Abstract
Tailgut cysts are rare benign retrorectal cysts arising from persistent remnants of an embryonic hindgut. Malignant transformation inside this lesion is very uncommon and occurrence of neuroendocrine tumours in this context is extremely rare. We report the case of a 56-year-old woman who underwent surgical excision of a presacral tailgut cyst, which was found incidentally to include a neuroendocrine tumour.
Keywords: Retrorectal cystic hamartoma, Tailgut cyst, Neuroendocrine tumour, Presacral tumour, Posterior approach
Tailgut cysts (TGCs) are rare benign cysts that are found in the presacral space, usually in middle aged women. They are developmental lesions from persistent remnants of an embryonic hindgut. The possible complications of a TGC are mainly infection and malignancy.1,2 Tumours inside a TGC are extremely rare and malignancies mostly comprise adenocarcinomas or neuroendocrine tumours (NETs).3 A NET in the presacral space is likely to be secondary to direct extension or metastatic invasion of a primary rectal malignancy.4
Preoperative diagnosis of a NET within a TGC is difficult; NETs are usually found incidentally on histological examination. We present a new case of a NET within a TGC in a female patient and summarise the clinicopathological characteristics of these tumours.
Case history
A 56-year-old woman with an anal fistula was referred to our department. She had experienced anal discomfort and suppuration for two months. On physical examination, an external orifice was observed, and a painless and soft retrorectal mass was palpated on digital rectal examination. Tumour marker values (carcinoembryonic antigen, carbohydrate antigen) were unremarkable. The lesion was further evaluated using magnetic resonance imaging (MRI), which revealed a 4.1 cm × 4.1 cm mass with both cystic and solid components located in the retrorectal space. It was a well-defined and non-enhancing lesion with partial hyperintensity on T1-weighted imaging and heterogeneous high signal intensity on T2 imaging (Fig 1). The mass displaced the posterior rectal wall without infiltration; local invasion was not detected. Endorectal ultrasonography was performed and a heterogeneous retrorectal mass was found; the posterior rectal wall was unaltered (Fig 2).
Figure 1.
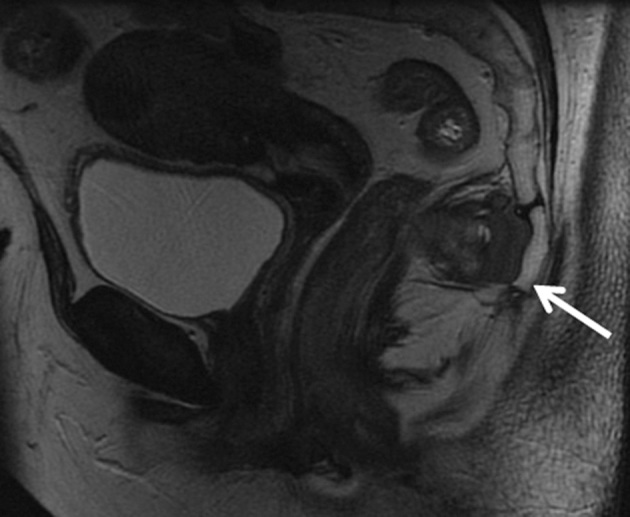
T2-weighted coronal magnetic resonance imaging demonstrating a mass with both cystic and solid components located in the retrorectal space (arrow), which displaced the posterior rectal wall without infiltration
Figure 2.
