Abstract
Background & objectives:
Cervical cancer is a major health problem and a leading cause of death among women in India. Of all the associated risk factors, high-risk human papillomavirus (HPV) infections being the principal aetiologic agent, two HPV vaccines are in use for the control of cervical cancer. The present study was undertaken to explore the knowledge, attitude and practice (KAP) on HPV vaccination among the healthcare providers in India.
Methods:
A cross-sectional study was conducted among 590 healthcare professionals from 232 hospitals and 80 PHCs of nine districts of Delhi-NCR (National Capital Region). A total of 590 (526 female, 64 male) healthcare providers were surveyed.
Results:
Only 47 per cent of respondents recommended young women to get vaccinated against HPV. Majority of respondents (81%) were found to be aware about the existence of vaccines for cervical cancer prevention. District-wise, highest (88.3%) awareness about the existence of vaccines against HPV was reported from Gautam Budh Nagar and lowest (64%) in Faridabad. Although 86 per cent of gynaecologists were aware about the names of HPV vaccines available in the market, only 27 per cent of paramedical staff had this knowledge. There was a significant difference between the respondents from government and private sectors regarding their awareness about HPV vaccines. Lack of awareness about the principal cause, risk factors and symptoms for cervical cancer and HPV vaccination was significantly (P< 0.05) reported in the respondents from paramedical staff category.
Interpretation & conclusions:
The findings reinforce continued medical education of healthcare providers, particularly those from the government sector on HPV vaccination for cervical cancer prevention. Public education is also pertinent for a successful HPV vaccination programme in the country.
Keywords: Cervical cancer, healthcare providers, hospitals and PHCs, human papilloma virus, KAP, vaccine
Worldwide about 15 per cent and nearly 26 per cent of cancer cases in developing countries are attributed to infectious agents, particularly viruses1. Cervical cancer, which is mainly caused by specific types of high-risk (HR) human papillomavirus (HPV) infection, is a leading cause of cancer-related deaths among women in India. HR HPV types 16 and 18 infections are considered responsible for about 75-80 per cent of cervical cancer worldwide2. In India, annually, about 1,32,000 new cancer cases and 80,000 deaths occur, and the prevalence of HPV type 16 was found to be exclusively very high3. Low-risk (LR) HPV types 6 and 11 cause almost all cases of genital warts4. Prevention of HPV would, therefore, reduce the incidence of cervical cancers as well as genital warts, along with the morbidity, mortality and costs associated with these diseases.
Two prophylactic vaccines, namely Gardasil® (MSD Merck & Co. Inc.,) and Cervarix® (GlaxoSmithKline Biologicals) approved by the USFDA (US Food and Drug Administration) are available for vaccination of adolescent girls. According to the study of Basu et al5, prophylactic HPV vaccination can reduce the burden of cervical cancer in India by more than 75 per cent.
Healthcare providers in hospitals and primary health centres (PHCs) including the paramedical staff constitute the most visible, front-line personnel providing health education to patients and the general population. Since paramedical staffs play an integral role in educating women in the prevention of diseases, they can influence cervical cancer screening adherence and health promotion among women. Wong et al6 in a study on Malaysian women reported that during screening most respondents revealed to have never been approached for cervical cancer and HPV screening during their visits to healthcare professionals. Many respondents also said that they would agree to be screened if this was recommended by their healthcare provider.
Several knowledge, attitude and practice (KAP) studies have been reported from other countries such as Mexico, Thailand and Pakistan. Songthap et al7 reported a cross-sectional survey-based study to evaluate acceptability, knowledge and attitude regarding HPV and HPV vaccine among healthcare providers working in hospitals located in Bangkok, Thailand. Marlow et al8 compared the knowledge about HPV and HPV vaccination among the participants from the US, the UK and Australia.
As documented through various formative research and other studies, accurate, in-depth knowledge about HPV vaccination tends to be low in developing countries in comparison to developed countries, worldwide6,7,8. Therefore, the present study was designed to find out KAP of healthcare providers on HPV and HPV vaccination in the low-resource setting of our country.
Material & Methods
This cross-sectional study was based on a 1-year survey conducted in hospitals and PHCs of the State of Delhi and National Capital Region (NCR), comprising Faridabad, Gurgaon, Ghaziabad and Gautam Budh Nagar for assessing the awareness, attitude and practice of healthcare providers for HPV vaccination between August 2012 and April 2013. Data generated through questionnaire from healthcare providers were from public hospitals (48), private hospitals (184) and PHCs (80).
