Abstract
Background: Yoga has been found to be an effective posttraumatic stress disorder (PTSD) treatment for a variety of trauma survivors, including females with chronic PTSD.
Aim/Purpose: The current study builds on extant research by examining an extended trauma-sensitive yoga treatment for women with chronic PTSD. The study sought to optimize the results of a treatment protocol examined in a recent randomized controlled trial with a shorter duration and without assignment or monitoring of home practice.
Materials and Methods: The authors examined a 20-week trauma-sensitive yoga treatment in a non-randomized single-group treatment feasibility study for women with chronic treatment-resistant PTSD (N = 9). The authors examined PTSD and dissociation symptom reduction over several assessment periods.
Results: The results indicate that participants experienced significant reductions in PTSD and dissociative symptomatology above and beyond similar treatments of a shorter duration.
Conclusions: The findings suggest that more intensive trauma-sensitive yoga treatment characterized by longer duration and intentional assignment and monitoring of home practice may be more advantageous for individuals with severe and chronic PTSD. The implications of the findings for the potentially more substantial role of yoga as an intervention for a subset of adults with chronic treatment-resistant PTSD are discussed.
Keywords: : PTSD, yoga, chronic PTSD, PTSD treatment
Introduction
Yoga is among the most widely used complementary healthcare practices in the United States1 and has been found to be promising for the treatment of a variety of mental and physical health problems, including posttraumatic stress disorder (PTSD).2,3 Yoga is hypothesized to be helpful for individuals with PTSD because the mindfulness it fosters can lead to increased emotion regulation, as noticing fear-related sensations can counteract avoidance symptoms.4 Individuals with PTSD also show impaired awareness of bodily sensations and a lack of cognizance of the connection between environmental stimuli and internal reactions5,6—two areas that are addressed in yoga.7
Research indicates that time-limited yoga treatment (i.e., lasting ≤10 weeks) may be effective for treating PTSD and related symptoms in tsunami survivors,8 veterans,9,10 military personnel,11 and survivors of intimate partner violence.12 Case studies also suggest that yoga may be helpful for traumatized youth in residential care.13 In addition, yoga treatments have been specifically designed for trauma survivors.7,14,15 While some research has failed to find a significant difference between yoga treatment and control conditions,16 a notable randomized controlled trial (RCT) indicated that adult participants with PTSD who completed an eight-session Kundalini yoga treatment exhibited significant improvement in PTSD symptomatology and greater changes in perceived stress, anxiety, and resilience compared with the control group.17 In addition, a study of yoga for military personnel with PTSD suggested that participants exhibited reductions in PTSD symptoms, and that treatment effects were visibly higher than a waitlist control benchmark derived from a meta-analysis of treatment studies for military personnel with PTSD.11
Van der Kolk et al. recently tested the efficacy of a 10-week Trauma Center Trauma-Sensitive Yoga (TCTSY) program in a RCT with a sample of 64 women with chronic treatment-resistant PTSD.18 Results indicated that compared with women who completed women's health education classes, participants who completed yoga were more likely no longer to meet the criteria for PTSD and exhibited significant decreases in tension and depression. The effect size for reductions in PTSD for the yoga treatment (d = 1.07, p < 0.001) was comparable to other effective and well-researched treatments.19 While these initial findings are promising, research in this area is relatively new, and factors influencing the impact of TCTSY on trauma survivors (e.g., duration and frequency of practice) have not been empirically investigated.
Duration and frequency of yoga practice
Duration of yoga practice (i.e., weeks or months of total practice) has been shown to be associated with a variety of positive outcomes, including lower depression,a lower levels of inflammatory hormones,20 and wellness.b In contrast, some researchers have failed to find a significant relationship between practice duration and body awareness, body satisfaction, stress, and relaxation.21,22 These contradictory findings suggest that further research is needed to elucidate the mechanisms by which yoga produces positive mental health outcomes.
