Abstract
INTRODUCTION
The development of pancreatic infection is associated with the development of a deteriorating disease with subsequent high morbidity and mortality. There is agreement that in mild pancreatitis there is no need to use antibiotics; in severe pancreatitis it would appear to be a logical choice to use antibiotics to prevent secondary pancreatic infection and decrease associated mortality.
MATERIALS AND METHODS
A non-systematic review of current evidence, meta-analyses and randomized controlled trials was conducted to assess the role of prophylactic antibiotics in acute pancreatitis and whether it might improve morbidity and mortality in pancreatitis.
RESULTS
Mixed evidence was found to support and refute the role of prophylactic antibiotics in acute pancreatitis. Most studies have failed to demonstrate much benefit from its routine use. Data from our unit suggested little benefit of their routine use, and showed that the mortality of those treated with antibiotics was significantly higher compared with those not treated with antibiotics (9% vs 0%, respectively, P = 0.043). In addition, the antibiotic group had significantly higher morbidity (36% vs 5%, respectively, P = 0.002).
CONCLUSIONS
Antibiotics should be used in patients who develop sepsis, infected necrosis-related systemic inflammatory response syndrome, multiple organ dysfunction syndrome or pancreatic and extra-pancreatic infection. Despite the many other factors that should be considered, prompt antibiotic therapy is recommended once inflammatory markers are raised, to prevent secondary pancreatic infection. Unfortunately, there remain many unanswered questions regarding the indications for antibiotic administration and the patients who benefit from antibiotic treatment in acute pancreatitis.
Keywords: Acute Pancreatitis, Pancreatic Infection, Antibiotics, SIRS, Necrotising Pancreatitis
Introduction
Acute pancreatitis is not an uncommon gastrointestinal emergency. Its incidence varies from 5 to 80 cases per 100,000 inhabitants per year, with an overall mortality rate of 10–15%.1 More than two-thirds of patients will recover within 1 week. The remaining one-third will experience multiple systemic and/or local complications, with a high mortality rate of 10–30%, 80% of deaths being due to infectious complications.3
The use and efficacy of prophylactic antibiotic therapy in acute pancreatitis has long been a point of controversy. The role of prophylactic antibiotics to prevent infection and reduce mortality in pancreatitis was first evaluated in the 1970s, where several randomised controlled trials (RCTs) had been conducted and concluded that prophylactic antibiotics were effective in preventing secondary pancreatic infections and therefore in reducing the related mortality.4–6 However, in the 2000s, there have been multiple large controlled trials, with conflicting results,7–9 different consensuses reached and differing guidelines for the use of prophylactic antibiotics.10
We review the literature and the different attitudes towards and guidelines for the routine use of prophylactic antibiotics to prevent infectious complications and decrease the mortality from acute pancreatitis, and outline the situations where antibiotics may have a definite role and should be used.
Infection in pancreatitis: focus on mechanism of secondary pancreatic infection
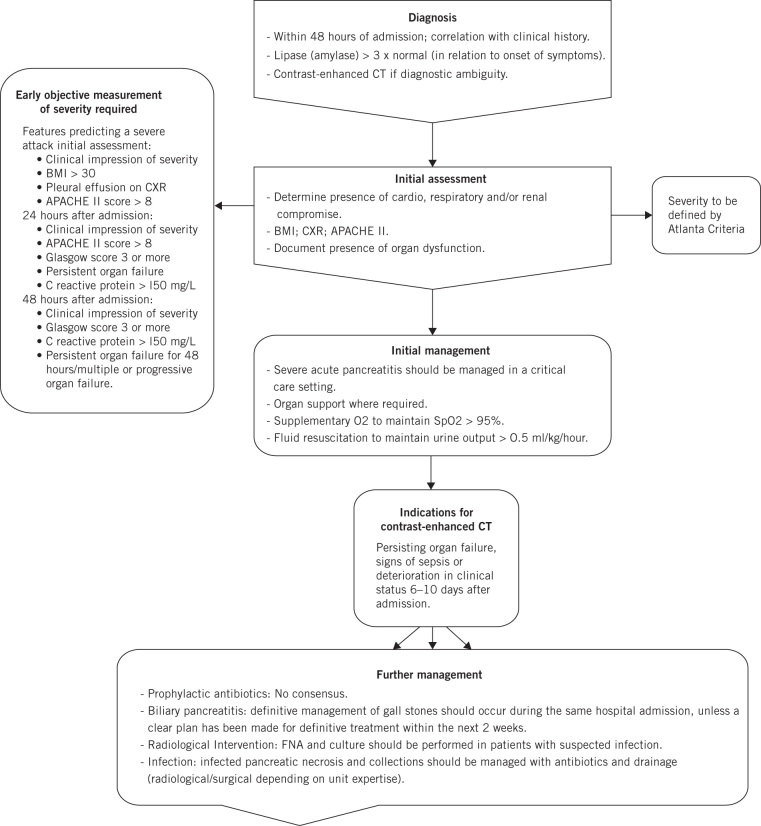
Acute pancreatitis is a self-limiting disease. It ranges from a mild degree inflammation that lasts for few days to severe pancreatitis, which is a serious and life-threatening condition that needs close observation and multidisciplinary management, especially in the presence of multiple organ failure or severe pancreatic infections (Fig 1).