Statistical sampling of PHCs and hospitals was done, using the formula applicable for survey research with normal approximation to hyper geometric. Sampling was done using the following formula: n=Nz^2pq/(E^2(N − 1) + z^2pq).
n=sample size of PHCs/hospitals to be surveyed, N=total no. of PHCs/hospitals on sample frame, z=confidence level (1.96 at confidence interval of 95%) = 1.96E (± error) = Standard error or sampling error [i.e., coefficient of variance or relative error × population estimate (p)] = 0.06 × 0.8 = 0.048 (standard margin of error for surveys ranges from 5 to 10% and maximum at 20%), p is the anticipated proportion of facilities with the attribute of interest (80% = 0.8), q = 1 − p…. (1 − 0.8 = 0.2).
It was anticipated that each of the key estimates of the survey of small number of facilities will be in the range of about 50-100 per cent. In that case, the largest sample size needed was when the percentage with the given attribute was 80, and this was the sample size to be used. Thus, p=0.8. For precision requirements, relative error (coefficient of variation) of 6 per cent was taken. The sample size thus calculated at 95 per cent level of confidence using the above formula was 71 PHCs and 232 hospitals.
The overall percentage of government hospitals was less (12.8%; 48 government hospitals) in comparison to private hospitals (i.e., 87.2%; 327 private hospitals) and unevenly distributed over different geographic areas of the State of Delhi and NCR. All government hospitals were included from each stratum and the remaining were the private hospitals, matching with the number of hospitals from each stratum.
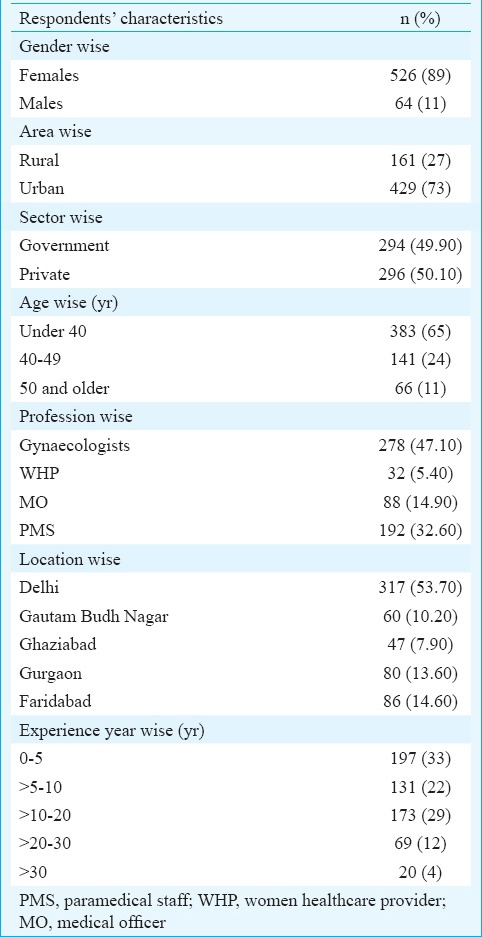
Sampling of service providers (women healthcare professionals, gynaecologists and oncologists) at hospitals and (medical officers and paramedical staff) at PHCs: The survey was conducted in five districts/regions of Delhi-NCR covering 232 hospitals and 80 PHCs. A total of 590 respondents participated in the survey who were from different socio-professional stratum (Table I). As per the Indian Public Health Standards9, the total number of medical officers (MOs) and paramedical staff ranges from 2 to 5 in PHCs. As this is a small sample, all service providers present at the time of survey were interviewed. Besides Delhi, the regions/districts covered under NCR comprised Faridabad, Gurgaon, Ghaziabad and Gautam Budh Nagar.
Table I.
Sociodemographic profile of healthcare providers included in the survey (n=590)
Research tool: A self-administered validated questionnaire was used to assess the KAP for HPV and HPV vaccination of service providers working in different hospitals and PHCs. As questions were designed for assessing the overall knowledge of different healthcare providers at hospitals and PHCs, some of them were not attempted by those who did not know the answer. The healthcare providers comprised oncologists, gynaecologists, MOs and also the paramedical staff. All the data were entered and cross-checked thrice to avoid any error during the data entry. The data were analyzed using SPSS version 17.0 (SPSS Inc. Chicago, IL, USA).
The study protocol was approved by the Research Ethics Committee of World Healthal Trust. All the participants of the survey were explained about this study and prior approval was taken from all the competent medical authorities of each district.
