Abstract
Studies assessing the impacts of school-based water, sanitation, and hygiene (WASH) interventions have revealed inconsistent improvements in pupils' health and educational outcomes. This may be in part due to suboptimal project fidelity or adherence. As part of a matched-control trial of a comprehensive school-based WASH project in Mali, we measured the degree to which schools met four prespecified WASH targets, comprised of 15 criteria, 0–3 years after program implementation. We compared achievement of the targets and criteria between beneficiary and matched control schools, and compared achievement within beneficiary schools at baseline and at follow-up visits. We assessed the “as-treated” associations between WASH target achievement and pupil diarrhea, respiratory symptoms, and absence. Between 44% and 81% of beneficiary schools achieved each target. Although adherence was inconsistent across schools, beneficiary schools, on average, met more WASH targets than matched control schools, and beneficiary schools also met more WASH targets at follow-up than at baseline. Very few of the targets were individually associated with health and absenteeism outcomes. Increasing achievement of multiple WASH targets together was associated with a lower odds of pupils having diarrhea (P trend < 0.01) and having respiratory symptoms (P trend < 0.01), but was not associated with roll-call absence (P trend = 0.14) or pupil-reported absence (P trend = 0.41). These results indicate that a comprehensive WASH intervention and a focus on increasing adherence may help maximize the health effects of school WASH programs, but that WASH alone might not be sufficient to decrease pupils' absenteeism.
Introduction
Inadequate water, sanitation, and hygiene (WASH) causes an estimated 83 million disability adjusted life years (DALYs) annually, contributing to nearly one-third of DALYs associated with environmental risk.1 Schools can play an important role in the transmission cycle; crowded and unsanitary school WASH conditions have the potential to serve as foci for disease transmission. According to best estimates by The United Nations Children's Fund, only 51% of schools in low-income settings have access to water, and 45% have adequate sanitation facilities.2 Access to microbiologically safe water, hygienic sanitation facilities, and water and soap for handwashing, along with sufficient behavior change, has the potential to both limit transmission at the school and foster improved WASH practices in future generations.
Although there is biological plausibility supporting the health and educational benefits of providing WASH in schools, evaluations of school WASH programs have shown mixed results.3–8 Improvements to WASH at schools have sometimes been shown to reduce diarrheal disease,6,9 acute respiratory infections,10 soil-transmitted helminth reinfections,11 and absence among pupils.3,12 However, these effects are often not consistent between studies and within studies they are dependent on study context and/or the subgroup of pupils under study.
Possible reasons for the mixed results of school WASH trials may be weak program design (i.e., weak theory of change), poor program fidelity (e.g., whether the program achieved implementation targets), limited adherence (e.g., low level of engagement by beneficiaries), or weak evaluation design and implementation. Very few rigorous studies have focused on evaluating these factors within school WASH trials. Recent school WASH trials in Kenya investigated intervention fidelity and adherence and found improvements to WASH infrastructure, but usually not to optimal levels.4,13–15 The lack of consistent evidence of impact may also be that pupils' health and education are influenced by many other factors that are not related to the WASH conditions in schools, such as socioeconomic factors. Further, without proper pupil behaviors and operation and maintenance of facilities, WASH programs may be insufficient in breaking the transmission cycle and may even increase exposure to fecal pathogens.12 In addition, some school WASH programs target only one WASH intervention, such as handwashing, and a more comprehensive program may be necessary to fully disrupt the disease transmission cycle.
Another related reason for these mixed results may relate to the measure of effect. Most trials report the intention-to-treat (ITT) results—the average effect of the intervention on the outcome without regard to the achievement of project outputs and outcomes, or fidelity and adherence.16 However, it is known that if fidelity of the project or adherence to an intervention is poor, the ITT results may not reflect the true effect of the intervention on the outcomes for adherers.17 As-treated, per-protocol, or instrumental variable analyses are better suited to measure the contribution of fidelity and subsequent adherence. Recent secondary analyses have been used to supplement previous WASH trials, and show that the pupils attending the more adherent schools were those who were less likely to have diarrhea or to be absent.14,15
A comprehensive school-based WASH project—the Dubai Cares Initiative in Mali for WASH in schools (DCIM)—was carried out in over 900 primary and secondary schools in Mali between 2011 and 2014. Results from an ITT analysis showed beneficiary schools had lower rates of self-reported diarrhea and respiratory infection symptoms and absence due to diarrhea, but higher rates of roll-call absence compared with the control schools.9 The purpose of this article is to report on project fidelity and adherence vis-à-vis achievement of predetermined WASH performance output and outcome targets, and to conduct an as-treated analyses to quantify the extent to which the achievement of these WASH targets—both individually and collectively—impacted children's diarrhea, respiratory infection symptoms, and absence.
Methods
Study setting.
The DCIM program was implemented in 916 primary and secondary schools in six of Mali's nine regions, including Bamako District, Koulikoro, Gao, Mopti, Timbuktu, and Sikasso; however, an armed conflict began in March 2012 and the program was discontinued in Timbuktu, Gao, and parts of Mopti regions. The project was implemented by CARE Mali, Oxfam GB, Save the Children US, UNICEF-Mali, and WaterAid Mali, and was financially supported by the Dubai Cares Foundation.
Core activities of the project are listed in Table 1. The comprehensive WASH program included water supply, sanitation, WASH supplies, and information, education, and communication activities. The program was adapted over time, so that lessons learned from earlier phases of implementation were applied to improve the program as it progressed. Over the 4 years of program implementation, improvements were made to the design of the latrines and handwashing stations as well as approaches for hygiene promotion among children. Most of the partners also shifted to using a community-led total sanitation approach to engage the surrounding communities. Performance monitoring data were collected following the completion of program activities to inform on the program's success in creating sustained improvements in the school WASH environments.
Table 1.
Core program activities
| Domain | Activity |
|---|---|
| Water supply | Installation or rehabilitation of water points so that there was at least one improved water point on the school compound. Improved water point classified as a borewell or covered well with a pump. |
| Sanitation | Installing or rehabilitating latrines so that there was at least one improved latrine for every 70 boys and girls. Improved latrine classified as a pit latrine covered with a concrete slab and disabled-friendly access. |
| WASH supplies | Each school provided with a hygiene kit including handwashing and drinking water containers, anal cleansing kettles, trash bins, brooms, handwashing soap, bleach, and disinfectant. Materials were provided one time only. |
| Information, education, communication and capacity-strengthening activities | Promotion of good WASH practices and behavior change at school and within the community; training on hygiene promotion to teachers and school management committees; establishment of school hygiene clubs or children's government; and establishment of management systems to ensure sustained financing, monitoring, and maintenance. |
WASH = water, sanitation, and hygiene.
Study sample.
Our study sample consisted of 100 beneficiary schools and 100 matched control schools that were used in the previously reported ITT analysis. The inclusion criteria for beneficiary schools participating in the study were that they were primary schools scheduled to receive the DCIM intervention by June 2013 and located in parts of Mali that were not part of the armed conflict (i.e., not in Timbuktu and Gao regions or unstable areas within Mopti region). Matched control schools were selected based on educational district, water and sanitation access, and enrollment size. Within each school, 20 boys and 20 girls from grades 3–6 were systematically sampled from class registers and the same pupils were followed until study completion. Pupils who left the cohort (7.4%) during the school year were replaced with other pupils in the same class using systematic random sampling. Pupils who advanced into the seventh grade at the end of the first school year (11.4%) were replaced with incoming third graders. Further details on matching and selection are available elsewhere.9
Data collection.
