Abstract
Laparoscopic Roux-en-Y gastric bypass is one of the most commonly performed bariatric procedures and most patients are women of reproductive age. Consequently, general surgeons and obstetricians need to be aware that these patients are at risk of bariatric specific surgical complications during their pregnancy. We report a case involving a 32-year-old woman who had undergone Roux-en-Y gastric bypass surgery 2 years previously. She presented at 25 weeks of gestation with a closed loop obstruction due to a retrograde jejunojejunal intussusception that was initially misdiagnosed as acute pancreatitis.
Keywords: Gastric bypass, Pregnancy, Intussusception, Small bowel obstruction, Complication
Modification of gastrointestinal tract anatomy by creating two separate limbs (alimentary and biliopancreatic) in patients undergoing Roux-en-Y reconstruction increases the risk of misdiagnosis, especially in patients with small bowel obstruction.1 We report a case involving a pregnant patient with a retrograde intussusception that was originally diagnosed as acute pancreatitis based on symptoms and laboratory findings.
Case history
A 32-year-old woman at 25 weeks of gestation presented to the emergency department of a regional hospital with a 2-day history of abdominal pain, nausea and vomiting. Her medical history included a laparoscopic appendicectomy ten years previously, laparoscopic resection of an ovarian cyst six years previously and a Roux-en-Y gastric bypass (RYGB) for morbid obesity (weight 136kg, body mass index 48kg/m2) two years previously. After the bypass surgery, she lost over 58kg of body weight (current weight 78kg, current body mass index 27kg/m2, estimated excess weight loss 86%). Her obstetric history included two Caesarean deliveries in 2009 and 2011.
On admission, the patient’s abdomen was soft and mildly distended with tenderness in the upper left quadrant. She was afebrile. All laboratory parameters were normal. The patient was discharged with symptomatic treatment. No radiological investigations were performed because of the fetus.
The next day, the patient returned with persistent symptoms. Examination findings of the abdomen were normal but she had tachycardia at 140 beats per minute with normal arterial pressure. Laboratory testing showed an elevated lipase concentration (537u/l, reference range 75–395u/l) and C-reactive protein concentration (108mg/l, reference range <6mg/l). Her white cell blood count was also elevated (20 × 109/l, reference range 4–10 × 109/l), with 83% neutrophils. Acute pancreatitis was diagnosed and the patient was transferred to the medical intensive care unit of a central university hospital.
The patient’s clinical examination findings on admission to the intensive care unit were unchanged but her lipase concentration had increased to 2,300u/l and her white blood count had decreased to 17.9 × 109/l. Right upper quadrant abdominal ultrasonography findings were normal. Distension of the bowel was observed. Fetal ultrasonography findings were normal. Endoscopy showed normal anatomical findings post-RYGB. Forty-eight hours after admission, computed tomography (CT) was performed to evaluate the acute pancreatitis. This showed marked dilation of the excluded stomach and a biliopancreatic limb resulting from an intussusception at the jejunojejunostomy (Fig 1). An emergency consultation with a bariatric surgeon was carried out at this time.
Figure 1.
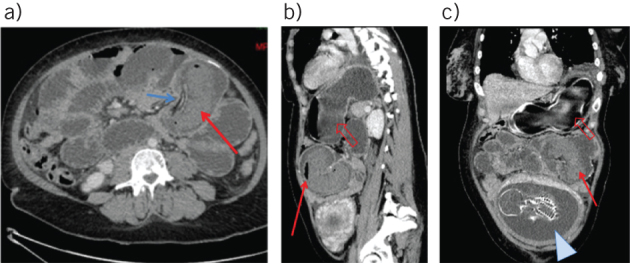
Axial, sagittal and coronal contrast enhanced computed tomography of a 32-year-old woman with a history of Roux-en-Y gastric bypass: sausage-like mass appearance of intussusception (red arrow) with mesenteric vessels inside (blue arrow) (A); markedly dilated gastric remnant (open arrow), air–fluid levels in the intussuscipiens (solid arrow) (B); and fetus (arrowhead) (C)
The patient was taken to theatre. Emergency laparotomy showed antiperistaltic intussusception of the common limb passing back up across the enteroenterostomy and into the Roux limb. A gastrotomy was performed for decompression. The gastrotomy was closed using a linear stapler. The intussusception was reduced, revealing 20cm of non-viable jejunum beginning 5cm distal to the enteroenterostomy. Resection and revision of the jejunojejunal anastomosis (side-to-side) with the Roux limb was performed (Fig 2).