Results
Cervical cancer is a major cancer among Indian women (Q: 1-Do you agree that cervical cancer tops among Indian women?): The awareness of 590 healthcare providers was assessed for their knowledge about HPV and HPV vaccination. Of the total respondents, 84 per cent agreed that cervical cancer was the most commonly occurring cancer among all the gynaecological cancers in Indian women (Table II). A significant difference (P<0.05) was observed in the awareness levels of gynaecologists (91.3%) and paramedical staff (72.4%) on the fact that cervical cancer tops all cancers that affect Indian women (Table II). There was, however, no significant difference between the respondents from rural (76.4%) and urban (85.3%) areas, and also between the respondents from government (81.2%) and private (88.9%) sectors on their awareness about cervical cancer being the most common cancer affecting Indian women (Table II).
Table II.
Knowledge and practice on human papillomavirus vaccination among healthcare providers from different socio-professional profiles
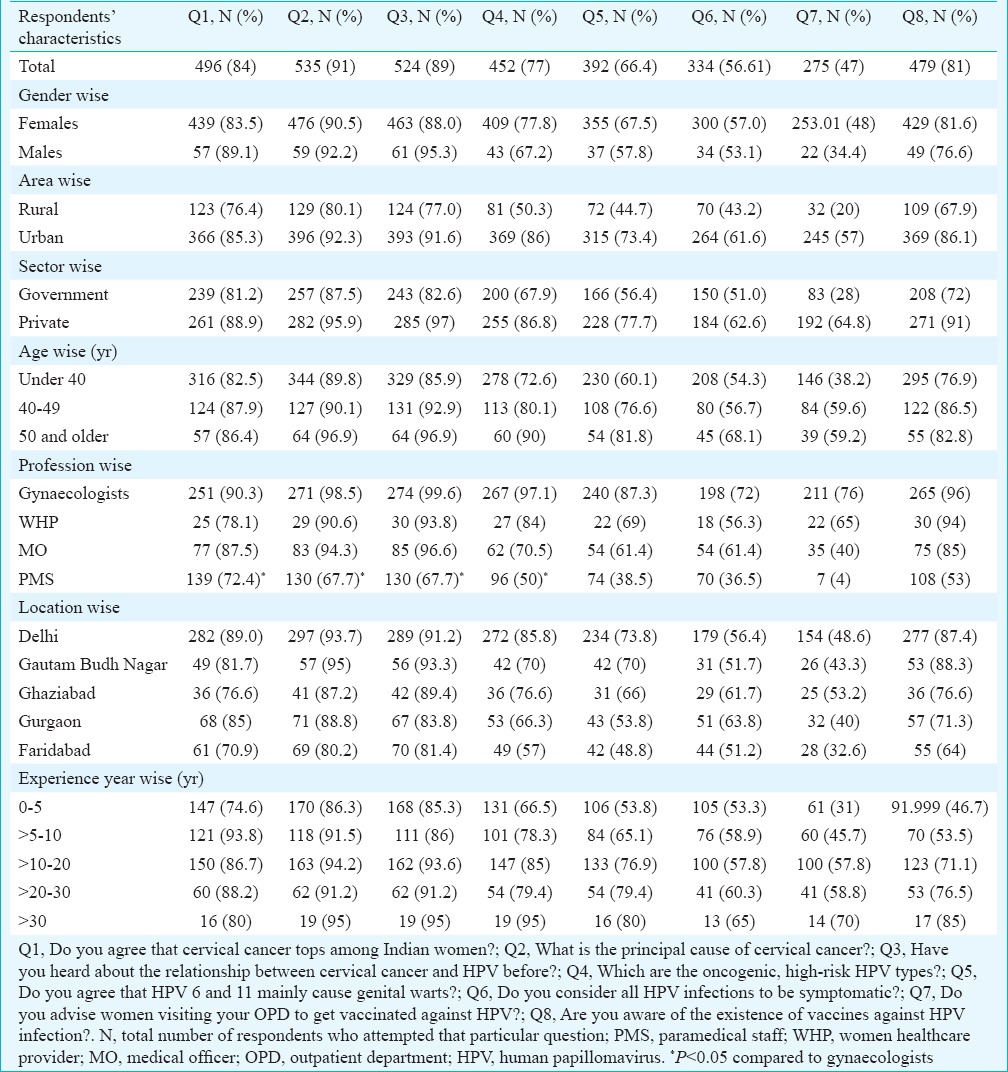
Principal cause of cervical cancer (Q: 2-What is the principal cause of cervical cancer?): As shown in Table II, 91 per cent of the respondents were aware about the fact that HPV was the principal cause of cervical cancer. Among both the genders, knowledge for HPV as principal cause was found to be similar. While 80 per cent of the respondents from rural area were found to be aware of this fact, 92.3 per cent of urban respondents had this knowledge. Age and experience of years were associated, but profession was found to be significantly associated as 98.5 per cent of the gynaecologists were found to be aware in comparison with 67.7 per cent of paramedical staff (P<0.05). Among all the five locations, Faridabad was reported with minimum knowledge about it (Table II).
