Abstract
Paraneoplastic syndrome affects less than 1% of cancer patients. Diagnosis of paraneoplastic syndrome with neurological presentation requires screening for an underlying malignancy, including a complete history, physical examination and imaging studies. Treatment often results in symptom stability, rather than improvement. Paraneoplastic polymyositis can precede or instantaneously occur at diagnosis or treatment of a primary tumour, while neurological symptoms can persist even following cancer treatment. We report a rare case of metaplastic breast carcinoma with an unusual presentation of paraneoplastic polymyositis.
Keywords: Paraneoplastic syndrome, Metaplastic carcinoma, Diagnosis, Neurology, Breast cancer
Paraneoplastic syndrome is a rare condition, affecting less than 1% of cancer patients.1 Diagnosis of paraneoplastic syndrome with neurological presentation requires screening for an underlying malignancy. This process includes a complete history, physical examination and imaging studies.1 Treatment often results in symptom stability, rather than improvement.1 Paraneoplastic polymyositis can precede or instantaneously occur at diagnosis or treatment of a primary tumour. Neurological symptoms can persist even following cancer treatment.2
Polymyositis belongs to a heterogeneous group of autoimmune diseases called inflammatory myopathies, which are characterised by proximal skeletal muscle weakness, cutaneous manifestations, elevated serum creatine kinase activity and inflammatory cells in muscle biopsy. Polymyositis is a cell-mediated autoimmune disorder.3 The first reported association between malignancy and myositis was made by Stertz G et al in 1916.4 The reported incidence for inflammatory myositis varies from 0.5 to 0.89 per 100,000 per year.5
We report a rare case of metaplastic breast carcinoma with an unusual presentation of paraneoplastic polymyositis.
Case presentation
A 66-year-old caucasian female presented with progressive difficulties with walking and climbing stairs, and developed proximal muscle weakness, paresthesia and gait ataxia over a period of 11 months. She became wheelchair-dependent and required hospital admission under the care of a neurologist. The patient had no relevant past medical history.
Cerebrospinal fluid oligoclonal bands were negative, and a raised creatine kinase (CPK) level of 825 IU/L was detected on admission. Autoantibodies directed against anti-Ro, anti-Jo and anti-La, and extractable nuclear antigen antibodies, were detected. The antinuclear antibody test was positive. Electromyography was consistent with myopathy. An open-muscle biopsy of the leg revealed endomysial mononuclear cells and myonecrosis indicative of inflammatory myopathy.
Patient was referred for radiological investigations. Computed tomography of the chest, abdomen and pelvis was unremarkable. Magnetic resonance imaging of the lower limbs showed inflammatory changes consistent with myositis and myopathy. As part of the investigations for the neurological presentation of paraneoplastic syndrome with myositis, fluorodesoxyglucose (FDG)-positron emission tomography (PET) was performed, which demonstrated a discrete moderate focus of uptake in the superior aspect of the left breast and proximal muscles (Fig 1). In view of these findings, the patient was referred to breast clinic for triple assessment.
Figure 1.
Discrete moderate focus of uptake in the superior aspect of the left breast and proximal muscles. 304×171mm (96×96 DPI)
The patient’s breast examination was normal, apart from left breast tissue thickening at the 12 o’clock P-2 (benign) position. Craniocaudal (Fig 2) and mediolateral oblique (Fig 3) views on mammography, and breast ultrasound (Fig 4), showed an indistinct 12-mm (M-3 and U-4) breast lesion. Ultrasound of the axilla revealed an indeterminate lymph node. Core biopsy from the breast confirmed the presence of metaplastic breast carcinoma, with extensive squamous differentiation. Oestrogen, progesterone and human epidermal growth factor receptor 2 status were all normal, as was a fine needle aspiration from the axilla.
Figure 2.
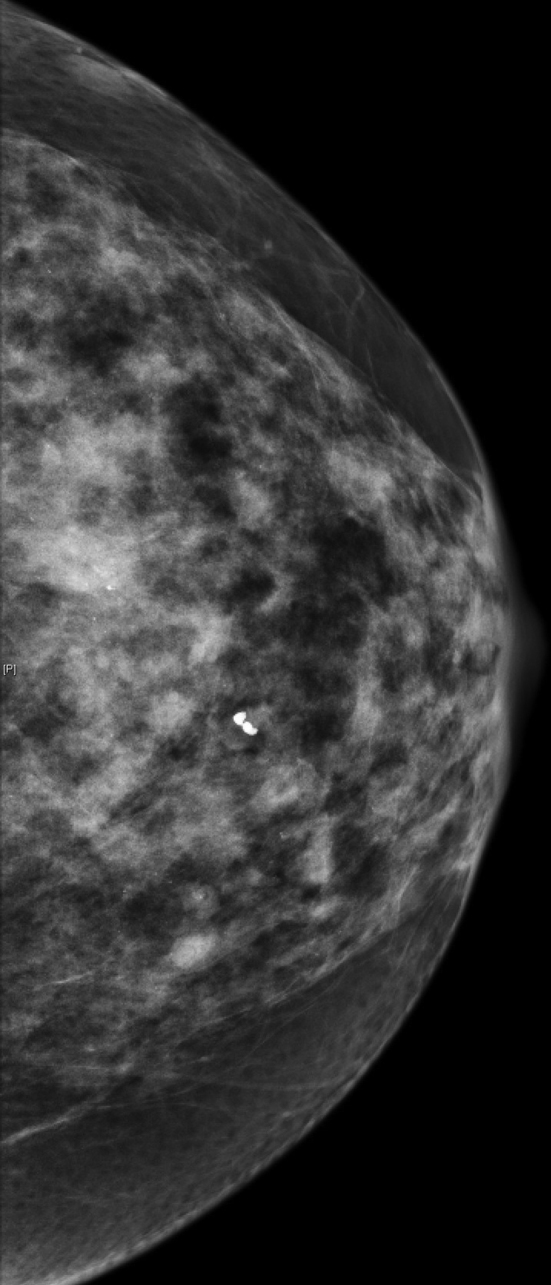
Left breast mammogram, craniocaudal view, of the oval lesion. 210×442mm (96×96 DPI)
Figure 3.