The frequency of yoga practice has been shown to be positively related to mental and physical health outcomes. For instance, in a sample of primarily female abuse survivors, Dale et al. found that frequency of yoga practice was positively related to self-concept, even after controlling for the effects of trauma history.23 In a sample of veterans who suspected that they had PTSD, frequency of yoga practice was negatively related to PTSD symptomatology.c Similarly, in samples of healthy yoga-practicing adults, practice frequency has been found to be positively associated with positive psychological attitudes, vitality,d good health,24 relaxation,22 and anti-inflammatory hormones (i.e., health-enhancing hormones).20 Yoga practice frequency has also been found to be negatively associated with stress,22 self-objectification,21 and inflammatory hormones (i.e., hormones related to diabetes and other physical and mental health problems).20 Some research suggests that the addition of home practice,23 as well as the frequency of home practice, are associated with increased benefits from yoga.24
Duration and homework adherence in PTSD treatment
Results from studies of empirically supported treatments for PTSD suggest that between 20% and 50% of participants continue to meet diagnostic criteria for PTSD after a course of psychotherapy.19,25 However, closer examination of these results indicates that most participants exhibit significant decreases in PTSD symptomatology, suggesting a variable rate of treatment response across individuals with PTSD.26 For example, studies examining cognitive processing therapy (CPT) suggest that the duration of treatment (i.e., the number of treatment sessions) impacts clinical indicators. For example, Chard lengthened the standard 12-session CPT protocol to 17 sessions and found that that only 7% of the participants continued to meet PTSD criteria after treatment completion.27 In addition, Galovski et al. adjusted standard CPT treatment such that termination occurred whenever participants made sufficient treatment gains (i.e., end-state criteria was defined as clinically non-significant depression and PTSD symptoms).26 The results suggested that the majority of participants met end-state criteria prior to or at the 12th session, while approximately a quarter of the sample made sufficient gains by session 18. Importantly, the number of sessions needed to make sufficient treatment gains was predicted by baseline depression and time since trauma but not by baseline PTSD. In sum, findings from Chard and from Galovski et al. suggest that treatment responsiveness in relation to treatment duration is variable and that individuals with more significant symptomatology may respond better to longer-term treatment.
Research also suggests that homework adherence is related to treatment outcomes. A recent meta-analysis suggests that homework adherence is a small yet significant predictor of treatment outcomes across anxiety disorders.28 However, the significance of homework adherence as a predictor of PTSD treatment response varies across studies.29,30 Interestingly, Bluett et al. examined the efficacy of prolonged exposure (PE) for chronic PTSD and found that the degree to which patients perceived homework to be helpful, rather than amount completed, was related to distress reduction.31 Taken together, these studies suggest that the degree to which treatment components are practiced (i.e., homework) outside of treatment sessions, as well as treatment session frequency, may be related to treatment outcomes, though results are inconsistent.
Current study
The present study built on van der Kolk et al.'s RCT by examining the effectiveness of an extended TCTSY treatment for PTSD with a non-randomized sample of women with chronic PTSD.18 Specifically, the current research examined the effectiveness of the same yoga treatment (i.e., TCTSY delivered by the same teachers and in the same setting) that involved twice the number of sessions (once per week over 20 weeks) and yoga practice at home (i.e., homework) that was highly monitored. An examination of more intensive TCTSY treatment characterized by longer duration and more intentional monitoring of home practice allowed for an assessment of the maximum yield of PTSD symptom reduction for individuals treated with TCTSY. Finally, van der Kolk et al. found a non-significant reduction in dissociative symptoms.18 Given the increased mindfulness, somatic awareness, and body acceptance thought to result from TCTSY, it was possible that women in the present study would also experience reductions in dissociative symptoms. Thus, it was hypothesized that (1) participants would exhibit significant decreases in PTSD symptoms, (2) women would experience significant reductions in dissociative symptomatology, (3) most women would no longer meet diagnostic criteria for PTSD at treatment completion, and (4) participants would exhibit more robust decreases in PTSD compared with women who completed the 10-week treatment.
