Abstract
Few studies have examined the prevalence of hypertension among Asians living in the United States. Multiyear data from the Los Angeles County Health Survey were used to investigate the prevalence of hypertension among Asians and Asian subgroups, and risk factors associated with the disease, using descriptive analysis and multivariate logistic regression. Age-adjusted prevalence of hypertension in Asians was 23.4%. Among Asian subgroups, age-adjusted prevalence of hypertension was lowest among Chinese (20.0%), and highest among Filipinos (32.7%), and several factors were identified as associated with hypertension. Hypertension among Asian-Americans is a serious public health concern, requiring culturally sensitive best practices, and evidence-based approaches to improve prevention and control among Asians.
Keywords: Hypertension, Adult, Asian Americans, Risk factors, Evidence-based medicine
Highlights
-
•
The prevalence of hypertension among Asians was 23.4% in Los Angeles County.
-
•
The prevalence of hypertension varied among Asian subgroups.
-
•
Several risk factors were identified as associated with hypertension among Asians.
-
•
Evidence based intervention should consider culturally sensitive approaches.
1. Background/objective
Asians have emerged as the fastest growing major ethnic minority population in the United States, currently comprising 5.6% of the U.S. population and 36% of immigrants (United States. Dept. of Commerce. U.S. Census Bureau, 2012, 2010 American Community Survey and other Census Bureau data;). However, few studies have examined the prevalence of hypertension among Asians living in the United States.
The primary objective of this study was to investigate the prevalence of hypertension among adult (18 years or older) Asians and Asian ethnic subgroups in Los Angeles County (LAC), which has the largest county population of Asians in the U.S. In 2014, Asians comprised approximately 15% of the LAC population (about 1,500,000) (Population Estimates, n.d.). A secondary objective of this study was to investigate risk factors associated with hypertension among Asians.
2. Methods
We aggregated data from the four most recent cycles of the Los Angeles County Health Survey (2005, 2007, 2011, and 2015), a periodic, random-digit-dial telephone survey of the non-institutionalized population of Los Angeles County. Methodologic changes were made to the survey beginning in 2011. In the 2011 and 2015 surveys, the Los Angeles County Health Survey (LACHS) incorporated cell phone users and adopted a more sophisticated raking procedure in weighting the survey data. These changes were made to maintain survey representativeness and validity and are similar to those made to the Behavioral Risk Factor Surveillance System in 2011 (Pierannunzi et al., 2012). Additional details regarding the survey design, content, and weighting methodology are reported elsewhere (Simon et al., 2001, Yi et al., 2015). Interviews were conducted in English, Spanish, Mandarin, Cantonese, Korean, and Vietnamese, with one adult randomly selected from each household. Asians comprised 3191 individuals in the sample. The comparison groups included Latinos (n = 11,420), whites (n = 13,442), and blacks (n = 3188). The remaining survey sample consisted of 585 adults who identified as Pacific Islander, American Indian/Alaska Native, and Other. These were excluded from the study due to inadequate sample sizes. The final study sample included 31,241 adults.
Hypertension was defined by a positive response to the question “Have you ever been told by a doctor or other health professional that you have high blood pressure or hypertension?” Similar definitions of self-reported doctor-diagnosed hypertension have been used in other studies (Tormo et al., 2000, Ikeda et al., 2014).
We conducted descriptive analysis to quantify the prevalence of hypertension and other factors that had previously been demonstrated to be associated with hypertension. Furthermore, we performed multivariate logistic regression among Asian respondents to examine the associations between hypertension and demographic characteristics (age and gender), socio-economic status (education and federal poverty level), acculturation proxies (nativity, number of years living in the US, and language used most at home), body mass index (BMI), and health behaviors (physical activity, smoking and drinking). All analyses were conducted using Statistical Analysis System version 9.3 (SAS Institute Inc., Cary, NC).
3. Results
3.1. Demographic characteristics of the Asian sample
The characteristics of the study sample (unweighted): among the adult Asians (3191) 53.8% were female. The median age was 49.0 years. 14.5% were 18–29 years old, 37.7% were 30–49 years old, 26.7% were 50–64 years old, and 21.2% were 65 years or older. 35.2% were Chinese, 14.6% were Korean, 17.1% were Filipino, 10.3% were Japanese, 6.8% were Vietnamese, 7.5% were South Asian and 8.4% were Other Asian.
