Abstract
Purpose
To compare the clinical efficacy and complications of limited internal fixation combined with external fixation (LIFEF) and open reduction and internal fixation (ORIF) in the treatment of Pilon fracture.
Methods
We searched databases including Pubmed, Embase, Web of science, Cochrane Library and China Biology Medicine disc for the studies comparing clinical efficacy and complications of LIFEF and ORIF in the treatment of Pilon fracture. The clinical efficacy was evaluated by the rate of nonunion, malunion/delayed union and the excellent/good rate assessed by Mazur ankle score. The complications including infections and arthritis symptoms after surgery were also investigated.
Results
Nine trials including 498 pilon fractures of 494 patients were identified. The meta-analysis found no significant differences in nonunion rate (RR = 1.60, 95% CI: 0.66 to 3.86, p = 0.30), and the excellent/good rate (RR = 0.95, 95% CI: 0.86 to 1.04, p = 0.28) between LIFEF group and ORIF group. For assessment of infections, there were significant differences in the rate of deep infection (RR = 2.18, 95% CI: 1.34 to 3.55, p = 0.002), and the rate of arthritis (RR = 1.26, 95% CI: 1.03 to 1.53, p = 0.02) between LIFEF group and ORIF group.
Conclusion
LIFEF has similar effect as ORIF in the treatment of pilon fractures, however, LIFEF group has significantly higher risk of complications than ORIF group does. So LIFEF is not recommended in the treatment of pilon fracture.
Keywords: External fixators; Fracture fixation, internal; Meta-analysis; Pilon fractures
Fractures which occur at the end of the tibial bone and often involve high-energy ankle joint injuries are commonly described as pilon fractures or plafond fracture, accounting for about 1% of lower limb fractures and 7%–10% of all tibial fractures.1, 2 Pilon fractures most often occur in the fall from a great height and accidents of high-energy axial compression violence, and low-energy rotation shear force when skating and falling over.3, 4, 5, 6 Due to the anatomic features of distal tibia, severe fracture and severe soft tissue injury, nonunion, malunion, delayed union and infections often occur after surgery.7 Therefore, the treatment of pilon fractures remains challenging to orthopedic surgeons. However, orthopedic surgeons have reached a consensus that in the treatment of pilon fracture they should follow the principle of reconstructing the anatomic joint, restoring tibial alignment, providing fast soft tissue healing, and facilitate bone union, which helps to receive satisfactory ankle function.8, 9, 10
Generally, the most common used surgical procedures in the treatment of pilon fracture are open reduction and internal fixations (ORIF) and limited internal fixations combined with external fixation (LIFEF). Because ORIF can restore the anatomic structure of distal tibia, it has been regarded as a safe surgical procedure with good results. However, the extensive dissection of soft tissue might lead to increased complications, such as infection, skin necrosis, tensity wheal and other complications.11, 12, 13, 14 LIFEF has been widely used for pilon fracture in recent years, but results in poor restoration of articular surface and high rates of traumatic arthritis.15, 16, 17 Each method has its own advantages and disadvantages, and the treatment for pilon fractures remains controversial. Therefore, we performed a systematic review and meta-analysis to study the clinical efficacy and complications of LIFEF in the treatment of pilon fracture compared with ORIF.
Materials and methods
Literature search
We searched electronic databases included PubMed, Embase, Web of Science, Cochrane Library and China Biology Medicine disc for studies which compared ORIF and LIFEF for the treatment of pilon fractures. The search terms were as follow: pilon fracture, platfond fracture, distal tibial fracture, external fixation, internal fixation, ORIF and LIFEF. Articles were searched from all years to December 2015. No language restrictions were used. In addition, we searched abstracts from conference proceedings, theses and reference lists of all identified studies for further relevant studies. The unpublished investigations were not involved.
Inclusion and exclusion criteria
We included articles with patients diagnosed with pilon fracture, and the intervention of LIFEF or ORIF in experimental group. All randomized controlled trials, non-randomized trials, prospective studies, cohort studies and retrospective studies were included in the present study. And there were no age and region restriction. Articles were excluded if they were editorials, case reports, author replies, reviews and comments. Studies that included other underlying diseases that could confound or interfere with the assessment of clinical efficacy and complications were also excluded. And those studies which did not report relative outcomes were also excluded.
