Abstract
Jailed women are four-five times more likely to have had cervical cancer compared to women without criminal justice histories. Previous research has shown that an important contributor to cervical cancer risk, and perhaps lack of follow-up, is incarcerated women's low health literacy about broader reproductive health issues. Little work has been done to address this disparity. Thus, the objective of this study was to test the effectiveness of an intervention to improve incarcerated women's cervical health literacy and ultimately address cervical cancer disparities. Using a waitlist control design, we compared changes in cervical health literacy (knowledge, beliefs, self-efficacy, and confidence for screening and follow-up) among 188 incarcerated women who completed a 10-hour intervention between 2014 and 2016 in three Kansas City jails. We used bivariate tests and multivariate analyses that controlled for baseline cervical health literacy level and key covariates. Women in the intervention group showed significant gains in seven out of eight cervical health literacy domains (all p < 0.01), whereas the control group only improved in one domain (p < 0.01). When controlling for covariates, the intervention group had less barriers, perceptions of seriousness, susceptibility to disease, and increased self-efficacy for cervical health screening and follow-up, compared to the control group (all p < 0.05). A brief intervention is an effective way to improve jailed women's cervical health literacy, but should be provided alongside systemic efforts that expand access to correctional preventive health services, including the human papillomavirus vaccine, community-based cancer screenings, and health insurance after women leave jails and transition back to communities.
Keywords: Health literacy, Cervical cancer, Cervical health literacy, Jails, Women's health
Highlights
-
•
Incarcerated women are at high risk for cervical cancer.
-
•
A brief intervention can improve high-risk women's cervical health literacy.
-
•
Information and cancer preventing technologies could be extended to high-risk women.
1. Introduction
Over the past 40 years the U.S. has witnessed a significant drop in cervical cancer rates, due to longstanding routine Papanicolaou (Pap) testing, new advances in human papillomavirus (HPV) typing, HPV vaccine, and most recently, expanded coverage for women's health services through the Affordable Care Act (ACA) (Centers for Disease Control and Prevention (CDC), 2016; Koh & Sebelius, 2010). However, the most vulnerable women in the U.S. – the one million American women in jails and prisons, or under community correctional supervision – may have missed the benefits of these interventions altogether (Kaeble et al., 2015, Binswanger et al., 2009). This group of women, particularly in the industrialized countries where research has been conducted over the last four decades, has demonstrably higher rates of cervical cancer, abnormal Pap test histories, and lower rates of Pap screening compared to women without criminal justice histories (Binswanger et al., 2009, Audet-LaPointe, 1971). To date, there is little data available on incarcerated women's experiences with HPV vaccine, though recent studies indicate that these women are likely under-vaccinated as well (Ramaswamy et al., 2011).
The path to poor cervical health among incarcerated women starts early, as they bear the burden of all the markers of cervical cancer risk: poverty, low education, tobacco use, early sex initiation, a lifetime of exposure to sexual and physical trauma, and other risks like high rates of HPV and histories of sexually transmitted infection (STIs) (Ramaswamy et al., 2011, Herbst et al., 2016). However, most incarcerated women in the U.S. have had exposure to routine cervical health screening as they are of childbearing age and have had, on average, two pregnancies (Ramaswamy et al., 2011, Binswanger et al., 2005).These studies report routine Pap screening rates among incarcerated women in the U.S. as high as 84–90% (Ramaswamy et al., 2011, Binswanger et al., 2005), though others report that less than half of these women gain access to recommended clinical follow-up after an abnormal Pap test (Martin et al., 2008). In probing incarcerated women about their Pap screening and follow-up experiences, we and others have found that they do in fact report low levels of cervical health literacy (Binswanger et al., 2005, Ramaswamy et al., 2015), which may partly explain their poor cervical health outcomes relative to the general population.
The Institute of Medicine (IOM) report, Health Literacy, A Prescription to End Confusion, says that, “Health literacy level is the product of a complex set of skills and interactions on the part of the individual, the health care system, the education system, and the cultural and societal context” (Nielsen-Bohlman et al., 2004). Incarcerated women have uniquely complicated barriers when it comes to cervical health literacy – specifically, complex risk histories and environments that may affect their ability to act on knowledge about cervical health. For example, one barrier to knowledge stems from frequent STI checks, which inadvertently cause confusion over pelvic and Pap screening (Kelly et al., 2017). Furthermore, these women's long trauma histories tend to impact on their beliefs about Pap screening – that is, an expectation of fear, discomfort, and questionable safety during gynecological exams (Ramaswamy & Kelly, 2015). Finally, their self-efficacy for Pap screening and follow-up may be compromised by drug use; mental health problems; trading sex for money, drugs, or shelter; and a lifetime of cycling in and out of the criminal justice system (Ramaswamy and Kelly, 2015, Clarke et al., 2007).
Thus, we operationalize cervical health literacy broadly as knowledge, beliefs, self-efficacy, and confidence for navigating health systems, in part as a reflection of the IOM report and our own need to tailor an intervention to the high-risk group of women we work with given the unique risk histories and environments in which they interact (Ramaswamy et al., 2015). We developed the Sexual Health Empowerment (SHE) Project (Ramaswamy et al., 2015), an intervention focused on “interactive health literacy” (Nutbeam, 2000), where we impart both knowledge and skills to increase women's cervical health literacy. Our objective was to test the effectiveness of an empirically-based, theory-informed, and pilot-tested cervical health literacy intervention designed to reduce the persistent cervical health disparities faced by incarcerated women.
