 0.65 (0.36, 0.93) | 0.49 (0.26, 0.72) |
| Direct cost before hospitalization** | 0.05 (0.02, 0.07) | 0.03 (0.01, 0.05) |
| Direct cost after hospitalization | 0.35 (0.18, 0.52) | 0.31 (0.14, 0.47) |
| Indirect cost | 0.25 (0.12, 0.38) | 0.15 (0.06, 0.24) |
ARI = acute respiratory illness; CI = confidence interval.
P values of paired sample t tests.
Oral syrups, special foods, oral rehydration solution/fluids administered before taking children to a care provider.
Incidence = (illness episodes × 1,000/total observed child-years).
US$1 = taka 69 was the exchange rate in 2007–2008.
Self-prescribed medicine, special food, and fluids purchased before visiting a care provider; 14-day recall time.
Wage loss because of working days lost; calculated based on days lost because of child illness, visit to health-care providers, and stay with hospitalized patients. Calculation is based on minimum wage rate in rural Bangladesh of taka 300 per day.
Practitioner visit/registration, medicine, and homecare.
Disease incidence and visits to health-care practitioners were more frequent for ARI than diarrhea (Table 2), whereas homecare treatment and hospitalization incidences were similar. Outpatient care costs per episode were similar for diarrhea and ARI. However, estimated outpatient care costs per 1,000 child-years and estimated annual outpatient care costs per household were significantly higher for ARI treatment than for diarrhea treatment. Hospitalization costs per episode of diarrhea and ARI were similar and were considerably higher than per episode outpatient care costs. Visits to unqualified health-care practitioners for diarrhea or ARI were at least five times more common than to qualified health-care practitioners. The medicine costs per child per episode for diarrhea was significantly greater for unqualified versus qualified practitioners ($1.05 versus 0.52, P = 0.001) and for ARI (unqualified = $1.45 versus qualified = $1.20, P = 0.001; data not shown). Per episode of diarrhea or ARI, outpatient care treatment costs were similar for unqualified and qualified health-care practitioners. Direct and indirect costs for outpatient treatment were similar, but for hospitalization, direct costs of treatment were higher than indirect (Table 2).We estimated that in rural Bangladeshi households with a child < 5 years of age, the average household spent 1% of annual income ($12 of $1,196) on management of childhood diarrhea and ARI.
Diarrheal disease incidence (RR = 0.83; 95% confidence interval [CI] = 0.72, 0.96), incidence of visiting unqualified health-care practitioners for outpatient treatment (RR = 0.84; 95% CI = 0.74, 0.96), and average costs of outpatient treatment by unqualified health-care practitioners (RR = 0.83; 95% CI = 0.71, 0.97) were inversely proportional to wealth, but the frequency of diarrhea hospitalization (RR = 1.38; 95% CI = 1.05, 1.82), hospitalization incidence (RR = 1.33; 95% CI = 1.05, 1.70), and direct costs of hospitalization care (RR = 1.66; 95% CI = 1.28, 2.16) were directly proportional to wealth (Table 3). For ARI, there were no trends by wealth status for incidence, disease frequency, or visiting unqualified health-care practitioners. By contrast, costs for ARI homecare treatment and outpatient treatment were directly proportional to wealth (Table 3).
Table 3.