Materials and Methods
Participants
Nine women participated in the study, and six completed treatment. Participants were aged between 25 and 55 years (M = 40.7 years) and were primarily white (n = 5), followed by black (n = 2), Asian (n = 1), and Latina (n = 1). Participants in the current study were assessed using the same inclusion and exclusion criteria as the primary RCT.18 These women met the DSM-IV criteria for PTSD as measured by the Clinician Administered PTSD Scale (CAPS). Participants also had to meet a PTSD diagnosis based on the Frequency >1/Intensity ≥2 (F1/I2), Total Severity ≥45 (TSEV45), and Item Severity ≥4 (ISEV4) CAPS scoring rules.32 As in the primary RCT, participants were deemed to have treatment unresponsive, chronic PTSD as defined by the occurrence of an index trauma at least 12 years prior to intake combined with the continued presence of PTSD diagnosis following completion of at least 3 years of therapy focused on the treatment of PTSD. Participants were required to remain in ongoing supportive psychotherapy, as well as any pre-existing pharmacological treatment, for the duration of the study. Participants were engaged in different modalities of supportive therapy at a variety of mental health agencies and were not required to inform their therapists about their involvement in the study. However, participants provided investigators with signed releases of information allowing researchers to contact them in the case of an emergency. Exclusionary criteria included alcohol or substance abuse/dependence in the last 6 months, pregnancy or breastfeeding, unstable medication, or active suicide risk or life-threatening self-mutilation. Participants were also excluded if they had participated in five or more yoga sessions in the past or if they had a Global Assessment of Functioning (GAF) score <40.33 Of the 22 women who were assessed, 10 were excluded because they did not meet inclusion criteria or had scheduling problems. Of those who were enrolled in the study, three women dropped out of the study before treatment began, and three dropped out in the middle of treatment.
Measures
The current study utilized the CAPS and Davidson Trauma Scale for PTSD (DTS) to measure PTSD.34,35 The CAPS was administered by a master's or doctoral-level clinician. It is a widely used structured interview assessment used to diagnose and measure PTSD symptomatology.34 The CAPS has exhibited strong psychometric properties in a variety of research and clinical populations.36 Internal consistency has been established as good (α = 0.87 for each subscale; 0.94 for total score), and scales correlate highly with other measures of PTSD (Minnesota Multiphasic Personality Inventory [MMPI-2 PTSD] subscale, r = 0.77; Mississippi PTSD Scale, r = 0.91; Structured Clinical Interview for DSM-IV [SCID PTSD] scale, r = 0.89).34 Additionally, inter-rater reliability for severity and frequency has been found to be excellent for avoidance, arousal, and intrusion subscales (r > 0.92).34 The DTS is a self-report measure that assesses severity and frequency of DSM-IV PTSD symptoms within the past week. This measure has evidenced strong reliability and validity across trauma-exposed populations.35 Scores from the Dissociative Experiences Scale (DES)37 were also examined. The DES is a self-report measure of dissociation that has exhibited strong reliability and validity across a variety of samples.37–40 The recommended clinical cutoff score is 15 or 20 for determining clinically significant dissociation.41 A measure of homework compliance was also collected weekly. The homework log asked participants to provide information about the frequency (days of the week) and duration (number of minutes of practice per day) of practice, as well as the type of practice (e.g., using a DVD or CD, or attending a class at a gym or yoga studio).
Procedures
Recruitment and assessment
All study procedures were approved by the Institutional Review Board. Participants were recruited from the community and completed an initial phone screen that included questions about study eligibility and interest in study participation. Women who participated in the study were assessed at seven time points: 1 month before the onset of treatment (time 1), 1 week before treatment (time 2; pretreatment), week 5 of treatment (time 3), in the middle of treatment (time 4), week 15 of treatment (time 5), 1 week after treatment (time 6; post-treatment), and 2 months after treatment (time 7; follow-up). The CAPS and DES were administered at five time points (CAPS: times 1, 2, 4, 6, and 7; DES: times 1, 3, 4, 6, and 7), and the DTS was administered at six time points (times 2–7).
Treatment
Between pre- and post-assessments, women completed a 20-week trauma-informed hatha yoga treatment. The program consisted of weekly, hour-long, instructor-led yoga classes. In addition to attending weekly TCTSY sessions, participants were asked to complete home-practice using a TCTSY DVD or CD as a guide. It was recommended that participants practice at home for 30 min three times per week. A research assistant contacted the women weekly by phone to remind them of upcoming classes and to complete their home-practice assignments. In addition, homework logs (described in Measures) were collected at every class session.