The evaluation took place between January 2013 and May 2014, with a baseline collection occurring between December 2010 and April 2011 among schools initially selected for the intervention. As discussed earlier, an armed conflict resulted in a shift of the study site and impacted the availability of baseline data in the schools included in our evaluation.9 Enumerators performed four to six unscheduled visits to each school following the completion of all intervention activities. At each visit, enumerators conducted observations of school WASH facilities, interviews with the school director, pupil surveys, and a roll call in all classes. Data were entered on Android-enabled devices using Open Data Kit software.18 All pupil surveys were administered in that pupil's local language. No compensation was given for participation in the study.
WASH performance targets.
Four main program targets relating to water supply, sanitation, handwashing, and WASH supplies were set by the partners. Each target was composed of three to five criteria, for a total of 15 criteria (listed in Table 2). These targets and criteria included factors associated with program fidelity (e.g., provision of water points, latrines, and supplies) as well as adherence by the schools (e.g., making handwashing containers and soap available, maintaining latrine cleanliness, repairing broken water points). Fidelity here is defined as the delivery of program outputs, whereas adherence is defined as the behaviors of beneficiaries in taking up and maintaining behaviors.
Table 2.
Mean WASH performance target data for beneficiary schools and matched control schools
| Beneficiary schools | Matched control schools | ||||||
|---|---|---|---|---|---|---|---|
| Follow-up %‡ (SD) | Baseline %‡ (SD) | % change* | P* | Follow-up %§ (SD) | % change† | P† | |
| Number of schools | 100 | 94 | 100 | ||||
| % of visits where schools met all four targets | 23 (34) | 0 (0) | 23 | – | 0 (0) | 23 | – |
| % of visits where schools met water supply target: functional, improved water point on school grounds | 81 (34) | 36 (48) | 45 | < 0.01 | 44 (47) | 37 | < 0.01 |
| % of visits where a water point was on school grounds, any | 90 (30) | 50 (50) | 40 | < 0.01 | 59 (48) | 31 | < 0.01 |
| % of visits where a water point was on school grounds, improved | 90 (30) | 41 (50) | 49 | < 0.01 | 56 (50) | 34 | < 0.01 |
| % of visits where a water point was on school grounds, functional | 82 (34) | 45 (50) | 37 | < 0.01 | 47 (46) | 35 | < 0.01 |
| % of visits where schools met sanitation target: at least one improved latrine that is clean and with no cracks in floors/walls/ceiling for every 70 pupils and latrines are sex segregated | 44 (42) | 11 (31) | 33 | < 0.01 | 5 (18) | 39 | < 0.01 |
| % of visits was a pupil latrine was on school grounds, any | 97 (15) | 79 (41) | 18 | < 0.01 | 83 (35) | 15 | 0.01 |
| % of visits where there was at least one improved latrine per 70 pupils | 71 (43) | 56 (50) | 15 | 0.02 | 39 (45) | 32 | < 0.01 |
| % of visits where there was at least one clean improved latrine per 70 pupils | 54 (41) | n/a§ | – | – | 21 (35) | 33 | < 0.01 |
| % of visits where there was at least one improved latrine with no cracks in floors/walls/ceiling per 70 pupils | 69 (42) | n/a§ | – | – | 34 (44) | 35 | < 0.01 |
| % of visits where there were sex-segregated latrines | 74 (38) | 26 (44) | 48 | < 0.01 | 14 (30) | 60 | < 0.01 |
| % of visits where schools met handwashing target: at least one handwashing container with water and soap available to pupils | 59 (36) | 20 (41) | 39 | < 0.01 | 5 (18) | 54 | < 0.01 |
| % of visits where a handwashing container was present | 81 (33) | 39 (49) | 42 | < 0.01 | 9 (24) | 72 | < 0.01 |
| % of visits where a handwashing container was present with water | 74 (36) | n/a§ | – | – | 8 (22) | 66 | < 0.01 |
| % of visits where a handwashing container was present with soap | 57 (36) | n/a§ | – | – | 5 (18) | 52 | < 0.01 |
| % of visits where schools met WASH supplies target: All WASH supplies present | 76 (29) | 9 (28) | 65 | < 0.01 | 9 (23) | 65 | < 0.01 |
| % of visits where a drinking water container was present | 96 (15) | 49 (50) | 47 | < 0.01 | 57 (44) | 39 | < 0.01 |
| % of visits where a kettle was present | 98 (9) | 37 (49) | 61 | < 0.01 | 53 (44) | 45 | < 0.01 |
| % of visits where detergent or bleach was present | 86 (24) | 37 (49) | 49 | < 0.01 | 27 (38) | 59 | < 0.01 |
| % of visits where soap was present | 88 (21) | 37 (49) | 51 | < 0.01 | 21 (33) | 67 | < 0.01 |
SD = standard deviation; WASH = water, sanitation, and hygiene.
Comparing beneficiary schools between follow-up and baseline. P values based on linear regression models accounting for repeated observations within schools.
Comparing beneficiary schools to matched control schools at follow-up. P values based on linear regression models controlling for the effect of the matching cluster.
Percentages were calculated by aggregating averages across rounds for individual schools and then taking the mean within each intervention arm.
Baseline information was not available for some individual criteria.
Health and educational outcomes.
We assessed several health and educational outcomes: 1) roll-call absence in the previous week (any absence versus none), 2) pupil-reported absence in the past week (any versus none), 3) pupil-reported diarrhea in the past week (any versus none), and 4) pupil-reported respiratory infection symptoms in the previous week (any versus none).
Roll-call absence was collected on all pupils and was defined as absence at the time of the roll call. Pupil-reported absence was collected by asking present pupils from grades 3–6 whether they had been absent half a day or more in the previous week, with pupils from the subsample who were absent that day also noted as absent. Diarrhea and respiratory infection were both collected by asking present pupils from grades 3–6 whether they had diarrhea or respiratory infection symptoms in the past week. The case definition of diarrhea was three or more loose/watery stools in a 24-hour period.19 Pupils reporting any cough, runny nose, stuffy nose, or sore throat were defined as having respiratory infection symptoms.
Analysis.
All data were analyzed using STATA, version 14 (StataCorp, College Station, TX). We first discuss the analysis measuring the performance of the program on achieving WASH performance targets, and then the analysis measuring the impact of achievement of these WASH targets on health and educational outcomes.
The DCIM intervention was not fully implemented in all of the sample beneficiary schools until the third round of data collection that took place in October 2013, and so we only use data from rounds 3–6 in this analysis. Individual schools' performance at meeting the WASH target indicators often varied between data collection rounds. Our goal of collecting these indicators at multiple time points was to be able to have an overall picture of how often these schools were adhering to the interventions. To fulfill this purpose, we aggregated the data from all of the rounds under study and created a proportion variable. For this variable, a value of one (or 100%) represents total achievement of a single WASH target or criterion at all rounds, a value of zero represents no achievement at all rounds, and values between zero and one represented varied achievement across the study rounds. We use these aggregate variables in each of our analyses.
Impact of the program on achievement of WASH targets.