The relationship of household level wealth scores with illness proportions, care-seeking, incidence, and costs of diarrhea and ARI in rural Bangladesh, 2007
| Indicators | Diarrhea | ARI |
|---|---|---|
| RR† (95% CI) | RR† (95% CI) | |
| Children with illness* that sought care across continuous wealth scores | ||
| Disease (in 14 days) (N = 808) | 0.84 (0.73, 0.96) | 0.93 (0.86, 1.01) |
| Homecare (in 14 days) (N = 808) | 1.06 (0.83, 1.36) | 0.99 (0.77, 1.27) |
| Visited practitioner (in 2 months) (N = 808) | 0.89 (0.78, 1.02) | 0.98 (0.92, 1.06) |
| Visited qualified only | 0.72 (0.40, 1.30) | 0.91 (0.72, 1.15) |
| Visited unqualified only | 0.93 (0.80, 1.08) | 0.99 (0.90, 1.08) |
| Visited both | 0.68 (0.43, 1.06) | 1.11 (0.80, 1.54) |
| Hospitalization (in 1 year) (N = 1,962) | 1.38 (1.05, 1.82) | 0.95 (0.66, 1.38) |
| Incidence per 1,000 child-years across continuous wealth scores | ||
| Disease incidence | 0.83 (0.72, 0.96) | 0.92 (0.83, 1.03) |
| Homecare incidence (N = 808) | 1.05 (0.83, 1.34) | 0.98 (0.75, 1.29) |
| Incidence of visiting practitioner (N = 808) | 0.81 (0.72, 0.91) | 0.96 (0.88, 1.04) |
| Only qualified | 0.76 (0.45, 1.27) | 0.89 (0.73, 1.10) |
| Only unqualified | 0.84 (0.74, 0.96) | 0.95 (0.86, 1.05) |
| Both categories | 0.62 (0.42, 0.92) | 1.10 (0.86, 1.39) |
| Incidence of hospitalization (N = 1,962) | 1.33 (1.05, 1.70) | 0.85 (0.65, 1.10) |
| Mean costs per episode of illness (in US$‡) across continuous wealth scores | ||
| Overall cost including homecare, outpatient, and hospitalization (N = 808) | 0.87 (0.63, 1.20) | 1.12 (0.93, 1.37) |
| Homecare (N = 808) | 1.10 (0.87, 1.39) | 1.51 (1.24, 1.84) |
| Outpatient care (N = 808) | 0.96 (0.74, 1.26) | 1.16 (0.99, 1.36) |
| Qualified only | 0.98 (0.52, 1.83) | 1.56 (1.19, 2.05) |
| Unqualified only | 0.93 (0.68, 1.28) | 1.03 (0.87, 1.22) |
| Both | 1.46 (0.90, 2.35) | 1.64 (1.17, 2.31) |
| Hospitalization (N = 1,962) | 0.90 (0.74, 1.09) | 1.03 (0.87, 1.23) |
| Mean cost of illness per 1,000 child-years across continuous wealth scores (in US$‡) | ||
| Overall cost including outpatient and hospitalization (N = 808) | 1.07 (0.92, 1.25) | 0.95 (0.87, 1.04) |
| Outpatient care (N = 808) | ||
| Homecare | 1.23 (1.00, 1.50) | 1.50 (1.36, 1.65) |
| Visiting any practitioner | 0.83 (0.74, 0.94) | 1.15 (1.06, 1.25) |
| Direct§ | 0.98 (0.85, 1.13) | 1.23 (1.11, 1.36) |
| Indirect∥ | 0.71 (0.64, 0.80) | 1.06 (0.98, 1.14) |
| Visiting qualified only | ||
| Total | 0.77 (0.57, 1.04) | 1.34 (0.93, 1.91) |
| Direct§ | 0.65 (0.55, 0.76) | 1.44 (1.03, 2.01) |
| Indirect∥ | 0.81 (0.60, 1.12) | 1.16 (0.77, 1.74) |
| Visiting unqualified only | ||
| Total | 0.83 (0.71, 0.97) | 1.01 (0.92, 1.11) |
| Direct§ | 1.00 (0.84, 1.18) | 1.09 (0.98, 1.21) |
| Indirect∥ | 0.69 (0.60, 0.81) | 0.94 (0.86, 1.03) |
| Visiting both qualified and unqualified | ||
| Total | 0.88 (0.56, 1.37) | 2.03 (1.29 (3.20) |
| Direct§ | 0.96 (0.53, 1.73) | 1.85 (1.08, 3.17) |
| Indirect∥ | 0.80 (0.56, 1.15) | 0.94 (0.86, 1.03) |
| Hospitalization (N = 1,962) | ||
| Overall cost | 1.17 (0.89, 1.55) | 0.87 (0.54, 1.41) |
| Direct cost§ before hospitalization | 1.66 (1.28, 2.16) | 1.20 (0.87, 1.65) |
| Direct cost§ during hospitalization | 1.15 (0.89, 1.49) | 0.82 (0.48, 1.40) |
| Indirect cost∥ | 1.15 (0.85, 1.55) | 0.93 (0.61, 1.40) |
| Mean cost of illness per household in the year preceding the interview across continuous wealth scores (in US$‡) | ||
| Overall cost including homecare, outpatient care, and hospitalization (N = 808) | 0.91 (0.69, 1.21) | 1.00 (0.86, 1.16) |
| Homecare (N = 808) | 1.22 (0.86, 1.74) | 1.49 (1.12, 1.96) |