Figure 1.
Acute pancreatitis management
Severe pancreatitis comprises two phases.12 The early stage – the first 14 days from the onset of the disease – is characterised by a systemic inflammatory response syndrome (SIRS), which may be complicated by multiple organ dysfunction syndrome (MODS). In 15–20% of cases, this may be followed by a stage of secondary bacterial infection within the inflamed pancreas, typically 2–3 weeks from the onset of pancreatitis.13
Pathogenesis of secondary bacterial pancreatic infection is still debated. Pathogens can reach the pancreas through the haematogenous pathway, via the biliary system, ascending from the duodenum via the main pancreatic duct, or through transmural colonic migration via translocation of the colonic bacteria to the lymphatics. Most pathogens in pancreatic infection are gastrointestinal Gram-negative bacteria (Escherichia coli, Pseudomonas, Proteus, Klebsiella), which occur via disruption of the intestinal flora and damage to the bowel mucosa. Impaired body defences predispose to translocation of the gastrointestinal organisms and toxins with subsequent secondary pancreatic infection. But Gram-positive bacteria (Staphylococcus aureus, Streptococcus faecalis, Enterococcus), anaerobes and, occasionally, fungi have also been found.14–16 Infection of sterile necrosis is attributed to bacteria of gut origin in up to 70% of cases.17
In mild pancreatitis, the mortality rate is less than 1%,12 in contrast to severe pancreatitis, which ranges from 10% in cases of sterile pancreatic necrosis to as high as 25% with infected necrosis.17 Consequently, interest has focused on the identification of pancreatic necrosis and the potential benefits of prophylactic antibiotics to prevent secondary infection of the necrotic pancreatic tissue.
Mortality in pancreatitis: are antibiotics protective?
Infection in acute pancreatitis has been encountered in 30–40% of patients. The most dangerous is necrotising pancreatitis, which constitutes around 30% of this group, with reported associated poor prognosis and high mortality. Furthermore, 80% of deaths from acute pancreatitis are due to secondary pancreatic infection.18 The use of antibiotic prophylactically in acute pancreatitis is still a matter of controversy, however. Many authors have advocated their use routinely, while others have condemned this practice.
UK guidelines and consensus statements have advocated the prompt and judicious use of antibiotic prophylaxis in the setting of severe acute pancreatitis.19 The role of prophylactic antibiotics in severe acute pancreatitis with associated necrosis remains unclear. Eighteen meta-analyses of RCTs were identified, between the years 1998 and 2015, which sought to determine whether prophylactic antibiotics reduce mortality and the incidence of infection in pancreatic necrosis in patients with severe acute pancreatitis and necrotising pancreatitis (Table 1). The number of trials in each meta-analysis varied from 3 to 11, with a total study population ranging from 160 to 1,279 patients. Overall, 6 of the 18 studies concluded that prophylactic antibiotics significantly reduced total mortality, which includes 17 RCTs,18,20–24 while 4 studies concluded that prophylactic antibiotics significantly reduced the incidence of pancreatic necrosis.18,20,25,26 The two most recent studies included,20 supported the use of antibiotics.