WASH performance targets and criteria were assessed for associations between beneficiary schools at baseline and follow-up as well as between beneficiary schools and control schools at follow-up. For the comparison between beneficiary schools at baseline and follow-up, mixed-effects linear regression models were used, including random intercepts in the models to account for repeated measures over time. For the comparison between beneficiary and control schools at follow-up, mixed-effects linear regression models controlling for the matching cluster were used. Results were stratified by implementation year to determine program sustainability. Point estimates, absolute percentage differences, and P values are reported for each comparison.
Impact of the WASH targets on health and educational outcomes.
We used the four standardized WASH performance targets as our “exposure” variables of interest. We also sought to understand the aggregate effects of achievement of multiple WASH targets, rather than just to each separately. In our analyses, we calculated the sum of each of the previously discussed aggregated WASH targets to create an ordinal variable with integers ranging from 0 to 4. For this WASH target variable, a value of four represents achievement of each of the four WASH targets across all rounds of data collection, a value of zero represents no achievement of any of the WASH targets across all rounds, and values between zero and four represent varying achievement across rounds and/or across targets.
To adjust for non-WASH factors that might also be associated with our outcomes of interest, we included a number of control variables in our models. The control variables were the educational district matching cluster, time of year, school enrollment, urban or rural zone, pupil grade, and pupil sex. All confounder variables were specified a priori.
We used multilevel, mixed-effects logistic regression models to assess the association between each of the four WASH performance targets and each of the outcomes, controlling for the covariates listed earlier and accounting for clustering of pupils within schools and repeated measures of pupils over time. We also used similarly adjusted multilevel, mixed-effects logistic regression models to assess the association between the overall WASH target variable and each of the outcomes. The overall WASH target variable was included in the models using indicator variables to calculate estimates for each adherence level. A separate model was also run including the ordinal variable to calculate a P trend. We included random intercepts in the models to account for clustering of pupils within schools and of repeated measures of students over time. The models were used to produce adjusted odds ratio (OR) estimates for each of the associations of interest.
Ethical approval.
Ethical approval was obtained by Emory University's Institutional Review Board (Atlanta, GA), the Mali Ministry of Education, and the Center National de la Recherche Scientifique et Technique (Bamako, Mali). We obtained “in loco parentis” consent from the school director and the school management committee in each school. All pupils why received a survey gave verbal assent. The trial was registered at ClinicalTrials.gov (NCT01787058).
Results
Achievement of WASH targets.
Baseline data were available for 94 of the beneficiary schools; six of the beneficiary schools were enrolled in the program following baseline data collection. Half of the beneficiary schools received the complete DCIM intervention in 2013, 26% in 2012, and 23% in 2011.
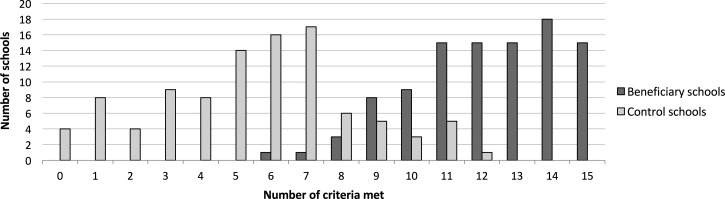
At follow-up, beneficiary schools were more likely to meet each of the targets and criteria for drinking water supply, sanitation, handwashing, and WASH supplies compared with both the beneficiary schools at baseline and the matched control schools. On average, beneficiary schools met all four WASH targets and 15 corresponding criteria at 23% of follow-up observations. None of the control schools or the beneficiary schools at baseline met all of the targets. Figure 1 shows the number of control and beneficiary schools that met different counts of the criteria averaged across the follow-up visits. The distributions for the beneficiary and control histograms were distinct, with beneficiary schools meeting an average of 12.2 (95% confidence interval [CI] = 11.7–12.6) criteria while control schools met 5.5 (95% CI = 4.9–6.1).
Figure 1.
Distribution of the number of WASH criteria met at beneficiary and control schools (number of criteria is averaged across all follow-up rounds).
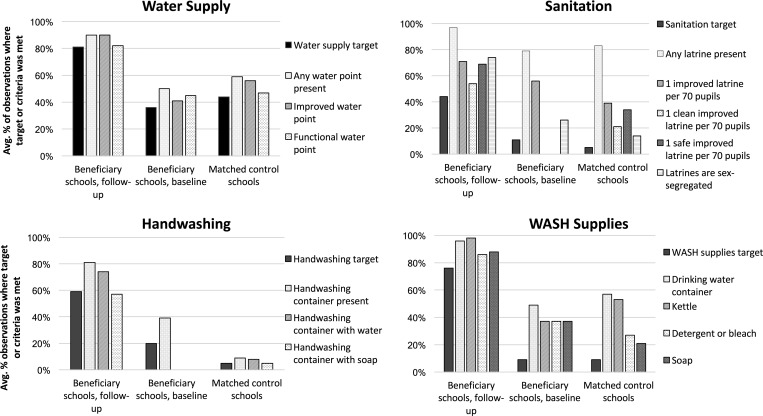
School performance at meeting each of the targets and their criteria is shown in Figure 2 . At follow-up, beneficiary schools were most likely to meet the water supply target (81%) followed by the WASH supplies (76%) and handwashing (59%) targets, with fewest schools meeting the sanitation target (44%, Table 2). Ten percent of beneficiary schools did not receive a water point, while at a further 8% of observations a water point was present, but it was nonfunctional. At 29% of observations, beneficiary schools did not have a sufficient number of accessible latrines to meet the predetermined ratio of 70 pupils per latrine, at 26% of observations schools did not maintain sex separation in the latrines, and a lack of cleanliness among existing latrines was found at 17% of observations. At 26% of observations, beneficiary schools lacked handwashing water and, although schools had soap at 88% of observations, soap was present at handwashing containers only 57% of observations. Fourteen percent of the time beneficiary schools did not have bleach or detergent for cleaning and soap was not present at 12% of observations.
Figure 2.
Mean percentage of schools that met WASH performance targets and criteria.
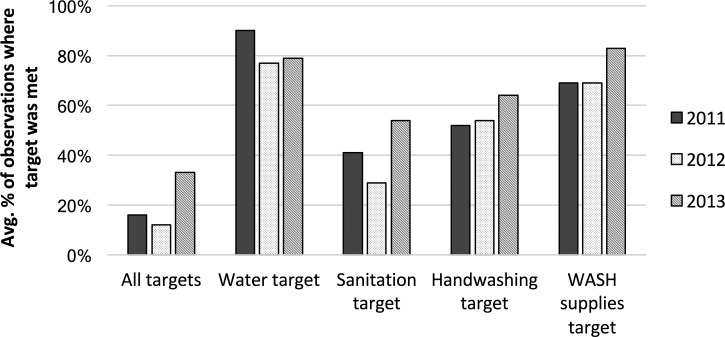
Figure 3 presents the rare at which beneficiary schools achieved the WASH performance targets by the year of implementation, and can provide some insight into the sustainability of the program. Schools where the program was implemented in 2013 met all four targets 32.7% of the time, twice as often as schools where the program was implemented in 2012 (11.5%) or 2011 (15.9%). The 2013 schools also performed somewhat better at meeting the sanitation (2013, 53.9%; 2012, 28.5%; 2011, 40.9%), handwashing (2013, 63.9%; 2012, 54.5%; 2011, 51.8%), and WASH supplies (2013, 82.5%; 2012, 68.9%; 2011, 68.8%) targets. Schools where the program was implemented in 2011 performed best at meeting the water supply target (2013, 79.1%; 2012, 77.2%; 2011, 90.0%), likely due to the fact that not all schools in the later groups received water points due to budgetary and environmental restrictions.