Figure 2.
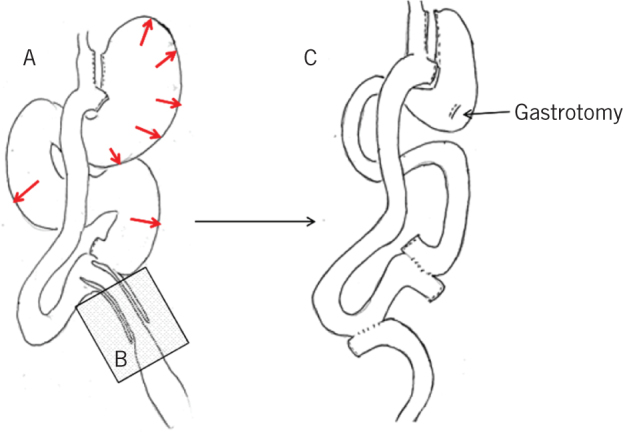
Schematic representation of the intussusception (A), the resection (B) and the reconstruction (C) of the jejunojejunostomy
The patient’s recovery was uneventful. She was discharged 15 days postoperatively, tolerating a regular diet. The pregnancy was also uneventful and the patient gave birth by Caesarean delivery at term.
Discussion
Five cases have been published of intussusception leading to closed loop obstruction in pregnant patients with a history of Roux-en-Y reconstruction (Table 1).2–5 Our patient differs from these cases in that she is the first such patient reported to have elevated plasma concentrations of pancreatic enzymes.
Table 1.
Pregnancies complicated by intussusceptions after Roux-en-Y gastric bypass
| Authors | Time after bypass (BMI) | Gestational age | Initial diagnosis | CT | Intussusception type | Delay between admission and surgery | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Wax, 20072 | 1 yr | 21 wks | Clinical suspicion of internal hernia (several days of abdominal pain) | No | Retrograde | <24h | Laparoscopy. Intussusception of the proximal common channel. Reduction with enteropexy. |
Both in good condition |
| Tohamy, 20093 | 5 yrs | 33 wks | Intussusception (CT at admission) | Yes | Retrograde | <24h | Laparoscopy. Intussusception of the proximal common channel. Reduction. |
Both in good condition |
| Ranade, 20134 | 10 yrs(24kg/m2) | 33 wks | Gastritis | Yes(1 day after admission) | Retrograde | 3 days | Vaginal delivery with oxytocin. Exploration with laparotomy 1 day after delivery. Intussusception of the proximal common channel and perforation. Resection and anastomosis. |
Both in good condition |
| Bokslag, 20145(2 cases) | 1.5 yrs(30kg/m2) | 34 wks | Urinary tract infection; deterioration after 12h | No | Retrograde | <24h | Caesarian (midline) section for fetal distress and abdominal exploration. Intussusception of the JJ anastomosis and perforation. Resection of the JJ anastomosis and revision. |
Both in good condition |
| 9 yrs(25kg/m2) | 24 wks | Intussusception (MRI at admission) | MRI | Retrograde | <24h | Laparoscopic exploration with conversion to laparotomy. Intussusception of the common channel and perforation. Resection of the JJ anastomosis and revision. |
Preterm birth (25 wks) of twins. One perinatal death. |
BMI = body mass index; CT = computed tomography; MRI = magnetic resonance imaging; Rg = retrograde; JJ = jejunojejunal
Our case highlights the difficulty in the management of abdominal pain in patients with a history of bariatric surgery involving Roux-en-Y reconstruction. The unique anatomical changes with RYGB create a number of mesenteric defects and possible retrograde peristalsis. Consequently, internal hernia6 and retrograde intussusception7 can become major causes of small bowel obstruction after RYGB.