2. Methods
2.1. Study site
Participant recruitment occurred at three county jails that straddle both sides of the Kansas City, Kansas and Missouri state line. The two urban jails had capacity for 800 and 300 inmates each; the third jail in a suburban location had capacity for 1000 inmates. Fifteen percent of the total population was female. The two urban jails were within fives miles from a major medical center, and the third was about 10 miles from the nearest hospital. Health departments, low-cost clinics, and community-based behavioral health clinics serve the area. Inmates in all three facilities undergo a medical intake process and can request medical treatment and medicines for a fee through jail health services (indigent patients accrue debt), which were contracted out to correctional health care corporations at each of the facilities. Preventive health care services, for example Pap tests and STI screening, were not available unless medically necessary.
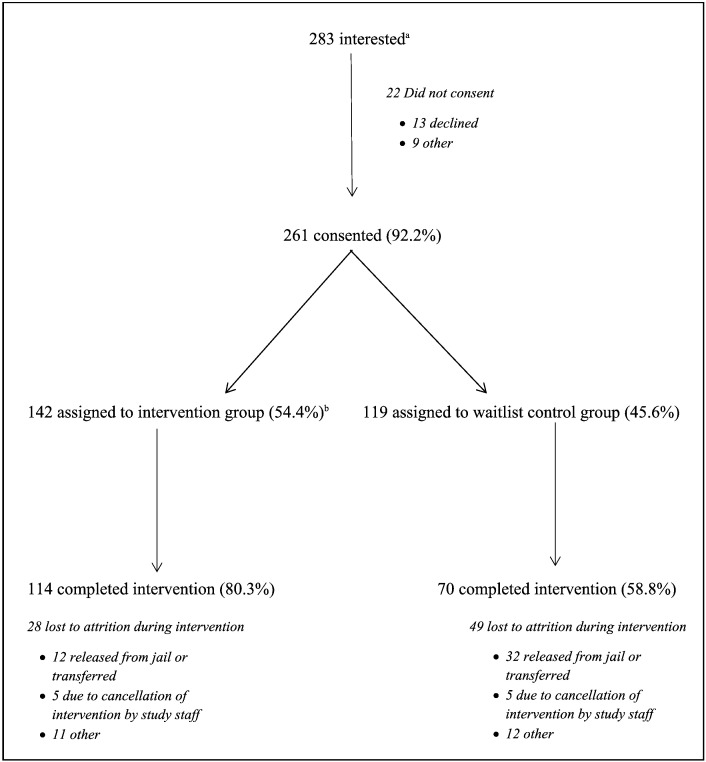
We recruited participants on a rolling basis at minimum and medium security housing units in 26 intervention cohort groups across the three facilities from September 2014 to March 2016. Fig. 1 describes average daily census, recruitment, and intervention participation.
Fig. 1.
Intervention participation flowchart.
Notes.
aFrom September 2014 to March 2016, we recruited participants in 26 cohorts. During each recruitment cohort, the average daily census at the jail was 38.9; an average of 10.9 participants were interested; and an average of 10.0 participants were recruited. Within each cohort, participants were randomly assigned to the intervention (average of 5.5 participants) or waitlist control group (average of 4.6 participants).
bIf ≤ 5 participants were recruited during a cohort, then all participants were assigned to the intervention group.
2.2. Intervention
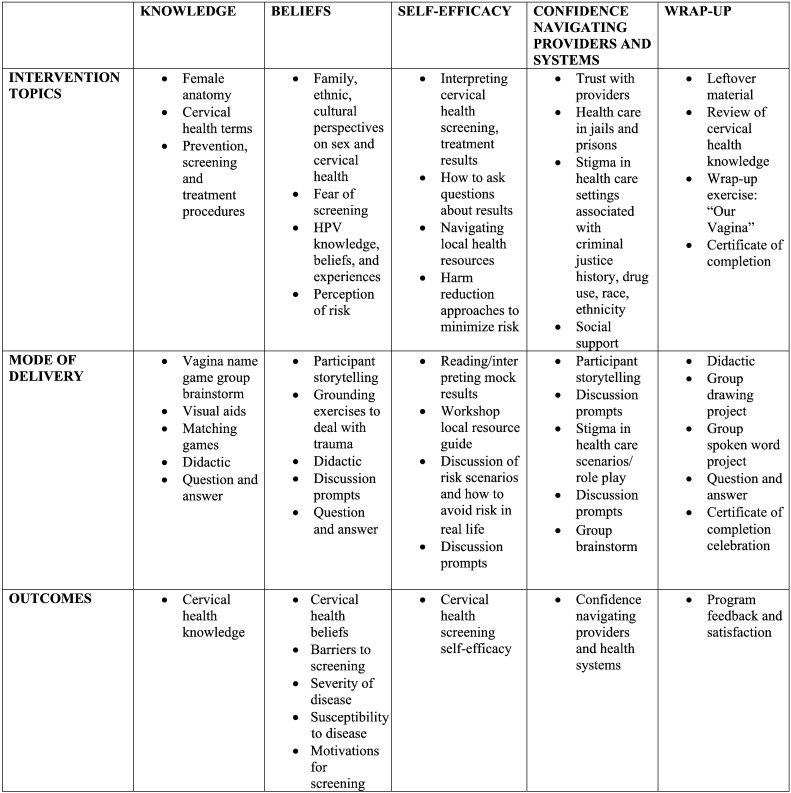
The SHE Project was a cervical health literacy intervention designed to improve incarcerated women's knowledge about cervical health, reduce barriers to screening and treatment that stem from beliefs about cervical cancer, improve self-efficacy for cervical cancer screening and follow-up, and increase women's confidence for navigating interactions with health care providers and systems (Ramaswamy et al., 2015 and see Fig. 2). The content of these individual sessions was driven by our own data collection on the cervical health literacy of incarcerated women (Ramaswamy & Kelly, 2015), as well as the general literature on cancer health literacy and unique barriers that incarcerated women might face (Hunter, 2005, Eggleston et al., 2007, Binswanger et al., 2011, Lindau et al., 2006, Magee et al., 2005). But the overall flavor of the intervention was rooted in social and feminist theory. We sought to understand women's experiences within their social and political contexts, emphasizing: the role of romantic and sexual partnerships, family, and community in women's lives; the impact of race, class, and gender on specific health outcomes; and a rejection of status quo values and assumptions about women in general (Bourdieu, 1984, Andrist and MacPherson, 2001).