Figure 3.
Mean percentage of beneficiary schools that met WASH performance targets at follow-up by the year of program implementation.
Impact of the WASH targets on health and educational outcomes.
Absence.
When considering the WASH targets individually, only handwashing was associated with a higher odds of roll-call absence (OR = 1.37; 95% CI = 1.01–1.84; P = 0.04; Table 3), whereas the other three targets were not associated with roll-call absence. Achievement of a greater number WASH targets was not associated with differences in roll-call absence (P trend = 0.14). Pupils attending those schools that met all of the WASH targets had similar odds of absence as pupils in schools that met none of the targets (OR = 1.06; 95% CI = 0.81–1.39; P = 0.65). We found no associations between any of the WASH targets, individually or collectively, and pupil-reported absence.
Table 3.
ORs comparing achievement of WASH targets among pupils attending 200 Malian primary schools
| aOR (95% CI) | P | P trend | |
|---|---|---|---|
| Roll call absence | |||
| WASH components model* | n/a | ||
| Sanitation target | 0.97 (0.76–1.22) | 0.77 | |
| Water supply target | 0.90 (0.73–1.10) | 0.32 | |
| Handwashing target | 1.37 (1.01–1.84) | 0.04 | |
| WASH supplies target | 0.98 (0.74–1.30) | 0.91 | |
| Achievement of WASH targets model* | 0.14 | ||
| 0 targets met | Referent | ||
| > 0–1 targets met | 0.94 (0.76–1.18) | 0.62 | |
| > 1–2 targets met | 0.90 (0.72–1.14) | 0.39 | |
| > 2–3 targets met | 1.18 (0.94–1.49) | 0.14 | |
| > 3–4 targets met | 1.06 (0.81–1.39) | 0.65 | |
| Pupil-reported absence | |||
| WASH components model* | n/a | ||
| Sanitation target | 0.96 (0.74–1.24) | 0.76 | |
| Water supply target | 1.04 (0.84–1.31) | 0.69 | |
| Handwashing target | 0.79 (0.57–1.09) | 0.15 | |
| WASH supplies target | 1.13 (0.83–1.53) | 0.43 | |
| Achievement of WASH targets model* | 0.41 | ||
| 0 targets met | Referent | ||
| > 0–1 targets met | 0.85 (0.67–1.08) | 0.19 | |
| > 1–2 targets met | 0.90 (0.70–1.15) | 0.40 | |
| > 2–3 targets met | 0.91 (0.71–1.17) | 0.47 | |
| > 3–4 targets met | 0.83 (0.62–1.11) | 0.20 | |
aOR = adjusted odds ratio; CI = confidence interval; WASH = water, sanitation, and hygiene.
The adjusted model controlled for educational district matching cluster, time of year, school enrollment, urban or rural zone, pupil grade, and pupil sex, and for clustering of pupils within schools and for repeated measures of pupils over time.
Diarrhea.
Only the sanitation target was associated with a lower odds of diarrhea (OR = 0.68; 95% CI = 0.50–0.93; P = 0.02; Table 4 ), whereas the other three targets were not associated with diarrhea. Increasing achievement of all of the WASH targets together was strongly associated with a lower odds of diarrhea among pupils (P trend < 0.01). Pupils attending schools that met all of the WASH targets had a lower odds of diarrhea than pupils attending schools that met none of the targets (OR = 0.65; 95% CI = 0.47–0.92; P = 0.01).
Table 4.
ORs comparing achievement of WASH targets and health outcomes among pupils attending 200 Malian primary schools
| aOR (95% CI) | P | P trend | |
|---|---|---|---|
| Pupil-reported diarrhea | |||
| WASH components model* | n/a | ||
| Sanitation target | 0.68 (0.50–0.93) | 0.02 | |
| Water supply target | 0.81 (0.62–1.05) | 0.11 | |
| Handwashing target | 1.01 (0.68–1.49) | 0.95 | |
| WASH supplies target | 0.96 (0.67–1.38) | 0.83 | |
| Achievement of WASH targets model* | < 0.01 | ||
| 0 targets met | Referent | ||
| > 0–1 targets met | 0.77 (0.58–0.12) | 0.06 | |
| > 1–2 targets met | 0.58 (0.43–0.78) | < 0.01 | |
| > 2–3 targets met | 0.56 (0.42–0.75) | < 0.01 | |
| > 3–4 targets met | 0.65 (0.47–0.92) | 0.01 | |
| Pupil-reported respiratory symptoms | |||
| WASH components model* | n/a | ||
| Sanitation target | 0.97 (0.75–1.25) | 0.80 | |
| Water supply target | 0.97 (0.79–1.21) | 0.79 | |
| Handwashing target | 0.80 (0.58–1.11) | 0.18 | |
| WASH supplies target | 0.89 (0.66–1.20) | 0.47 | |
| Achievement of WASH targets model* | < 0.01 | ||
| 0 targets met | Referent | ||
| > 0–1 targets met | 1.16 (0.92–1.47) | 0.22 | |
| > 1–2 targets met | 0.96 (0.74–1.23) | 0.73 | |
| > 2–3 targets met | 0.84 (0.66–1.07) | 0.17 | |
| > 3–4 targets met | 0.75 (0.56–1.00) | 0.04 | |
aOR = adjusted odds ratio; CI = confidence interval; WASH = water, sanitation, and hygiene.
The adjusted model controlled for educational district matching cluster, time of year, school enrollment, urban or rural zone, pupil grade, and pupil sex, and for clustering of pupils within schools and for repeated measures of pupils over time.
Respiratory symptoms.
None of the WASH targets were individually associated with respiratory symptoms, although all were in the preventive direction (Table 4). However, when considered collectively, increasing achievement of all of the WASH targets together was associated with a lower odds of pupils having respiratory symptoms (P trend < 0.01).
Discussion
In our assessment of program fidelity and adherence, we found that beneficiary schools had improved WASH environments compared with the control schools. Although beneficiary schools were found to meet all four WASH targets (and 15 criteria) at only 23% of follow-up visits on average, the beneficiary schools exhibited considerable gains in WASH access compared both to the matched control schools and to the beneficiary schools at baseline. Beneficiary schools appeared to face some challenges in sustaining their WASH programs over time, as schools that received the intervention in 2013 (closer in time to the 2013–2014 evaluation period) met more WASH targets than schools that received the intervention in 2012 and 2011. We also observed that increased access and adherence to the WASH targets was important for improving health, but not absence, and particularly with fidelity and adherence to multiple WASH targets together.
Impact of WASH targets on health and educational outcomes.
