Abstract
Introduction
Paediatric trauma is a significant burden to healthcare worldwide and accounts for a large proportion of deaths in the UK.
Methods
This retrospective study examined the epidemiological data from a major trauma centre in the UK between January 2012 and December 2014, reviewing all cases of moderate to severe trauma in children. Patients were included if aged ≤16 years and if they had an abbreviated injury scale score of ≥2 in one or more body region.
Results
A total of 213 patients were included in the study, with a mean age of 7.8 years (standard deviation [SD]: 5.2 years). The most common cause of injury was vehicle related incidents (46%). The median length of hospital stay was 5 days (interquartile range [IQR]: 4–10 days). Approximately half (52%) of the patients had to stay in the intensive care unit, for a median of 1 day (IQR: 0–2 days). The mortality rate was 6.6%. The mean injury severity score was 19 (SD: 10). Pearson’s correlation coefficient showed a positive correlation for injury severity score with length of stay in hospital (p<0.001).
Conclusions
There is significant variation in mechanism of injury, severity and pattern of paediatric trauma across age groups. A multidisciplinary team approach is imperative, and patients should be managed in specialist centres to optimise their care and eventual functional recovery. Head injury remained the most common, with significant mortality in all age groups. Rib fractures and pelvic fractures should be considered a marker for the severity of injury, and should alert doctors to look for other associated injuries.
Keywords: Paediatrics, Polytrauma, Rib fracture, Pelvic fracture, Major trauma centre, Trauma network
Paediatric trauma is a significant burden to healthcare worldwide1 and accounts for a large proportion of deaths in the UK.2,3 Children are not just small adults and often require different expertise to deal with emergencies efficiently. Knowledge regarding the demographics of paediatric trauma workload as well as the patterns and timings of presentation help plan for the judicious use of available resources. Although a number of reports have been published, literature addressing this important issue is still lacking. Bayreuther et al published the largest analysis of paediatric trauma in the UK based on the Trauma Audit and Research Network (TARN) national database.3 This demonstrated a trend of decreasing overall mortality year on year with improved hospital care and hospital coordination in a trauma network.
Addenbrooke’s Hospital in Cambridge is the level 1 major trauma centre (MTC) for the East of England region (Fig 1). It is one of only 12 combined adult and children’s MTCs in the UK. The MTC covers an area of 7,335 square miles (19,000km2), encompassing a population of 5.9 million people. It has a mixture of rural, residential, light industrial and coastal regions. The aim of this study was to independently analyse paediatric trauma data in our MTC so as to identify the patterns of injury as well as the associated mechanisms of injury and to assess the outcome.
Figure 1.
East of England trauma network.
Methods
This was a retrospective analysis of our hospital trauma database, which reviewed all cases of moderate to severe trauma in children aged ≤16 years over a period of three years (January 2012 – December 2014). Children were included in the study if they had an AIS score of ≥2 in one or more regions of body. Permission for the study was granted by the institutional patient safety and quality department.
Data reviewed included: patient demographics; transfer information; day, month and time of presentation; mechanism and type of injury; systems involved; Glasgow coma scale (GCS) score; abbreviated injury scale (AIS) score; injury severity score (ISS); and probability of survival calculated from the GCS score and ISS. Injuries were categorised according to seven body areas: head, face, thorax, abdomen, limbs, spine and pelvis. Different injury patterns were assessed in relation to age group, mechanism of injury and mortality rate. Outcome variables of interest included mortality, length of hospital stay and length of stay in the intensive care unit.
Statistical analysis
Data were analysed on Excel® (Microsoft, Redmond, WA, US) and Minitab® version 17 (Minitab, Coventry, UK). The chi-squared test was used to compare variations between different groups. A p-value of <0.05 was considered statistically significant. Correlation between variables was assessed using Pearson’s correlation coefficient, with the threshold for significance set at p<0.01.
Results
The records of 213 children (137 male, 76 female) were reviewed, with a mean age of 7.8 years (standard deviation [SD]: 5.2 years). The patients were stratified into four age groups: <1 year, 1–5 years, 6–10 years and 11–16 years. The distribution of patients among these groups is shown in Table 1.
Table 1.