Data analysis
Two authors assessed the included articles independently and used the “MINORS appraisal scores” to evaluate the risk of bias of included retrospective trials.18 And other authors extracted relative data using a pre-designed data extraction form. All disagreements were resolved through discussion. The description of all outcomes we assessed were dichotomous data, and we extracted the number of events happened and the number of patients in each group, then we calculated the relative risks (RR) and 95% confidence interval (CI) for all results. We assessed the degree of heterogeneity between the included studies through visual examination of the combined data presented in the forest plots, and we tested the heterogeneity using a standard chi-square test. p < 0.05 was considered significantly different. We used RevMan 5.3 (Cochrane Collaboration, London, UK) to calculate all statistical tests and the risk of bias.
Results
Identification and selection of studies
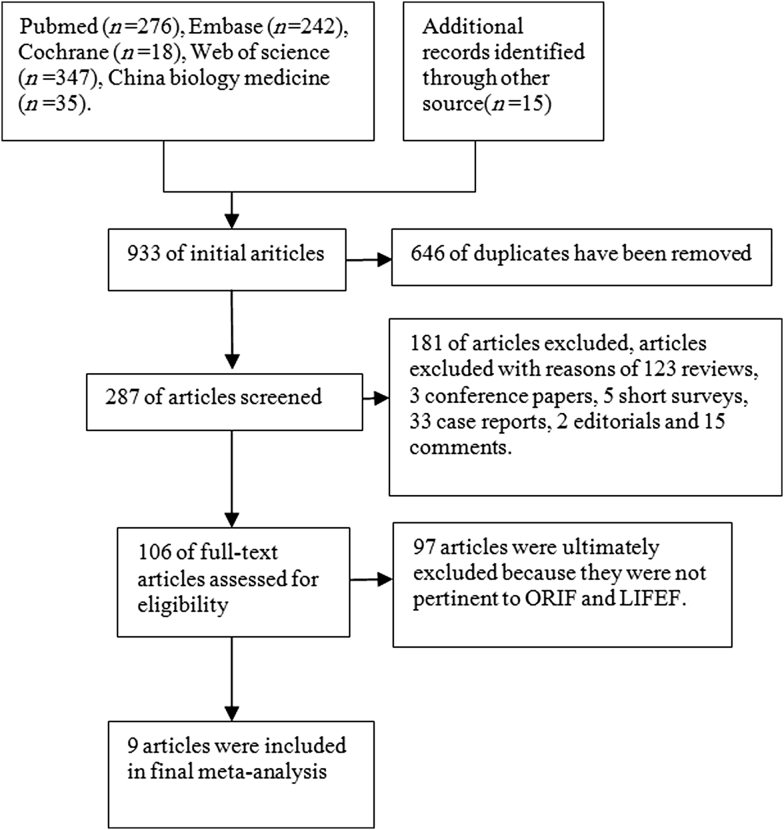
A total of 933 articles (242 from Embase, 18 from Cochrane library, 276 from PubMed Medline, 347 from Web of Science, 35 from China Biology Medicine disc and 15 from other sources) were obtained from the initial search. All studies were selected strictly according to the criteria described. After 646 duplicates, 123 reviews, 3 conference papers, 33 case reports, 5 short surveys, 15 comments, and 2 editorials were removed. There were 106 studies for the full-text screening, and 97 studies were ultimately excluded because they were not pertinent to ORIF and LIFEF. Finally 9 trials were included in present study. The selection process and reasons for exclusion were summarized in Fig. 1.
Fig. 1.
Flow chart summarizing trials selection process.
Description and quality of studies
Nine articles directly comparing LIFEF and ORIF for the treatment of pilon fracture were included in this meta-analysis, including one randomized controlled trial (RCT),19 one cohort study12 and 7 retrospective studies.15, 20, 21, 22, 23, 24, 25 Totally 498 fractures in 494 patients were included in this study, and all eligible patients were followed up for at least 12 months. The demographic characteristics of patients are summarized in Table 1. Methodological quality of RCT and non-RCT studies were evaluated with the “assessing risk of bias” tool of Cochrane and methodological index for non-randomized studies (MINORS) form, respectively. Results are summarized in Table 2.
Table 1.