Classes were taught by a registered yoga teacher with specialized training in TCTSY, as well as a licensed mental health counselor. The classes were developed to create safety and predictability for the participants to facilitate better the practice of making choices in their bodies based on what they felt in the moment. Safety was created in the environment by setting up mats in the same design each week, covering windows for privacy, accounting for the location of exits when setting up the classes, and using lighting that was bright enough for students to see easily around the room. The instructor practiced the yoga forms with the students, rarely leaving her mat and never giving any physical assistance. Yoga forms were virtually the same week-to-week in order to provide predictability and to give participants the chance to explore making choices in their bodies. Although participants were encouraged to ask the instructor questions or give feedback before or after class, they were asked to maintain quiet during the class. Processing of trauma histories or the group experience was discouraged.
Each weekly class began with a brief invitation for participants to focus their attention on the present moment and to practice making choices in their body based on what they were feeling on that particular day. During sessions 2–10, the yoga instructor introduced one of the themes of TCTSY (e.g., being in the present moment; see Appendix for a more detailed protocol). Students were invited to interact with the given theme as they moved through the yoga class. Each session included seated, standing, and mat-based/floor forms, each of which lasted approximately 15–18 min. All sessions ended with a rest period between 3 and 5 min.
For the first 10 weeks, students began their yoga practice with 15–18 min of chair yoga that included seated mountain, neck circles, twists, breath awareness, and synchronizing breath and movement. Students were then invited to practice standing forms for another 15–18 min, including standing mountain, warrior one and two, tree, and sun breath. Subsequently, students were invited to move to the mat where a series of forms were practiced seated or on their stomach, including cobra, table, downward dog, and seated forward folds. The class concluded with a 15–18 min of floor forms, including twisting, bridge, knee-to-chest, and a hip stretch. Students were then invited to take a few moments to rest their bodies and to interact with stillness and silence for 3 min. The facilitator offered a range of choices to enhance comfort during this time, including giving participants the option to move to seated, or to lie on their back or on their side. Classes ended with a brief centering practice during which participants were offered the opportunity to notice if there were any changes in their body after practicing yoga.
After week 10, sessions remained mostly the same. However, several participants asked not to begin seated in the chair, and instead began to practice in a seated position on the mat. In addition, 2 min of rest were added to the end of class (i.e., sessions 11–20 included a 5-min rest period). Supplemental information about the yoga practice utilized in the current study is available in Weste and two books on TCTSY.7,42
Data analysis
Descriptive statistical analyses were performed to examine the range of scores on the CAPS, DTS, and DES. CAPS scores were also examined to determine the degree of symptom reduction in subsamples of completers and early completers (i.e., individuals who chose to stop treatment before the final session). The present study utilized a longitudinal data analysis (LDA) technique known as hierarchical linear modeling (HLM) using the linear and nonlinear modeling software program (HLM7).43 HLM is widely considered to be one of the best analytic tools for describing developmental patterns and identifying predictors of change.44 HLM is used to describe intra-individual developmental patterns and identify inter-individual predictors of developmental patterns.45 HLM allows one to model the slope and intercept for each individual participant. In other words, one can observe both the initial level of the outcome at the outset of the study (i.e., the intercept) and the degree of change in the outcome over time (i.e., the slope).46 HLM can also be used when data are ignorably missing, which eliminates the need to delete individuals with missing data, including those with missing data for entire waves.44,45 Notably, this allows for the inclusion of participants who did not complete treatment (i.e., early completers), and in the present study, women who completed the study did not have any missing data on the CAPS or DTS. Despite the relatively small sample, HLM