Demographics of the 213 paediatric trauma patients
| Sex | |
| Male | 137 (64.3%) |
| Female | 76 (35.7%) |
| Age | |
| Mean age in years | 7.8 (SD: 5.2) |
| <1 year | 28 (13.1%) |
| 1–5 years | 60 (28.2%) |
| 6–10 years | 50 (23.5%) |
| 11–16 years | 75 (35.2%) |
| Type of injury | |
| Blunt | 210 (98.6%) |
| Penetrating | 3 (1.4%) |
| Mechanism of injury | |
| Vehicle related incident | 98 (46.0%) |
| Fall from <2m | 57 (26.8%) |
| Fall from >2m | 26 (12.2%) |
| Blow(s) | 13 (6.1%) |
| Non-accidental injury (suspected) | 8 (3.6%) |
| Hanging | 3 (1.4%) |
| Crush | 2 (0.9%) |
| Blast | 1 (0.5%) |
| Stabbing | 1 (0.5%) |
| Other | 4 (1.9%) |
SD = standard deviation
Distribution of admissions
During the study period, 97 patients attended our emergency department directly while 116 were transferred from other hospitals in the trauma network. Consequently, 54% of patients were not resident in the Cambridgeshire area, with 7% actually coming from areas beyond the East of England region.
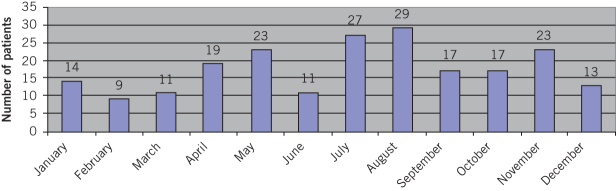
On average, 5.9 patients were admitted per month. Cumulative admissions for each calendar month over the three-year study period are shown in Figure 2. The highest frequency of admissions occurred in July (n=27) and August (n=29) while February (n=9), March (n=11) and June (n=11) experienced the lowest numbers of admissions. When comparing the four quarters of the year, the third quarter (July to September) had the highest proportion of admissions.
Figure 2.
Distribution of paediatric trauma admissions by months over the three-year study period
In terms of days of the week, 137 patients (64.3%) were admitted to the emergency department on weekdays, equating to an average of 27.4 admissions per day from Monday to Friday. This compared with 76 patients (35.7%) being admitted at the weekend, which corresponds to an average of 38.0 admissions per day for Saturdays and Sundays. Similarly, there were considerably more admissions during the evening than late at night and in the early morning with the highest levels of attendance between 5pm and 8pm (Fig 3).
Figure 3.
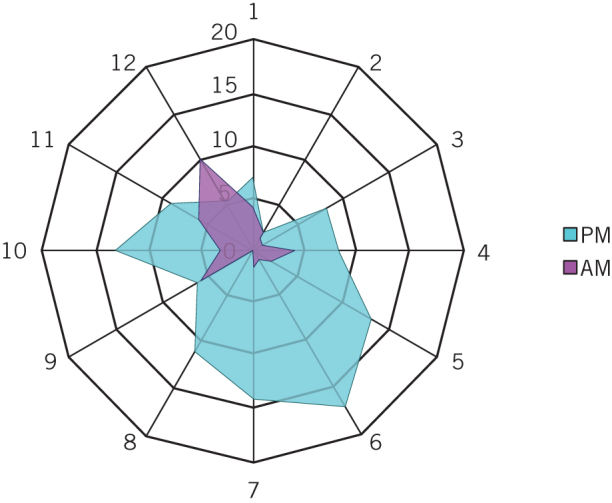
Radar chart of paediatric trauma emergency department arrival time plotted in two 12-hour overlapping graphs
Mechanism of injury
Most of the injuries occurred on roads (37.1%) or at home (31.4%), followed by public areas (14.6%) and institutions (7.8%). Vehicle related incidents were the most common mechanism of injury overall (46.0%). Table 2 shows the frequency of different mechanisms of injury for the four different age groups. All suspected NAI cases presented with either head injury or asphyxia related brain injury. Three cases of hanging were also reported; two of them were most likely accidental while playing alone and one was suspected self-harm.
Table 2.