Our findings revealed somewhat novel results about the contributions of WASH on health and educational outcomes than did the initial ITT analysis.9 The ITT results showed a significant preventive association between the comprehensive intervention and diarrhea (OR = 0.71; 95% CI = 0.60–0.85; P < 0.01).9 We observed in our as-treated study that the sanitation component was the target the most strongly associated with improved diarrhea outcomes. We also observed that increasing achievement of multiple WASH components was associated with lower diarrhea. For respiratory symptoms, the ITT analysis found a significant association with the intervention (OR = 0.75; 95% CI = 0.65–0.86; P < 0.01).9 In our as-treated analysis, we did not find an association with any individual WASH targets; however, achievement of all WASH components was associated with lower respiratory infection prevalence. Achievement of targets within multiple WASH components may be important for preventing both diarrhea and respiratory symptoms. This points to the importance of interventions that address multiple routes of transmission (i.e., WASH), an issue that has been challenged in a review that found multiple interventions, were no more effective than single interventions in community settings,20 and is subject to an ongoing multicenter study.21 We report elsewhere on the positive impact of the intervention on reducing absence due to diarrhea and respiratory infection9; as this was a secondary outcome of the study, we did not further explore this analysis.
The ITT results revealed no association with pupil-reported absence (OR = 0.93; 95% CI = 0.79–1.09; P = 0.38), and higher rates of roll-call absence among beneficiary schools compared with the control schools (OR = 1.23; 95% CI = 1.06–1.42; P < 0.01).9 We also did not find any associations here between achievement of WASH targets and pupil-reported absence. For roll-call absence, we observed that only the handwashing target was associated with increased absence, although it is not clear what the biological mechanism might be that could explain this counter-intuitive finding. We otherwise did not observe any associations or trends between achievement of WASH targets and roll-call absence. Taken together, the biological mechanism and adherence trends for our as-treated results suggest plausibility of the associations between the WASH targets and diarrhea and respiratory symptoms, whereas the as-treated results for the absence outcomes suggest that there was no effect of the intervention on absence and that the previously reported negative ITT results for roll-call absence may have been due to something besides the interventions, such as the limitations of the matched study design and civil unrest that occurred throughout the study time period. Future WASH evaluation studies that are found to have suboptimal adherence may benefit from an as-treated, per-protocol, or instrumental variable analysis to supplement the ITT results.
Achievement of WASH targets.
Among the four predetermined WASH targets, water access was most frequently attained. Only 10% of schools did not receive a water point, a result confined to one program partner due to the hydrogeological and budget constraints discussed earlier, pointing to high level of program fidelity. Only 8% of school water points were not functional at the time of observation, suggesting a high level of construction quality and beneficiary adherence to the maintenance of the water points. The rate of functionality of the water point was high compared with national averages from other sub-Saharan African contexts (70–80% 1–3 years after construction).22 Where water points had been constructed or rehabilitated in 2011, 3 years before the evaluation, over 90% of schools met the water access target, indicating that the program ensured high access to water in that period and sustained this result following the intervention.
Although WASH supplies were provided by the program as a one-time donation, beneficiary schools were largely able to maintain the presence of these supplies, particularly durable items such as water containers and anal cleansing kettles. Consumable supplies such as detergent and bleach were less likely to be present, suggesting the need for improvements in budgetary allocations for the recurrent costs of consumable supplies. Schools where the program was implemented in 2011 or 2012 were less likely to have all elements of the WASH supply list, indicating a potential lack of sustained replacement of supplies as they were exhausted or damaged over time.
Handwashing containers were present in schools at 81% of observations; however, schools did not always ensure that these containers had water or soap nearby. Ensuring that pupils had access to soap was a particular challenge; although handwashing soap was observed to be present at 88% of beneficiary schools on average, soap was observed next to a handwashing station only 57% of the time. These results are in line with an in-progress review that reported the functionality rate of school handwashing facilities as being between 0% and 70%23 and somewhat better than a trial in Kenya which found soap in 40% of schools, though in Kenya soap was never provided directly by the program.7 In our study, the discrepancy between soap being present at schools and being available to pupils may in part be due to the practice of reserving soap in the school director's office to prevent loss or theft, which discourages pupils from using soap for handwashing. Alternatively, there may have been insufficient changes to norms and habits to influence either the teachers to put out the soap on a daily basis, or for children to request soap when none was put out for use. A slightly higher percentage of schools met the handwashing target in the schools where the program had been implemented in 2013 compared with 2012 and 2011, indicating a potential drop-off in ensuring continued provision of water and soap for pupil handwashing over time. Alternatively, the implementing agencies may have improved their strategies for promoting soap provision over the course of the program, enabling better results.
Nearly all beneficiary schools were observed to have latrines available to pupils on the school grounds, again pointing to high level of program fidelity. However, nearly 30% of beneficiary schools exceeded the target ratio of 1 latrine per 70 pupils. This was in part due to the practice of locking latrine doors, which some schools undertake to prevent misuse or to extend latrine life by alternating which latrines are used. Latrines were not included in calculation of the target if they were locked; even if keys are available to pupils on demand, this practice can discourage the use of latrines. Schools also faced challenges in ensuring latrine cleanliness and enforcing separation of the latrines by sex. Stratified analyses by the year of implementation suggest that the ability of schools to sustain access to latrines varied over time.
Overall, schools where the DCIM intervention was implemented in 2013 were twice as likely to meet all four WASH performance targets as schools where the program was implemented in 2011. This is unsurprising when considering that failure to meet even one of the 15 individual criteria precludes a school from attaining this global standard, and the likelihood of encountering at least one case of missing materials or broken infrastructure would increase over time. Improved performance among schools in the 2013 cohort may also have been due to changes in implementation as the program progressed, suggesting the benefit from continuous learning and program improvement, and the ability of this program to do so.
Limitations.
Our study had several limitations. The matching, along with the inclusion of additional control variables in the models, was done to minimize confounding; however, there is still the possibility of confounding by unknown or unmeasured confounders (as is the case for all nonrandomized studies). A limitation of our study is that we did not have reliable baseline data, especially in control schools. The lack of baseline data limits our ability to ensure equivalent groups at baseline, control for differences in the outcome variable at baseline, or to control for other baseline covariates in our model. We did match on two key predictors, presence of school toilets and access to water at the school. Although there is biological plausibility supporting our second study question—that is, to assess the associations between school WASH adherence and health and educational outcomes—it is alternatively possible that schools that adhere to WASH may have been fundamentally different than nonadherent schools in some way that was not accounted for in our models. For example, this may have influenced the absenteeism results discussed earlier. For our other study aim—that is, to assess the impact of the intervention on project fidelity and WASH adherence—it is difficult to conceptualize any potential confounder that could have led to such dramatic and consistent increases across all 15 WASH criteria and all four WASH targets (comparing beneficiary schools to both the control group and to beneficiary schools at baseline).
Another limitation is that several of the health and education outcomes were pupil reported, and so there is the possibility of reporting biases, although we used short recall periods and multiple measures of outcomes to mitigate these biases. Finally, it is unclear how the civil unrest throughout Mali might have affected our outcomes, especially absenteeism, during the study. Although this may appear to limit external validity overall, this is also not the only WASH trial to have happened during the midst of civil unrest7 and so it is probably important to understand the limitations of these types of WASH interventions among all of the various contexts where they may be implemented.