Table 1.
Meta-analyses showing benefits of antibiotic treatment in acute pancreatitis
| Study | Year | Study type | Studies (n) | Patients | Pancreatitisa | Significant reduction with antibiotics | ||
|---|---|---|---|---|---|---|---|---|
| Total(n) | Controls(n) | All-cause mortality | Infection/pancreatic necrosis | |||||
| Ukai et al20 | 2015 | RCT | 6 | 397 | 195 | NP | Yes | Yes |
| Lim et al21 | 2015 | RCT (9) Cohort (2) | 11 | 864 | 413 | NP | All studies: Yes RCT alone: No Cohort alone: Yes |
No |
| Jiang et al31 | 2012 | RCT | 11b | 183 (< 2000) 439 (> 2000) | 95 219 | SAP | Yes < 2000 No > 2000 | – |
| Wittau et al32 | 2011 | RCT | 14 | 841 | 421 | SAP | No | No |
| Bai et al33 | 2010 | RCT | 9 | 519 | 256 | NP | No | No |
| Yao et al25 | 2010 | RCT | 9 | 564 | 277 | NP | No | Yes |
| Villatoro et al27 | 2010 | RCT | 7 | 404 | 201 | NP | No | No |
| Jafri et al30 | 2009 | RCT | 8 | 502 | 249 | SAP | No | No |
| Hart et al34 | 2008 | RCT | 7 | 429 | NP | No | No | |
| Bai et al38 | 2008 | RCT | 7 | 467 | 231 | NP | No | No |
| Xu et al26 | 2008 | RCT | 8 | 540 | 270 | NP | No | Yes |
| Dambrauskas et al18 | 2007 | RCT | 10 | 1,279 | 638 | NP | Yes | Yes |
| De Vries et al35 | 2007 | RCT | 6 | 397 | 194 | SAP | No | No |
| Mazaki et al36 | 2006 | RCT | 6 | 329 | 162 | NP | No | No |
| Xiong et al37 | 2006 | RCT | 6 | 338 | 165 | SAP | No | No |
| Villatoro et al22 | 2006 | RCT | 5 | 294 | NP | Yes | No | |
| Sharma et al23 | 2001 | RCT | 3 | 160 | 76 | NP | Yes | No |
| Golub et al24 | 1998 | RCT | 8 | 514 | 255 | SAP | Yes | – |
NP, necrotising pancreatitis; RCT, randomised controlled trial; SAP, severe acute pancreatitis
a All patients with SAP/NP alone.
b 4 up to year 2000, 7 after 2000 (no studies in year 2000 itself)
Ukai et al20 included six RCTs in which antibiotics (within 72 hours) were administered early in patients with acute necrotising pancreatitis, with the exclusion of studies with delayed or indeterminate timing of antibiotic administration. This meta-analysis showed a significant reduction in mortality and the incidence of infected pancreatic necrosis if prophylactic antibiotics are administrated early. However, this study had several limitations, as RCTs included in this study compared the use and non-use of antibiotics, not the timing of administration. The study advocates further RCTs to determine the effect of the timing of antibiotic administration on mortality and pancreatic necrosis infection.
Lim et al21 analysed nine RCTs and two cohort studies to determine the benefits of prophylactic antibiotics. The study did not show a significant reduction in the incidence of pancreatic necrosis in the total study population, RCT population or cohort population. However, total mortality was significantly reduced in the named groups. Importantly, analysis of the nine RCTs did not show a significant reduction in mortality with prophylactic antibiotics. A significant limitation of the study was the heterogeneity of the studies analysed, with mixed treatment regimens and populations. Although the study suggested benefits of prophylactic antibiotic in all-cause mortality, we must be aware that this was not significant in the RCT population. In addition, the study did not demonstrate a reduction in infection within pancreatic necrosis in any study population.