is on the list of recommendations of the Institute of Medicine's guidelines to maximize information from small clinical trials in order to obtain reliable and valid results, and the inclusion of several assessments helps attenuate the limitations of a small sample.47 A series of unconditional models (i.e., examining change over time without any predictors) were run to identify the change model that best fit the data. The models that were evaluated were: (a) linear change with time modeled as the number of assessment with the first occasion coded as 0 and each subsequent occasion increasing by one, (b) quadratic change modeled using two time variables, the linear time variable plus a quadratic time variable that was computed by squaring the linear time variable, and (c) natural log change with time modeled as the natural log of the assessment occasion. All time effects were modeled as random effects. Because the CAPS was measured twice before the start of treatment, piecewise growth modeling was conducted, which parsed the overall trajectory into the baseline period (1 month pre-assessment to 1 week pre-assessment) and treatment response (1 week pretreatment through the follow-up assessment).45
Results
Table 1 depicts descriptive statistics for the CAPS, DTS, and DES. Treatment completers exhibited a clinically significant reduction in PTSD symptoms (defined as a 30% reduction in CAPS mean score48,49), as evidenced by a 45% reduction in raw mean CAPS score between pretreatment (i.e., 1 week pretreatment) and 2-month follow-up. Importantly, at the midpoint assessment, treatment completers evidenced a 25% drop in mean CAPS, while early completers' CAPS scores were 54% lower than baseline. The overall sample exhibited a 36% drop in CAPS at the midpoint assessment. Additionally, all but one of the completers (83%) no longer met the criteria for a PTSD diagnosis 1 week after treatment ended, and two achieved asymptomatic status (i.e., CAPS score <22).32 At the 2-month follow-up, 4/6 (67%) women did not meet the diagnostic criteria for PTSD (i.e., four women no longer met the criteria for PTSD at follow-up, and one of those women was asymptomatic). Finally, none of the early completers was asymptomatic at any point in treatment, though two of them no longer met the diagnostic criteria at week 10 of treatment. With respect to dissociation, results suggest that treatment completers experienced a 47% drop in DES between the 1-month pretreatment assessment and the 2-month follow-up assessment based on raw scores, while early completers exhibited a 39% decrease at the midpoint assessment. In van der Kolk et al.'s study, participants exhibited a 35% reduction in dissociative symptoms from pre- to post-treatment. Notably, participants in the present study exhibited a wide range of dissociative symptomatology across study participation. At baseline, 4/6 treatment completers and 1/3 early completers had clinically significant dissociation (DES score >15). At follow-up, only one woman had clinically significant dissociation, and the same early completer maintained a clinically significant DES score.
Table 1.
Descriptive Statistics
| Measure | Sample | Estimate | Raw/estimated | Time 1 (1 month pretreatment) | Time 2 (1 week pretreatment) | Time 3 (treatment week 5) | Time 4 (week 10/midpoint) | Time 5 (treatment week 15) | Time 6 (1 week post-treatment) | Time 7 (2-month follow-up) |
|---|---|---|---|---|---|---|---|---|---|---|
| CAPS | ITT | n | 9 | 9 | 9 | 6 | 6 | |||
| N = 9 | M (SD) | Raw | 72.89 (16.06) | 68.89 (18.50) | 44.00 (23.97) | 35.33 (21.71) | 35.50 (20.77) | |||
| N = 9 | M (SD) | Estimated | 72.89 (15.14) | 67.49 (18.17) | 45.95 (16.69) | 33.36 (19.92) | 24.42 (23.37) | |||
| DTS | ITT | n | 9 | 8 | 9 | 7 | 7 | 6 | ||
| N = 9 | M (SD) | Raw | 64.00 (27.01) | 46.88 (23.55) | 35.56 (25.42) | 31.36 (29.12) | 23.00 (14.93) | 29.88 (18.85) | ||
| N = 9 | M (SD) | Estimated | 64.82 (26.46) | 46.72 (22.38) | 34.61 (24.54) | 28.48 (25.67) | 28.33 (23.56) | 34.17 (19.96) | ||
| DES | ITT | n | 9 | 8 | 9 | 7 | 6 | |||
| N = 9 | M (SD) | Raw | 15.8 (6.49) | 12.58 (5.63) | 8.41 (6.71) | 8.92 (6.95) | 8.99 (7.29) | |||
| N = 9 | M (SD) | Estimated | 15.52 (5.97) | 11.59 (6.36) | 9.26 (6.83) | 7.61 (7.24) | 6.35 (7.59) | |||
SD, standard deviation; ITT, intention to treat; CAPS, Clinician Administered PTSD Scale, administered at T1, T2, T4, T6, and T7; DTS, Davidson Trauma Scale, administered at T2–T7; DES, Dissociative Experiences Scale, administered at T1, T3, T4, T6, and T7; raw, mean calculated at each assessment separately using all available data at that time point; estimated, estimates derived from the multilevel regression equation, which includes all data points available at all time points.