Conclusion
Our results describe both WASH target achievements and shortcomings comparing the DCIM beneficiaries to both control schools and to the beneficiary schools at baseline. The program achieved high levels of fidelity at achieving outputs such as provision of improved, functional water supply, improved latrines, handwashing stations, and WASH supplies, but more limited adherence among beneficiaries, such as provision of soap at handwashing stations, enforcement of the sex-segregated use of latrines, and latrine cleaning. A critical gap across the WASH sector are innovative and effective ways to ensure behavior change and habit formation among teachers and pupils to ensure adherence to toilet maintenance and daily soap provision for students. There is evidence of a slight decline in the sustainability of the WASH program over the 3-year period covered by the study, indicating the need for further improvements in ensuring that schools have the motivation and resources to maintain their WASH systems over time. We found that increased access and adherence to multiple WASH components was important for improving health but that there was no effect of the intervention on pupil absence. These findings suggest that a comprehensive WASH intervention and a focus on increasing adherence may help maximize the health effects of school WASH programs, but that WASH alone might not be sufficient to decrease pupils' absenteeism.
ACKNOWLEDGMENTS
We would like to thank the Government and people of Mali as well as the tireless research team, including Karim Diamoutene, Alpha Oumar Haidara, Nouhoum Kone, Moussa Samake, Seydou Samaké, Yacouba Sogore, Abdoulaye Sow, Fatoumata Habib Traoré, and Salif Ismaïla Traoré. We also thank the UNICEF, WaterAid, CARE, Oxfam, and Save the Children teams for their support, specifically Jérémie Toubkiss, Heather Murphy, Lahatra Rakotondradalo, Yagouba Diallo, Seydou Niafo, Toureba Keita, Assitan Sogoré, Salimata Togola, Soma Konaré, Salia Diallo, Mamadou Kanté, Fatoumata Haidara, Mamadou Diallo, Zoumana Cisse, Ousmane Haidara, and Thierno Bocoum. Thanks to Sarah Porter who supported the initial proposal development.
Disclaimer: The funder had no involvement in its design, in collection, analysis, or interpretation of the data, or in the preparation of this manuscript.
Footnotes
Financial support: Funding for this impact evaluation was provided by Dubai Cares Foundation.
Authors' addresses: Joshua V. Garn, Victoria Trinies, and Matthew C. Freeman, Department of Environmental Health, Rollins School of Public Health, Emory University, Atlanta, GA, E-mails: jgarn@emory.edu, vtrinies@gmail.com, and matthew.freeman@emory.edu. Jérémie Toubkiss, Evaluation Office, The United Nations Children's Fund Headquarter, New York City, NY, E-mail: jtoubkiss@unicef.org.
References
- 1.Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A, Delwiche K, Estep K, Frostad JJ, Astha KC, Kyu HH, Moradi-Lakeh M, Ng M, Slepak EL, Thomas BA, Wagner J, Aasvang GM, Abbafati C, Abbasoglu Ozgoren A, Abd-Allah F, Abera SF, Aboyans V, Abraham B, Abraham JP, Abubakar I, Abu-Rmeileh NM, Aburto TC, Achoki T, Adelekan A, Adofo K, Adou AK, Adsuar JC, Afshin A, Agardh EE, Al Khabouri MJ, Al Lami FH, Alam SS, Alasfoor D, Albittar MI, Alegretti MA, Aleman AV, Alemu ZA, Alfonso-Cristancho R, Alhabib S, Ali R, Ali MK, Alla F, Allebeck P, Allen PJ, Alsharif U, Alvarez E, Alvis-Guzman N, Amankwaa AA, Amare AT, Ameh EA, Ameli O, Amini H, Ammar W, Anderson BO, Antonio CA, Anwari P, Argeseanu Cunningham S, Arnlöv J, Arsenijevic VS, Artaman A, Asghar RJ, Assadi R, Atkins LS, Atkinson C, Avila MA, Awuah B, Badawi A, Bahit MC, Bakfalouni T, Balakrishnan K, Balalla S, Balu RK, Banerjee A, Barber RM, Barker-Collo SL, Barquera S, Barregard L, Barrero LH, Barrientos-Gutierrez T, Basto-Abreu AC, Basu A, Basu S, Basulaiman MO, Batis Ruvalcaba C, Beardsley J, Bedi N, Bekele T, Bell ML, Benjet C, Bennett DA, Benzian H, Bernabé E, Beyene TJ, Bhala N, Bhalla A, Bhutta ZA, Bikbov B, Bin Abdulhak AA, Blore JD, Blyth FM, Bohensky MA, Bora Başara B, Borges G, Bornstein NM, Bose D, Boufous S, Bourne RR, Brainin M, Brazinova A, Breitborde NJ, Brenner H, Briggs AD, Broday DM, Brooks PM, Bruce NG, Brugha TS, Brunekreef B, Buchbinder R, Bui LN, Bukhman G, Bulloch AG, Burch M, Burney PG, Campos-Nonato IR, Campuzano JC, Cantoral AJ, Caravanos J, Cárdenas R, Cardis E, Carpenter DO, Caso V, Castañeda-Orjuela CA, Castro RE, Catalá-López F, Cavalleri F, Çavlin A, Chadha VK, Chang JC, Charlson FJ, Chen H, Chen W, Chen Z, Chiang PP, Chimed-Ochir O, Chowdhury R, Christophi CA, Chuang TW, Chugh SS, Cirillo M, Claßen TK, Colistro V, Colomar M, Colquhoun SM, Contreras AG, Cooper C, Cooperrider K, Cooper LT, Coresh J, Courville KJ, Criqui MH, Cuevas-Nasu L, Damsere-Derry J, Danawi H, Dandona L, Dandona R, Dargan PI, Davis A, Davitoiu DV, Dayama A, de Castro EF, De la Cruz-Góngora V, De Leo D, de Lima G, Degenhardt L, del Pozo-Cruz B, Dellavalle RP, Deribe K, Derrett S, Des Jarlais DC, Dessalegn M, deVeber GA, Devries KM, Dharmaratne SD, Dherani MK, Dicker D, Ding EL, Dokova K, Dorsey ER, Driscoll TR, Duan L, Durrani AM, Ebel BE, Ellenbogen RG, Elshrek YM, Endres M, Ermakov SP, Erskine HE, Eshrati B, Esteghamati A, Fahimi S, Faraon EJ, Farzadfar F, Fay DF, Feigin VL, Feigl AB, Fereshtehnejad SM, Ferrari AJ, Ferri CP, Flaxman AD, Fleming TD, Foigt N, Foreman KJ, Paleo UF, Franklin RC, Gabbe B, Gaffikin L, Gakidou E, Gamkrelidze A, Gankpé FG, Gansevoort RT, García-Guerra FA, Gasana E, Geleijnse JM, Gessner BD, Gething P, Gibney KB, Gillum RF, Ginawi IA, Giroud M, Giussani G, Goenka S, Goginashvili K, Gomez Dantes H, Gona P, Gonzalez de Cosio T, González-Castell D, Gotay CC, Goto A, Gouda HN, Guerrant RL, Gugnani HC, Guillemin F, Gunnell D, Gupta R, Gupta R, Gutiérrez RA, Hafezi-Nejad