Abstract
INTRODUCTION
Pectus excavatum (PE) is the most common paediatric chest wall deformity. The majority of patients are treated for cosmetic purposes, with the modified Ravitch and Nuss procedures the most commonly performed. We tested the preferences of healthy individuals over their choice of procedure.
METHODS
The study was conducted from February to August 2014. A five-item illustrated questionnaire was administered to teenagers and young adults aged 14–26 years over their willingness to seek medical advice if they had PE, provided its cosmetic appearance was the only complaint. They were asked about their preference over the modified Ravitch and Nuss procedures, with the surgical details for both procedures explained by medical professionals, alongside illustrated outcomes.
RESULTS
Two hundred and two healthy individuals were interviewed. The median age was 19.5 years (14–26 years) and 141 (69.8%) were male. Sixty seven (33.2%) participants refused any intervention, while 11 (5.4%) initially wanted an intervention but refused after understanding the surgical procedures available. Of the 135 respondents who chose surgical correction, 84 (62.2%) preferred the modified Ravitch operation, while 51 (37.8%) preferred the Nuss procedure. The main reason for choosing the modified Ravitch technique was not having something metal in the chest, while most participants who chose the Nuss procedure felt that it was “cosmetically better”.
CONCLUSIONS
Patients have preferences over the choice of procedure for PE repair that can affect the treatment decision. Paediatric and thoracic surgeons should therefore be experienced in performing both procedures.
Keywords: Pectus, Choice behaviour, Thoracic wall
Pectus excavatum (PE) is the most common developmental chest wall abnormality, occurring in 8 of every 1000 live births. The defect is noticeable at birth in about 86% of patients with pectus deformity, whereas a later onset may be observed in patients with Marfan syndrome. The indications for repair of PE deformities are mainly cosmetic, although patients with severe deformities may develop symptoms.1–4
In 1949, Ravitch described a technique of PE repair requiring sub-perichondrial resection of all deformed costal cartilages, xiphoid excision and sternal osteotomy, with anterior fixation of the sternum.1 With minor modifications, this has remained the procedure of choice for nearly five decades. In 1998, a minimally invasive technique was introduced by Donald Nuss as an alternative to the traditional open Ravitch procedure.2 Avoidance of extensive dissection, cartilage resection and andosteotomy made the Nuss procedure an attractive surgical option for PE repair.
Clinically, the deformity does not cause significant physiological dysfunction in many patients with PE. The cosmetic disfigurement can, however, cause a serious loss of self-esteem and affect social behaviour.5
The majority of thoracic and paediatric surgeons today prefer one procedure over the other, based on their surgical expertise, cosmetic preference or beliefs in a better clinical outcome. Interestingly, no investigation has considered the patient's preference in choosing between the two procedures. The aim of this study was therefore to test whether healthy individuals would be keen to correct their deformity if they suffered from PE and, weighing the advantages and disadvantages of both the modified Ravitch technique (MRT) and Nuss procedures, what would be their preferred method of treatment.
Methods
A cross-sectional study was conducted over a 6-month period between February and August 2014, in which a non-probability quota sampling method was used targeting teenagers and young adults aged from 14 to 26 years.
A five-item interview questionnaire (Fig 1) was administered by medical professionals trained in thoracic surgery with a special interest in chest wall deformities. The term ‘pectus excavatum’ was defined as: a deformity in the growth of the central bone of the rib cage causing it to grow inwards, creating a sunken chest.
Figure 1.
The five-item questionnaire
Participants were shown a number of photographs to illustrate the deformity, with each sexes shown same-sex photos. An example of male deformity is shown in Figure 2.
Figure 2.

An example of a patient with moderate pectus excavatum
The questionnaire was divided into three main sections. The first was basic demographic data, including name, age, gender and regularity of sports playing. The second focused on the willingness of the participants to seek medical advice, if they had the pectus deformity, to correct it, provided that they had no other complaints other than its cosmetic appearance. The third section concerned the surgical method of preference over the MRT and the Nuss procedure, regardless their ability to pay for them, and the most likely reason for their choice.
The two operations were briefly explained to the participants as follows.
The modified Ravitch technique consists of an 8–12cm transverse incision, with removal of lower cartilages attached to the rib cage in a fashion that would allow their re-growth over the next few months, followed by reconstruction of the breast bone to straighten it out, with no metal bar insertion. The breast bone support is achieved through adherent non-biological material [a Gore-Tex patch; W. L. Gore & Associates, Newark, DE, USA] that is incorporated into human tissue over time, with no need for a second surgical procedure to remove it.