Mechanism of injury by age group
| Age | Vehicle related incident | Fall from <2m | Fall from >2m | Blow(s)* | NAI | Hanging | Crush | Blast | Stabbing | Other** | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| <1 year (n=28) | 5 (2.3%) | 8 (3.8%) | 3 (1.4%) | 3 (1.4%) | 6 (2.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (1.4%) | 28 (13.1%) |
| 1–5 years (n=60) | 18 (8.4%) | 25 (11.7%) | 10 (4.7%) | 3 (1.4%) | 2 (0.9%) | 0 (0%) | 1 (0.5%) | 1 (0.5%) | 0 (0%) | 0 (0%) | 60 (28.2%) |
| 6–10 years (n=50) | 29 (13.6%) | 9 (4.2%) | 7 (3.3%) | 3 (1.4%) | 0 (0%) | 1 (0.5%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.5%) | 50 (23.4%) |
| 11–16 years (n=75) | 46 (21.6%) | 15 (7.0%) | 6 (2.8%) | 4 (1.9%) | 0 (0%) | 2 (0.9%) | 1 (0.5%) | 0 (0%) | 1 (0.5%) | 0 (0%) | 75 (35.2%) |
| All ages (n=213) | 98 (46.0%) | 57 (26.8%) | 26 (12.2%) | 13 (6.1%) | 8 (3.8%) | 3 (1.4%) | 2 (0.9%) | 1 (0.5%) | 1 (0.5%) | 4 (1.9%) | 213 (100%) |
*mainly related to sports injuries caused by ball, bat, racket or helmet; **cases in which mechanism of injury was not clear
NAI = non-accidental injury (suspected)
Pattern of injuries
Injuries were stratified based on seven different body regions (Table 3). Head injuries were the most common (54.0%), followed by limb injuries (39.9%). The overall mortality rate for head injuries was 8.7%. This was the only injury type that was fatal in isolation, death occurring in two cases. Pelvic fracture was the least common injury (7.0%) and all but one of these were associated with injuries in other body regions. Table 4 shows the breakdown of regional injuries by age group.
Table 3.
Patterns of regional injuries and associated mortality
| Regional injuries | Isolated injuries | Mortality | Associated injuries | Mortality | Total injuries | Mortality |
|---|---|---|---|---|---|---|
| Head | 48 (22.5%) | 2 (4.2%) | 67 (31.4%) | 8 (11.9%) | 115 (54.0%) | 10 (8.7%) |
| Face | 2 (0.9%) | 0 (0%) | 37 (17.4%) | 3 (8.1%) | 39 (18.3%) | 3 (7.8%) |
| Thorax | 0 (0%) | 0 (0%) | 36 (16.9%) | 5 (13.9%) | 36 (16.9%) | 5 (13.9%) |
| Abdomen | 18 (8.4%) | 0 (0%) | 21 (9.8%) | 2 (9.5%) | 39 (18.3%) | 2 (5.1%) |
| Limbs | 38 (17.8%) | 0 (0%) | 47 (22.1%) | 4 (8.5%) | 85 (39.9%) | 4 (4.7%) |
| Spine | 7 (3.3%) | 0 (0%) | 15 (7.0%) | 2 (13.3%) | 22 (10.3%) | 2 (9.1%) |
| Pelvis | 1 (0.5%) | 0 (0%) | 14 (6.6%) | 1 (7.1%) | 15 (7.0%) | 1 (6.7%) |
Table 4.
Patterns of regional injuries by age group
| Regional injuries | <1 year (n=28) | 1–5 years (n=60) | 6–10 years (n=50) | 11–16 years (n=75) | All ages (n=213) |
|---|---|---|---|---|---|
| Head | 28 (13.1%) | 28 (13.1%) | 25 (11.7%) | 34 (16.0%) | 115 (54.0%) |
| Face | 12 (5.6%) | 8 (3.8%) | 7 (3.3%) | 12 (5.6%) | 39 (18.3%) |
| Thorax | 2 (0.9%) | 8 (3.8%) | 12 (5.6%) | 14 (6.6%) | 36 (16.9%) |
| Abdomen | 1 (0.5%) | 5 (2.3%) | 14 (6.6%) | 19 (8.9%) | 39 (18.3%) |
| Limbs | 2 (0.9%) | 34 (15.9%) | 21 (9.9%) | 28 (13.1%) | 85 (39.9%) |
| Spine | 3 (1.4%) | 4 (1.9%) | 3 (1.4%) | 12 (5.6%) | 22 (10.3%) |
| Pelvis | 1 (0.5%) | 5 (2.3%) | 4 (1.9%) | 5 (2.3%) | 15 (7.0%) |
Length of stay
The median length of stay in hospital was 5 days (interquartile range [IQR]: 4–10 days) and in the intensive care unit, it was 1 day (IQR: 0–2 days). Length of hospital stay correlated positively with ISS (r=0.280, p<0.001).