N, Hagan H, Hagstromer M, Halasa YA, Hamadeh RR, Hammami M, Hankey GJ, Hao Y, Harb HL, Haregu TN, Haro JM, Havmoeller R, Hay SI, Hedayati MT, Heredia-Pi IB, Hernandez L, Heuton KR, Heydarpour P, Hijar M, Hoek HW, Hoffman HJ, Hornberger JC, Hosgood HD, Hoy DG, Hsairi M, Hu G, Hu H, Huang C, Huang JJ, Hubbell BJ, Huiart L, Husseini A, Iannarone ML, Iburg KM, Idrisov BT, Ikeda N, Innos K, Inoue M, Islami F, Ismayilova S, Jacobsen KH, Jansen HA, Jarvis DL, Jassal SK, Jauregui A, Jayaraman S, Jeemon P, Jensen PN, Jha V, Jiang F, Jiang G, Jiang Y, Jonas JB, Juel K, Kan H, Kany Roseline SS, Karam NE, Karch A, Karema CK, Karthikeyan G, Kaul A, Kawakami N, Kazi DS, Kemp AH, Kengne AP, Keren A, Khader YS, Khalifa SE, Khan EA, Khang YH, Khatibzadeh S, Khonelidze I, Kieling C, Kim D, Kim S, Kim Y, Kimokoti RW, Kinfu Y, Kinge JM, Kissela BM, Kivipelto M, Knibbs LD, Knudsen AK, Kokubo Y, Kose MR, Kosen S, Kraemer A, Kravchenko M, Krishnaswami S, Kromhout H, Ku T, Kuate Defo B, Kucuk Bicer B, Kuipers EJ, Kulkarni C, Kulkarni VS, Kumar GA, Kwan GF, Lai T, Lakshmana Balaji A, Lalloo R, Lallukka T, Lam H, Lan Q, Lansingh VC, Larson HJ, Larsson A, Laryea DO, Lavados PM, Lawrynowicz AE, Leasher JL, Lee JT, Leigh J, Leung R, Levi M, Li Y, Li Y, Liang J, Liang X, Lim SS, Lindsay MP, Lipshultz SE, Liu S, Liu Y, Lloyd BK, Logroscino G, London SJ, Lopez N, Lortet-Tieulent J, Lotufo PA, Lozano R, Lunevicius R, Ma J, Ma S, Machado VM, MacIntyre MF, Magis-Rodriguez C, Mahdi AA, Majdan M, Malekzadeh R, Mangalam S, Mapoma CC, Marape M, Marcenes W, Margolis DJ, Margono C, Marks GB, Martin RV, Marzan MB, Mashal MT, Masiye F, Mason-Jones AJ, Matsushita K, Matzopoulos R, Mayosi BM, Mazorodze TT, McKay AC, McKee M, McLain A, Meaney PA, Medina C, Mehndiratta MM, Mejia-Rodriguez F, Mekonnen W, Melaku YA, Meltzer M, Memish ZA, Mendoza W, Mensah GA, Meretoja A, Mhimbira FA, Micha R, Miller TR, Mills EJ, Misganaw A, Mishra S, Mohamed Ibrahim N, Mohammad KA, Mokdad AH, Mola GL, Monasta L, Montañez Hernandez JC, Montico M, Moore AR, Morawska L, Mori R, Moschandreas J, Moturi WN, Mozaffarian D, Mueller UO, Mukaigawara M, Mullany EC, Murthy KS, Naghavi M, Nahas Z, Naheed A, Naidoo KS, Naldi L, Nand D, Nangia V, Narayan KM, Nash D, Neal B, Nejjari C, Neupane SP, Newton CR, Ngalesoni FN, Ngirabega Jde D, Nguyen G, Nguyen NT, Nieuwenhuijsen MJ, Nisar MI, Nogueira JR, Nolla JM, Nolte S, Norheim OF, Norman RE, Norrving B, Nyakarahuka L, Oh IH, Ohkubo T, Olusanya BO, Omer SB, Opio JN, Orozco R, Pagcatipunan RS, Jr, Pain AW, Pandian JD, Panelo CI, Papachristou C, Park EK, Parry CD, Paternina Caicedo AJ, Patten SB, Paul VK, Pavlin BI, Pearce N, Pedraza LS, Pedroza A, Pejin Stokic L, Pekericli A, Pereira DM, Perez-Padilla R, Perez-Ruiz F, Perico N, Perry SA, Pervaiz A, Pesudovs K, Peterson CB, Petzold M, Phillips MR, Phua HP, Plass D, Poenaru D, Polanczyk GV, Polinder S, Pond CD, Pope CA, Pope D, Popova S, Pourmalek F, Powles J, Prabhakaran D, Prasad NM, Qato DM, Quezada AD, Quistberg DA, Racapé L, Rafay A, Rahimi K, Rahimi-Movaghar V, Rahman SU, Raju M, Rakovac I, Rana SM, Rao M, Razavi H, Reddy KS, Refaat AH, Rehm J, Remuzzi G, Ribeiro AL, Riccio PM, Richardson L, Riederer A, Robinson M, Roca A, Rodriguez A, Rojas-Rueda D, Romieu I, Ronfani L, Room R, Roy N, Ruhago GM, Rushton L, Sabin N, Sacco RL, Saha S, Sahathevan R, Sahraian MA, Salomon JA, Salvo D, Sampson UK, Sanabria JR, Sanchez LM, Sánchez-Pimienta TG, Sanchez-Riera L, Sandar L, Santos IS, Sapkota A, Satpathy M, Saunders JE, Sawhney M, Saylan MI, Scarborough P, Schmidt JC, Schneider IJ, Schöttker B, Schwebel DC, Scott JG, Seedat S, Sepanlou SG, Serdar B, Servan-Mori EE, Shaddick G, Shahraz S, Levy TS, Shangguan S, She J, Sheikhbahaei S, Shibuya K, Shin HH, Shinohara Y, Shiri R, Shishani K, Shiue I, Sigfusdottir ID, Silberberg DH, Simard EP, Sindi S, Singh A, Singh GM, Singh JA, Skirbekk V, Sliwa K, Soljak M, Soneji S, Søreide K, Soshnikov S, Sposato LA, Sreeramareddy CT, Stapelberg NJ, Stathopoulou V, Steckling N, Stein DJ, Stein MB, Stephens N, Stöckl H, Straif K, Stroumpoulis K, Sturua L, Sunguya BF, Swaminathan S, Swaroop M, Sykes BL, Tabb KM, Takahashi K, Talongwa RT, Tandon N, Tanne D, Tanner M, Tavakkoli M, Te Ao BJ, Teixeira CM, Téllez Rojo MM, Terkawi AS, Texcalac-Sangrador JL, Thackway SV, Thomson B, Thorne-Lyman AL, Thrift AG, Thurston GD, Tillmann T, Tobollik M, Tonelli M, Topouzis F, Towbin JA, Toyoshima H, Traebert J, Tran BX, Trasande L, Trillini M, Trujillo U, Dimbuene ZT, Tsilimbaris M, Tuzcu EM, Uchendu US, Ukwaja KN, Uzun SB, van de Vijver S, Van Dingenen R, van Gool CH, van Os J, Varakin YY, Vasankari TJ, Vasconcelos AM, Vavilala MS, Veerman LJ, Velasquez-Melendez G, Venketasubramanian N, Vijayakumar L, Villalpando S, Violante FS, Vlassov VV, Vollset SE, Wagner GR, Waller SG, Wallin MT, Wan X, Wang H, Wang J, Wang L, Wang W, Wang Y, Warouw TS, Watts CH, Weichenthal S, Weiderpass E, Weintraub RG, Werdecker A, Wessells KR, Westerman R, Whiteford HA, Wilkinson JD, Williams HC, Williams TN, Woldeyohannes SM, Wolfe CD, Wong JQ, Woolf AD, Wright JL, Wurtz B, Xu G, Yan LL, Yang G, Yano Y, Ye P, Yenesew M, Yentür GK, Yip P, Yonemoto N, Yoon SJ, Younis MZ, Younoussi Z, Yu C, Zaki ME, Zhao Y, Zheng Y, Zhou M, Zhu J, Zhu S, Zou X, Zunt JR, Lopez AD, Vos T, Murray CJ. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNICEF . Raising Even More Clean Hands: Advancing Health, Learning and Equity through WASH in Schools. New York, NY: UNICEF; 2012. [Google Scholar]
- 3.Bowen A, Ma H, Ou J, Billhimer W, Long T, Mintz E, Hoekstra RM, Luby S. A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. Am J Trop Med Hyg. 2007;76:1166–1173. [PubMed] [Google Scholar]