The Nuss procedure includes two cuts (approximately 2–4cm each) on each side of the chest, with insertion of a metal bar that runs behind the breastbone, causing it to be pushed forward. The metal bar is stabilized with two plates that lie on each side, under the skin wound. Another operation is then needed after approximately 2 years to remove the metal bar.
A detailed verbal and written explanation regarding postoperative complications was given to each volunteer, including pain, wound complications, chest wall flexibility, cardiac injury, bleeding and quality of life. We mentioned no significant differences in terms of hospital stay, postoperative pain or the incidence of recurrence between the two procedures. Illustrative examples of postoperative scars at different intervals, with different outcomes, were shown for each operation (see Figs 3 and 4).
Figure 3.

Postoperative scar following the Nuss procedure
Figure 4.

Postoperative scar following the modified Ravitch technique
Volunteers were given opportunities to ask questions about the procedures. Numerous texts and illustrations were available from the interviewing doctors. Volunteers were given the opportunity to delay their responses until they had carried out internet research or canvassed the opinion of their friends/parents.
Study participation was on a voluntary basis and the confidentiality of all obtained information was assured. Institutional research board (IRB) approval was obtained under ASU-IRB 14-175. Approval was obtained from the IRB for the questionnaire format as the best possible methodology.
Statistical analysis
Collected data was analysed and processed using SPSS Statistics version 20 (IBM, Armonk, NY, USA). General descriptive statistics, and Shapiro–Wilks, Fisher's exact and chi-squared tests were performed on all data. Statistical significance was considered if p<0.05.
Results
Data was assessed for normality assumption using the Shapiro-Wilks test, which indicated that our data was not normally distributed (p<0.05).
A total of 202 healthy individuals were interviewed. The median age of participants was 19.5 years (range 14–26 years), 141 (69.8%) were male, with mean age 19.6±2.42 years, while 61 (30.2%) were female, with mean age of 19.3±2.76 years.
Of the respondents, 135 (66.8%) said that they would undergo surgical correction of PE, while 67 (33.2%) refused. Eleven (5.4%) participants changed their decision to undergo PE treatment and refused either operation after explanation of the surgical technique for both procedures.
Choice of procedure
Of the 135 respondents who chose surgical correction of PR, 84 (62.2%) preferred the MRT, while 51 (37.8%) preferred the Nuss procedure. Of those who chose the MRT, 34 (75.6%) were female, while 40 (78.4%) of those who chose the Nuss procedure were male.
The most common reason for choosing the MRT was “the idea of having something metal, as in the Nuss operation” (n=55, 64.7%), followed by “the need for a second surgery after few years with the Nuss operation” (n=27, 31.8%). The least common reason was that the MRT is “cosmetically better” (n=3, 3.5%). The option "other" was not chosen by any volunteer.
The most common reason for choosing the Nuss procedure (n=51) was that it is “cosmetically better” (n=45, 88.2%), followed by it being “less invasive” (n=6, 11.8%). Again, the option "other" was not chosen by any volunteer.
One hundred and sixteen (57.4%) participants reported that they did not play sports regularly, while 86 (42.6%) did. There was no significant association between the regularity of sports playing and the type of surgery preferred (p=0.634).
There was a significant association between the gender of the participants and the type of surgery chosen, with 78.4% those who chose the Nuss operation being male and 21.6% females (p=0.024) (Fig 5). However, there was no significant association between the participants’ gender and the reason for choosing either the modified Ravitch or the Nuss operation, (p=0.148 and p=0.838 respectively).
Figure 5.
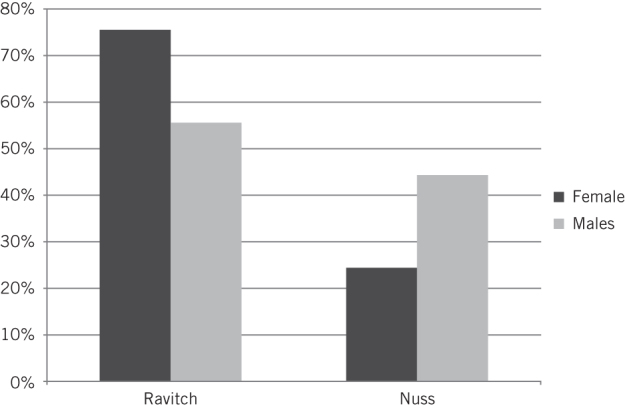
Relation between gender and surgical preferred
A binary logistic regression model assessing the effect of age, regularity of playing sports and gender on participants’ surgical preference was statistically significant (p<0.0005). The model explained 5.6%, on Nagelkerke R2 logistic regression analysis, of the variance in participants’ preference of the type of surgery, and correctly classified 62.2% of cases. Females were 2.52 times more likely to choose the modified Ravitch operation than males (p=0.027). Both increasing age and playing sports regularly had no effect on the choice of procedure (p>0.05).