| Outpatient care (N = 808) | 0.89 (0.68, 1.17) | 1.19 (1.01, 1.41) |
| Visited qualified only | 0.71 (0.54, 0.93) | 1.37 (0.93, 2.04) |
| Visited unqualified only | 0.91 (0.65, 1.25) | 1.06 (0.89, 1.27) |
| Visited both health-care practitioners | 0.91 (0.56, 1.48) | 1.97 (1.22, 3.16) |
| Hospitalization care (N = 1,962) | 1.23 (0.86, 1.76) | 0.99 (0.64, 1.53) |
| Direct cost§ before hospitalization | 1.79 (1.23, 2.59) | 1.26 (0.93, 1.72) |
| Direct cost§ after hospitalization | 1.20 (0.81, 1.77) | 0.94 (0.56, 1.57) |
| Indirect cost∥ | 1.21 (0.81, 1.79) | 1.05 (0.68, 1.61) |
ARI = acute respiratory illness; CI = confidence interval; RR = risk ratio.
Diarrhea or ARI.
RR < 1 indicates an inverse relationship between health outcome and wealth, and/or between cost of treatment and wealth; RR > 1 indicates a direct relationship between health outcome and wealth and/or between cost of treatment and wealth. For example, if RR for diarrhea (in 14 days) = 0.84, this indicates that for every unit increase of household wealth there were 16% fewer cases of diarrhea.
US$1 = taka 69 using the 2007–2008 exchange rate.
Direct costs refer to cost of visiting/registration, medicine, diagnostics, and transportation.
Indirect costs refer to costs related to wage loss.
Discussion
The largest portion of childhood diarrhea and ARI treatment costs was for outpatient treatment and most outpatient costs were incurred visiting unqualified health-care practitioners. Although costs of treatment by unqualified health-care practitioners per 1,000 child-years or per household in the year preceding the interview were greater than costs for treatment by qualified health-care practitioners, costs per episode were similar for both practitioner types for both illnesses.
Costs of treatment by unqualified health-care practitioners were significantly higher among poorer households attributable to a greater number of visits among poorer compared with richer households.20 Unqualified practitioner do not charge visiting fees, and they are abundant in rural communities, minimizing transportation costs and wage loss.21–23 However, since they often run their own drug shops, they may prescribe a greater quantity of drugs compared with qualified health-care practitioners,24–26 increasing overall cost per episode of illness, suggested by analysis of medicine costs in this study.
Previous studies in Bangladesh and India found that every year households spent an average of 2–10% on treatments.20,26,27 A prospective cohort study in rural India showed that households spent 10% of their income on management of all types of childhood diseases, with the majority of this expenditure for private doctors; over 60% of the sick children were treated by private doctors, whose services were more expensive than doctors at government health centers. We estimated that rural Bangladeshi households spent 1% of their income on childhood diarrhea and ARI management in line with other studies conducted in Bangladesh.27,28
The 2007 Bangladesh Demographic and Health Survey (BDHS), conducted during a similar time frame, reported diarrhea prevalence of 9.7% among children < 5 years of age from rural areas using a 2-week recall period, compared with 13% among our study participants. The somewhat higher diarrhea prevalence reported here, which may be attributed to the selected population for subsequent intervention, was chosen from those with poor sanitation and safe water coverage compared with other areas in Bangladesh.29 ARI prevalence was higher among our study children (21%) compared with the national estimates (4.8%) reported in BDHS 2007; however, BDHS 2007 used a different ARI definition.