- 4.Caruso BA, Freeman MC, Garn JV, Dreibelbis R, Saboori S, Muga R, Rheingans R. Assessing the impact of a school-based latrine cleaning and handwashing program on pupil absence in Nyanza Province, Kenya: a cluster-randomized trial. Trop Med Int Health. 2014;19:1185–1197. doi: 10.1111/tmi.12360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garn JV, Greene LE, Dreibelbis R, Saboori S, Rheingans RD, Freeman MC. A cluster-randomized trial assessing the impact of school water, sanitation and hygiene improvements on pupil enrolment and gender parity in enrolment. J Water Sanit Hyg Dev. 2013;3:592–601. doi: 10.2166/washdev.2013.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freeman MC, Clasen T, Dreibelbis R, Saboori S, Greene LE, Brumback B, Muga R, Rheingans R. The impact of a school-based water supply and treatment, hygiene, and sanitation programme on pupil diarrhoea: a cluster-randomized trial. Epidemiol Infect. 2014;142:340–351. doi: 10.1017/S0950268813001118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freeman MC, Greene LE, Dreibelbis R, Saboori S, Muga R, Brumback B, Rheingans R. Assessing the impact of a school-based water treatment, hygiene and sanitation programme on pupil absence in Nyanza Province, Kenya: a cluster-randomized trial. Trop Med Int Health. 2012;17:380–391. doi: 10.1111/j.1365-3156.2011.02927.x. [DOI] [PubMed] [Google Scholar]
- 8.Rosen L, Manor O, Engelhard D, Brody D, Rosen B, Peleg H, Meir M, Zucker D. Can a handwashing intervention make a difference? Results from a randomized controlled trial in Jerusalem preschools. Prev Med. 2006;42:27–32. doi: 10.1016/j.ypmed.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Trinies V, Garn JV, Chang HH, Freeman MC. The impact of a comprehensive school WASH program on absenteeism, diarrhea, and respiratory infection symptoms: a matched-control trial in Mali. Am J Trop Med Hyg. 2016;10:1418–1425. doi: 10.4269/ajtmh.15-0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Talaat M, Afifi S, Dueger E, El-Ashry N, Marfin A, Kandeel A, Mohareb E, El-Sayed N. Effects of hand hygiene campaigns on incidence of laboratory-confirmed influenza and absenteeism in schoolchildren, Cairo, Egypt. Emerg Infect Dis. 2011;17:619–625. doi: 10.3201/eid1704.101353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freeman MC, Clasen T, Brooker SJ, Akoko DO, Rheingans R. The impact of a school-based hygiene, water quality and sanitation intervention on soil-transmitted helminth reinfection: a cluster-randomized trial. Am J Trop Med Hyg. 2013;89:875–883. doi: 10.4269/ajtmh.13-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greene LE, Freeman MC, Akoko D, Saboori S, Moe C, Rheingans R. Impact of a school-based hygiene promotion and sanitation intervention on pupil hand contamination in Western Kenya: a cluster randomized trial. Am J Trop Med Hyg. 2012;87:385–393. doi: 10.4269/ajtmh.2012.11-0633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alexander KT, Robert D, Betty O, Richard R. Improving service delivery of water, sanitation, and hygiene in primary schools: a cluster-randomized trial in western Kenya. J Water Health. 2013;11:507–519. doi: 10.2166/wh.2013.213. [DOI] [PubMed] [Google Scholar]
- 14.Garn JV, Brumback BA, Drews-Botsch CD, Lash TL, Kramer MR, Freeman MC. Estimating the effect of school water, sanitation, and hygiene improvements on pupil health outcomes. Epidemiology. 2016;27:752–760. doi: 10.1097/EDE.0000000000000522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brumback BA, He Z, Prasad M, Freeman MC, Rheingans R. Using structural-nested models to estimate the effect of cluster-level adherence on individual-level outcomes with a three-armed cluster-randomized trial. Stat Med. 2014;33:1490–1502. doi: 10.1002/sim.6049. [DOI] [PubMed] [Google Scholar]
- 16.Hernan MA, Robins JM. Instruments for causal inference: an epidemiologist's dream? Epidemiology. 2006;17:360–372. doi: 10.1097/01.ede.0000222409.00878.37. [DOI] [PubMed] [Google Scholar]
- 17.Ten Have TR, Normand SL, Marcus SM, Brown CH, Lavori P, Duan N. Intent-to-treat vs. non-intent-to-treat analyses under treatment non-adherence in mental health randomized trials. Psychiatr Ann. 2008;38:772–783. doi: 10.3928/00485713-20081201-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartung C, Anokwa Y, Brunette W, Lerer A, Tseng C, Borriello G. Proceedings of the 4th ACM/IEEE International Conference on Information and Communication Technologies and Development (ICTD) New York, NY: 2010. Open data kit: tools to build information services for developing regions. [Google Scholar]
- 19.Baqui AH, Black RE, Yunus M, Hoque AR, Chowdhury HR, Sack RB. Methodological issues in diarrhoeal diseases epidemiology: definition of diarrhoeal episodes. Int J Epidemiol. 1991;20:1057–1063. doi: 10.1093/ije/20.4.1057. [DOI] [PubMed] [Google Scholar]
- 20.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM., Jr Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005;5:42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 21.Arnold BF, Null C, Luby SP, Unicomb L, Stewart CP, Dewey KG, Ahmed T, Ashraf S, Christensen G, Clasen T, Dentz HN, Fernald LCH, Haque R, Hubbard AE, Kariger P, Leontsini E, Lin A, Njenga SM, Pickering AJ, Ram PK, Tofail F, Winch PJ, Colford JM., Jr Cluster-randomised controlled trials of individual and combined water, sanitation, hygiene and nutritional interventions in rural Bangladesh and Kenya: the WASH Benefits study design and rationale. BMJ Open. 2013;3:e003476. doi: 10.1136/bmjopen-2013-003476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carter RC, Ross I. Beyond ‘functionality’ of handpump-supplied rural water services in developing countries. Waterlines. 2016;35:94–110. [Google Scholar]
- 23.Toubkiss J, Bickel S. Equity, Scalability and Sustainability in UNICEF WASH Programming: Evidence from UNICEF Evaluations 2007–2015. New York, NY: UNICEF Evaluation Office; 2016. [Google Scholar]