Description of the studies included in the meta-analysis.
| Authors | Year | Case No. | Fractures | Age (years) | Gender (male/female) | Follow-up (months) |
|---|---|---|---|---|---|---|
| Davidovitch et al15 | 2011 | 20 | 21 | 43 | 12/8 | 12 |
| 26 | 26 | 39 | 17/9 | |||
| Duan et al23 | 2014 | 12 | 12 | 23–67 | 7/5 | 36 |
| 11 | 11 | 21–64 | 7/4 | |||
| Guo et al20 | 2015 | 26 | 26 | 41.2 ± 9.6 | 8/18 | 12 |
| 52 | 52 | 40.7 ± 10.1 | 14/38 | |||
| Harris et al21 | 2006 | 16 | 16 | 57.6 | 7/9 | 26 |
| 60 | 63 | 40.6 | 38/22 | |||
| Huang25 | 2013 | 33 | 33 | 36.5 ± 18.5 | 23/10 | 36 |
| 43 | 43 | 35.5 ± 17.5 | 25/18 | |||
| Pan24 | 2013 | 22 | 22 | 40.5 ± 23.5 | 13/9 | 24 |
| 31 | 31 | 41.5 ± 22.5 | 19/12 | |||
| Richards et al12 | 2012 | 27 | 27 | 46.96 ± 13.1 | NR | 12 |
| 18 | 18 | 40.66 ± 13.3 | NR | |||
| Wang et al19 | 2010 | 29 | 29 | 37.2 ± 10.9 | 26/3 | 24 |
| 27 | 27 | 40.1 ± 10.7 | 25/2 | |||
| Xiao et al22 | 2005 | 22 | 22 | 18–65 | 14/8 | 16 |
| 20 | 20 | 23–54 | 12/8 |
Table 2.
Methodological index for non-randomized studies (MINORS) form in the meta-analysis comparing LIFEF and ORIF.
| Authors | Year | Criteria |
Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |||
| Davidovitch et al15 | 2011 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 19 |
| Duan et al23 | 2014 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 1 | 1 | 1 | 2 | 1 | 17 |
| Guo et al20 | 2015 | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 21 |
| Harris et al21 | 2006 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 19 |
| Huang25 | 2013 | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 18 |
| Pan24 | 2013 | 2 | 0 | 1 | 1 | 0 | 2 | 2 | 1 | 1 | 1 | 2 | 1 | 14 |
| Richards et al12 | 2012 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 20 |
| Xiao et al22 | 2005 | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 1 | 1 | 1 | 1 | 2 | 15 |
The criteria included the following items: (1) a clearly stated aim; (2) inclusion of consecutive patients; (3) prospective data collection; (4) endpoints appropriate to the aim of the study; (5) unbiased assessment of the study endpoint; (6) a follow-up period appropriate to the aims of the study; (7) <5% loss to follow-up; (8) prospective calculation of the sample size; (9) an adequate control group; (10) contemporary groups; (11) baseline equivalence of groups; (12) adequate statistical analyses. Items were scored as follows: 0 (not reported); 1 (reported but inadequate); or 2 (reported and adequate). The ideal global score for comparative studies was 24.
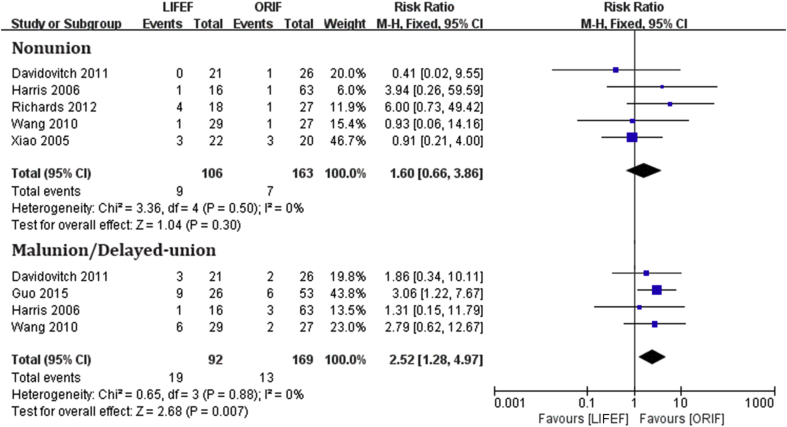
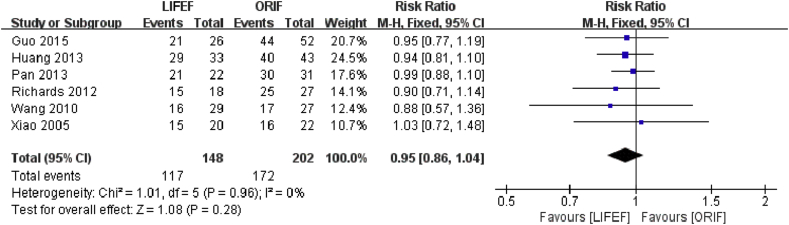
Clinical efficacy of LIFEF