Fig. 2.
Sexual Health Empowerment (SHE) Project intervention topics, delivery, outcomes.
Note.
More information about intervention development and content can be found in Ramaswamy et al. (2015). The intervention manual and training in delivery can also be requested at www.kumc.edu/she.
The intervention was delivered in small-group format on five sequential days, each for a two-hour period, resulting in 10 total hours of contact. The group format was selected to allow women to leverage the social capital in the room, and sort through the strengths and weaknesses brought to the group, given women's insider knowledge of communities, correctional facilities, and the streets. Finally, we developed the intervention for short-term correctional facilities with lower security housing units so we could track for a subsequent study the long-term cervical health screening and follow-up outcomes for women as they transition back to their communities.
2.3. Study design, sample, and procedures
We employed a waitlist control design to evaluate the effectiveness of the intervention. We chose this design to address the ethical dilemma of using an untreated control group, since we felt strongly that all participants would benefit from a reproductive health intervention beyond just providing pamphlets or some other form of basic self-directed health education. Thus, in each cohort we systematically assigned half the participants to receive the intervention in week one, and the other half to receive the intervention in week two (see Fig. 1), with the latter group comprising the waitlist control group for each recruitment cohort.
Systematic intervention group assignment occurred according to seating during consent: every other person went to the week one group (intervention group), while the rest went to the week two group (waitlist control group). There were no exceptions to this, unless ≤ 5 participants were recruited during a cohort, in which case all participants were assigned to the intervention group, resulting in a slightly imbalanced sample (54.4% intervention cases and 45.6% control cases). The intervention and waitlist control groups were similar on all sociodemographic and health history characteristics (see Table 1), except more women in the control group had an abnormal Pap test history or HPV diagnosis (61.8% vs. 44.6% and 18.4% vs. 11.7%, respectively, p < 0.05). We have no information about what accounted for these differences.
Table 1.
Participant characteristicsa.
| Total (n = 188), mean ± SD or No. (%) | Intervention (n = 112), mean ± SD or No. (%) | Waitlist control (n = 76), mean ± SD or No. (%) | p-Valueb | |
|---|---|---|---|---|
| Age | 34.02 ± 9.45 | 34.09 ± 9.41 | 33.92 ± 9.58 | 0.905 |
| Race | 0.482 | |||
| White | 94 (50.0) | 52 (46.4) | 42 (55.3) | |
| Black | 56 (29.8) | 38 (33.9) | 18 (23.7) | |
| Other | 34 (18.1) | 20 (17.9) | 14 (18.4) | |
| Latina ethnicity | 17 (9.0) | 9 (8.0) | 8 (10.5) | 0.697 |
| High school or more | 118 (62.8) | 71 (63.4) | 47 (61.8) | 0.410 |
| Homeless or institutionalized | 48 (25.5) | 28 (25.0) | 20 (26.3) | 0.637 |
| Employedc | 61 (32.5) | 40 (35.7) | 21 (27.6) | 0.107 |
| Received public benefitsd | 89 (47.3) | 58 (51.8) | 31 (40.8) | 0.331 |
| Insured | 73 (38.8) | 43 (38.4) | 30 (39.5) | 0.902 |
| Has primary care doctor | 72 (38.3) | 46 (41.1) | 26 (34.2) | 0.357 |
| Has medical home | 131 (69.7) | 77 (68.8) | 54 (71.1) | 0.484 |
| Past month tobacco use | 152 (80.9) | 86 (76.8) | 66 (86.8) | 0.190 |
| Hazardous/harmful alcohol usee | 97 (51.6) | 59 (52.7) | 38 (50.0) | 0.718 |
| Past year drug dependencef | 117 (62.2) | 66 (58.9) | 51 (67.1) | 0.256 |
| History of exchanging sex | 64 (34.0) | 35 (31.3) | 29 (38.2) | 0.593 |
| History of STIsg | 118 (62.8) | 65 (58.0) | 53 (69.7) | 0.103 |
| Past year IPVh | 119 (63.3) | 67 (59.8) | 52 (68.4) | 0.247 |
| Child physical or sexual abusei | 51 (27.1) | 28 (25.0) | 23 (30.3) | 0.690 |
| Mental health problemsj | 138 (73.4) | 79 (70.5) | 59 (77.6) | 0.280 |
| Lifetime months incarcerated | 26.53 ± 49.40 | 25.67 ± 46.91 | 27.83 ± 53.23 | 0.773 |
| Number of pregnancies to term | 2.68 ± 2.02 | 2.78 ± 2.09 | 2.51 ± 1.91 | 0.142 |
| Pap screening in past three years | 126 (67.0) | 76 (67.9) | 50 (65.8) | 0.772 |
| Abnormal Pap test history | 97 (51.6) | 50 (44.6) | 47 (61.8) | 0.049 |
| HPV diagnosis | 27 (14.4) | 13 (11.6) | 14 (18.4) | 0.047 |
| Cervical cancer diagnosis | 26 (13.8) | 14 (12.5) | 12 (15.8) | 0.189 |
Notes.