The characteristics of the weighted study population of Asian subgroups are detailed in Table 1.
Table 1.
Characteristics of the Study Population of Asian Subgroupsa.
| Characteristic | Chinese | Korean | Filipino | Japanese | Vietnamese | South Asian | Other Asian |
|---|---|---|---|---|---|---|---|
| (n = 1122) | (n = 547) | (n = 466) | (n = 330) | (n = 217) | (n = 240) | (n = 269) | |
| weighted % (95% ci) | weighted % (95% ci) | weighted % (95% ci) | weighted % (95% ci) | weighted % (95% ci) | weighted % (95% ci) | weighted % (95% ci) | |
| Age (yrs) | |||||||
| 18–29 | 23.9 (20.6, 27.3) | 19.4 (14.4, 24.4) | 29.1 (22.9, 35.2) | 17.4 (10.8, 24.1) | 18.6 (11.0, 26.1) | 30.6 (22.6, 38.7) | 22.8 (15.8, 29.9) |
| 30–49 | 38.3 (34.8, 41.8) | 40.9 (35.8, 46.0) | 40.7 (35.0, 46.4) | 29.3 (23.3, 35.2) | 45.2 (36.8, 53.5) | 49.1 (41.0, 57.1) | 41.8 (34.5, 49.2) |
| 50–64 | 22.3 (19.4, 25.2) | 20.9 (17.0, 24.8) | 20.4 (16.4, 24.4) | 30.3 (24.5, 36.0) | 25.7 (18.6, 32.7) | 12.4 (8.2, 16.6) | 24.1 (17.7, 30.5) |
| 65 + | 15.4 (13.2, 17.7) | 18.9 (15.4, 22.4) | 9.8 (7.1, 12.6) | 23.1 (18.2, 27.9) | 10.6 (6.6, 14.7) | 7.9b (4.2, 11.6) | 11.3 (7.3, 15.3) |
| Gender | |||||||
| Female | 50.5 (46.9, 54.2) | 45.8 (40.5, 51.0) | 44.7 (38.8, 50.6) | 45.3 (38.7, 52.0) | 50.1 (41.8, 58.5) | 66.1 (58.4, 73.8) | 48.7 (41.2, 56.3) |
| Male | 49.5 (45.8, 53.1) | 54.2 (49.0, 59.5) | 55.3 (49.4, 61.2) | 54.7 (48.0, 61.3) | 49.9 (41.5, 58.2) | 33.9 (26.2, 41.6) | 51.3 (43.7, 58.8) |
| Hypertension | |||||||
| Yes | 19.6 (16.9, 22.3) | 22.5 (18.2, 26.7) | 28.5 (23.4, 33.6) | 29.2 (23.7, 34.7) | 22.2 (15.5, 28.8) | 15.5 (9.9, 21.1) | 23.1 (17.1, 29.1) |
| No | 80.4 (77.7, 83.1) | 77.5 (73.3, 81.8) | 71.5 (66.4, 76.6) | 70.8 (65.3, 76.3) | 77.8 (71.2, 84.5) | 84.5 (78.9, 90.1) | 76.9 (70.9, 82.9) |
| Education | |||||||
| < HS | 14.4 (11.8, 16.9) | 11.2 (7.9, 14.5) | 3.0b (0.2, 5.8) | 1.0b (0.0, 1.9) | 30.5 (23.0, 38.1) | 0.7b (0.0, 1.6) | 7.8b (3.1, 12.5) |
| HS/some college | 39.0 (35.3, 42.7) | 39.4 (34.0, 44.8) | 45.2 (39.2, 51.2) | 43.4 (36.6, 50.1) | 42.4 (34.2, 50.6) | 35.2 (26.8, 43.6) | 41.3 (33.5, 49.2) |
| College or post graduate degree | 46.6 (43.0, 50.2) | 49.4 (44.1, 54.7) | 51.8 (45.8, 57.8) | 55.7 (48.9, 62.4) | 27.1 (18.9, 35.2) | 64.2 (55.8, 72.5) | 50.9 (43.1, 58.6) |
| Household income | |||||||