Left breast mammogram, mediolateral oblique view. At the 12 o'clock position, there is a 12.6mm oval lesion, which contains some echogenic calcifications. 316×521mm (96×96 DPI)
Figure 4.

At the 12 o'clock position, there are some echogenic calcifications. This is graded as R3 U4. Ultrasound in the low left axilla shows a lymph node, which has a slightly thickened cortex measuring up to 1.7mm. The length of the lymph node is 10.3mm. The lymph nodes superior to this are, overall, less prominent. 213×161mm (96×96 DPI)
The patient underwent wire-guided wide local excision and sentinel lymph node biopsy under general anesthetic. Due to the difficulty of wire localisation with radiologically indistinct tumour features, a second operation was required for complete excision of the superiolateral margins. Final histology revealed a tumour size of 16mm, with negative sentinel nodes. The postoperative course was uneventful.
The patient was referred for adjuvant therapies, consisting of chemotherapy with six cycles of 5-fluorouracil, epirubicin, cyclophosphamide and docetaxel, followed by external beam radiotherapy of 40.05 Gy delivered over 15 fractions plus further left breast irradiation of 10 Gy over 5 fractions. The patient’s neurologist started a tapering dose of prednisolone and azathioprine alongside her breast cancer to prevent further progression of the neurological condition.
After 8 months of treatment, CPK levels had fallen to 245 IU/L, with no further deterioration. Yearly mammographic and clinical surveillance following completion of treatment revealed she was clinically well, with no evidence of breast cancer recurrence or paraneoplastic syndrome symptoms.
Discussion
Paraneoplastic syndrome in breast cancer is a very rare condition, particularly with neurological presentation of polymyositis and myopathy. Certainly this is the first case in our breast unit, which treats more than 300 breast cancers a year. Metaplastic breast carcinoma is one of the rarest breast cancer types and represents 0.25%–1.00% proportion of all breast cancers.6 The Mayo clinic reported 27 patients over period of 20 years with metaplastic breast carcinoma.6
Metaplastic breast cancer presents with axillary nodal involvement less frequently than adenocarcinoma of the breast. Presenting as high-density masses on mammograms, with circumscribed, obscured or irregular margins and a highly heterogeneous nature, can lead to difficulties in identification during surgery. Histologically, the tumour is poorly differentiated, node-negative, with high Ki67 and p53 positivity and a high potential for metastatic spread.7 It is difficult to establish whether a rare subtype of breast metastatic carcinoma has contributed to the unusual myopathy and myositis in this case.
Studies have shown that comorbidities such as pulmonary fibrosis, dysphagia, muscle disease severity, tumour stage and patient age affect the prognosis of patients with inflammatory myositis. Inflammatory myopathy may proceed alongside or become evident after the diagnosis of a malignancy. Song et al described three cases of myositis that occurred before breast cancer,8 while Yeh et al published five cases of myositis that were diagnosed later.9 The clinical expression of paraneoplastic polymyositis is the same as that of polymyositis without cancer.2 Polymyositis is diagnosed using the erythrocyte sedimentation rate and serum levels of muscle enzymes, alongside myogenic signs on electromyography.2
Immune dysfunction is central to the pathophysiology underlying paraneoplastic syndrome in breast cancer. An immunological response is elicited by the ectopic expression of intra- or extracellular neuronal antigens by the tumour,10 which leads to cross-reactivity between the tumour cells and components of the nervous system. This creates anti-tumoral antibodies and associated onconeuronal antigen-specific T lymphocytes that attack the nervous system, producing neurological symptoms. In a review by Altaha et al, specific autoantibodies were detected in 36% of patients with breast cancer-associated paraneoplastic neurological syndromes.11 Roja et al found that onconeural antibodies were present in only half of patients with paraneoplastic breast cancer.12
A definite diagnosis of paraneoplastic polymyositis was confirmed in our case due to symmetrical proximal muscle weakness, a lack of dermatological findings, elevated enzymes, myositis-specific autoantibodies (anti-Jo) and an indicative muscle biopsy. This underlines the rarity and unique presentation of polymyositis as a paraneoplastic syndrome for clinically occult breast cancer.13
Paraneoplastic polymyositis is a medical emergency. Immunological treatment is varied and includes use of corticosteroids, tacrolimus, clophosphamide, intravenous immunoglobulin and rituximab.2 Cancer treatment often leads to symptom improvement in paraneoplastic polymyositis, as described by Minisini et al, who reported a case in which paraneoplastic polymyositis associated with metastatic breast cancer improved after treatment with capecitabine.14 Standard breast cancer therapies are recommended. As in our case, improvement of polymyositis symptoms were noted after cancer treatment with detailed clinical follow-up.