Relationship between HPV and cervical cancer (Q: 3-Have you heard about the relationship between cervical cancer and HPV before?): Respondents from rural areas were found to have low knowledge (77%) in comparison with respondents from urban areas (91.6%) about the relationship between cervical cancer and HPV. A similar pattern was observed between the respondents from government health centres and those from the private sectors. A significant difference in awareness levels was observed between gynaecologists (99.6%) and paramedical staff (67.7%) (P<0.05) (Table II).
Knowledge about the HR and LR HPV types (Q: 4-Which are the oncogenic, high-risk HPV types? Q: 5-Do you agree that HPV 6 & 11 mainly cause genital warts?): Seventy seven per cent of the respondents knew about the oncogenic or HR HPV types whereas 23 per cent of the respondents did not know anything about the existence of oncogenic HPV types (Table II). Sixty six per cent of the respondents were aware of this fact that HPV types 6 and 11 mainly cause genital warts. Delhi was on top with high level of awareness about the oncogenic HPV types (85.8%). On the other hand, only 57 per cent of respondents from Faridabad were found to be aware about the oncogenic HPV types. Knowledge about both HR and LR HPV types was found maximum in the respondents having maximum years of experience. Among all the categories of healthcare providers included in this survey, gynaecologists (87.3%) showed the highest awareness about the HPV types that cause genital warts, while only 38.5 per cent of the paramedical staff was aware about the LR HPV responsible for genital warts. Similarly, awareness about the HPV types 6 and 11 was low among women healthcare professionals (69%) and MOs (61.4%) (Table II).
Symptoms of HPV infection (Q: 6- Do you consider all HPV infections to be symptomatic?): There was awareness on several issues/facts such as oncogenic HPV types; HPV types 6 and 11 causing genital warts; all associated risk factors and major symptoms related to cervical cancer were found to be in increasing order as the number of years of respondents’ experience increases (Table II).
Practice for recommending HPV vaccination (Q: 7- Do you advise women visiting your outpatient department to get vaccinated against HPV?): From results shown in Table II, only 47 per cent of the respondents recommended young women to get vaccinated against HPV. The remaining 53 per cent of the respondents either did not recommend HPV vaccination or did not know anything about it and, therefore, were not contributing to cervical cancer prevention through HPV vaccination. Although 76 per cent of gynaecologists were recommending younger women to get vaccinated against HPV, only four per cent of the paramedical staff were doing so. Only 20 per cent respondents from rural area were reported to have recommended the HPV vaccine. Although 53.2 per cent of the respondents from Ghaziabad recommended that all women should get vaccinated against HPV, only about 32.6 per cent of the respondents from Faridabad were found to recommend HPV vaccination. It was also found that as the respondents’ number of years of experience increased, a progressive increase in their number was observed who advised young women for HPV vaccination. An insignificant difference was observed in the percentage of male and female respondents who advised HPV vaccination.
Awareness about the existence of HPV vaccines (Q: 8- Are you aware of the existence of vaccines against HPV infection?): Of the 590 respondents, 81 per cent were found to be aware about the existence of vaccines for the prevention of cervical cancer (Table II). Although 96 per cent of the gynaecologists were aware of the existence of the HPV vaccines, only 53 per cent of the paramedical staff had this awareness. It was also observed that, from the government and private sectors, 72 and 91 per cent of the respondents, respectively, were aware of the existence of HPV vaccines. It was also observed that, from the urban and rural areas, 86 and 68 per cent of the respondents, respectively, were aware of the existence of HPV vaccines. Among all the five locations, the highest awareness (88.3%) of respondents towards the existence of vaccines against HPV was observed from Gautam Budh Nagar and lowest awareness (64%) was reported from Faridabad. A maximum of 85 per cent of the respondents were found to be aware about the existence of HPV vaccines from the group of more than 30 years of experience. Female respondents were observed to be more aware than male respondents about the existence of HPV vaccines.