Participant characteristics are presented for the 188 participants whose data were analyzed in the intent-to-treat analysis, which included 112 participants in the intervention group (participants who completed baseline and post-intervention survey) and 76 participants in the waitlist control group (participants who completed baseline and pre-intervention survey).
p-Values < 0.05 for comparisons between groups are boldfaced.
Full-time, part-time, or on and off.
Cash assistance, food stamps, social security, or disability.
Assessed using AUDIT-C, which is scored on a scale of 0–12 (scores of 0 reflect no alcohol use). In women, a score of 3 or more is considered positive for alcohol problems (Bradley et al., 2007).
Assessed using DSM IV criteria, where If participants answer “yes” to 3 of 6 DSM-IV criteria, they were classified as drug dependent (Compton et al., 2004).
Lifetime diagnosis by a clinician of hepatitis B or C, human immunodeficiency virus, syphilis, gonorrhea, chlamydia, trichomoniasis, herpes, or HPV.
Adapted from Verbal HITS scale, where responses dichotomized so that 1 = any IPV in past year, 0 = no IPV in past year (Sherin et al., 1998).
Adapted from Childhood Experiences of Violence Questionnaire, where responses dichotomized across categories so that 1 = any violence, 0 = no violence (Walsh et al., 2008).
Lifetime diagnosis by a clinician of depression, anxiety, bipolar disorder, or post-traumatic stress disorder.
Participants were eligible for the study if they were sentenced to a minimum or medium security housing unit in the adult facility, which held women age 18 or older. Though we know routine Pap screening is not recommended for women under age 21, we did not want to exclude younger women from the anticipated benefits of a cervical health literacy program. There were no medical exclusions barring eligibility, since our endpoint was to assess the effectiveness of a cervical health literacy program regardless of past medical experiences. Though we did not formally screen for psychological distress, we did not enroll women if they exhibited distress that would impede our ability to obtain written consent (only one person met this exclusion criteria).
We recruited participants several ways: by posting flyers in the housing units advertising the availability of a sexual health educational program; through word-of-mouth recruitment from special programs staff, correctional officers, jail case managers, and other participants; and via direct discussion of the program by study staff in the women's housing units. Interested individuals signed up and were brought to the special programs room at each jail, or to the common area of the housing unit in one facility, on the first day of the study. Study staff explained the study, read consent forms aloud as individuals read along, and answered their questions. After consenting, all participants completed a 158-item baseline survey. The baseline survey was also read aloud by study staff as participants read along. Study staff were available if participants needed assistance reading. Once the baseline survey was complete, participants were systematically assigned to receive the intervention either starting that day (intervention group) or starting the following week (waitlist control group). Women not assigned to the intervention group during systematic intervention group assignment returned to their housing units. Study staff then began Day 1 of the program. After participants in the intervention group completed the program on Day 5, they completed an 82-item post-intervention survey.
When the waitlist control group came in the following week, prior to starting the Day 1 program, they completed a 73-item pre-intervention survey. After completing the program, the waitlist control group also completed the same 82-item post-intervention survey on Day 5. The primary analysis of treatment effectiveness for this study was a comparison of changes in cervical health literacy from baseline to post-intervention for the intervention group; and from baseline to pre-intervention for the waitlist control group (‘true’ control conditions).
The study protocol was approved by a review committee on the protection of human participants.
2.4. Measures
Primary outcomes for this study were measures of cervical health literacy, operationalized as knowledge, beliefs, self-efficacy, and confidence around cervical health screening and follow-up. At pre- and post-test, we used the Pap Knowledge Scale (Fernandez et al., 2009), Health Belief Model Scale for Cervical Cancer and Pap Smear Test (Guvenc et al., 2010), Self-Efficacy Scale for Pap Smear Screening Participation (Hogenmiller et al., 2007), and three questions we developed based on our own preliminary studies about confidence around navigating health systems specific to women with criminal justice involvement (Ramaswamy et al., 2015). The Health Belief Model Scale included five different domains of health beliefs: benefits of screening (e.g. regular Pap tests best way for cancer to be diagnosed early), barriers to screening (e.g. afraid of Pap tests for fear of bad results), perceived seriousness (e.g. cervical cancer would change life), susceptibility to cervical cancer (e.g. chances of getting cervical cancer high), and motivation for screening (e.g. engaging in activities to improve health) (Guvenc et al., 2010). The baseline survey also included questions that assessed participants' sociodemographic characteristics, interaction with the health care system, substance use, sexual health risks, trauma, mental health problems, criminal justice involvement, reproductive health, and cervical cancer risk history (scales described in Table 1).
2.5. Data management and analysis
Completed surveys, identified by unique study ID numbers, were scanned and sent securely to Captricity, a data managing service. Captricity made available a secure and password-protected database in which study staff double-checked the data with clickable photo images of paper survey entries for accuracy. Prior to analysis, missing data due to nonresponse were handled by multiple imputations, in which an expectation-maximization algorithm provided prior estimates of missing values for a subsequent Monte Carlo Markov Chain procedure (Enders, 2010). We created a large number (100) of imputed datasets to ensure accurate recovery of missing data and combined analysis results from each imputed dataset to make valid statistical inferences.
Descriptive statistics were calculated to demonstrate sample sociodemographics and summarize measured variables. To test the primary hypothesis that the intervention would increase cervical health knowledge, reduce barriers to screening that stem from beliefs about cervical cancer, and improve self-efficacy for screening and follow-up, each outcome was compared within and between the intervention and control groups using bivariate tests (chi-square or Fisher's exact test, dependent- or independent-samples t-test with Satterthwaite approximation as appropriate). Further, general linear models were fitted to estimate the intervention effect (i.e. group differences at post-test), after controlling for baseline cervical health literacy scores and key covariates (education, health insurance, and access to a medical home or usual place of care). Statistical significance was determined at 0.05 alpha level and all analyses were conducted using SAS 9.4.
