Abstract
Deciduosis (ectopic or extrauterine decidua) is a phenomenon seen in the ovary and cervix and on serosal surfaces of abdominal and pelvic organs. It is thought to be the result of progesterone effects on extrauterine mesenchymal cells during pregnancy. Although deposits are typically asymptomatic and incidentally found in surgically removed tissues on microscopy, deciduosis has also been known to cause pain and intraperitoneal haemorrhage.
We sourced all cases of appendiceal deciduosis that have occurred in Sir Charles Gairdner Hospital and Bunbury Hospital between the years 2006 and 2014. Clinical information was obtained from patients’ medical records. Four cases of ectopic decidua of the appendix, all of which were incidentally found in pregnant patients presenting with features highly suggestive of appendicitis, were reviewed. These patients underwent appendicectomy and subsequent histopathology findings showed deciduosis with no evidence of appendicitis.
Deciduosis of the appendix can mimic acute appendicitis in pregnancy. At present, it is difficult to confidently differentiate one from the other either by way of clinical presentation or with current imaging modalities.
Keywords: Appendicitis, Pregnancy, Deciduosis
Introduction
Deciduosis (ectopic or extrauterine decidua) is most commonly seen in the ovary and cervix and, rarely, on serosal surfaces of abdominal and pelvic organs. Although it is typically asymptomatic and incidentally found, it has been documented to cause pain and intraperitoneal haemorrhage.1 We reviewed four cases of ectopic decidua of the appendix, all of which were incidentally found in pregnant patients presenting with features highly suggestive of appendicitis.
Case report
Case 1
A 30-year-old, 26-week gravid woman presented with a 3-day history of right Iliac fossa (RIF) pain. Her white cell count was 16.4 (neutrophilia) and C-reactive protein (CRP) 12. Magnetic resonance imaging (MRI) revealed an 8-mm diameter appendix with surrounding inflammatory change, in keeping with acute appendicitis (Fig 1). An enlarged inflamed appendix was found intraoperatively. Histology reported extensive periappendiceal and serosal decidual reaction without acute inflammation.
Figure 1.
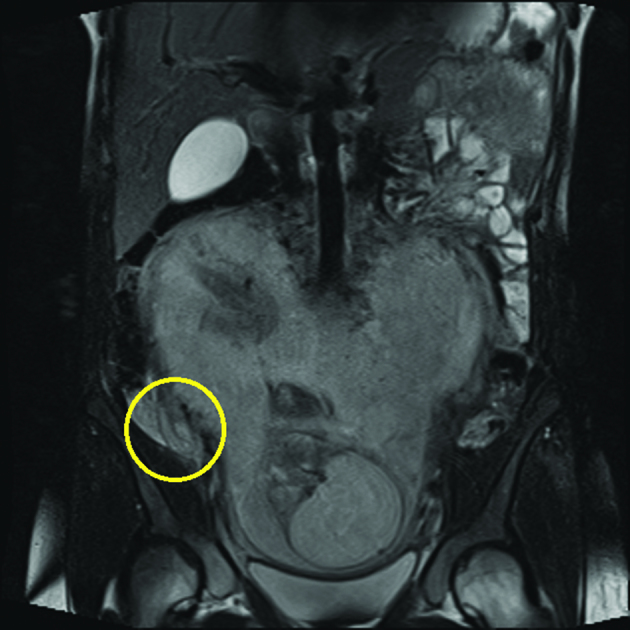
Dilated appendix with periappendiceal fluid collection
Figure 2.
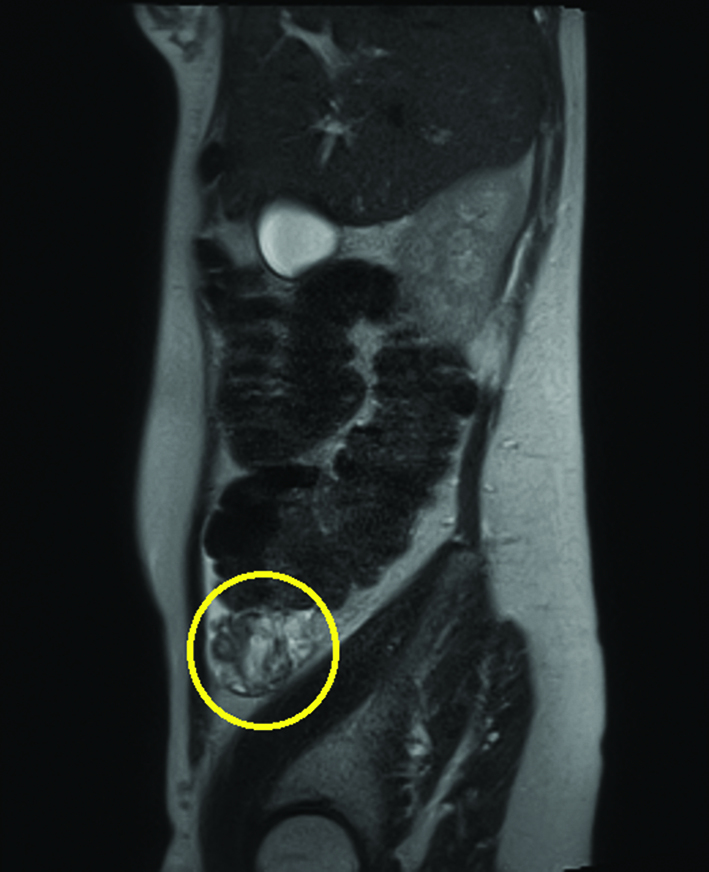
Phlegmon at caecal pole
Case 2
A 36-year-old, 20-week gravid woman presented with a 1-day history of RIF pain radiating to the right groin, associated with nausea. Her white cell count was 13.7 (neutrophilia) and CRP less than 5. There was evidence of urinary tract infection on urine culture. She was initially treated with intravenous ceftriaxone for 48 hours for presumptive pyelonephritis. As the response was poor after 3 days, she was investigated with ultrasound, which showed a non-specific mass in the right iliac fossa and free fluid. MRI revealed phlegmon of the caecal pole, likely secondary to a ruptured appendix. Intraoperatively, the appendix was enlarged. Histology reported subserosal deciduosis without features of acute appendicitis.