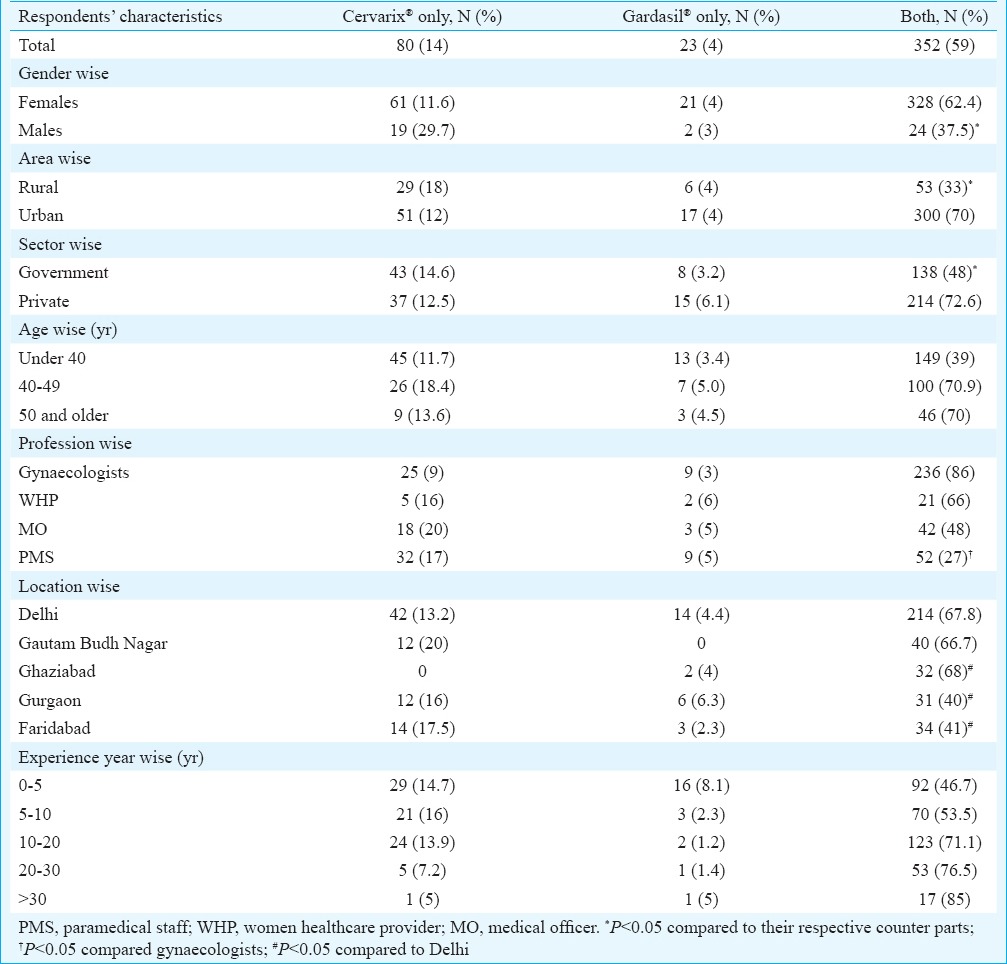
Awareness about the name of available vaccines in market: As shown in Table III, 59 per cent of respondents were aware about the names of both the HPV vaccines available in the market. Moreover, 14 per cent of the respondents knew about the availability of Cervarix®, and only four per cent of the respondents knew about Gardasil®. Although 86 per cent of gynaecologists were aware about the names of HPV vaccines available in the market, only 27 per cent of the respondents from the paramedical staff category had this awareness. There was a significant difference (P<0.05) reported between the respondents from government and private sectors (48 vs. 72.6%, respectively), regarding their awareness about HPV vaccines available in the market. There was a significant difference (P<0.05) reported between the respondents from urban and rural areas i.e., 70 and 33 per cent, respectively, regarding their awareness about HPV vaccines available in the market. It was found that as the number of years of experience increased, the percentage of awareness for the existence of HPV vaccines available in the market also increased progressively. There was a significant difference (P<0.05) for the awareness of HPV vaccines available in the market between male (37.5%) and female (62.4%) respondents.
Table III.