3. Results
Participants were on average 34 years old (SD = 9.45) (see Table 1). Half were White (n = 94, 50.0%), and a third were Black (n = 56, 29.8%). Less than 10% (n = 17) of women reported Latina ethnicity. Two-thirds (n = 118, 62.8%) had completed high school or more education, but only 18.3% (n = 34) were employed full-time prior to incarceration. Less than half of the participants had health insurance (n = 73, 38.8%), but most had access to a medical home or usual place of care (n = 131, 69.7%). Two-thirds of women (n = 126, 67.0%) reported a Pap screening in the past three years. Over half (n = 97, 51.6%) had a lifetime abnormal Pap test history, 14.4% (n = 27) had ever been diagnosed with HPV, and 13.8% (n = 26) had received a cervical cancer diagnosis in the past.
Comparisons of cervical health literacy pre- and post-intervention showed that the intervention group experienced significant changes for seven out of eight domains, including increased knowledge about cervical health (p < 0.001, Cohen's d = 0.32), more perceived benefits to screening (p < 0.01, d = 0.28), reduced barriers to screening (p < 0.001, d = 0.40), reduced perception of seriousness (p < 0.001, d = 0.37), reduced susceptibility to disease (p < 0.01, d = 0.30), and greater motivation (p < 0.001, d = 0.34) and self-efficacy (p < 0.001, d = 0.58) for seeking out cervical health screening and follow-up care (see Fig. 3). The control group only improved in terms of motivation for seeking out screening (p < 0.01, d = 0.36) at post-test. The changes were significantly different between the groups for knowledge (p < 0.5, d = 0.33), reduced barriers (p < 0.05, d = 0.32), perception of the disease's seriousness (p < 0.05, d = 0.36), susceptibility to disease (p < 0.05, d = 0.32), and self-efficacy (p < 0.05, d = 0.36).
Fig. 3.
Cervical health literacy scores at pre-test (baseline) and post-test (post-intervention for intervention cases, pre-intervention for waitlist control cases).
Legend. Black circles and lines represent the intervention group, and gray circles and lines represents the control group.
Note. The intent-to-treat analysis on the primary outcomes includes 112 participants in the intervention group (participants who completed baseline and post-intervention survey) and 76 participants in the waitlist control group (participants who completed baseline and pre-intervention survey).
When controlling for covariates (pre-test cervical health literacy scores, education, health insurance, and access to medical home or usual place of care), the intervention and control groups were significantly different on four outcomes: reduced barriers (p < 0.01, partial η2 = 0.05), perception of seriousness (p < 0.01, partial η2 = 0.05), susceptibility to disease (p < 0.05, partial η2 = 0.03), and increased self-efficacy for cervical health screening and follow-up (p < 0.01, partial η2 = 0.05) (see Table 2).
Table 2.
General linear modeling results.
| Parameter | DV = knowledge (post) |
DV = benefit (post) |
DV = barriers (post) |
DV = seriousness (post) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | t | p | Estimate | SE | t | p | Estimate | SE | t | p | Estimate | SE | t | p | |
| Intercept | 2.68 | 0.33 | 8.15 | 0.000 | 3.28 | 0.26 | 12.65 | 0.000 | 0.97 | 0.18 | 5.48 | 0.000 | 1.98 | 0.25 | 7.89 | 0.000 |
| Pre-test score | 0.35 | 0.07 | 5.12 | 0.000 | 0.33 | 0.05 | 6.61 | 0.000 | 0.53 | 0.06 | 8.69 | 0.000 | 0.41 | 0.07 | 6.10 | 0.000 |
| High school or more | 0.35 | 0.12 | 2.89 | 0.004 | 0.08 | 0.10 | 0.83 | 0.407 | 0.07 | 0.07 | 1.01 | 0.313 | − 0.16 | 0.10 | − 1.48 | 0.138 |
| Insured | − 0.06 | 0.12 | − 0.47 | 0.637 | − 0.05 | 0.10 | − 0.49 | 0.622 | 0.01 | 0.07 | 0.20 | 0.842 | 0.04 | 0.11 | 0.34 | 0.731 |
| Has medical home | 0.05 | 0.13 | 0.41 | 0.685 | 0.20 | 0.11 | 1.89 | 0.058 | − 0.01 | 0.08 | − 0.13 | 0.897 | − 0.17 | 0.12 | − 1.47 | 0.142 |
| Group (intervention) | 0.20 | 0.12 | 1.76 | 0.079 | 0.17 | 0.09 | 1.86 | 0.063 | − 0.20 | 0.07 | − 2.93 | 0.003 | − 0.31 | 0.10 | − 3.07 | 0.002 |
| Parameter | DV = susceptibility (post) | DV = motivation (post) | DV = self-efficacy (post) | DV = confidence (post) | ||||||||||||
| Estimate | SE | t | p | Estimate | SE | t | p | Estimate | SE | t | p | Estimate | SE | t | p | |
| Intercept | 1.52 | 0.23 | 6.51 | 0.000 | 1.36 | 0.20 | 6.71 | 0.000 | 1.09 | 0.17 | 6.46 | 0.000 | 1.21 | 0.21 | 5.71 | 0.000 |
| Pre-test score | 0.45 | 0.07 | 6.79 | 0.000 | 0.56 | 0.06 | 9.01 | 0.000 | 0.69 | 0.05 | 13.72 | 0.000 | 0.58 | 0.06 | 10.52 | 0.000 |
| High school or more | − 0.02 | 0.12 | − 0.16 | 0.872 | − 0.03 | 0.12 | − 0.28 | 0.779 | 0.03 | 0.09 | 0.41 | 0.685 | 0.02 | 0.11 | 0.19 | 0.847 |
| Insured | 0.02 | 0.12 | 0.20 | 0.843 | 0.07 | 0.12 | 0.56 | 0.574 | − 0.09 | 0.09 | − 1.02 | 0.307 | 0.08 | 0.11 | 0.69 | 0.489 |
| Has medical home | − 0.14 | 0.13 | − 1.14 | 0.255 | 0.09 | 0.13 | 0.71 | 0.475 | 0.01 | 0.10 | 0.14 | 0.889 | − 0.02 | 0.12 | − 0.18 | 0.859 |
| Group (intervention) | − 0.24 | 0.11 | − 2.16 | 0.031 | 0.20 | 0.11 | 1.80 | 0.072 | 0.24 | 0.08 | 2.95 | 0.003 | 0.04 | 0.10 | 0.37 | 0.709 |
Note. p-values < 0.05 are boldfaced.