Our study found that direct and indirect costs of illness contributed almost equally to outpatient care costs; however, for hospitalization care, direct costs was approximately two-thirds: 61% for diarrhea and 69% for ARI, consistent with a Bangladeshi study on influenza-associated costs at tertiary level hospitals.30 Higher direct than indirect costs for hospitalization episodes may be attributed to bed rent, food costs, and specialized doctor fees, as frequently more detailed diagnosis is required compared with outpatient care visit. Transportation costs, which we defined as direct costs, are likely higher in rural compared with urban areas, contributing to higher overall direct costs.31 Our study found that costs of medicine were greater than registration and diagnosis costs, perhaps because unqualified health-care practitioners prescribe a greater quantity of drugs, but perform fewer diagnostic tests and do not charge visiting fees, which is consistent with a study from nationally representative surveys in 11 Asian countries.32
This study has limitations. Data were collected using three different recall durations, which could affect the comparability of rates and costs across different categories. However, we minimized this effect by maintaining uniformity in presentation of data as child-years and typical year figures across all three-recall durations. It is possible that more than one episode of diarrhea or ARI occurred within the 14-day illness recall time thereby underestimating incidence. Additionally, there may be bias in recalling costs when data were collected for a longer recall time. Among 47 patients hospitalized for diarrhea or ARI, we found no significant difference in average outpatient costs for the two recall periods (< 2 months, $2.70 versus 2–12 months, $2.50; P = 0.76). Similarly, there was no significant difference in hospitalization cost for the 2–12 months recall period compared with the < 2-month period ($24 versus $18; P = 0.46; data not shown). Our data were collected from rural households in underserved districts including an overrepresentation of the CHT population and therefore may not be generalizable to the Bangladeshi population, but the study covered a large population that is broadly similar to rural Bangladesh. It is likely that costs would be different in urban areas; access to services might be greater in urban areas and could affect health-seeking behaviors.33 We collected the study data in late 2007. Costs have risen in the intervening years; Bangladesh has an average annual inflation rate of ∼6%, and the costs for visiting health-care providers, medicines, pathological tests, and daily wage rates have increased.34 Thus absolute costs calculated here will not reflect those in subsequent years, and changes in incidence may have occurred. However, trends for incidence, practitioner visited, direct and indirect costs, associations with wealth, and comparisons among the two illnesses can be used to inform diarrhea and ARI prevention programs.
The study found that the majority of spending for clinical care of childhood diarrhea and ARI was on outpatient care provided by unqualified providers. Of particular note and policy relevance is the higher cost burden on the poorest segment of the population and is worthy of further exploration. It is possible that practitioners perceive that poorer people require additional treatment support, possibly because they visit less frequently, or drug shop owners see less educated people as vulnerable targets for sales. Since quality of clinical care is critical for improved child health outcomes,35 attention to care provided by health-care practitioners is particularly important. Unqualified health-care practitioners based in rural areas are readily available and often provide services on credit.24 The government system, by contrast, has difficulty attracting qualified health-care practitioners to rural posts. The government could consider providing incentives for providers to work and live in rural areas, as programs in other settings have done.36,37 Earlier studies in Bangladesh and India suggest that treatments from unqualified health-care practitioners were often inappropriate and recommended avoiding these practitioners.38–40 To overcome shortages in qualified health personnel in rural areas, the government could provide training to community health workers on disease identification, referral, and distribution of treatment such as oral rehydration solution for diarrhea or antibiotics for pneumonia; this model has been successful in Bangladesh and in other countries.41–44 Efforts to upgrade the skills of existing unqualified providers and integrate them into the qualified health-care system should also be considered. Integrating community health workers and encouraging appropriate homecare treatment could reduce the number of health-care provider visits and hospitalizations and may be a feasible, cost-effective measure to reduce cost of illness.45
ACKNOWLEDGMENTS
We thank the UK Department for International Development for the financial support. We are also grateful to the field team supervised by Mamun-Ar-Rashid, Bimal Das and Abdul Alim Beg, and study participants. We also acknowledge Meghan L. Scott for her frequent review. icddr,b is thankful to the Governments of Australia, Bangladesh, Canada, Sweden, and the United Kingdom for providing core/unrestricted support.