Relation between socio-professional profile of healthcare providers and their knowledge about available human papillomavirus vaccines
Discussion
Adequate knowledge and positive attitude about HPV vaccination are essential prerequisites for healthcare professionals to provide patient education about HPV. Increasing uptake of HPV vaccines should be a priority in developing countries since they contribute to 88 per cent of global cervical cancer burden10. Opinion of healthcare providers, having different professional profiles and training, about patient education on HPV infection and the current scenario of existing facilities for the detection and treatment of cervical cancer in hospitals and primary health centres (PHCs) of Delhi-NCR has been reported11,12.
In this study, a majority of healthcare providers (84-90%) were found to be aware about cervical cancer and HPV. Among all the five districts that were surveyed, maximum awareness among healthcare providers related to cervical cancer, was observed among the respondents from Delhi whereas only 70 per cent respondents from Faridabad had adequate knowledge related to cervical cancer. The number of years of experience of respondents played an important role in their understanding about various aspects of cervical cancer. For example, the most predominant aetiological factor for cervical cancer is persistent infection of certain HR-HPVs, while LR types are associated with benign cervical lesions and genital warts. In India, the most common (98%) oncogenic types are HPV types 16 and 18 with HPV 16 (80-90%) prevalent exclusively13,14. The present investigation revealed that 77 per cent of the respondents knew about the oncogenic or HR HPV types. Lack of awareness about the principal cause, risk factors and symptoms for cervical cancer and HPV vaccination was reported from the respondents from paramedical staff category.
A significant difference in awareness level about the existence of HR-oncogenic HPV types was, however, observed among healthcare providers of different professional profiles. Among all the categories of healthcare providers included in this survey, gynaecologists showed the highest awareness about the HPV types that cause genital warts. It was observed that awareness related to HPV types was low among the respondents from rural sector and lower than expected among respondents from government sector. This finding warrants the need for providing periodic educational interventions for all healthcare professionals, particularly paramedical staff, working in PHCs and government health centres in rural areas.
Similar to our study, Dabash et al15 reported that many healthcare providers knew about the link between cervical cancer and HPV, yet gaps in understanding the natural history of cervical cancer, its preventable nature, treatment of precancerous lesions and knowledge of stage-appropriate clinical management of cancer were present. Raychaudhuri and Mandal16 highlighted the comparative status of awareness on cervical cancer between slum dwellers of urban and rural North Bengal. Similarly, a study conducted among the female educated youth from India, Nepal and Srilanka had concluded that the awareness of cervical cancer was 66 per cent in India, 58.8 per cent in Nepal and 57.7 per cent in Srilanka17. In a study carried out in Kolkata, 41 per cent of college students included in the survey were aware of the link between sexual activity and cervical cancer18. A review study by Perlman et al19 on awareness and knowledge of HPV vaccination reported the urgent need for public education about HPV and HPV vaccines.
HPV is largely asymptomatic, making it difficult to recognize and detect this infection among the general population, which limits any behavioural modification. Although both Cervarix® and Gardasil® provide immunity against HPV types 16 and 18, the latter additionally protects against HPV types 6 and 11. Both vaccines need to be administered with three doses over a 6-month period.
To develop an effective HPV vaccination programme, it is crucial to understand the healthcare providers’ knowledge of HPV and their attitude towards HPV vaccination. Our findings showed that only 47 per cent of the respondents recommended young ladies to get vaccinated against HPV. As more than half of the total respondents did not recommend HPV vaccination or did not know anything about it, they were not contributing to cervical cancer prevention through HPV vaccination. It was also found that as the respondents’ number of years of experience increased, a progressive increase in their number was observed who advised for HPV vaccination. It is reported that 89 per cent of paediatricians in the US recommend HPV vaccines for girls aged 16-18 yr, while only 46 per cent recommend vaccines for younger girls20.
In a study by Pandey and Chandravati21 from Lucknow, cervical cancer awareness and knowledge of Gardasil® vaccination were evaluated among north Indian women and 28.1 per cent awareness was reported for this HPV vaccine. Another cross-sectional study among the medical students of a tertiary care hospital in Delhi reported that 18 per cent of them did not know that HPV vaccination prevented cervical cancer and 50 per cent thought that vaccination induced false sense of security22. A study by Pandey et al23 to evaluate awareness regarding the availability of vaccine against cervical cancer among 618 undergraduate medical students, by explorative questionnaire-based survey reported that 75.6 per cent were aware of it. Female students had better awareness regarding the availability of vaccine, target population for vaccination and about the catch-up programme. Our study also revealed better awareness about the existence of HPV vaccine among female respondents. Shekhar et al24 conducted a cross-sectional study among the nursing staff in a tertiary-level teaching institution of rural India and found that only 25 per cent of the participants had heard of vaccines to prevent cervical cancer.