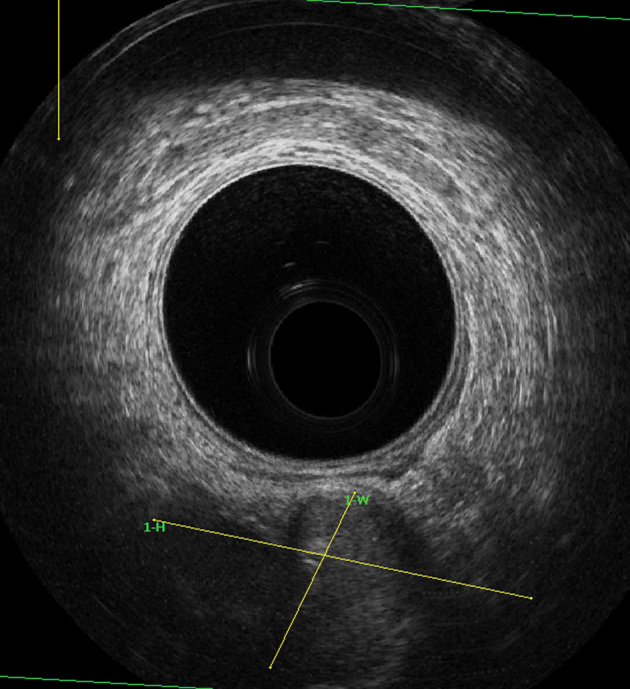
Endorectal ultrasonography demonstrating a heterogeneous retrorectal mass
The patient underwent a complete resection via a transsacral approach (Kraske); fistula-in-ano was not detected intraoperatively. A partial coccygectomy was included to achieve better surgical exposure and a biological mesh was fixed to the levator ani muscle after the tumour resection. Primary closure was carried out without drains. There were no lesions in the anal sphincter or blood loss.
Histopathological examination (Fig 3) revealed a well delineated multilocular cyst and a solid lesion measuring 4.5 cm × 2.5 cm. Microscopically, the cystic space contained mucinous material and no contiguous osseous tissue, hair or other structures were identified. In addition, a tumour composed of multiple solid nests of uniform epithelial cells distributed in a fibrovascular network without necrosis was encountered in the cystic component. The cells had rounded nuclei with speckled chromatin and inconspicuous nucleoli. The tumour showed neuroendocrine immunoreactivity (Fig 4) for the markers cytokeratin AE1/AE3, CD56, synaptophysin and chromogranin. The Ki-67 proliferation index was less than 2%. Findings were consistent with a diagnosis of a well-differentiated (low-grade) NET.
Figure 3.
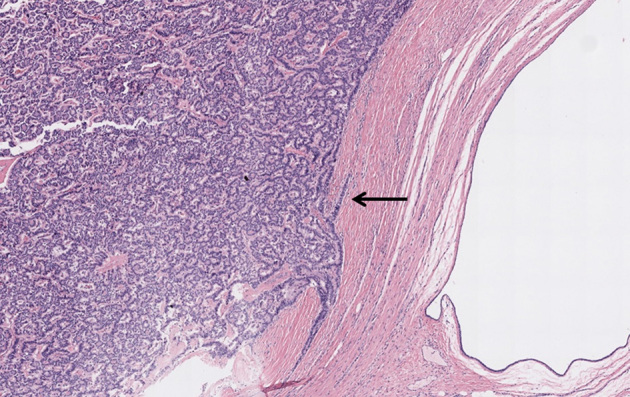
Histological features of the tailgut cyst (haematoxylin and eosin stain, 40× magnification)
Figure 4.
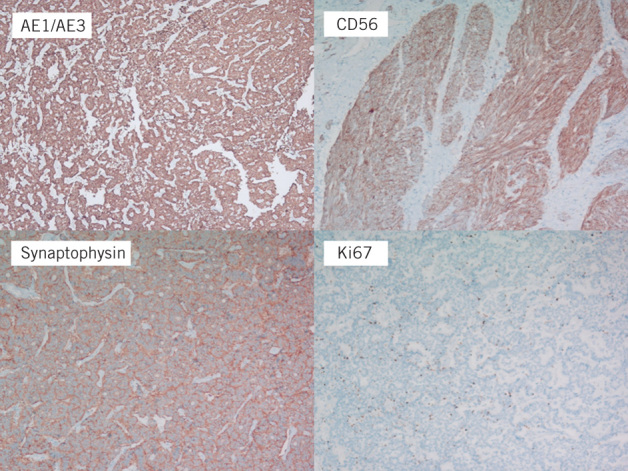
Immunoreactivity and Ki-67 proliferation index for tumour cells with neuroendocrine differentiation (400× magnification)
The patient’s postoperative course was uneventful and she was discharged after five days. At seven months following surgery, she is asymptomatic with no evidence of complications or recurrence.