Footnotes
Authors' addresses: Amal K. Halder, Probir K. Ghosh, and Leanne Unicomb, Centre for Communicable Diseases, icddr,b, Dhaka, Bangladesh, E-mails: amalkrishna.halder@gmail.com, probir@icddrb.org, and leanne@icddrb.org. Stephen P. Luby, Department of Medicine, Stanford University, Stanford, CA, E-mail: sluby@stanford.edu. Shamima Akhter, Center for Equity and Health Systems, icddr,b, Dhaka, Bangladesh, E-mail: sakhter@icddrb.org. Richard B. Johnston, Joint Monitoring Programme for Water Supply and Sanitation, WHO, Geneva, Switzerland, E-mail: leanne@icddrb.org.
References
- 1.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE. Child Health Epidemiology Reference Group of WHO and UNICEF Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 2.UNICEF . Levels & Trends in Child Mortality—Report 2014: Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation. New York, NY: UNICEF; 2014. [Google Scholar]
- 3.Dongre AR, Deshmukh PR, Garg BS. Health expenditure and care seeking on acute child morbidities in peri-urban Wardha: a prospective study. Indian J Pediatr. 2010;77:503–507. doi: 10.1007/s12098-010-0063-8. [DOI] [PubMed] [Google Scholar]
- 4.Sarker AR, Islam Z, Khan IA, Saha A, Chowdhury F, Khan AI, Qadri F, Khan JA. Cost of illness for cholera in a high risk urban area in Bangladesh: an analysis from household perspective. BMC Infect Dis. 2013;13:518. doi: 10.1186/1471-2334-13-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roess AA, Winch PJ, Ali NA, Akhter A, Afroz D, El Arifeen S, Darmstadt GL, Baqui AH. Bangladesh PROJAHNMO Study Group Animal husbandry practices in rural Bangladesh: potential risk factors for antimicrobial drug resistance and emerging diseases. Am J Trop Med Hyg. 2013;89:965–970. doi: 10.4269/ajtmh.12-0713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute of Population Research and Training (NIPORT) Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh: NIPORT; 2013. [Google Scholar]
- 7.Kumar S. Much health care in rural India comes from unqualified practitioners. BMJ. 2004;328:975. doi: 10.1136/bmj.328.7446.975-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piechulek H, Al-Sabbir A, Mendoza-Aldana J. Diarrhea and ARI in rural areas of Bangladesh. Southeast Asian J Trop Med Public Health. 2003;34:337–342. [PubMed] [Google Scholar]
- 9.Huda TMN, Unicomb L, Johnston RB, Halder AK, Yushuf Sharker MA, Luby SP. Interim evaluation of a large scale sanitation, hygiene and water improvement programme on childhood diarrhea and respiratory disease in rural Bangladesh. Soc Sci Med. 2012;75:604–611. doi: 10.1016/j.socscimed.2011.10.042. [DOI] [PubMed] [Google Scholar]
- 10.López-Alarcón M, Villalpando S, Fajardo A. Breast-feeding lowers the frequency and duration of acute respiratory infection and diarrhea in infants under six months of age. J Nutr. 1997;127:436–443. doi: 10.1093/jn/127.3.436. [DOI] [PubMed] [Google Scholar]
- 11.Kongsbak K, Wahed M, Friis H, Thilsted S. Acute-phase protein levels, diarrhoea, Trichuris trichiura and maternal education are predictors of serum retinol: a cross-sectional study of children in a Dhaka slum, Bangladesh. Br J Nutr. 2006;96:725–734. [PubMed] [Google Scholar]
- 12.Burton DC, Flannery B, Onyango B, Larson C, Alaii J, Zhang X, Hamel MJ, Breiman RF, Feikin DR. Healthcare-seeking behaviour for common infectious disease-related illnesses in rural Kenya: a community-based house-to-house survey. J Health Popul Nutr. 2011;29:61–70. doi: 10.3329/jhpn.v29i1.7567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO Diarrhoea. 2014. http://www.who.int/topics/diarrhoea/en/ Available at. Accessed October 15, 2016.
