To the Editor
Critical pump failure in the era of continuous-flow left ventricular assist devices (CF-LVADs) is exceedingly rare.1,2 Complete pump stoppage after LVAD thrombosis can lead to rapid clinical decompensation and requires prompt intervention.3 In this presentation, we report the first percutaneous intervention to successfully deactivate an LVAD outflow graft after a Heartware HVAD (Heartware International, Framingham, Massachusetts) failure with the use of an Amplatzer Septal Occluder (St Jude Medical, St Paul, Minnesota).
Case Report
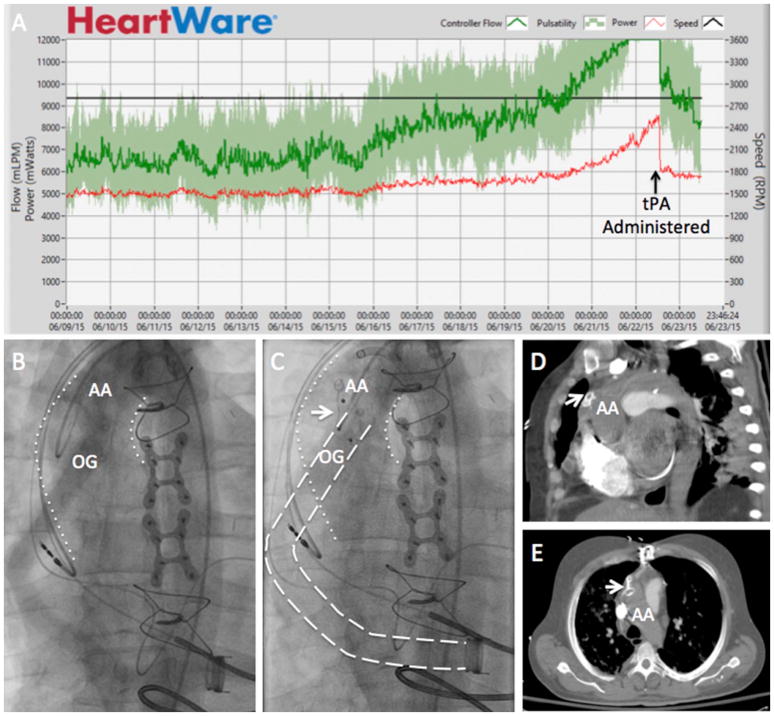
A 47-year-old man with ischemic cardiomyopathy (status: post–coronary artery bypass graft surgery) underwent implantation of a Heartware HVAD as destination therapy. Nine months after implantation, he presented with tenderness and induration over his lower sternum as well as with high flow and power alarms with the classic fingerprint of device thrombosis on his screen waveform and log file (Fig. 1A). He was found to have an elevated lactate dehydrogenase (LDH) level, and the clinical diagnosis of LVAD thrombosis was made. The patient was taken to the cardiac catheterization laboratory (CCL) for catheter-directed administration of tissue plasminogen activator, as previously described.4 The patient’s flow and power transiently improved, but his LDH continued to rise (Fig. 1A). Three days later, the patient’s LVAD began alarming with power spikes followed by complete pump stoppage. The patient was started on dobutamine for inotropic support. In the setting of medical noncompliance, hemorrhagic stroke, prior sternotomy, and active chest wall infection, he was thought to be a poor candidate for device exchange.
Fig. 1.
(A) Log file revealing rising power and flow suggestive of pump thrombosis before treatment with tissue plasminogen activator (tPA). (B) Fluoroscopy before closure of the left ventricular assist device (LVAD) outflow graft, showing retrograde flow from the ascending aorta (AA) to the outflow graft (OG). (C) Successful closure of the LVAD outflow graft with the use of a 14 mm Amplatzer Septal Occluder (arrow). Aortogram shows filling of the aorta but not the outflow graft. (D, E) Computerized tomography in (D) sagittal and (E) coronal views confirming appropriate Amplatzer deployment at the anastomosis of the outflow graft and ascending aorta (AA).