| 0–99% FPL | 20.3 (17.3, 23.3) | 15.7 (12.3, 19.1) | 17.1 (12.0, 22.1) | 2.9b (0.9, 4.8) | 21.3 (15.2, 27.3) | 9.3b (4.8, 13.8) | 11.1b (6.0, 16.3) |
| 100–199% FPL | 24.6 (21.5, 27.7) | 30.5 (25.7, 35.4) | 18.5 (13.9, 23.2) | 13.7 (8.3, 19.0) | 27.0 (19.7, 34.4) | 17.3 (10.9, 23.6) | 23.5 (16.8, 30.3) |
| 200% or above FPL | 55.1 (51.5, 58.7) | 53.8 (48.6, 58.9) | 64.4 (58.5, 70.3) | 83.5 (77.9, 89.1) | 51.7 (43.4, 60.0) | 73.4 (66.2, 80.7) | 65.3 (57.8, 72.8) |
| Nativity | |||||||
| Foreign born in US 0–9 yrs | 23.7 (20.4, 27.0) | 23.6 (18.8, 28.4) | 16.3 (11.8, 20.8) | 5.7 (1.6, 9.9)b | 22.8 (15.5, 30.1) | 30.5 (22.6, 38.4) | 14.6 (8.4, 20.7) |
| Foreign born in US 10 + yrs | 53.8 (50.1, 57.4) | 62.5 (57.3, 67.6) | 52.0 (46.1, 58.0) | 15.8 (11.1, 20.6) | 62.8 (54.1, 71.5) | 52.9 (44.8, 61) | 57.6 (49.8, 65.3) |
| US Born | 22.5 (19.4, 25.6) | 14.0 (10.7, 17.2) | 31.6 (25.9, 37.4) | 78.4 (72.6, 84.2) | 14.4b (6.8, 22.1) | 16.6 (10.8, 22.3) | 27.9 (20.9, 34.8) |
| Language most used at home | |||||||
| Asian language | 72.8 (69.6, 76.1) | 81.9 (77.6, 86.1) | 32.2 (26.6, 37.9) | 11.5 (6.8, 16.2) | 84.2 (76.5, 91.8) | 28.6 (21.2, 36) | 29.0 (21.7, 36.3) |
| English | 27.2 (23.9, 30.4) | 18.1 (13.9, 22.4) | 67.8 (62.1, 73.4) | 88.5 (83.8, 93.2) | 15.8b (8.2, 23.5) | 71.4 (64.0, 78.8) | 71.0 (63.7, 78.3) |
| Smoking status | |||||||
| Non-smoker/former smoker | 89.4 (86.9, 91.9) | 81.6 (77.0, 86.2) | 87.2 (82.9, 91.5) | 89.9 (86.0, 93.8) | 86.1 (80.3, 91.9) | 92.3 (88.0, 96.5) | 91.3 (87.9, 94.7) |
| Current/non-regular | 10.6 (8.1, 13.1) | 18.4 (13.8, 23.0) | 12.8 (8.5, 17.1) | 10.1 (6.2, 14.0) | 13.9 (8.1, 19.7) | 7.7b (3.5, 12.0) | 8.7 (5.3, 12.1) |
| Alcohol drinking | |||||||
| Non-drinkers | 60.8 (57.2, 64.5) | 57.6 (52.3, 62.9) | 57.8 (51.9, 63.8) | 47.3 (40.7, 54.0) | 63.7 (55.2, 72.2) | 58.5 (50.7, 66.3) | 61.8 (54.4, 69.3) |
| Low-mod drinkers | 31.4 (27.9, 34.9) | 25.3 (20.6, 30.1) | 26.5 (21.2, 31.8) | 42.9 (36.3, 49.5) | 16.4 (9.6, 23.3) | 34.4 (26.9, 41.8) | 25.6 (19.4, 31.8) |
| Heavy or binge drinkers | 7.7 (5.7, 9.7) | 17.1 (12.8, 21.3) | 15.7 (11.0, 20.4) | 9.7b (5.1, 14.4) | 19.9 (12.7, 27.0) | 7.1b (3.2, 11.0) | 12.5b (6.5, 18.6) |
| Physical activityc | |||||||
| Meets guidelines | 46.0 (42.4, 49.7) | 41.2 (35.9, 46.5) | 57.7 (51.9, 63.4) | 49.0 (42.2, 55.7) | 46.6 (38.2, 54.9) | 54.9 (46.9, 62.9) | 50.0 (42.4, 57.6) |