According to a study conducted in China, healthcare providers scored well on the HPV Vaccine knowledge scale. The majority of urban providers scored 7 out of 8 points, and the majority of rural providers scored 6 out of 8 points. Nearly 68 and 58 per cent of urban and rural providers, respectively, had heard of the HPV vaccine25. In our study, 59 per cent of respondents were aware about the names of both the HPV vaccines available in the market. Only 27 per cent of the respondents from the paramedical staff category had this awareness. There was a significant difference reported between the respondents from government and private sectors regarding their awareness about HPV vaccines available in the market. This finding reinforces the importance of public education for a successful HPV vaccination programme in the country. In India where the burden of this disease is high, patient education for primary screening and HPV vaccination is pertinent which could be only possible if healthcare providers are well informed themselves about the various aspects of cervical cancer prevention and management.
In conclusion, to alleviate the burden of cervical cancer, a coordinated government action is necessary to make the health system delivery efficient. Adequate support to voluntary organizations/non-governmental organizations working in health sector for increasing awareness on cervical cancer among both healthcare providers and the general public could further help in reducing the burden of this disease. Public health education on the safety and efficacy of HPV vaccination is much needed.
Acknowledgment
The research survey was conducted with research grant received from the Indian Council of Medical Research, Ministry of Health and Family Welfare, Government of India. Dr Richa Shrivastava's contribution towards data analysis and report preparation is acknowledged. Authors thank Shri Paramdeep Singh, Ms Neha Sethi, Dr Roli Shrivastava, Shri Dharmendra Pratap Singh, Ms Anju Shrivastava and Miss Apeksha Yadav for their support during the survey.
Footnotes
Conflicts of Interest: None.
References
- 1.Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118:3030–44. doi: 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- 2.Clifford G, Francheschi S, Diaz M, Munoz N, Villa LL. HPV type-distribution in women with and without cervical neoplastic diseases. Vaccine. 2006;24(Suppl 3):26–34. doi: 10.1016/j.vaccine.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 3.Das BC, Sharma JK, Gopalakrishna V, Luthra UK. Analysis by polymerase chain reaction of the physical state of human papillomavirus type 16 DNA in cervical preneoplastic and neoplastic lesions. J Gen Virol. 1992;73:2327–36. doi: 10.1099/0022-1317-73-9-2327. [DOI] [PubMed] [Google Scholar]
- 4.Lacey CJ, Lowndes CM, Shah KV. Burden and management of non-cancerous HPV-related conditions: HPV-6/11 disease. Vaccine. 2006;24(Suppl 3):35–41. doi: 10.1016/j.vaccine.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Basu P, Roychowdhury S, Bafna UD, Chaudhury S, Kothari S, Sekhon R, et al. Human papillomavirus genotype distribution in cervical cancer in India: results from a multi-center study. Asian Pac J Cancer Prev. 2009;10:27–34. [PubMed] [Google Scholar]
- 6.Wong LP, Wong YL, Low WY, Khoo EM, Shuib R. Knowledge and awareness of cervical cancer and screening among Malaysian women who have never had a Pap smear: a qualitative study. Singapore Med J. 2009;50:49–53. [PubMed] [Google Scholar]
- 7.Songthap A, Pitisuttithum P, Kaewkungwal J, Fungladda W, Bussaratid V, Koonsaeng S. Knowledge, attitudes, and acceptability of a human papillomavirus vaccine among healthcare providers. Southeast Asian J Trop Med Public Health. 2009;40:1048–56. [PubMed] [Google Scholar]
- 8.Marlow LA, Zimet GD, McCaffery KJ, Ostini R, Waller J. Knowledge of human papillomavirus (HPV) and HPV vaccination: an international comparison. Vaccine. 2013;31:763–9. doi: 10.1016/j.vaccine.2012.11.083. [DOI] [PubMed] [Google Scholar]
- 9.Indian Public Health Standards (IPHS). Guidelines for Primary Health Centers. Directorate General of Health Services. New Delhi: Ministry of Health & Family Welfare, Government of India; 2012. [Google Scholar]