- 14.Luby SP, Halder AK. Associations among handwashing indicators, wealth, and symptoms of childhood respiratory illness in urban Bangladesh. Trop Med Int Health. 2008;13:835–844. doi: 10.1111/j.1365-3156.2008.02074.x. [DOI] [PubMed] [Google Scholar]
- 15.Luby SP, Halder AK, Tarique NH, Unicomb L, Rohnston RB. The effect of handwashing at recommended times with water alone and with soap on child diarrhea in rural Bangladesh: an observational study. PLoS Med. 2011;8:e1001052. doi: 10.1371/journal.pmed.1001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21:459–468. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 17.Hutchinson MK, Holtman MC. Analysis of count data using Poisson regression. Res Nurs Health. 2005;28:408–418. doi: 10.1002/nur.20093. [DOI] [PubMed] [Google Scholar]
- 18.Hall DB. Zero-inflated Poisson and binomial regression with random effects: a case study. Biometrics. 2000;56:1030–1039. doi: 10.1111/j.0006-341x.2000.01030.x. [DOI] [PubMed] [Google Scholar]
- 19.World Bank Bangladesh—Household Income and Expenditure Survey: Key Findings and Results 2010. 2011. http://documents.worldbank.org/curated/en/2011/06/16494498/bangladesh-household-income-expenditure-survey-key-findings-results-2010 Available at. Accessed June 15, 2014.
- 20.Rahman MM, Gilmour S, Saito E, Sultana P, Shibuya K. Health-related financial catastrophe, inequality and chronic illness in Bangladesh. PLoS One. 2013;8:e56873. doi: 10.1371/journal.pone.0056873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed SM, Hossain MA, Rajachowdhury AM, Bhuiya AU. The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Hum Resour Health. 2011;9:3. doi: 10.1186/1478-4491-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saksena P, Xu K, Elovainio R, Perrot J. Health Services Utilization and Out-of-Pocket Expenditure at Public and Private Facilities in Low-Income Countries. Geneva, Switzerland: WHO; 2010. World Health Report (2010) Background Paper 20. [DOI] [PubMed] [Google Scholar]
- 23.Asenso-Okyere WK, Anum A, Osei-Akoto I, Adukonu A. Cost recovery in Ghana: are there any changes in health care seeking behaviour? Health Policy Plan. 1998;13:181–188. doi: 10.1093/heapol/13.2.181. [DOI] [PubMed] [Google Scholar]
- 24.Ahmed SM, Hossain MA. Knowledge and practice of unqualified and semi-qualified allopathic providers in rural Bangladesh: Implications for the HRH problem. Health Policy. 2007;84:332–343. doi: 10.1016/j.healthpol.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 25.Ahmed SM, Hossain MA, Chowdhury MR. Informal sector providers in Bangladesh: how equipped are they to provide rational health care? Health Policy Plan. 2009;24:467–478. doi: 10.1093/heapol/czp037. [DOI] [PubMed] [Google Scholar]
- 26.Shahrawat R, Rao KD. Insured yet vulnerable: out-of-pocket payments and India's poor. Health Policy Plan. 2012;27:213–221. doi: 10.1093/heapol/czr029. [DOI] [PubMed] [Google Scholar]
- 27.Tong N. Background Paper 6.22 Pneumonia. Geneva, Switzerland: WHO; 2013. Update on 2004 Background Paper: Priority Medicines for Europe and the World “A Public Health Approach to Innovation.”. [Google Scholar]
- 28.Kelley L, Black R. Research to support household and community IMCI. Report of a meeting, 22–24 January 2001, Baltimore, Maryland, USA. J Health Popul Nutr. 2001;19:S111–S154. [PubMed] [Google Scholar]
- 29.Local Government Division, Government of Bangladesh National Policy for Safe Water Supply & Sanitation 1998. 1998 http://www.dphe.gov.bd/pdf/National-Policy-for-Safe-Water-Supply-&-Sanitation-1998.pdf Available at. Accessed October 15, 2016. [Google Scholar]