The largest meta-analysis, by Dambrauskas et al18 in 2007, used 10 RCTs with a total study population of 1,279, which showed a significant reduction in mortality and incidence of infected pancreatic necrosis with prophylactic antibiotics. This study incorporated RCTs used in previous studies by Sharma et al23 and Golub et al,24 which had both advocated the use of prophylactic antibiotics to significantly reduce mortality. Dambrauskas et al18 excluded previous work assessing the role of penicillins as it was ‘separately evaluated and did not show any beneficial effect in this meta-analysis’. Studies using penicillins were also excluded as they have poor pancreatic penetrance. The study concluded that carbapenems are associated with a significant reduction in mortality and incidence of infected pancreatic necrosis compared with other intravenous antibiotics.
Villatoro et al22 performed a meta-analysis in 2006 including five RCTs with a total of 294 patients, which showed a significant reduction in mortality but not the incidence of infection in pancreatic necrosis. Villatoro et al27 reanalysed the data in 2010, including a further two RCTs and increasing the meta-analysis population to 404 patients.28 This reanalysis did not show a significant reduction in mortality or incidence of infection in pancreatic necrosis. Subgroup analysis did identify a significant reduction in infected pancreatic necrosis patients receiving imipenem. The meta-analysis also concluded that the RCTs used for analysis were not adequately powered.
A greater body of evidence currently does not support the use of prophylactic antibiotics. As mentioned above, 6 of the 18 studies included in the current review were associated with reduced mortality when prophylactic antibiotics were used and the remaining 12 meta-analyses did not recommend the use of prophylactic antibiotic as there was no significant reduction in mortality with them.25–27,30–38 These meta-analyses used a combined total of 14 RCTs with total study population varied from 329 to 841 patients.
We agree with the recent pooled evidence that prophylactic antibiotics in patients with acute pancreatitis are not associated with a significant decrease in mortality or morbidity. Recently, unpublished data from our unit showed overall mortality of 3.3% and morbidity of 16.7% following admission of acute pancreatitis patients. The mortality rate of those treated with antibiotics was significantly higher compared with those treated without antibiotic (9% vs 0%, respectively, P = 0.043). The antibiotic group had significantly higher morbidity (36% vs 5%, respectively, P = 0.002). This probably reflects our rationale of no role for antibiotics in acute pancreatitis except with defined indications for their use, which is discussed in the next section.
Situations where physicians should suggest the use of antibiotics
Many authors claim that prophylactic antibiotics in all patients with acute pancreatitis is not associated with a significant decrease in secondary pancreatic infection and mortality. Thus, we do not recommend routine prophylactic antibiotics for all patients with acute pancreatitis.
We agree with Dambrauskas et al39 and Ukai et al20 that prompt use of antibiotics once the physician detects early raised inflammatory markers (which carries a high risk of secondary pancreatic infection) is mandatory and this subset of patients benefits most from timely administration of antibiotics. Riche et al40 showed that procalcitonin and interleukin 6 serum levels were elevated very early in patients who eventually developed necrosis infection. Biomarkers should be used in addition to clinical information to identify a subgroup of patients in whom antibiotic prophylaxis is likely to be ineffective.
On the other hand, many factors must be considered when managing patient with severe acute pancreatitis: the nutritional status of the patient, the timing of antibiotic administration, timing and type of surgery, the necessity of percutaneous drainage or laparoscopy, the treatment of gallstone pancreatitis and whether patients were monitored in an intensive care unit. We recommend the use of prophylactic antibiotics in acute pancreatitis in patients with increased white blood count or overt clinical signs of sepsis (hypotension, fever, collapse – following adequate resuscitation).