- 10.Madhivanan P, Srinivas V, Marlow L, Mukherjee S, Narayanappa D, Mysore S, et al. Indian parents prefer vaccinating their daughters against HPV at older ages. Asian Pac J Cancer Prev. 2014;15:107–10. doi: 10.7314/apjcp.2014.15.1.107. [DOI] [PubMed] [Google Scholar]
- 11.Chawla PC. Role of healthcare providers in patient education on HPV infection and cervical cancer prevention – A crosssectional study in public & private health centers of Delhi-NCR, India. Int J Latest Res Sci Technol. 2014;3:140–6. [Google Scholar]
- 12.Chawla PC, Chawla AK, Shrivastava R, Shrivastava A, Chaudhary S. Situation analysis of existing facilities for screening, treatment and prevention of cervical cancer in hospitals/primary health centers of Delhi-NCR region, India. Asian Pac J Cancer Prev. 2014;15:5475–82. doi: 10.7314/apjcp.2014.15.13.5475. [DOI] [PubMed] [Google Scholar]
- 13.Bharadwaj M, Hussain S, Nasare V, Das BC. HPV & HPV vaccination: issues in developing countries. Indian J Med Res. 2009;130:327–33. [PubMed] [Google Scholar]
- 14.Bhatla N, Joseph E. Cervical cancer prevention & the role of human papillomavirus vaccines in India. Indian J Med Res. 2009;130:334–40. [PubMed] [Google Scholar]
- 15.Dabash R, Vajpayee J, Jacob M, Dzuba I, Lal N, Bradley J, et al. A strategic assessment of cervical cancer prevention and treatment services in 3 districts of Uttar Pradesh, India. Reprod Health. 2005;2:11–6. doi: 10.1186/1742-4755-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raychaudhuri S, Mandal S. Socio-demographic and behavioural risk factors for cervical cancer and knowledge, attitude and practice in rural and urban areas of North Bengal, India. Asian Pac J Cancer Prev. 2012;13:1093–6. doi: 10.7314/apjcp.2012.13.4.1093. [DOI] [PubMed] [Google Scholar]
- 17.Joy T, Sathian B, Bhattarai C, Chacko J. Awareness of cervix cancer risk factors in educated youth: a cross-sectional, questionnaire based survey in India, Nepal, and Sri Lanka. Asian Pac J Cancer Prev. 2011;12:1707–12. [PubMed] [Google Scholar]
- 18.Saha A, Chaudhury AN, Bhowmik P, Chatterjee R. Awareness of cervical cancer among female students of premier colleges in Kolkata, India. Asian Pac J Cancer Prev. 2010;11:1085–90. [PubMed] [Google Scholar]
- 19.Perlman S, Wamai RG, Bain PA, Welty T, Welty E, Ogembo JG. Knowledge and awareness of HPV vaccine and acceptability to vaccinate in Sub-Saharan Africa: a systematic review. PLoS One. 2014;9:e90912. doi: 10.1371/journal.pone.0090912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daley MF, Liddon N, Crane LA, Beaty BL, Barrow J, Babbel C, et al. A national survey of pediatrician knowledge and attitudes regarding human papillomavirus vaccination. Pediatrics. 2006;118:2280–9. doi: 10.1542/peds.2006-1946. [DOI] [PubMed] [Google Scholar]
- 21.Pandey S, Chandravati Human papillomavirus-mediated cervical cancer awareness and Gardasil vaccination: a pilot survey among North Indian women. J Community Health. 2013;38:907–10. doi: 10.1007/s10900-013-9697-6. [DOI] [PubMed] [Google Scholar]
- 22.Mehta S, Rajaram S, Goel G, Goel N. Awareness about human papilloma virus and its vaccine among medical students. Indian J Community Med. 2013;38:92–4. doi: 10.4103/0970-0218.112438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pandey D, Vanya V, Bhagat S, Vs B, Shetty J. Awareness and attitude towards human papillomavirus (HPV) vaccine among medical students in a premier medical school in India. PLoS One. 2012;7:e40619. doi: 10.1371/journal.pone.0040619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shekhar S, Sharma C, Thakur S, Raina N. Cervical cancer screening: knowledge, attitude and practices among nursing staff in a tertiary level teaching institution of rural India. Asian Pac J Cancer Prev. 2013;14:3641–5. doi: 10.7314/apjcp.2013.14.6.3641. [DOI] [PubMed] [Google Scholar]
- 25.Zhao CQ, Yang HT, Xue DB, Yang M. High-risk human papillomavirus DNA testing and histologic follow up in women with abnormal cytology. Zhonghua Bing Li Xue Za Zhi. 2012;41:774–8. doi: 10.3760/cma.j.issn.0529-5807.2012.11.017. [DOI] [PubMed] [Google Scholar]