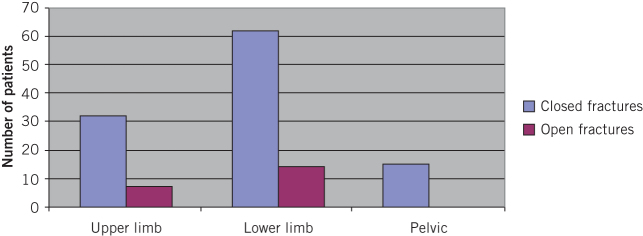
Orthopaedic injuries
There were 88 patients with orthopaedic injuries involving the upper limb, lower limb and pelvis. Spinal injuries were not included as those are managed by neurosurgeons in our institution. The mean age was 7.7 years (SD: 4.8 years). There were similar numbers of patients with isolated orthopaedic injuries (n=43, 48.9%) and patients who had other associated injuries (n=45, 51.1%). There were 39 patients (44.3%) with upper limb injuries while lower limb and pelvic injuries were identified in 76 (86.4%) and 15 (17.0%) cases respectively (Fig 4). Half of the patients had a single long bone fracture whereas the other half had multiple fractures. The most common mechanism for orthopaedic injuries was vehicle related collisions (n=52, 59.1%), followed by falls from <2m height (n=26, 29.5%).
Figure 4.
Orthopaedic injuries in paediatric trauma patients
Four patients with orthopaedic injuries died, equating to a mortality rate of 4.5% in this group. None of these patients had an isolated injury. Three had an associated head injury and one had multiple long bone fractures with an associated abdominal injury. One of them also had a pelvic/acetabular fracture.
Outcome and mortality
A total of 14 patients died (overall mortality rate 6.6%). Nine of these were direct admissions while five were transferred from other hospitals. Seven of the deaths were associated with road traffic collisions, three were due to hanging, one resulted from suspected NAI with head injury, one followed a fall from a horse leading to an injured cervical spine causing cord compression, one was due to a head injury sustained while jumping on a bouncy castle and one child died after pulling a television on to himself. Ten of the fourteen mortalities had some element of head injury involved. One patient had pelvic fractures with associated injuries, and three died of asphyxia and hypoxic brain injury related to hanging.
Discussion
Trauma accounts for significant child mortality and morbidity worldwide. Approximately 830,000 children die every year from unintentional injuries.1 Road traffic collisions, falls and drowning are among the most common mechanisms. Although 95% of these injuries occur in low income and middle income countries, paediatric injuries also remain a significant problem in high income countries, accounting for 40% of all paediatric mortality.1 In the UK, trauma remains a major cause of child mortality, ranging from 16% in those aged 1–4 years to 40% in 15–19-year-olds.3
Our study shows a male predilection for polytrauma of 2:1. Similar findings have been noted in other studies, with the highest rate being 3:1.4–6 The average age for paediatric polytrauma patients has uniformly been reported in the literature as less than 10 years,7–11 with a significant proportion being infants. Paediatric trauma admissions seem to follow a pattern of increased frequency in the spring and summer months.12 Furthermore, a significant number of admissions occur in the evening, between 5pm and 8pm. This pattern of attendance has an implication for the staffing of paediatric trauma services.
Paediatric polytrauma affects the whole family. Over half of the patients in our regional trauma centre were not from the catchment area of the immediate hospital, and it is likely that the distance to be travelled by the parents has an economic and emotional impact.
Mechanism of injury and injury pattern vary according to different age groups. In our study, all but three patients suffered blunt injuries. Vehicle related injuries and falls were the two most common mechanisms overall, accounting for 75% of admissions. Vehicle related injuries were more common in children aged 6–16 years while younger children were more prone to falls.