After extensive goals of care discussions, a multidisciplinary team arrived to a decision to take the patient to the CCL for percutaneous LVAD deactivation. Bilateral common femoral artery access was obtained. Aortography was performed with the use of power injection of contrast through a pigtail catheter to define the aorta and LVAD outflow graft anatomy (Fig. 1B). A 0.035 in. × 260 cm Advantage glidewire (Terumo, Somerset, New Jersey) was advanced through a 6-French Hockey Stick 2 (HS2) catheter (Medtronic, Minneapolis, Minnesota) and inserted in the distal portion of the LVAD outflow graft. The HS2 catheter was exchanged for a 0.035 in. × 135 cm Quick Cross catheter (Spectranetics, Colorado Springs, Colorado), and the glidewire was exchanged for a 0.035 in. × 260 cm Amplatz extra stiff wire (Cook, Bloomington, Indiana). Over the extra stiff wire, an 8-French Torque View catheter (St Jude Medical, St Paul, Minnesota) was advanced into the LVAD outflow graft. The known diameter of the LVAD outflow graft was 10 mm and to ensure complete occlusion with effacement of the ostium of the outflow graft, a 14-mm Amplatzer Septal Occluder was successfully deployed in the LVAD outflow graft at the level of anastomosis with the ascending aorta (Fig. 1C–E). Given the patient’s improved clinical stability after percutaneous deactivation, he was taken to the operating room for debridement of his chest wall abscess and transection of his driveline. The patient was discharged home 3 days later, off all anticoagulation, in a palliative care route, and free of the burden of his LVAD. At the time of writing, >8 months after HVAD deactivation, the patient remained free of inotropes and without any complications from his procedure.
Discussion
Although exceedingly rare in the era of durable CF-LVADs, catastrophic pump failure leading to LVAD stoppage requires prompt attention. Unlike pulsatile LVADs, CF-LVADs do not have valves, and therefore retrograde flow is an important concern in the event of pump failure and can lead to elevated left-sided filling pressures and reduced end-organ perfusion.3 Additionally, stasis of flow promotes thrombus formation in the outflow graft that can serve as a source of distal embolization. Although complete thrombosis of the outflow graft may eventually eliminate retrograde flow, this process is not instantaneous, and patients can clinically decompensate in the interim. Percutaneous closure of the LVAD outflow graft is an intriguing option to stabilize patients or for patients who are not surgical candidates for exchange. Transient stabilization with the use of a 14–16-mm peripheral balloon inflated in the outflow graft has been reported.5 Catheter-based device deactivation of the LVAD outflow graft has been reported in a patient with a Heartmate II (Thoratec Corp, Pleasanton, California) with myocardial recovery who did not wish to undergo a repeated sternotomy for device explantation.6 Our case report is the 1st report of minimally invasive closure of the LVAD outflow graft after pump failure. It is also the 1st report of percutaneous closure of a Heartware HVAD outflow graft. Percutaneous closure of the LVAD outflow graft may allow for rapid and durable correction of retrograde outflow graft flow and can also be used to deactivate the LVAD in inoperable patients.
Footnotes
Disclosures
Atman P. Shah has served as a consultant and proctor for St Jude Medical. Nir Uriel is a consultant for Heartware International and Thoratec (St Jude Medical). Valluvan Jeevanandam is a consultant for Thoratec (St Jude Medical). The other authors report no potential conflicts of interest.
References
- 1.Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, et al. Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) Study Group. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001;345:1435–43. doi: 10.1056/NEJMoa012175. [DOI] [PubMed] [Google Scholar]
- 2.Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson LW, Blume ED, et al. Sixth INTERMACS annual report: a 10,000-patient database. J Heart Lung Transplant. 2014;33:555–64. doi: 10.1016/j.healun.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Giridharan GA, Koenig SC, Soucy KG, Choi Y, Pirbodaghi T, Bartoli CR, et al. Hemodynamic changes and retrograde flow in lvad failure. ASAIO J. 2015;61:282–91. doi: 10.1097/MAT.0000000000000200. [DOI] [PubMed] [Google Scholar]
- 4.Thenappan T, Anderson AS, Jeevanadham V, Rich JD, Shah AP. Treatment of left ventricular assist device thrombosis with extended catheter-directed intraventricular thrombolytic therapy. Circ Heart Fail. 2013;6:e27–9. doi: 10.1161/CIRCHEARTFAILURE.113.000013. [DOI] [PubMed] [Google Scholar]
- 5.Chrysant GS, Horstmanshof DA, Snyder T, Chaffin JS, Elkins CC, Kanaly PJ, et al. Successful percutaneous management of acute left ventricular assist device stoppage. ASAIO J. 2010;56:483–5. doi: 10.1097/MAT.0b013e3181ed937f. [DOI] [PubMed] [Google Scholar]
- 6.Zeigler SM, Sheikh AY, Lee PH, Desai J, Banerjee D, Oyer P, et al. A novel, catheter-based approach to left ventricular assist device deactivation after myocardial recovery. Ann Thorac Surg. 2014;98:710–3. doi: 10.1016/j.athoracsur.2013.09.073. [DOI] [PubMed] [Google Scholar]