| Some PA | 17.0 (14.3, 19.7) | 12.9 (9.2, 16.5) | 16.3 (11.9, 20.6) | 15.9 (10.8, 21.0) | 20.7 (14.1, 27.3) | 17.2 (11.2, 23.1) | 21.1 (14.7, 27.5) |
| Inactive | 37.0 (33.5, 40.5) | 46.0(40.8, 51.1) | 26.1 (21.1, 31.0) | 35.1 (28.9, 41.4) | 32.7 (24.7, 40.8) | 27.9 (20.7, 35.2) | 28.9 (22.2, 35.6) |
| Regular BMI standardd | |||||||
| Under/normal | 71.2 (67.7, 74.7) | 65.6 (60.1, 71.1) | 48.6 (42.6, 54.6) | 62.4 (56.1, 68.8) | 70.2 (61.8, 78.7) | 56.7 (48.6, 64.7) | 55.8 (48.1, 63.5) |
| Overweight | 22.5 (19.3, 25.6) | 30.8 (25.6, 36.0) | 37.6 (31.7, 43.5) | 29.2 (23.4, 35) | 25.3 (17.8, 32.8) | 35.6 (27.9, 43.3) | 34.2 (26.8, 41.5) |
| Obesity | 6.3 (4.2, 8.4) | 3.6b (0.8, 6.4) | 13.8 (9.7, 18.0) | 8.4 (4.9, 11.9) | 4.5b (0.0, 10.3) | 7.7b (3.3, 12.2) | 10.0 (5.8, 14.2) |
Data are weighted proportions. South Asian includes Asian Indian, Sri Lankan, Pakistani, and Bangladeshi.
The estimate is statistically unstable (relative standard error ≥ 23%) and therefore may not be appropriate to use for planning or policy purposes.
To meet Physical Activity Guidelines at least one of the following at least one of the following criteria must be fulfilled: 1) Vigorous Activity - hard physical activity causing heavy sweating, large increases in breathing and heart rate - for 20 + minutes, ≥ 3 days/wk, 2) Moderate Activity - cause light sweating, slight increases in breathing and heart rate - for 30 + minutes, ≥ 5 days/wk, 3) A combination of Vigorous and Moderate Activity meeting the time criteria for ≥ 5 days/wk. [REFERENCES: Vigorous Activity: U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: U.S. Government Printing Office, November 2000. Moderate Activity: Centers for Disease Control and Prevention/American College of Sports Medicine, http://www.cdc.gov/nccdphp/dnpa/physical/recommendations/index.htm].
Overweight: 25 ≤ BMI < 30.0 kg/m2. Obesity: BMI ≥ 30.0 kg/m2.
3.2. Prevalence of hypertension among Asians compared to other races/ethnicities
The age-adjusted prevalence of hypertension was lower among Asians compared to other race/ethnic groups in 2005. However, hypertension increased by 18% among Asians, from 19.6% in 2005 to 23.1% in 2015. Hypertension prevalence did not increase among other racial/ethnic groups over this time period (Table 2).
Table 2.
Age-adjusted prevalence of hypertension by races/ethnicities, and adjusted odds ratios of hypertension among Asian subgroups, LA CountyRR.