Almost a third (31%) of the children involved in motor vehicle collisions in our study were pedestrians versus cars while 14% were cyclists versus cars. Interestingly, there were incidents involving children riding motorbikes. Three of these (2 boys and 1 girl) were aged under 13 years and were involved in motocross (a form of off-road motorcycle racing). The two boys sustained femur fractures that required fixation (average ISS 8.5) while the girl had multiple fractures including the humerus and pelvis (ISS 27). One 15-year-old boy had been riding his off-road motorcycle without supervision and collided with a car, resulting in death. Motocross is known to be a high risk sport with an injury rate of 22.72 per thousand.13 The pattern of injuries seen in our cohort of patients reflects that reported elsewhere.14
NAI and teenage suicide continue to be challenging for all communities.15 In our study, there were eight cases (3.8%) of suspected child abuse; six of these were in the <1-year age group. Three cases of asphyxia from hanging were also highlighted (two boys aged 9 and 11 years, and one girl aged 14 years). These findings are comparable with general UK data. The national incidence of suicide among children aged 10–14 years has remained unchanged between 1970 and 2010: for girls, the rate of suicides was 0.23 per 100,000 population per year and for boys, it was 0.71.16
Several other studies have reported 34–41% of injuries being casued by vehicle related collisions and 8–16% being the result of falls.17,18 Howard et al,19 Durbin et al20 and Al-Jazaeri et al21 investigated the effect of seating position and restraints on the risk of injury to children in motor vehicle crashes. Unrestrained passengers sitting in the front were at highest risk of injury compared with restrained children sitting in the back. Lack of an age appropriate child restraint and middle seating position were associated with a greater risk of head and neck trauma in younger children while adolescents were at increased risk of abdominal injuries associated with the use of lap/shoulder belts, single vehicle collision and vehicle extrication.22
The head was the most commonly injured body region in our study (54.0%), with an overall mortality rate of 8.7%. It was the only isolated injury type that was fatal. The mortality rate for head injury increased to 11.9% when combined with injuries in other regions (Table 3).
Although thoracic injuries were less frequent (16.9%), they had the highest overall mortality rate (13.9%). Importantly, none of the injuries to the thorax were isolated. This reflects the amount of energy transferred, to cause such injuries. Ribs in children are pliable and can deform under load without fracture, leading to lung and mediastinal injuries. As a result, rib fracture in children is considered a marker for injury severity.15
Limb injuries were the second most common injury in our study (39.9%). Almost half of the limb injuries were isolated. Although none of them were fatal, they can add considerably to the morbidity of the child. Letts et al assessed the outcome and long-term results in a cohort of 149 polytrauma children.23 The most common complications were limb deformity, secondary to fracture (18%) and infection (15%). The incidence for pelvic fractures in paediatric trauma patients has been reported as 2.4–7.5%.24,25 In our study, the incidence of pelvic fractures was 7.0%, with a mortality rate of 6.7%. Only 1 of the 15 patients with injury to the pelvis had no other associated injuries, again indicating the severity of impact and the amount of energy transferred to the body in these cases.
Conclusions
In paediatric trauma, there is significant variation in pattern of injury and associated mechanisms across age groups. Head injury remains the most common injury, with significant mortality for all ages. Rib fractures and pelvic fractures should be considered a marker for injury severity, and should alert doctors to look for other associated injuries. Awareness of the peak paediatric polytrauma admission times in the evening and summer can aid with staff and resource planning.
Although mortality from trauma is low in paediatric patients, we must continue to improve the safety of children. This can be achieved by improving the safety of roads, the home and sports facilities, and also by using appropriate safety equipment and parental supervision where necessary.
Acknowledgement
The authors would like to acknowledge the staff in the East of England trauma network office for providing the data.