Surgical intervention in patients with sepsis secondary to acute pancreatitis is associated with very poor outcome; hence, early identification of pancreatic infection was attempted, with good results obtained by radiologically guided fine-needle aspiration. Ultrasonographically guided fine-needle aspiration cytology is a safe, fast and reliable technique for the diagnosis of infected necrosis and is recommended to differentiate infected from sterile pancreatic necrosis, and where systemic inflammatory response syndrome persists beyond the first week after onset of symptoms.41
Antibiotics in pancreatitis: focus on type of antimicrobials
The ideal drug to use should:
have specific activity against the bacteria responsible for pancreatic infections
be able to penetrate the pancreatic tissue, pancreatic exocrine secretions, and peri-pancreatic fluid/exudates at therapeutic mean inhibitory concentrations
be able to penetrate the pancreas during acute pancreatitis; and
have a clear-cut clinical capacity to reduce the development of infected necrosis.42
There is no evidence to support the previous criteria of ideal antibiotics, and physicians should realise that pancreatic infection normally starts in necrotic tissue. No antibiotics effectively penetrate necrotic tissue without blood supply, which makes pancreatic infections sometimes very resistant to antibiotics.
Imipenem, clindamycin, piperacillin, fluoroquinolones and metronidazole are known to have adequate tissue penetration and bactericidal properties in infected pancreatic necrosis, in contrast to penicillins, first-generation cephalosporins, aminoglycosides and tetracyclines, which are ineffective in acute pancreatitis.43 Meropenem is shown to have as wide a spectrum as imipenem in preventing septic complications in acute pancreatitis.45 The use of systemic antibiotics in pancreatic infections must be accompanied with drainage, either surgical or percutaneous.
One of the main problems of prolonged administration of antibiotics in severe acute pancreatitis is the development of multidrug resistance bacterial and fungal infection, which is associated with long hospital stay and poor outcome.46 Hence, each case should be individually evaluated, weighing the benefits of antibiotics against the significant adverse events associated with their use, including increased bacterial resistance and fungal infections. Microbiologists with a specific interest in pancreatitis should be involved in such decisions, and blood culture is highly suggested as this might detect bloodstream infections associated with pancreatitis.
Conclusions
Evidence is accumulating to suggest that prophylactic antibiotics in patients with acute pancreatitis is not associated with a significant decrease in secondary pancreatic infection and mortality. We do not therefore recommend routine prophylactic antibiotic therapy for all patients with acute pancreatitis. Conversely, the prompt use of prophylactic antibiotics once a physician detects early markers associated with high risk of pancreatic infection is mandatory.
Being able to identify biomarkers indicating pancreatic infection and whether they predict responsiveness to antibiotics would significantly enhance the clinical management of acute pancreatitis. The considerable variations among patients make it difficult to find solutions in clinical trials using standard cohorts with mean conditions.
References
- 1.Yousaf M, McCallion K, Diamond T. Management of severe acute pancreatitis. Br J Surg 2003; : 407–420. [DOI] [PubMed] [Google Scholar]
- 2.Toouli J, Brooke-Smith M, Bassi C et al. . Working Party of the Program Commitee of the Bangkok World Congress of Gastroenterology. Guidelines for the management of acute pancreatitis. J Gastroenterol Hepatol 2002; : S15–S39. [DOI] [PubMed] [Google Scholar]
- 3.Heinrich S, Schafer M, Rousson V et al. . Evidence-based treatment of acute pancreatitis: a look at established paradigms. Ann Surg 2006; : 154–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howes R, Zuidema GD, Cameron JL. Evaluation of prophylactic antibiotics in acute pancreatitis. J Surg Res 1975; : 197–200. [DOI] [PubMed] [Google Scholar]