Discussion
To the best of our knowledge, this is the first study to focus solely on the potential patient preference between the modified Ravitch and Nuss procedures in treating PE. The decision to have an operation for chest wall deformity may be negatively influenced by cultural backgrounds in some countries. As all our sample were Egyptian, and the indication for surgery was purely cosmetic, we expect that a larger percentage of patients would have been keen to have surgery in more Western societies, as their orientation towards body image as a deciding factor is likely to be stronger. Additionally, 5.4% of our sample was discouraged from proceeding with surgical correction after a thorough explanation of the surgical details.
Another significant factor is the influence of long-term perceived physical appearance, which the sample lacks. Surgeons often report that a patient’s decision to undergo surgical repair of a chest wall deformity (CWD) is strongly influenced by cosmetic concerns that are related to a perceived difference in physical appearance. These concerns may develop during adolescence, during which a patient’s body image might be influenced by peers who evaluate patients with CWD as being impaired in terms of physical appearance.5 Negative experiences in social relationships may occur and may contribute to a negative self-image, which is likely to persist and may affect quality of life, as well as psychological and emotional functioning. These associations have been shown to be present in other disfiguring conditions, such as burn injury and scleroderma.6,7 Our assumption that participants who play sports and have their chests exposed may be more willing to have their PE repaired was not supported by our study, as we found no relationship between playing sports and the willingness to have the deformity repaired or the choice of procedure.
Although the Nuss procedure has gained much in popularity since its introduction in 1998, a meta-analysis by Nasr et al suggested that there are no differences between the procedures with respect to overall complications, length of hospital stay and time to ambulation.8 Based on a descriptive review of many studies,8 it appears that a larger proportion of Nuss patients required epidural analgesia for a longer duration, but this did not translate into longer duration of hospitalisation. Consequently, both procedures remain acceptable.
When discussing postoperative outcomes, pain and the cosmetic result are extremely important when evaluating the procedures. Cosmoses remain the major indication for PE repair but one of the most poorly assessed parameters in the available literature. We found only three studies that used instruments to measure patient satisfaction. However, they used different instruments and it is impossible to combine the studies for a pooled estimate. Kelly et al,9 who performed the only prospective study, are planning to report their outcomes with regard to patient satisfaction in a future publication. Lam et al found an advantage with the Nuss procedure in terms satisfaction and less chest discomfort.10 Jo et al conducted an interview to measure the degree of postoperative satisfaction, classifying patients into four groups: excellent, good, fair, and poor.3. They found that 92.3% of patients in the Ravitch group and 93.3% in the Nuss group had good to excellent results, with no patients from either group classified as ‘poor’.
We wonder whether the individuals in our study would choose the same type of procedure if it would affect postoperative satisfaction. The assumption from Nuss-minded surgeons that two lateral scars nearly equivalent in length to a central transverse scar are better cosmetically for patients is more of a surgeon's hypothesis than a patient-related decision.
The senior author in our study proposed a Gore-Tex mesh to support the sternum in his MRT, which is supported by other studies.11,12 We believe, as others do, that this material offers solid support and resistance to infection, and can be left inside the patient. The main drawback is its higher cost. It is evident from our results that the idea of a metal bar left in situ and the need for a second operation with the Nuss procedure were the main drivers for our participants to choose the MRT. Most participants believe that the Nuss procedure is better cosmetically but the modification of not having to use a metal bar with the MRT was more motivating. We believe that surgeons using a retrosternal metal bar support, with the need for a second procedure, may have different results than ours if they perform a similar study, thus underlying the importance of counselling patients with different surgeon preferences.
In our study, we asked the reasons for our participants choosing their preferred method of treatment. We believe that this is better than speculating over reasons as did Antonoff and his colleagues.13 This is the only similar study to ours, in that it allowed patients with PE to choose between the modified Ravitch, Leonard and Nuss procedures. Similarly, they found that most patients chose to have the MRT, but the authors speculated was that it was the most popular procedure due to patient familiarity. We would disagree with this view. We examined internet-based literature from a spectrum of sources, ranging from informative sites maintained by physicians and hospitals and online encyclopaedias to blogs created by individual patients. Most of this material supports the Nuss procedure as the procedure of choice to treat PE. In contrast, 96.4% of our participants chose the modified Ravitch because they did not like the idea of having something metal in their body and the need to have a second operation. These are important patient-orientated concepts.