4. Discussion
We demonstrated that a brief jail-based intervention improves cervical health literacy among incarcerated women. Despite the high rates of cervical cancer among women with criminal justice histories, little has been done as far as intervention. We contribute to the field a manualized, easy to implement sexual health program that can be used for this high risk group. A uniqueness of the intervention is its emphasis on the women's real lives: trauma, drug use, sex work, poverty, being uninsured, stigma, and ongoing criminal justice involvement. An important consideration when working with women in short-term correctional facilities is that the group not only needs information on accessing resources from inside jail – they also need it as they transition back to communities and reestablish relationships with family, friends, community-based health providers, and institutions that can facilitate access to housing and health care. Population-tailored interventions work well to address women's deficits in knowledge, their pathways to risk and how those influence beliefs, and the specific challenges to self-efficacy they encounter (Mojica et al., 2016, Scarinci et al., 2012).
We still do not have information about the extent to which changes in cervical health literacy will translate to actionable uptake in cervical cancer prevention behaviors, like the HPV vaccine, routine Pap screenings, follow-ups for abnormal Pap tests, and treatment for the range of sexual and reproductive health problems that at-risk women face. The evidence from other health literacy interventions, though they are few, points in a promising direction: increases in health literacy are associated with increases in knowledge, self-efficacy for screening, and engagement in cancer preventing behaviors (Lindau et al., 2006, von Wagner et al., 2009, Lindau et al., 2002).
Our intervention reduced participants' perception of risk for getting cervical cancer and perception of how bad cervical cancer might be if they did get it. This counters other research that has the goal of increasing perception of risk and severity as a way to increase rates of cervical cancer screening (Williams et al., 2015, Bayu et al., 2016). Instead, we presented the risks of cervical cancer in more realistic terms, which is that from a population perspective, the risks are simply not substantial. For example, cervical cancer is not even in the top three leading causes of cancer deaths for women and is highly preventable and treatable if caught early (CDC, 2017). We chose to focus on the tools needed for prevention, timely screening, and barriers to follow-up, in addition to an emphasis on sexual health in general, rather than cervical cancer, specifically. Our goal as interventionists was to reduce fear associated with the disease so that women would be able to take action without this crippling barrier. Future studies will tease out whether this somewhat non-traditional approach was effective at changing screening practices.
Standard health literacy definitions and popular assessments of health literacy may overemphasize knowledge and numeracy, while ignoring the specific yet pervasive barriers that incarcerated women – or any specific group of women, for that matter – must confront in protecting their health (Lindau et al., 2006, von Wagner et al., 2009, Lindau et al., 2002). At a practical level for our sample, to our knowledge, no health literacy definition or assessment factors in the women's trauma histories. These histories, along with longstanding substance abuse and mental health challenges, overburden women with criminal justice involvement and often stand in the way of achieving health literacy and positive health outcomes. These realities result in a pressing need for interactive health literacy programs to confront the unique challenges that incarcerated women face.
The primary limitation of this study is that it does not yet demonstrate whether an increase in cervical health literacy directly translates to increased screening, which is a key outcome for cervical cancer prevention. But ours is an ongoing longitudinal study that will ultimately examine screening behaviors over time. A second limitation is whether an approach like ours can be scaled up and implemented beyond our jurisdiction. The good news is that the intervention is captured in a manual, tested, and executed with fairly few resources – at a minimum, one well-trained health educator. A final limitation is our departure from the gold standard in study design for testing intervention effectiveness. Our approach using an experimental waitlist control design proved workable, given that group differences were quite clear and that our study design is actually feasible in real-world criminal justice settings. Future studies will demonstrate whether findings translate to other groups of women, though the intervention is tailored to women with the common experiences of trauma, drug use, and criminal justice involvement. Qualitative data gathered during intervention sessions may also provide clues as to ways in which the intervention and delivery is unique to the field.
5. Conclusions
Our program was effective at improving incarcerated women's cervical health literacy. From a broader public health perspective, focus on the ‘biggest bang for the buck’ – particularly at the levels of practice and policy – are of great importance. Ultimately, behavioral interventions like ours would be provided alongside access to preventive health services in corrections, which is rare given the corporatization of both corrections and health care inside jails, where the bottom line is more important than prevention (Cooper et al., 2016). Such preventive services would include provision of the HPV vaccine, the frontline method for HPV-related cancer prevention. Offering vaccines in correctional settings capitalizes on the moment of opportunity for reaching vulnerable people disconnected from traditional forms of preventive health care (Ramaswamy & Freudenberg, 2007). Secondly, as community-based cancer screening venues, like Planned Parenthood and Title X clinics, are increasingly threatened with defunding in the U.S., women in the criminal justice system – and even the larger population of uninsured Americans – are denied key cancer prevention services (Canal, 2015). Expanded Medicaid access upon release from jails and enrollment in insurance through ACA would benefit high-risk women leaving jails and provide them with opportunities for accessing covered cancer prevention services (Riedel et al., 2016), though those benefits are under immediate threat as a result of dramatic political changes in the U.S. (Jost, 2016). The payoff of efforts to expand care is that the unnecessary medical, family, social, and economic costs associated with a preventable cancer could be easily eliminated by ensuring that those most at risk get connected to the health care and cancer preventing technologies they need most.