- 30.Bhuiyan MU, Luby SP, Alamgir NI, Homaira N, Mamun AA, Khan JA, Abedin J, Sturm-Ramirez K, Gurley ES, Zaman RU, Alamgir AS, Rahman M, Widdowson MA, Azziz-Baumgartner E. Economic burden of influenza-associated hospitalizations and outpatient visits in Bangladesh during 2010. Influenza Other Respi Viruses. 2014;8:406–413. doi: 10.1111/irv.12254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.N-SSATS . Differences and Similarities between Urban and Rural Outpatient Substance Abuse Treatment Facilities. Rockville, MD: Center for Behavioral Health Statistics and Quality, SAMHSA; 2011. http://oas.samhsa.gov Available at. Accessed October 15, 2016. [Google Scholar]
- 32.van Doorslaer E, O'Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, Harbianto D, Herrin AN, Huq MN, Ibragimova S, Karan A, Ng CW, Pande BR, Racelis R, Tao S, Tin K, Tisayaticom K, Trisnantoro L, Vasavid C, Zhao Y. Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. Lancet. 2006;368:1357–1364. doi: 10.1016/S0140-6736(06)69560-3. [DOI] [PubMed] [Google Scholar]
- 33.Chaudhury N, Hammer JS. Ghost doctors: absenteeism in rural Bangladeshi health facilities. World Bank Econ Rev. 2004;18:423–441. [Google Scholar]
- 34.Mahumud RA, Sultana M, Sarker AR. Trend of healthcare expenditures in Bangladesh over last decades. Am J Econ Financ Manag. 2015;1:97–101. [Google Scholar]
- 35.Oxman AD, Thomson MA, Davis DA, Haynes B. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ. 1995;153:1423–1431. [PMC free article] [PubMed] [Google Scholar]
- 36.Kolstad JR. How to make rural jobs more attractive to health workers. Findings from a discrete choice experiment in Tanzania. Health Econ. 2011;20:196–211. doi: 10.1002/hec.1581. [DOI] [PubMed] [Google Scholar]
- 37.Darmstadt GL, Baqui AH, Choi Y, Bari S, Rahman SM, Mannan I, Ahmed AS, Saha SK, Seraji HR, Rahman R, Winch PJ, Chang S, Begum N, Black RE, Santosham M, Arifeen SE. Bangladesh Projahnmo-2 (Mirzapur) Study Validation of a clinical algorithm to identify neonates with severe illness during routine household visits in rural Bangladesh. Arch Dis Child. 2011;96:1140–1146. doi: 10.1136/archdischild-2011-300591. [DOI] [PubMed] [Google Scholar]
- 38.Rahman MM, Huq M Rahman MA. Study on the pattern of prescriptions available at rural households in Bangladesh. South East Asia J Public Health. 1:12–16. [Google Scholar]
- 39.Barua N, Pandav CS. The allure of the private practitioner: is this the only alternative for the urban poor in India? Indian J Public Health. 2011;55:107–114. doi: 10.4103/0019-557X.85242. [DOI] [PubMed] [Google Scholar]
- 40.Narayana K. The Unqualified Medical Practitioners: Methods of Practice and Nexus with the Qualified Doctors. 2006. http://www.eaber.org/node/22330 Available at. Accessed June 15, 2014.
- 41.Rahman AS, Islam MR, Koehlmoos TP, Raihan MJ, Hasan MM, Ahmed T, Larson CP. Impact of NGO training and support intervention on diarrhoea management practices in a rural community of Bangladesh: an uncontrolled, single-arm trial. PLoS One. 2014;9:e112308. doi: 10.1371/journal.pone.0112308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lopes SC, Cabral AJ, de Sousa B. Community health workers: to train or to restrain? A longitudinal survey to assess the impact of training community health workers in the Bolama Region, Guinea-Bissau. Hum Resour Health. 2014;12:8. doi: 10.1186/1478-4491-12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, van Wyk BE, Odgaard-Jensen J, Johansen M, Aja GN, Zwarenstein M, Scheel IB. Lay health workers in primary and community health care. Cochrane Database Syst Rev. 2005:CD004015. doi: 10.1002/14651858.CD004015.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ande O, Oladepo O, Brieger WR. Comparison of knowledge on diarrheal disease management between two types of community-based distributors in Oyo State, Nigeria. Health Educ Res. 2004;19:110–113. doi: 10.1093/her/cyg004. [DOI] [PubMed] [Google Scholar]
- 45.Melek SP, Norris DT, Paulus J. Economic Impact of Integrated Medical-Behavioral Healthcare, Implications for Psychiatry. Denver, CO: Milliman Inc; 2014. Milliman American Psychiatric Association Report. [Google Scholar]