| Race/ethnicity | 2005 (n = 8361) | 2007 (n = 7019) | 2011 (n = 7942) | 2015 (n = 7919) | 2005–15 (n = 31,241) | Adjusted OR¥ |
|---|---|---|---|---|---|---|
| Latino | 25.9 (24.1, 27.1) | 26.5 (24.7, 28.3) | 24.4 (22.4, 26.3) | 23.6 (21.7, 25.5) | 25.0 (24.1, 26.0) | N/A |
| black | 37.0 (32.8, 41.2) | 39.1 (34.4, 43.9) | 38.3 (34.5, 42.1) | 32.4 (29.1, 35.8) | 37.0 (34.9, 39.1) | N/A |
| white | 22.8 (21.1, 24.5) | 22.8 (21.0, 24.6) | 21.9 (20.3, 23.4) | 21.8 (20.0, 23.6) | 22.2 (21.4, 23.1) | 1.00 |
| Asianb | 19.6 (17.1, 22.1)⁎ | 24.8 (21.6, 28.0) | 25.9 (22.3, 29.4) | 23.1 (20.0, 26.3) | 23.4 (21.9, 25.0) | – |
| Chinese | 18.0 (13.6, 22.3) | 19.2 (14.9, 23.5) | 22.8 (17.9, 27.7) | 19.1 (14.4, 23.7) | 20.0 (17.6, 22.4) | 1.07 (0.77, 1.50) |
| Korean | 16.7 (12.4, 20.9) | 24.0 (16.2, 31.9) | 26.9 (17.4, 36.3) | 19.9 (9.3, 30.5) | 21.7 (17.5, 25.8) | 1.29 (0.85, 1.96) |
| Vietnamese | 28.2 (22.2, 34.3) | 25.1 (13.5, 36.8) | - | 35.1 (20.7, 49.6) | 22.5 (17.1, 27.9) | 1.25 (0.73, 2.14) |
| South Asianξ | 18.2 (5.3, 31.1) | 22.0 (14.9, 29.1) | 27.7 (17.5, 38.0) | 26.3 (15.9, 36.7) | 23.2 (17.6, 28.7) | 1.15 (0.68, 1.94) |
| Japanese | 18.9 (13.4, 24.5) | 28.3 (20.7, 35.8) | 27.7 (18.0, 37.4) | 17.7 (11.7, 23.8) | 23.3 (19.4, 27.3) | 1.45 (1.09, 1.94) |
| Filipino | 25.6 (16.8, 34.5) | 34.3 (25.2, 43.3) | 38.9 (29.2, 48.7) | 31.3 (24.0, 38.6) | 32.7 (28.1, 37.3) | 2.05 (1.49, 2.82) |
| Other Asian | 15.5 (7.3, 23.6) | 24.4 (13.8, 35.0) | 22.8 (12.6, 33.0) | 29.3 (16.7, 42.0) | 24.7 (19.1, 30.2) | 1.21 (0.76, 1.94) |
bAfter controlling for age, Asian vs. white.
- The result was suppressed due to the small sample size.
¥ Model included Asian subgroups, age (categorical), gender, education, income, nativity, language most used at home, smoking, drinking, physical activity and BMI comparing to whites.
ξ Includes Asian Indian, Sri Lankan, Pakistani, Bangladeshi.
RRSurvey Response Rate: 24.5% in 2005; 18.0% in 2007; 28.4% in 2011; and 15.0% in 2015.
p < 0.05.
The age-adjusted prevalence of hypertension among Asians (23.4%) was lower than that of blacks for all years, was lower than that of Latinos in 2005, 2007 and 2015 but not 2011, and was lower than that of whites in 2005, but surpassed whites in 2007, 2011 and 2015.
3.3. Prevalence of hypertension among Asian subgroups
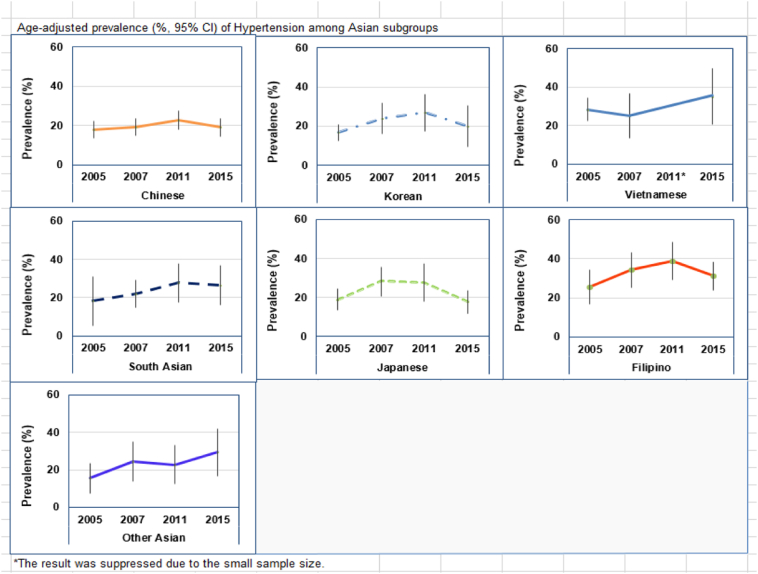
Among Asian subgroups, the age-adjusted prevalence of hypertension was the lowest among Chinese (20.0%), and highest among Filipinos (32.7%) (Table 2, Fig. 1). The age-adjusted prevalence of hypertension was significantly higher among Filipinos (p < 0.05), compared to whites. After adjusting for age, gender, Asian ethnic subgroups, education, income, nativity, language most used at home, smoking, drinking, physical activity and BMI, Filipinos were found to be at significantly higher risk for hypertension than whites, and Chinese were found to be at lower risk.