We evaluated the clinical efficacy of LIFEF in the treatment of pilon fracture by nonunion, malunion/delayed union and assessed excellent/good rate by Mazur ankle score.26 For nonunion, 5 studies with 269 fractures were included.12, 15, 19, 21, 22 The rate of nonunion was 9 of 106 in LIFEF group and 7 of 163 in ORIF group, respectively. The meta-analysis showed no significant difference in nonunion between 2 groups, the pooled RR was 1.60 (95% CI: 0.66 to 3.86, p = 0.30) and the heterogeneity among the studies was not significant (I2 = 0%) (Fig. 2). For malunion/delayed union, 4 studies15, 19, 20, 21 with 261 fractures reported the results of malunion/delayed union. The rate of malunion or delayed union was 19 of 92 fractures in LIFEF group and 13 of 169 fractures in ORIF group. The meta-analysis showed a significant difference in malunion/delayed union between 2 groups with the overall RR value was 2.52 (95% CI: 1.28 to 4.97, p = 0.007). LIFEF group had a higher malunion/delayed union rate than ORIF group did. The heterogeneity among the studies was not statistically significant (I2 = 0%) (Fig. 2). For excellent/good rate assessed by Mazur ankle score, 6 studies12, 19, 20, 22, 24, 25 with 350 fractures used the Mazur ankle score to assess the function of ankle after surgery. The excellent/good rate was 117 of 148 fractures in LIFEF group and 172 of 202 fractures in ORIF group, and the overall RR value was 0.95 (95% CI: 0.86 to 1.04, p = 0.28). The result showed no significant difference between 2 groups. The heterogeneity among the studies was not significant (I2 = 0%) (Fig. 3).
Fig. 2.
Outcome of nonunion and malunion/delayed-union (LIFEF versus ORIF).
Fig. 3.
Outcome of excellent/good rate by Mazur ankle score (LIFEF versus ORIF).
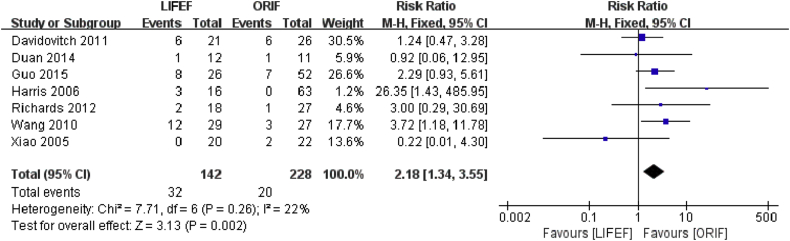
Complications of LIFEF
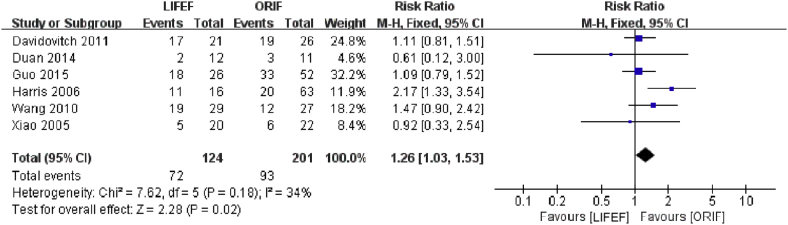
We assessed complications including infection and arthritis after surgery. For infection assessment, seven studies12, 15, 19, 20, 21, 22, 23 with 370 fractures were included in this meta-analysis. The rate of deep infection was 32 of 142 fractures in LIFEF group and 20 of 228 fractures in ORIF group, the overall pooled RR value was 2.18 (95% CI: 1.34 to 3.55, p = 0.002), suggesting a significant difference between the two groups and a higher rate of deep infection in LIFEF group. The heterogeneity among the studies was not significant (I2 = 22%) (Fig. 4). And for arthritis, six studies15, 19, 20, 21, 22, 23 with 325 fractures were included in the meta-analysis. The rate of arthritis was 72 of 124 fractures in LIFEF group and 93 of 201 fractures in ORIF group, with the pooled RR value of 1.26 (95% CI: 1.03 to 1.53, p = 0.02), suggesting a significant difference between the two groups and a higher rate of arthritis in LIFEF group. The heterogeneity among the studies was not significant (I2 = 34%) (Fig. 5).