References
- 1.World Health OrganizationWorld Report on Child Injury Prevention: Summary. Geneva: WHO; 2008. [PubMed] [Google Scholar]
- 2.Department of HealthSaving Lives: Our Healthier Nation. London: DH; 1999. [Google Scholar]
- 3.Bayreuther J, Wagener S, Woodford M et al. . Paediatric trauma: injury pattern and mortality in the UK. Arch Dis Child Educ Pract Ed 2009; : 37–41. [DOI] [PubMed] [Google Scholar]
- 4.Hu X, Wesson DE, Logsetty S, Spence LJ. Functional limitations and recovery in children with severe trauma: a one-year follow-up. J Trauma 1994; : 209–213. [DOI] [PubMed] [Google Scholar]
- 5.Condello AS, Hancock BJ, Hoppensack M et al. . Pediatric trauma registries: the foundation of quality care. J Pediatr Surg 2001; : 685–689. [DOI] [PubMed] [Google Scholar]
- 6.Bumbasirevic M, Lesic A, Bumbasirevic V et al. . Severe road traffic injuries and youth: a 4-year analysis for the city of Belgrade. Int J Inj Contr Saf Promot 2014; : 313–317. [DOI] [PubMed] [Google Scholar]
- 7.Schalamon J, v Bismarck S, Schober PH, Höllwarth ME. Multiple trauma in pediatric patients. Pediatr Surg Int 2003; : 417–423. [DOI] [PubMed] [Google Scholar]
- 8.Bulut M, Koksal O, Korkmaz A et al. . Childhood falls: characteristics, outcome, and comparison of the Injury Severity Score and New Injury Severity Score. Emerg Med J 2006; : 540–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ekenze SO, Anyanwu KK, Chukwumam DO. Childhood trauma in Owerri (south eastern) Nigeria. Niger J Med 2009; : 79–83. [PubMed] [Google Scholar]
- 10.Zwingmann J, Schmal H, Mehlhorn A et al. . Injury patterns in polytraumatized children and consequences for the emergency room management. Acta Chir Orthop Traumatol Cech 2010; : 365–370. [PubMed] [Google Scholar]
- 11.Lee YT, Feng XY, Lin YC, Chiang LW. Pediatric trauma team activation: are we making the right call? Eur J Pediatr Surg 2014; : 46–50. [DOI] [PubMed] [Google Scholar]
- 12.Masterson E, Borton D, O’Brien T. Victims of our climate. Injury 1993; : 247–248. [DOI] [PubMed] [Google Scholar]
- 13.Gobbi A, Tuy B, Panuncialman I. The incidence of motocross injuries: a 12-year investigation. Knee Surg Sports Traumatol Arthrosc 2004; : 574–580. [DOI] [PubMed] [Google Scholar]
- 14.Larson AN, Stans AA, Shaughnessy WJ et al. . Motocross morbidity: economic cost and injury distribution in children. J Pediatr Orthop 2009; : 847–850. [DOI] [PubMed] [Google Scholar]
- 15.Sharma OP, Oswanski MF, Stringfellow KC, Raj SS. Pediatric blunt trauma: a retrospective analysis in a Level I trauma center. Am Surg 2006; : 538–543. [PubMed] [Google Scholar]
- 16.Windfuhr K, While D, Hunt IM et al. . Suicide and accidental deaths in children and adolescents in England and Wales, 2001-2010. Arch Dis Child 2001; : 945–950. [DOI] [PubMed] [Google Scholar]
- 17.Cooper A, Barlow B, DiScala C, String D. Mortality and truncal injury: the pediatric perspective. J Pediatr Surg 1994; : 33–38. [DOI] [PubMed] [Google Scholar]
- 18.Holmes JF, Sokolove PE, Brant WE, Kuppermann N. A clinical decision rule for identifying children with thoracic injuries after blunt torso trauma. Ann Emerg Med 2002; : 492–499. [DOI] [PubMed] [Google Scholar]
- 19.Howard A, Rothman L, McKeag AM et al. . Children in side-impact motor vehicle crashes: seating positions and injury mechanisms. J Trauma 2004; : 1,276–1,285. [DOI] [PubMed] [Google Scholar]
- 20.Durbin DR, Chen I, Smith R et al. . Effects of seating position and appropriate restraint use on the risk of injury to children in motor vehicle crashes. Pediatrics 2005; : e305–e309. [DOI] [PubMed] [Google Scholar]
- 21.Al-Jazaeri A, Zamakhshary M, Al-Omair A et al. . The role of seating position in determining the injury pattern among unrestrained children involved in motor vehicle collisions presenting to a level I trauma center. Ann Saudi Med 2012; : 502–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Charyk Stewart T, McClafferty K, Shkrum M et al. . A comparison of injuries, crashes, and outcomes for pediatric rear occupants in traffic motor vehicle collisions. J Trauma Acute Care Surg 2013; : 628–633. [DOI] [PubMed] [Google Scholar]
- 23.Letts M, Davidson D, Lapner P. Multiple trauma in children: predicting outcome and long-term results. Can J Surg 2002; : 126–131. [PMC free article] [PubMed] [Google Scholar]
- 24.Spiguel L, Glynn L, Liu D, Statter M. Pediatric pelvic fractures: a marker for injury severity. Am Surg 2006; : 481–484. [PubMed] [Google Scholar]
- 25.Niedzielski KR, Guzikiewicz N, Małecki K, Golański G. Pelvic fractures in children and adolescents in polytrauma and high-energy injuries. Ortop Traumatol Rehabil 2013; : 41–48. [DOI] [PubMed] [Google Scholar]