Discussion
TGCs are uncommon retrorectal tumours that should be considered among the differential diagnosis of presacral lesions. Possible diagnoses in this area include teratoma, dermoid cyst, duplication or enterogenous cyst, sacral chordoma, anterior sacral meningocoele, neurogenic tumour and presacral abscess.1 Such tumours are generally described in women (female-to-male ratio 3:1). Approximately half of patients have an incidental diagnosis and are identified by imaging or routine physical examination.1,2
These cysts can rarely include malignant tumours such as adenocarcinomas, sarcomas or NETs.3,4 Only 20 patients with tailgut associated NETs have been reported previously in the medical literature. Given the small number of cases reported, it is hard to know the natural course and prognosis of these tumours.4 This malignant transformation is estimated in 2–13% and it is very difficult to make an accurate preoperative diagnosis, even with biopsy. Some features may support indirect evidence of malignant transformation inside a TGC on MRI (eg a polypoid mass, an irregular cyst wall or solid components).1,4
Resection of TGC is the treatment of choice. It is essential to prevent and treat potential complications such as infection, bleeding and malignancies. TGCs can be associated with morbidity and mortality if malignancy is not suspected and resection is not performed in a timely manner.1,2 Mathis et al reported 31 cases of TGC with 4 of these lesions including malignant transformation.3 Not all of the patients underwent resection initially and some patients had a preoperative percutaneous biopsy. Two of the four patients with malignancies died during the follow-up period; the authors therefore advise resection of TGCs in all cases.
The malignant potential of NETs is related to histological features, and there is a correlation between pathological grading and prognosis. Long-term survival is associated with complete excision and tumour histology results, with a much better prognosis for NETs than for other tumours such as adenocarcinomas.4 Until now, local recurrence of a TGC has not been described and only two patients developed distant metastases (survival data not available). In addition, none of the previous papers reported the Ki-67 proliferation index, which can indicate how aggressive a tumour is.1,4 Given the predominance in women, Liang et al have suggested that NETs arising in TGCs may be hormone associated and that oestrogen could play a role in the pathogenesis.5 The authors found strong oestrogen receptor immunoreactivity in neuroendocrine cells within a TGC and speculated that oestrogen receptor could be a potential therapeutic target in selected TCG patients.
Conclusions
When managing a TGC, considering the differential diagnosis of a presacral tumour and exhaustive preoperative study are essential. Complete excision allows a definite diagnosis and prevents potential complications. Malignant transformation inside a TGC is rare and careful histological examination is required to assess how aggressive the tumour is.
Acknowledgement
The material in this paper was presented at the 20th Congress of the Spanish Society of Coloproctology held in Elche, Spain, May 2016.
References
- 1.Prasad AR, Amin MB, Randolph TL et al. Retrorectal cystic hamartoma: report of 5 cases with malignancy arising in 2. Arch Pathol Lab Med 2000; : 725–729. [DOI] [PubMed] [Google Scholar]
- 2.Jang SH, Jang KS, Song YS et al. Unusual prerectal location of a tailgut cyst: a case report. World J Gastroenterol 2006; : 5,081–5,083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathis KL, Dozois EJ, Grewal MS et al. Malignant risk and surgical outcomes of presacral tailgut cysts. Br J Surg 2010; : 575–579. [DOI] [PubMed] [Google Scholar]
- 4.Mitsuyama T, Kubota M, Nakamura Y et al. Neuroendocrine tumor arising from tailgut cyst with spinal cord tethering: case report and literature review. Spine J 2015; : e1–e8. [DOI] [PubMed] [Google Scholar]
- 5.Liang JJ, Alrawi S, Fuller GN, Tan D. Carcinoid tumors arising in tailgut cysts may be associated with estrogen receptor status: case report and review of the literature. Int J Clin Exp Pathol 2008; : 539–543. [PMC free article] [PubMed] [Google Scholar]