Funding
All authors were supported by National Cancer Institute/National Institutes of Health, study R01CA181047, Sexual Health Empowerment for Cervical Health Literacy and Cancer Prevention, Principal Investigator, Megha Ramaswamy. The funding agency had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Conflicts
The authors have no conflicts of interest.
Transparency document
Transparency document.
Footnotes
The Transparency document associated with this article can be found, in the online version.
References
- Andrist L., MacPherson K. Conceptual models for women's health research: reclaiming menopause as an exemplar of nursing's contributions to feminist scholarship. Annu. Rev. Nurs. Res. 2001;19:29–60. [PubMed] [Google Scholar]
- Audet-LaPointe P. Detection of cervical cancer in a women's prison. Can. Med. Assoc. J. 1971;104:509–511. [PMC free article] [PubMed] [Google Scholar]
- Bayu H., Berhe Y., Mulat A., Alemu A. Cervical cancer screening service uptake and associated factors among age eligible women in Mekelle Zone, Northern Ethiopia, 2015: a community based study using Health Belief Model. PLoS One. 2016;11(3) doi: 10.1371/journal.pone.0149908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger I.A., White M.C., Pérez-Stable E.J., Goldenson J., Tulsky J.P. Cancer screening among jail in- mates: frequency, knowledge, and willingness. Am. J. Public Health. 2005;95(10):1781–1787. doi: 10.2105/AJPH.2004.052498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger I.A., Mueller S., Brendan Clark C., Cropsey K.L. Risk factors for cervical cancer in criminal justice settings. J. Women's Health. 2011;20:1839–1844. doi: 10.1089/jwh.2011.2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger I.A., Krueger P.M., Steiner J.F. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J. Epidemiol. Community Health. 2009;63(11):912–919. doi: 10.1136/jech.2009.090662. [DOI] [PubMed] [Google Scholar]
- Bourdieu P. Harvard University Press; Cambridge, MA: 1984. Distinction: A Social Critique of the Judgement of Taste. [Google Scholar]
- Bradley K.A., DeBenedetti A.F., Volk R.J., Williams E.C., Frank D., Kivlahan D.R. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007 Jul;31(7):1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Canal E. Defunding Planned Parenthood Would Put 900,000 Women's Lives at Risk Every Year. 2015. http://www.forbes.com/sites/emilycanal/2015/12/09/defunding-planned-parenthood-would-put-900000-womens-lives-at-risk-every-year/#65f6aad1b16d Retrieved from.
- Centers for Disease Control and Prevention Cancer Prevention and Control. 2017, March 8. https://www.cdc.gov/cancer/ Retrieved from.
- Centers for Disease Control and Prevention Cervical Cancer Statistics. 2016, June 20. https://www.cdc.gov/cancer/cervical/statistics/ Retrieved from.
- Clarke J., Phipps M., Rose J. Follow-up of abnormal Pap smears among incarcerated women. J. Correct. Health Care. 2007;13(1):22–26. [Google Scholar]
- Compton W.M., Grant B.F., Colliver J.D., Glantz M.D., Stinson F.S. Prevalence of marijuana disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Cooper R., Heldman C., Ackerman A.R., Farrar-Meyers V.A. Hidden corporate profits in the U.S. prison system: the unorthodox policy-making of the American Legislative Exchange Council. Contemp. Just. Rev. 2016;19(3):380–400. [Google Scholar]
- Eggleston K.S., Coker A.L., Das I.P., Cordray S.T., Luchok K.J. Understanding barriers for adherence to follow-up for abnormal Pap tests. J. Women's Health. 2007;16:311–330. doi: 10.1089/jwh.2006.0161. [DOI] [PubMed] [Google Scholar]
- Enders C.K. Guilford Press; New York, NY: 2010. Applied Missing Data Analysis. [Google Scholar]
- Fernandez M., Gonzales A., Tortolero-Luna G. Effectiveness of Cultivando La Salud: a breast and cervical cancer screening promotion program for low-income Hispanic women. Am. J. Public Health. 2009;99(5):936–943. doi: 10.2105/AJPH.2008.136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guvenc C., Akuz A., Acikel C.H. Health Belief Model scale for cervical cancer and Pap smear test: psychometric testing. J. Adv. Nurs. 2010;67(2):428–437. doi: 10.1111/j.1365-2648.2010.05450.x. [DOI] [PubMed] [Google Scholar]
- Herbst J.H., Branscomb-Burgess O., Gelaude D.J., Seth P., Parker S., Fogel C.I. Risk profiles of women experiencing initial and repeat incarcerations: implications for prevention programs. AIDS Educ. Prev. 2016;28(4):299–311. doi: 10.1521/aeap.2016.28.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogenmiller J.R., Atwood J.R., Lindsey A.M., Johnson D.R., Hertzog M., Scott J.C. Self-efficacy scale for Pap smear screening participation in sheltered women. Nurs. Res. 2007;56(6):369–377. doi: 10.1097/01.NNR.0000299848.21935.8d. [DOI] [PubMed] [Google Scholar]
- Hunter J.L. Cervical cancer educational pamphlets: do they miss the mark for Mexican immigrant women's needs? Cancer Control. 2005;12:42–50. doi: 10.1177/1073274805012004S07. Suppl. [DOI] [PubMed] [Google Scholar]
- Jost T. Health Affairs Blog. 2016, November 9. Day one and beyond: what Trump's election means for the ACA.http://healthaffairs.org/blog/2016/11/09/day-one-and-beyond-what-trumps-election-means-for-the-aca/ Retrieved from. [Google Scholar]