Fig. 1.
Age-adjusted prevalence (%, 95% CI) of hypertension among Asian subgroups.
3.4. Factors associated with hypertension among Asians
The prevalence of hypertension was highest among Asians aged 65 years or older, those who had less than a high school education, were living in poverty, foreign born but living in the U.S. over 10 years, did not meet physical activity guidelines or were physically inactive, or overweight or obese (Table 3).
Table 3.
Unadjusted prevalence of hypertension, crude and adjusted odds ratios of hypertension among Asians, LA County.
| Characteristic | % (95% CI) | Crude OR (95% CI) | Adjusted ORa (95% CI) |
|---|---|---|---|
| Age (years) | |||
| 18–29 | 4.9 (2.5, 7.2) | 1.00 | 1.00 |
| 30–49 | 13.9 (11.3, 16.4) | 3.13 (1.81, 5.41) | 2.99 (1.59, 5.63) |
| 50–64 | 32.9 (29.1, 36.8) | 9.59 (5.62, 16.34) | 8.90 (4.75, 16.68) |
| 65 + | 59.6 (55.2, 64.1) | 29.00 (16.95, 49.62) | 30.54 (16.41, 56.84) |
| Gender | |||
| Female | 21.0 (18.8, 23.3) | 1.00 | 1.00 |
| Male | 24.0 (21.4, 26.6) | 1.19 (0.98, 1.45) | 1.19 (0.91, 1.56) |
| Education | |||
| Less than high school | 34.2 (27.8, 40.5) | 1.00 | 1.00 |
| High school/some college or trade school | 22.1 (19.2, 25.1) | 0.56 (0.40, 0.77) | 0.93 (0.60, 1.42) |
| College or post graduate degree | 20.4 (18.2, 22.6) | 0.50 (0.36, 0.68) | 0.80 (0.52, 1.22) |
| Household Income | |||
| 0–99% FPL | 26.8 (22.2, 31.3) | 1.00 | 1.00 |
| 100–199% FPL | 24.1 (20.3, 27.8) | 0.87 (0.63, 1.18) | 0.89 (0.59, 1.33) |
| 200% or above FPL | 20.8 (18.7, 23.0) | 0.72 (0.55, 0.94) | 0.76 (0.52, 1.12) |
| Nativity | |||
| US born | 18.9 (16.0, 21.8) | 1.00 | 1.00 |
| Foreign born in US 0–9 years | 11.2 (7.9, 14.5) | 0.53 (0.36, 0.78) | 0.83 (0.51, 1.35) |
| Foreign born in US 10 + years | 28.7 (26.1, 31.3) | 1.71 (1.36, 2.15) | 1.14 (0.81, 1.61) |
| Language Most Used at Home | |||
| Asian language | 23.3 (20.9, 25.7) | 1.00 | 1.00 |
| English | 21.6 (19.0, 24.1) | 0.90 (0.74, 1.11) | 1.14 (0.82, 1.57) |
| Smoking status | |||
| Non-smoker/former smoker | 22.5 (20.7, 24.3) | 1.00 | 1.00 |
| Current/non-regular | 22.0 (16.3, 27.7) | 0.96 (0.68, 1.36) | 1.43 (0.94, 2.18) |
| Alcohol drinking | |||
| Non-drinkers | 24.6 (22.3, 26.8) | 1.00 | 1.00 |
| Low-mod drinkers | 22.2 (18.8, 25.6) | 0.87 (0.69, 1.10) | 0.99 (0.73, 1.34) |
| Heavy or binge drinkers | 12.8 (8.5, 17.2) | 0.45 (0.30, 0.68) | 0.66 (0.39, 1.13) |
| Physical activity | |||
| Meets guidelines | 21.1 (18.6, 23.5) | 1.00 | 1.00 |
| Not meet guidelines | 25.8 (21.0, 30.5) | 1.32 (0.99, 1.76) | 1.25 (0.87, 1.81) |
| No activity | 22.9 (20.0, 25.8) | 1.11 (0.89, 1.38) | 0.89 (0.68, 1.17) |
| Regular BMI standard | |||
| Normal/underweight | 17.6 (15.7, 19.6) | 1.00 | 1.00 |
| Overweight | 31.1 (27.3, 35.0) | 2.09 (1.67, 2.61) | 2.36 (1.79, 3.11) |
| Obesity | 34.3 (25.9, 42.7) | 2.38 (1.61, 3.52) | 3.56 (2.22, 5.71) |
Among all Asians, Hosmer-Lemeshow Goodness-of-Fit Test: X2 = 9.15, p = 0.33.