Our study included a participant male-to-female ratio of approximately 2:1. This is consistent with the male-to-female ratio for PE reported previously in the literature.2,3 Interestingly, there was a significant trend for a higher percentage of males choosing to have their PE repaired via the MRT. This may coincide with the low percentage of Nuss procedures performed in females in a number of studies. In a study by Fang and his colleagues,14 only 15 (12%) of 126 consecutive adult patients who had the Nuss procedure at their hospital were adult females, who had a mean age of 24 years. This is not in line with the typical male:female ratio for PE. Although this is not stated in their study, one may assume that this was partially caused by patient counselling and female refusal to have the procedure.
The limitations of our study include using healthy subjects rather than PE patients, and so perception of the disease could be inaccurate. We believe, however, that the type of repair an individual would choose would not be substantially influenced by having the disease. Another limitation is that, although the use of a Gore-Tex patch for sub-sternal support in the MRT by our author is supported by other studies, it is still not a routine practice.
It may be that, based on the current pattern of practice, a randomised controlled trial comparing the two surgical approaches is difficult to be performed. This is unfortunate, as the resistance to perform either procedure is based more on the bias of the treating surgeons rather than patient opinion or any conclusive data from the literature.
Conclusions
Patients can have different preferences as to the way they would like to have their PE repaired. In the context of the increasing popularity of the Nuss technique, it may be surprising that the majority of individuals would choose undergo the MRT. Paediatric and thoracic surgeons should therefore be experienced in performing both procedures, as the patient choice could alter the decision over the modality of treatment.
Acknowledgements
The authors declare no conflict of interest.
References
- 1.Ravitch MM. The Operative Treatment of Pectus Excavatum. Ann Surg 1949; : 429–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nuss D, Kelly RE, Croitoru DP et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998; : 545–552. [DOI] [PubMed] [Google Scholar]
- 3.Jo WM, Choi YH, Sohn YS et al. Surgical treatment for pectus excavatum. J Korean Med Sci 2003; : 360–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller KA, Woods RK, Sharp RJ et al. Minimally invasive repair of pectus excavatum: a single institution’s experience. Surgery 2001; : 652–7; discussion 657. [DOI] [PubMed] [Google Scholar]
- 5.Krille S, Müller A, Steinmann C et al. Self- and social perception of physical appearance in chest wall deformity. Body Image 2012; : 246–252. [DOI] [PubMed] [Google Scholar]
- 6.Benrud-Larson LM, Heinberg LJ, Boling C et al. Body image dissatisfaction among women with scleroderma: extent and relationship to psychosocial function. Health Psychol 2003; : 130–139. [PubMed] [Google Scholar]
- 7.Fauerbach JA, Heinberg LJ, Lawrence JW et al. Effect of early body image dissatisfaction on subsequent psychological and physical adjustment after disfiguring injury. Psychosom Med 2000; : 576–582. [DOI] [PubMed] [Google Scholar]
- 8.Nasr A, Fecteau A, Wales PW. Comparison of the Nuss and the Ravitch procedure for pectus excavatum repair: a meta-analysis. J Pediatr Surg 2010; : 880–886. [DOI] [PubMed] [Google Scholar]
- 9.Kelly RE, Cash TF, Shamberger RC et al. Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter study. Pediatrics 2008; : 1,218–1,222. [DOI] [PubMed] [Google Scholar]
- 10.Lam MW, Klassen AF, Montgomery CJ et al. Quality-of-life outcomes after surgical correction of pectus excavatum: a comparison of the Ravitch and Nuss procedures. J Pediatr Surg 2008; : 819–825. [DOI] [PubMed] [Google Scholar]
- 11.Kotoulas C, Papoutsis D, Tsolakis K et al. Surgical repair of pectus excavatum in young adults using the DualMesh 2-mm Gore-Tex. Interact Cardiovasc Thorac Surg 2003; : 565–568. [DOI] [PubMed] [Google Scholar]
- 12.Gorur R, Isitmangil T, Yildizhan A et al. Comparison of Retrosternal Metal Support and Absorbable Plaque in Correction of Pectus Deformities. J Ist Faculty Med 2008; : 73–77. [Google Scholar]
- 13.Antonoff MB, Erickson AE, Hess J et al. When patients choose: comparison of Nuss, Ravitch, and Leonard procedures for primary repair of pectus excavatum. J Pediatr Surg 2009; : 1,113–8; discussion 118. [DOI] [PubMed] [Google Scholar]
- 14.Fang FC, Cheng YL, Lee SC et al. Clinical experience of Nuss procedure for pectus excavatum in adult female patients. Thorac Cardiovasc Surg 2008; : 283–286. [DOI] [PubMed] [Google Scholar]