Fig. 4.
Outcome of infections (LIFEF versus ORIF).
Fig. 5.
Outcome of arthritis (LIFEF versus ORIF).
Discussion
Because of the complexity of fracture and severe soft tissue damage, the treatment of pilon fractures remains challenging to orthopedic surgeons. LIFEF and ORIF have been widely used in the treatment of pilon fracture in recent years, but the superiority remains controversial. Previous studies have reported varied results comparing ORIF and LIFEF procedures.27 Thus, it is essential to conduct a meta-analysis to evaluate the clinical efficacy and complications of ORIF and LIFEF in the treatment of pilon fractures and provide references for orthopedic surgeons.
Ultimately, one RCT, one cohort study and seven retrospective studies has been included in this systematic review and meta-analysis. The overall outcome showed a difference between two methods. For clinical efficacy assessment, the outcomes showed no significant difference in excellent/good rate and the rates of nonunion, malunion/delayed union, the pooled RR value was 2.52 (95% CI: 1.28 to 4.97, p = 0.007), indicating a significant difference between the two groups. LIFEF group had a higher malunion/delayed union rate than ORIF group did. For assessment of complications, we analyzed infections and arthritis after surgery, the pooled RR value was 2.18 (95% CI: 1.34 to 3.55, p = 0.002), and 1.26 (95% CI: 1.03 to 1.53, p = 0.02), showing a significant difference between the two groups. These two complications were significantly more common in the LIFEF group than in the ORIF group, which was opposite to previous studies.15, 19, 22
There were several limitations in our studies. First, this meta-analysis was limited primarily because most of the studies included were retrospective studies, which were more likely to have various kinds of bias. To confirm these outcomes, more high-quality RCTs should be conducted. Second, subgroup analysis was not performed on different types of pilon fractures because of small sample size and different classification standards used in original studies. Third, confounding factors such as underlying diseases and the use of drugs may confuse the outcome, however, there was still no way to control these confounding factors and bias and no established method to assess how these confounding factors and bias affect the overall outcome. Furthermore, we did not analyze the skin necrosis and tensity wheal because of data deficiency.
Based on this meta-analysis, LIFEF has similar effect as ORIF in the treatment of pilon fracture, however, LIFEF group has a significantly higher risk of complications than ORIF group does. So LIFEF is not recommended in the treatment of pilon fractures.
Fund
This work was supported by the Fundamental Research Funds for the Central Universities, China (lzujbky-2014-k16) and the National Science Foundation for Distinguished Young Scholars of Gansu Province, China (No. 1210RJDA010).
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Shen Q.J., Liu Y.B., Jin S. Analyses of relevant influencing factors in the treatment of tibial pilon fractures. Zhonghua Yi Xue Za Zhi. 2012;92:1909–1912. [PubMed] [Google Scholar]
- 2.McCann P.A., Jackson M., Mitchell S.T. Complications of definitive open reduction and internal fixation of pilon fractures of the distal tibia. Int Orthop. 2011;35:413–418. doi: 10.1007/s00264-010-1005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piper K.J., Won H.Y., Ellis A.M. Hybrid external fixation in complex tibial plateau and plafond fractures: an Australian audit of outcomes. Injury. 2005;36:178–184. doi: 10.1016/j.injury.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 4.Marsh J.L., Nepola J.V., Wuest T.K. Unilateral external fixation until healing with the dynamic axial fixator for severe open tibial fractures. J Orthop Trauma. 1991;5:341–348. doi: 10.1097/00005131-199109000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Kapukaya A., Subasi M., Arslan H. Management of comminuted closed tibial plafond fractures using circular external fixators. Acta Orthop Belg. 2005;71:582–589. [PubMed] [Google Scholar]
- 6.Mittal R., Matthews S.J., Zavras D.T. Management of ipsilateral pilon and calcaneal fractures: a report of 2 cases. J Foot Ankle Surg. 2004;43:123–130. doi: 10.1053/j.jfas.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Rommens P.M., Coosemans W., Broos P.L. The difficult healing of segmental fractures of the tibial shaft. Arch Orthop Trauma Surg. 1989;108:238–242. doi: 10.1007/BF00936208. [DOI] [PubMed] [Google Scholar]