The associations between hypertension and the dependent variables were found through crude/unadjusted ORs. These factors included age group, education, income, nativity, smoking status, alcohol drinking, BMI status.
After adjusting for age, gender, education, income, nativity, and language most used at home, smoking, alcohol drinking, physical activity, and BMI, Asian adults aged 30–49, 50–64, 65 + years were 3.0, 8.9, and 30.5 times more likely to report being diagnosed with hypertension, compared with those aged 18–29 years.
Asians who were foreign-born (but living in the U.S. over 10 years) had borderline increased odds of hypertension compared to those U.S. born.
Asian adults who were categorized as overweight or obese were, respectively, 2.4 and 3.6 times more likely to report being diagnosed with hypertension than their normal-to-underweight peers.
4. Discussion
Though the prevalence of hypertension among Asians has been increasing rapidly in other countries, few studies have examined the prevalence of hypertension among Asians and Asian subgroups in the United States. Although the prevalence of hypertension remains highest among Blacks in LA County (37%), hypertension among Asians and Asian subgroups may be an under-recognized public health concern. The 2011–12 National Health and Examination Survey found that hypertension in non-Hispanic Asians (18 +) was 24.7%, (Nwankwo et al., 2013) similar to the finding in our study. Los Angeles County is home to the largest and one of the most diverse Asian populations in the U.S., allowing us to report disaggregated results for Asians. We found the prevalence of hypertension varied among Asian subgroups, and was highest among Filipinos, who also have higher rates of obesity and diabetes (Shih et al., 2014). The prevalence of hypertension among Asians has been increasing rapidly—from our study and other studies in the US and in Asian countries (Jose et al., 2013, Wang et al., 2014). Increased attention should be paid to Asian subgroups that are at significantly increased risk for hypertension, particularly Filipinos.
Additionally, several factors were identified as associated with hypertension in this Asian sample. These include age group, federal poverty level, and being overweight or obese. This can inform the development of effective prevention programs targeting the population that this sample represents. These factors are similar to risk factors for hypertension that have been identified among other racial/ethnic groups in the U.S. that have been more thoroughly studied.
5. Limitations
We acknowledge several limitations of this study. The data are cross-sectional and cannot be used to infer causation. Second, the data are also self-reported, and therefore subject to recall bias. Third, the 2005–2007 data do not represent individuals living in group quarters, such as in nursing homes, college dormitories, or jails. Fourth, increasing proportion of cell phone only households in the populations were not considered in this study, and there may be differential rates of cell phone only users in different racial/ethnic groups and in different Asian subgroups. These may impact the results related to trends in prevalence of hypertension. Fifth, due to sample size limitations, the data were aggregated over a 10 year period to perform the multivariate logistic regression among Asian respondents. This limited our ability to examine trends over time, and we did not account for survey time periods in the modeling. Finally, although the response rates are low, they are comparable to those of other large state-based telephone surveys and reflect a decline in telephone survey response rates nationwide. However, studies have demonstrated that non-response does not necessarily introduce substantial bias into survey estimates (Keeter et al., 2006, Keeter et al., 2000). We compared our survey sample demographics and found the sample closely reflected the demographic makeup of the Los Angeles County's adult population (not shown). In addition, sample weights were used to account for differential probability of selection, nonresponse, noncoverage, and type of telephone service.
6. Conclusion
Hypertension among Asian Americans is a serious public health concern, with 23.4% of Asian adults in Los Angeles County reporting a hypertension diagnosis. The prevalence of hypertension varies significantly among Asian ethnic subgroups, with Filipinos having the highest prevalence. Risk factors for hypertension among Asian subgroups mirror those in the population at large. Culturally sensitive approaches should be incorporated into evidence based interventions to prevent and control hypertension among Asians and Asian subgroups in the U.S.
Conflict
All authors declare that they have no conflicts of interest.
Transparency document
Transparency document.