- 5.Finch WT, Sawyers JL, Schenker S. A prospective study to determine the efficacy of antibiotics in acute pancreatitis. Ann Surg 1976; : 667–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Witt C, Brinkhaus B, Jena S et al. . Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet 2005; : 136–143. [DOI] [PubMed] [Google Scholar]
- 7.Isenmann R, Runzi M, Kron M et al. . German Antibiotics in Severe Acute Pancreatitis Study G. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology 2004; : 997–1004. [DOI] [PubMed] [Google Scholar]
- 8.Xue P, Deng LH, Zhang ZD et al. . Effect of antibiotic prophylaxis on acute necrotizing pancreatitis: results of a randomized controlled trial. J Gastroenterol Hepatol 2009; : 736–742. [DOI] [PubMed] [Google Scholar]
- 9.Jiang K, Huang W, Yang XN et al. . Present and future of prophylactic antibiotics for severe acute pancreatitis. World J Gastroenterol 2012; : 279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nathens AB, Curtis JR, Beale RJ et al. . Management of the critically ill patient with severe acute pancreatitis. Crit Care Med 2004; : 2,524–2,536. [DOI] [PubMed] [Google Scholar]
- 11.Takeda K, Takada T, Kawarada Y et al. . JPN Guidelines for the management of acute pancreatitis: medical management of acute pancreatitis. J Hepatobiliary Pancreat Surg 2006; : 42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uhl W, Warshaw A, Imrie C et al. , International Association of P. IAP Guidelines for the Surgical Management of Acute Pancreatitis. Pancreatology 2002; : 565–573. [DOI] [PubMed] [Google Scholar]
- 13.Dupuis CS, Baptista V, Whalen G et al. . Diagnosis and management of acute pancreatitis and its complications. Gastrointest Interv 2013; : 36–46. [Google Scholar]
- 14.Luiten EJ, Hop WC, Lange JF et al. . Controlled clinical trial of selective decontamination for the treatment of severe acute pancreatitis. Ann Surg 1995; : 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sedman PC, Macfie J, Sagar P et al. . The prevalence of gut translocation in humans. Gastroenterology 1994; : 643–649. [DOI] [PubMed] [Google Scholar]
- 16.Schmid SW, Uhl W, Friess H et al. . The role of infection in acute pancreatitis. Gut 1999; : 311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dervenis C, Johnson CD, Bassi C et al. . Diagnosis, objective assessment of severity, and management of acute pancreatitis. Santorini Consensus Conference. Int J Pancreatol 1999; : 195–210. [DOI] [PubMed] [Google Scholar]
- 18.Dambrauskas Z, Gulbinas A, Pundzius J et al. . Meta-analysis of prophylactic parenteral antibiotic use in acute necrotizing pancreatitis. Medicina (Kaunas) 2007; : 291–300. [PubMed] [Google Scholar]
- 19.UK Working Party on Pancreatitis. UK guidelines for the management of acute pancreatitis. Gut 2005; : iii1–iii9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ukai T, Shikata S, Inoue M et al. . Early prophylactic antibiotics administration for acute necrotizing pancreatitis: a meta–analysis of randomized controlled trials. J Hepatobiliary Pancreat Sci 2015; : 316–321. [DOI] [PubMed] [Google Scholar]
- 21.Lim CLL, Lee W, Liew YX et al. . Role of antibiotic prophylaxis in necrotizing pancreatitis: a meta–analysis. J Gastrointest Surg 2015; : 480–491. [DOI] [PubMed] [Google Scholar]
- 22.Villatoro E, Bassi C, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev 2006; : CD002941. [DOI] [PubMed] [Google Scholar]
- 23.Sharma VK, Howden CW. Prophylactic antibiotic administration reduces sepsis and mortality in acute necrotizing pancreatitis: a meta-analysis. Pancreas 2001; : 28–31. [DOI] [PubMed] [Google Scholar]
- 24.Golub R, Siddiqi F, Pohl D. Role of antibiotics in acute pancreatitis: a meta-analysis. J Gastrointest Surg 1998; : 496–503. [DOI] [PubMed] [Google Scholar]
- 25.Yao L, Huang X, Li Y et al. . Prophylactic antibiotics reduce pancreatic necrosis in acute necrotizing pancreatitis: a meta-analysis of randomized trials. Digest Surg 2010; : 442–449. [DOI] [PubMed] [Google Scholar]