Cases 3 and 4
Two pregnant women, one of 35 years and one of 22 years, both presented with signs and symptoms consistent with acute appendicitis. Ultrasound scans were non-diagnostic. Both underwent appendicectomy. Intraoperatively, an inflamed appendix and a normal-looking appendix, respectively, were found. Histopathology reported deciduosis of the appendix with no features of acute appendicitis.
Discussion
Normal decidua consists of endometrial stromal cells transformed during pregnancy in response to ovarian and placental hormones, specifically progesterone. Ectopic decidual transformation is said to be the result of a de novo development from submesothelial stroma or from the decidual transformation of a pre-existing endometriosis during pregnancy.1 Deciduosis of the appendix had rarely been reported in the literature. The first case was described by Hirschberg (1905), in a patient who presented with symptoms consistent with right tubal pregnancy.2
Ectopic decidua has not generally been associated with clinical symptoms. However, appendiceal deciduosis can present with abdominal symptoms mimicking appendicitis. One suggestion for the cause of peritoneal irritation is the mechanical effect of the expanding endometrial tissue in response to increasing sex steroid hormone levels, leading to mechanical compression and irritation of affected tissues. Another possible mechanism is the effect of humoral factors. Decidual tissues have been demonstrated to contain a high concentration of prostaglandins, a substance known to have potent muscle-stimulating properties. These would act locally to induce contraction of muscle wall of the appendix.1
Appendicitis in pregnancy carries an incidence ranging from 1 in 1250 to 1 in 1500 pregnancies. Although uncommon, it represents the surgical complication most commonly encountered during gestation. Diagnosis of acute appendicitis during pregnancy can be challenging; not only does the gravid uterus displace the appendix from its normal anatomical location, the normal gestational leukocytosis also makes the white cell count a less reliable diagnostic tool. The high prevalence of nausea, vomiting and abdominal pain in the normal obstetric patient may also obscure the diagnosis. Ultrasound and MRI should be used to aid diagnosis when feasible.3 The high sensitivity and specificity of MRI for appendicitis in pregnancy (91.7% and 95.3%) makes it the best available investigative tool in the work-up of a patient during pregnancy.4
A fetal loss rate of 3–5% is given with uncomplicated appendicitis but up to 20% in perforated appendicitis. Similarly, maternal mortality also increases in perforated appendicitis. As delay in diagnosis of acute appendicitis has been thought to be associated with higher perforation rate, fetal mortality rate and postoperative mortality, a high index of suspicion must be held and a lower threshold for operative management is warranted. However, an increased rate of fetal loss and early delivery, also observed in women with negative appendicectomy, makes the accuracy of a negative diagnosis equally important.5
In all four cases presented here, the symptoms resolved following appendicectomy. These and the series of cases reported previously support the role of ectopic decidua in the development of clinical features mimicking acute appendicitis in the course of normal pregnancy. One may question whether it had been wise putting these patients through the risks of a negative appendicectomy. Two of the patients had MRI reporting appendicitis, thus making the decision to proceed to surgery obligatory. Surgeons and reporting radiologists should be aware that deciduosis of the appendix can mimic acute appendicitis but if it were possible to identify deciduosis with confidence, conservative management could be an alternative.
References
- 1.Suster S, Moran CA. Deciduosis of the appendix. Am J Gastroenterol 1990, : 841–845. [PubMed] [Google Scholar]
- 2.Hirschberg A. Deciduale zellbildungen am Wurmfortsatz bei Tubenschwangershaft (periappendicitis decidualis). Arch Gynak 1905, : 620–632. [Google Scholar]
- 3.Kapan S, Bozkurt MA, Turhan AN et al. Management of acute appendicitis in pregnancy. Ulus Travma Acil Cerrahi Derg 2013, : 20–24. [DOI] [PubMed] [Google Scholar]
- 4.Theilen LH, Mellnick VM, Longman RE et al. Utility of magnetic resonance imaging for suspected appendicitis in pregnant women. Am J Obstet Gynecol 2015; : 345.e1–6. [DOI] [PubMed] [Google Scholar]
- 5.Hiersch L, Yogev Y, Ashwal E et al. The impact of pregnancy on the accuracy and delay in diagnosis of acute appendicitis. J Matern Fetal Neonatal Med 2014; : 1,357–1,360. [DOI] [PubMed] [Google Scholar]