- Kaeble D., Glaze L.E., Tsoustis A., Minton T.D. Correctional Populations in the United States. 2015, December 29. Bureau of Justice Statistics.http://www.bjs.gov/index.cfm?ty=pbdetail&iid=5519 Retrieved from. [Google Scholar]
- Kelly P.J., Hunter J., Daily E.B., Ramaswamy M. Challenges to Pap smear follow-up among women in the criminal justice system. J. Community Health. 2017;42(1):15–20. doi: 10.1007/s10900-016-0225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh H.K., Sebelius K.G. Promoting prevention through the Affordable Care Act. N. Engl. J. Med. 2010;363(14):1296–1299. doi: 10.1056/NEJMp1008560. [DOI] [PubMed] [Google Scholar]
- Lindau S.T., Tomori C., Lyons T., Langseth L., Bennett C.L., Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am. J. Obstet. Gynecol. 2002;186(5):938–943. doi: 10.1067/mob.2002.122091. [DOI] [PubMed] [Google Scholar]
- Lindau S.T., Basu A., Leitsch S.A. Health literacy as a predictor of follow-up after an abnormal Pap smear: a prospective study. J. Gen. Intern. Med. 2006;21:829–834. doi: 10.1111/j.1525-1497.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee C.G., Hult J.R., Turalba R., McMillan S. Preventive care for women in prison: a qualitative community health assessment the Papanicolaou test and follow-up treatment at a California state women's prison. Am. J. Public Health. 2005;95:1712–1717. doi: 10.2105/AJPH.2005.063677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin R.E., Hislop T.G., Moravan V., Grams G.D., Calam B. Three-year follow-up study of women who participated in a cervical cancer screening intervention while in prison. Can. J. Public Health. 2008;99(4):262–266. doi: 10.1007/BF03403751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojica C.M., Morales-Campos D.Y., Carmona C.M., Ouyang Y., Liang Y. Breast, cervical, and colorectal cancer education and navigation: results of a community health worker intervention. Health Promot. Pract. 2016;17(3):353–363. doi: 10.1177/1524839915603362. [DOI] [PubMed] [Google Scholar]
- Nielsen-Bohlman L., Panzer A.M., Kindig D.A. National Academies Press; Washington, DC: 2004. Health Literacy: A Prescription to End Confusion. [PubMed] [Google Scholar]
- Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000;15(3):259–267. [Google Scholar]
- Ramaswamy M., Freudenberg N. Health promotion in jails and prisons: an alternative paradigm for correctional health services. In: Greifinger R., editor. Public Health is Public Safety: Improving Public Health Through Correctional Health Care. Springer Publishing Company; New York: 2007. [Google Scholar]
- Ramaswamy M., Kelly P.J. “The vagina is a very tricky little thing down there”: cervical health literacy among incarcerated women. J. Health Care Poor Underserved. 2015;26(4):1265–1285. doi: 10.1353/hpu.2015.0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaswamy M., Kelly P.J., Koblitz A., Kimminau K.S., Engelman K.K. Understanding the role of violence in incarcerated women's cervical cancer screening and history. Women Health. 2011;51(5):423–441. doi: 10.1080/03630242.2011.590875. [DOI] [PubMed] [Google Scholar]
- Ramaswamy M., Simmons R., Kelly P.J. The development of a brief jail-based cervical health promotion intervention. Health Promot. Pract. 2015;16(3):432–442. doi: 10.1177/1524839914541658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedel L.E., Barry C.L., McGinty E.E. Improving health care linkages for persons: the Cook County Jail Medicaid Enrollment Initiative. J. Correct. Health Care. 2016;22(3):189–199. doi: 10.1177/1078345816653199. [DOI] [PubMed] [Google Scholar]
- Scarinci I.C., Bandura L., Hidalgo B., Cherrington A. Development of a theory-based (PEN-3 and Health Belief Model), culturally relevant intervention on cervical cancer prevention among Latina immigrants using intervention mapping. Health Promot. Pract. 2012;13(1):29–40. doi: 10.1177/1524839910366416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherin K.M., Sinacore J.M., Li X.Q., Zitter R.E., Shakil A. HITS: A short domestic violence screening tool for use in a family practice setting. Fam. Med. 1998;30:508–512. [PubMed] [Google Scholar]
- von Wagner C., Semmler C., Good A., Wardle J. Health literacy and self-efficacy for participating in colorectal cancer screening: the role of information processing. Patient Educ. Couns. 2009;75(3):352–357. doi: 10.1016/j.pec.2009.03.015. [DOI] [PubMed] [Google Scholar]
- Walsh C., MacMillan H., Trocme N., Jamieson E., Boyle M. Measurement of victimization in adolescence; Development and validation of the Childhood Experiences of Violence Questionnaire. Child Abuse Negl. 2008;32:1037–1057. doi: 10.1016/j.chiabu.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Williams M., Moneyham L., Kempf M.C., Chamot, & E., Scarinci, I. Structural and sociocultural factors associated with cervical cancer screening among HIV-infected African American women in Alabama. AIDS Patient Care STDs. 2015;29(1):13–19. doi: 10.1089/apc.2014.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.