- 26.Xu T, Cai Q. Prophylactic antibiotic treatment in acute necrotizing pancreatitis: results from a meta-analysis. Scand J Gastroenterol 2008; : 1,249–1,258. [DOI] [PubMed] [Google Scholar]
- 27.Villatoro E, Mulla M, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev 2010; : CD002941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dellinger EP, Tellado JM, Soto NE et al. . Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized, double-blind, placebo-controlled study. Ann Surg 2007; : 674–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Røkke O, Bache Harbitz T, Liljedal J et al. . Early treatment of severe pancreatitis with imipenem: a prospective randomized clinical trial. Scand J Gastroenterol 2007; : 771–776. [DOI] [PubMed] [Google Scholar]
- 30.Jafri NS, Mahid SS, Idstein SR et al. . Antibiotic prophylaxis is not protective in severe acute pancreatitis: a systematic review and meta-analysis. Am J Surg 2009; : 806–813. [DOI] [PubMed] [Google Scholar]
- 31.Jiang K, Huang W, Yang X-N et al. . Present and future of prophylactic antibiotics for severe acute pancreatitis. World J Gastroenterol 2012; : 279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wittau M, Mayer B, Scheele J et al. . Systematic review and meta–analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol 2011; : 261–270. [DOI] [PubMed] [Google Scholar]
- 33.Bai Y, Gao J, Zou D-W et al. . Antibiotics prophylaxis in acute necrotizing pancreatitis: an update. Am J Gastroenterol 2010; : 705–707. [DOI] [PubMed] [Google Scholar]
- 34.Hart PA, Bechtold ML, Marshall JB et al. . Prophylactic antibiotics in necrotizing pancreatitis: a meta-analysis. South Med J 2008; : 1,126–1,131. [DOI] [PubMed] [Google Scholar]
- 35.de Vries AC, Besselink MGH, Buskens E et al. . Randomized controlled trials of antibiotic prophylaxis in severe acute pancreatitis: relationship between methodological quality and outcome. Pancreatology 2007; : 531–538. [DOI] [PubMed] [Google Scholar]
- 36.Mazaki T, Ishii Y, Takayama T. Meta-analysis of prophylactic antibiotic use in acute necrotizing pancreatitis. Br J Surg 2006; : 674–684. [DOI] [PubMed] [Google Scholar]
- 37.Xiong GS, Wu SM, Wang ZH. Role of prophylactic antibiotic administration in severe acute pancreatitis: a meta-analysis. Med Principles Practice 2006; : 106–110. [DOI] [PubMed] [Google Scholar]
- 38.Bai Y, Gao J, Zou D-W et al. . Prophylactic antibiotics cannot reduce infected pancreatic necrosis and mortality in acute necrotizing pancreatitis: evidence from a meta-analysis of randomized controlled trials. Am J Gastroenterol 2008; : 104–110. [DOI] [PubMed] [Google Scholar]
- 39.Dambrauskas Z, Pundzius J, Barauskas G. Predicting development of infected necrosis in acute necrotizing pancreatitis. Medicina 2006; : 441–449. [PubMed] [Google Scholar]
- 40.Riche FC, Cholley BP, Laisne MJ et al. . Inflammatory cytokines, C reactive protein, and procalcitonin as early predictors of necrosis infection in acute necrotizing pancreatitis. Surgery 2003; : 257–262. [DOI] [PubMed] [Google Scholar]
- 41.Rau B, Pralle U, Mayer JM et al. . Role of ultrasonographically guided fine–needle aspiration cytology in the diagnosis of infected pancreatic necrosis. Br J Surg 1998; : 179–184. [DOI] [PubMed] [Google Scholar]
- 42.Bassi C, Mangiante G, Falconi M et al. . Prophylaxis for septic complications in acute necrotizing pancreatitis. J Hepatobiliary Pancreatic Surg 2001; : 211–215. [DOI] [PubMed] [Google Scholar]
- 43.Demetri GD, von Mehren M, Antonescu CR et al. . NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 2010; : S1–41; quiz S42–S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Trudel JL, Wittnich C, Brown RA. Antibiotics bioavailability in acute experimental pancreatitis. J Am Coll Surg 1994; : 475–479. [PubMed] [Google Scholar]
- 45.Manes G, Rabitti PG, Menchise A et al. . Prophylaxis with meropenem of septic complications in acute pancreatitis: a randomized, controlled trial versus imipenem. Pancreas 2003; : e79–e83. [DOI] [PubMed] [Google Scholar]
- 46.Isenmann R, Schwarz M, Rau B et al. . Characteristics of infection with Candida species in patients with necrotizing pancreatitis. World J Surg 2002; : 372–376. [DOI] [PubMed] [Google Scholar]