- 8.Ruedi T.P., Allgower M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979;138:105–110. [PubMed] [Google Scholar]
- 9.Ramlee M.H., Kadir M.R., Murali M.R. Finite element analysis of three commonly used external fixation devices for treating Type III pilon fractures. Med Eng Phys. 2014;36:1322–1330. doi: 10.1016/j.medengphy.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Ruedi T., Matter P., Allgower M. Intra-articular fractures of the distal tibial end. Helv Chir Acta. 1968;35:556–582. [PubMed] [Google Scholar]
- 11.Dujardin F., Abdulmutalib H., Tobenas A.C. Total fractures of the tibial pilon. Orthop Traumatol Surg Res. 2014;100:S65–S74. doi: 10.1016/j.otsr.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 12.Richards J.E., Magill M., Tressler M.A. External fixation versus ORIF for distal intra-articular tibia fractures. Orthopedics. 2012;35:e862–867. doi: 10.3928/01477447-20120525-25. [DOI] [PubMed] [Google Scholar]
- 13.Calori G.M., Tagliabue L., Mazza E. Tibial pilon fractures: which method of treatment? Injury. 2010;41:1183–1190. doi: 10.1016/j.injury.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 14.Chen S.H., Wu P.H., Lee Y.S. Long-term results of pilon fractures. Arch Orthop Trauma Surg. 2007;127:55–60. doi: 10.1007/s00402-006-0225-3. [DOI] [PubMed] [Google Scholar]
- 15.Davidovitch R.I., Elkhechen R.J., Romo S. Open reduction with internal fixation versus limited internal fixation and external fixation for high grade pilon fractures (OTA type 43C) Foot Ankle Int. 2011;32:955–961. doi: 10.3113/FAI.2011.0955. [DOI] [PubMed] [Google Scholar]
- 16.Barbieri R., Schenk R., Koval K. Hybrid external fixation in the treatment of tibial plafond fractures. Clin Orthop Relat Res. 1996;332:16–22. doi: 10.1097/00003086-199611000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Bone L., Stegemann P., McNamara K. External fixation of severely comminuted and open tibial pilon fractures. Clin Orthop Relat Res. 1993;292:101–107. [PubMed] [Google Scholar]
- 18.Slim K., Nini E., Forestier D. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 19.Wang C., Li Y., Huang L. Comparison of two-staged ORIF and limited internal fixation with external fixator for closed tibial plafond fractures. Arch Orthop Trauma Surg. 2010;130:1289–1297. doi: 10.1007/s00402-010-1075-6. [DOI] [PubMed] [Google Scholar]
- 20.Guo Y., Tong L., Li S. External fixation combined with limited internal fixation versus open reduction internal fixation for treating Ruedi-Allgower type III pilon fractures. Med Sci Monit. 2015;21:1662–1667. doi: 10.12659/MSM.893289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris A.M., Patterson B.M., Sontich J.K. Results and outcomes after operative treatment of high-energy tibial plafond fractures. Foot Ankle Int. 2006;27:256–265. doi: 10.1177/107110070602700406. [DOI] [PubMed] [Google Scholar]
- 22.Xiao R., Tang Q., Cai C. Treatments of tibial pilon fractures with a combination of limited internal fixation and external fixation. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2005;19:603–606. [PubMed] [Google Scholar]
- 23.Duan D.P., You W.L., Ji L. Case-control study on effects of external fixation combined with limited internal fixation for the treatment of pilon fractures of Ruedi-Allgower type III. Zhongguo Gu Shang. 2014;27:29–33. [PubMed] [Google Scholar]
- 24.Pan W. Clinical observation of open reduction and internal fixation with limited internal fixation combined with external fixation support fixed on patients with tibial Pilon fractures. Gansu Med J. 2013;32:259–260. [Google Scholar]
- 25.Huang Y. The efficacy comparison of the operation methods for tibial pilon fracture between open reduction and internal fixation and limited internal fixation combined with external fixed support fixation. China Mod Dr. 2013;51:251–252. [Google Scholar]
- 26.Mazur J.M., Schwartz E., Simon S.R. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Jt Surg Am. 1979;61:964–975. [PubMed] [Google Scholar]
- 27.Tang X., Liu L., Tu C.Q. Comparison of early and delayed open reduction and internal fixation for treating closed tibial pilon fractures. Foot Ankle Int. 2014;35:657–664. doi: 10.1177/1071100714534214. [DOI] [PubMed] [Google Scholar]