Diagnosis is difficult to establish because of a lack of clinical signs. This is especially true in patients with a closed loop obstruction. The nasogastric tube cannot decompress the excluded structures. Obstruction of the biliopancreatic limb presents clinically only with abdominal pain6 located in the upper part of the abdomen owing to distension of excluded structures. An associated elevation of plasma pancreatic enzyme concentrations has also been well documented.8 Considering that rapid weight loss after bariatric surgery is associated with gallstone formation,9 acute pancreatitis often appears to be the more likely scenario.
McGowan and Wills were the first to report that the presence of a history of gastrectomy or Roux-en-Y anatomy should be determined in patients presenting with an acute abdominal condition with high plasma pancreatic enzyme concentrations.10 If such a history is present, pancreatic enzyme levels should be discounted as evidence of acute pancreatitis. Spector et al proposed that in patients with a history of laparoscopic RYGB who present with abdominal pain, an elevated amylase or lipase concentration should be considered as a marker of small bowel obstruction.8 Appropriate radiological evaluation should be performed by an expert radiologist familiar with the anatomical considerations.
Conclusions
In our case, the presence of a developing fetus resulted in the physicians’ reluctance to proceed with appropriate radiological imaging involving irradiation. For pregnant patients, a safe option is magnetic resonance imaging5 for exploration of the biliary tree and pancreas, and at the same time, for identifying bowel pathology. If magnetic resonance imaging is not available, CT should be performed. Nevertheless, in cases of internal hernia, the diagnosis (even with CT) might be missed. The threshold for laparoscopic exploration must therefore be low.
References
- 1.Elms L, Moon RC, Varnadore S et al. . Causes of small bowel obstruction after Roux-en-Y gastric bypass: a review of 2,395 cases at a single institution. Surg Endosc 2014; : 1,624–1,628. [DOI] [PubMed] [Google Scholar]
- 2.Wax JR, Wolff R, Cobean R et al. . Intussusception complicating pregnancy following laparoscopic Roux-en-Y gastric bypass. Obes Surg 2007; : 977–999. [DOI] [PubMed] [Google Scholar]
- 3.Tohamy AE, Eid GM. Laparoscopic reduction of small bowel intussusception in a 33-week pregnant gastric bypass patient: surgical technique and review of literature. Surg Obes Relat Dis 2009; : 111–115. [DOI] [PubMed] [Google Scholar]
- 4.Ranade A, Shah BC, Oleynikov D. Intussusception during pregnancy of a gastric bypass patient. Surg Obes Relat Dis 2013; : e84–e85. [DOI] [PubMed] [Google Scholar]
- 5.Bokslag A, Jebbink J, De Wit L et al. . Intussusception during pregnancy after laparoscopic Roux-en-Y gastric bypass. BMJ Case Rep 2014; bcr2014205357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stenberg E, Szabo E, Ågren G et al. . Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet 2016; : 1,397–1,404. [DOI] [PubMed] [Google Scholar]
- 7.Stephenson D, Moon RC, Teixeira AF, Jawad MA. Intussusception after Roux-en-Y gastric bypass. Surg Obes Relat Dis 2014; : 666–670. [DOI] [PubMed] [Google Scholar]
- 8.Spector D, Perry Z, Shah S et al. . Roux-en-Y gastric bypass: hyperamylasemia is associated with small bowel obstruction. Surg Obes Relat Dis 2015; : 38–43. [DOI] [PubMed] [Google Scholar]
- 9.Shiffman ML, Sugerman HJ, Kellum JM et al. . Gallstone formation after rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am J Gastroenterol 1991; : 1,000–1,005. [PubMed] [Google Scholar]
- 10.McGowan GK, Wills MR. Diagnostic value of plasma amylase, especially after gastrectomy. BMJ 1964; : 160–162. [DOI] [PMC free article] [PubMed] [Google Scholar]