Acknowledgments
The authors wish to thank Dr. Yan Cui, Mr. Jerome Blake, and other colleagues in the Office of Health Assessment and Epidemiology for their assistance.
Footnotes
The Transparency document associated with this article can be found, in the online version.
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.pmedr.2017.03.009.
Appendix A. Supplementary data
The following is the supplementary data related to this article.
Demographic Profile of Los Angeles County Adult (18 + years), LACHS1 Compared to PEPS (2010 American Community Survey and other Census Bureau data; Pew Research Center, 2012).
References
- 2010 American Community Survey and other Census Bureau data; Pew Research Center . State Department; U.S.: 2012. Asian-American Survey.http://www.pewsocialtrends.org/asianamericans-graphics/ [Google Scholar]
- Ikeda N. Control of hypertension with medication: a comparative analysis of national surveys in 20 countries. Bull. World Health Organ. 2014;92(1):10–19C. doi: 10.2471/BLT.13.121954. 10.2471/BLT.13.121954 (Epub Sep 30, 2013, [online] ISSN 0042–9686). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jose P., Zhao B., Chung S., Fortmann S., Palanippan L. PS1-46: variation in hypertension prevalence among Asian American subgroups: Results from PACS (pan Asian cohort study) Clin. Med. Res. 2013;11:136. [Google Scholar]
- Keeter S., Miller C., Kohut A., Groves R.M., Presser S. Consequences of reducing nonresponse in a national telephone survey. Public Opin. Q. 2000;64(2):125–148. doi: 10.1086/317759. [DOI] [PubMed] [Google Scholar]
- Keeter S., Kennedy C., Dimock M., Best J., Graighill P. Gauging the impact of growing nonresponse on estimates from a national RDD telephone survey. Public Opin. Q. 2006;70(5):759–779. [Google Scholar]
- Nwankwo T., Yoon S.S., Burt V., Gu Q. National Center for Health Statistics; Hyattsville, MD: 2013. Hypertension Among Adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief, no 133. [PubMed] [Google Scholar]
- Pierannunzi C., Town M., Garvin W., Shaw F.S., Balluz L. Methodologic changes in the behavioral risk factor surveillance system in 2011 and potential effects on prevalence estimates. MMWR Morb. Mortal. Wkly Rep. 2012;61(22):410–413. [PubMed] [Google Scholar]
- Population Estimates . 2014. American Community survey, census of population and housing, Current population survey, small area health insurance estimates, small area income and poverty estimates, state and county housing unit estimates, county business patterns, Nonemployer statistics, economic census, survey of business owners. Building Permits. [Google Scholar]
- Shih M., Du Y., Lightstone A.S., Simon P.A., Wang M.C. Stemming the tide: rising diabetes prevalence and ethnic subgroup variation among Asians in Los Angeles County. Prev. Med. 2014;63:90–95. doi: 10.1016/j.ypmed.2014.03.016. [DOI] [PubMed] [Google Scholar]
- Simon Paul A., Wold Cheryl M., Cousineau Michael R., Fielding Jonathan E. Meeting the data needs of a local health department: the Los Angeles County health survey. Am. J. Public Health. December 2001;91(12):1950–1952. doi: 10.2105/ajph.91.12.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tormo M.J., Navarro C., Chirlaque M.D., Barber X. Validation of self diagnosis of high blood pressure in a sample of the Spanish EPIC cohort: overall agreement and predictive values. Epic Group of Spain. J. Epidemiol. Community Health. 2000;54:221–226. doi: 10.1136/jech.54.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States. Dept. of Commerce. U.S. Census Bureau . U.S. Census Bureau; Washington DC: March 2012. The Asian Population: 2010 Census Briefs. By Elizabeth M. Hoeffel, Sonya Rastogi, Myoung Ouk Kim, and Hasan Shahid.http://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf [Google Scholar]
- Wang Fujun. Risk factors for hypertension in India and China: a comparative study. Health Popul. Perspect. Issues. 2014;37(1 & 2):40–49. [Google Scholar]
- Yi Stella S. Disparities in meeting physical activity guidelines for Asian-Americans in two metropolitan areas in the United States. Ann. Epidemiol. 2015;25:656–660. doi: 10.1016/j.annepidem.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.
Demographic Profile of Los Angeles County Adult (18 + years), LACHS1 Compared to PEPS (2010 American Community Survey and other Census Bureau data; Pew Research Center, 2012).