Conclusions
This case has illustrated the difficulties associated with a prompt diagnosis of an unusual case of paraneoplastic polymyositis from breast cancer. A key learning point within our case was an unexplained case of myositis in an adult, which should raise clinical suspicion of underlying causative malignancy, thus requiring a detailed multidisciplinary approach. The development of myositis as a paraneoplastic syndrome can be synchronised with the underlying malignancy or present months to years before the clinical cancer manifestation. FDG-PET is the investigation of choice for detecting clinically occult cancer diagnosis. Due to the high index of suspicion from the neurology team, despite initial normal imaging, a FDG-PET was performed. This showed high uptake in the breast. It was a technically challenging case for the surgical and radiology team to ensure complete tumour resection at the time of breast-conserving surgery. Moreover, the multidisciplinary team played a significant role in patient management.
Metaplastic carcinoma is an aggressive, rare subtype of invasive breast cancer that tends to have an aggressive clinical presentation. Although this patient’s neurological symptoms stabilised following breast surgical treatment coupled with medical management, it is important to note that reoccurrence of myositis could indicate recurrence of the underlying cancer.
Acknowledgements
The authors have no conflicts of interests and no financial ties to disclose.
References
- 1.Pelosof LC, Gerber DE. Paraneoplastic syndromes: an approach to diagnosis and treatment. Mayo Clin Proc 2010; : 838–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Croce S, Guèye M, Korganow AC et al. Paraneoplastic polymyositis associated with breast cancer: a therapeutic emergency. Breast Cancer Res Treat 2011; : 811–814. [DOI] [PubMed] [Google Scholar]
- 3.Buchbinder R, Forbes A, Hall S et al. Incidence of malignant disease in biopsy-proven inflammatory myopathy. A population-based cohort study. Ann Intern Med 2001; : 1,087–1,095. [DOI] [PubMed] [Google Scholar]
- 4.Stertz G. Polymyositis. Berl Klin Wochenschr 1916; : 489. [Google Scholar]
- 5.Christie A, McKay N, Nussey F. Dermatomyositis as presenting feature of ovarian cancer, treated with neo-adjuvant chemotherapy and interval debulking surgery. Gynecol Oncol Case Rep 2013; : 13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhruvil RS, Tseng WH, Martinez SR. Treatment Options for Metaplastic Breast Cancer. ISRN Oncol 2012; : 706162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rakha EA, Lee AH, Evans AJ et al. Tubular carcinoma of the breast: further evidence to support its excellent prognosis. J Clin Oncol 2010; : 99–104. [DOI] [PubMed] [Google Scholar]
- 8.Song YJ, Wu YF, Fan T. Dermatosis as the Initial Manifestation of Malignant Breast Tumors: Retrospective Analysis of 4 Cases. Breast Care (Basel) 2010; : 174–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeh CN, Chen SC, Hwang TL et al. Breast carcinoma in patients with dermatomyositis: a retrospective analysis of eight cases. Chang Gung Med J 2002; : 374–380. [PubMed] [Google Scholar]
- 10.de Beukelaar JW, Sillevis Smitt PA. Managing paraneoplastic neurological disorders. Oncologist 2006; : 292–305. [DOI] [PubMed] [Google Scholar]
- 11.Altaha R, Abraham J. Paraneoplastic neurologic syndrome associated with occult breast cancer: a case report and review of literature. Breast J 2003; : 417–419. [DOI] [PubMed] [Google Scholar]
- 12.Rojas-Marcos I, Rousseau A, Keime-Guibert F et al. Spectrum of paraneoplastic neurologic disorders in women with breast and gynecologic cancer. Medicine (Baltimore) 2003; : 216–223. [DOI] [PubMed] [Google Scholar]
- 13.Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet 2003; : 971–982. [DOI] [PubMed] [Google Scholar]
- 14.Minisini AM, Pauletto G, Bergonzi P et al. Paraneoplastic neurological syndromes and breast cancer. Regression of paraneoplastic neurological sensorimotor neuropathy in a patient with metastatic breast cancer treated with capecitabine: a case study and mini-review of the literature. Breast Cancer Res Treat 2007; : 133–138. [DOI] [PubMed] [Google Scholar]