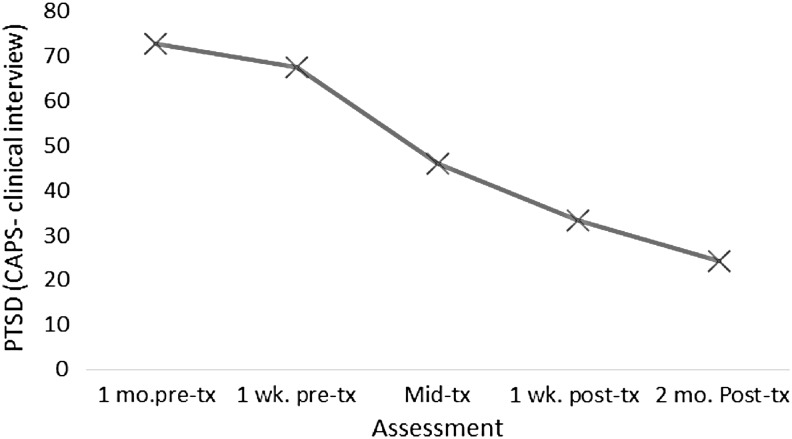
The HLM analysis examining the CAPS as the outcome variable suggested that the natural log piecewise change model fit the data best, with change during the baseline period (btime = −7.78, 95% confidence interval [CI] 1.98 to −17.55, p = 0.157) that was not statistically significant followed by substantial reductions during the treatment response period (btime = −31.06, 95% CI −19.16 to −42,97, p < 0.001) that was characterized by larger decreases across earlier assessments that become more shallow across time (see Fig. 1). The effect size estimate for the change from the 1 week pretreatment to the last assessment was d = −3.02 (95% CI −1.86 to −4.18), indicating a very large decrease in symptoms that is larger than the effect size of −1.07 for the sample who completed treatment in 10 weeks.18
FIG. 1.
Change in Clinician Administered PTSD Scale (CAPS). Estimates derived from the piecewise growth curve model conducted to evaluate change in CAPS. x-Axis: assessment; y-axis: PTSD (CAPS—clinical interview). PTSD, posttraumatic stress disorder.
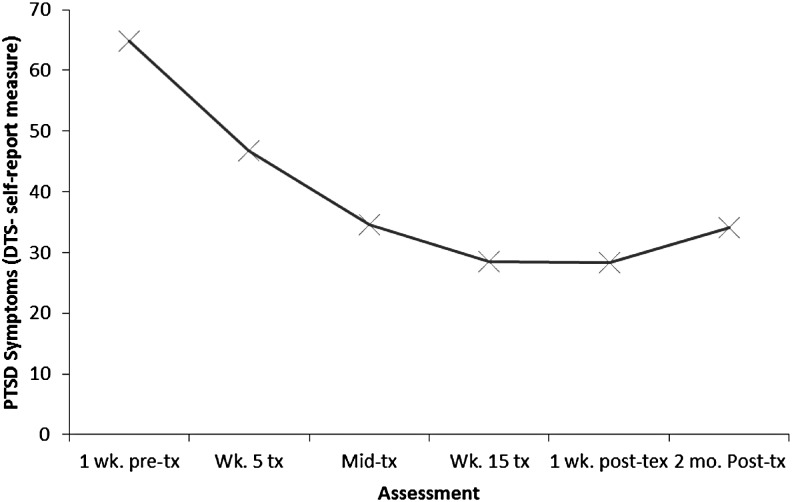
Results from the analyses examining the DTS as the outcomes suggest that the quadratic change model fit the data best, with statistically significant linear and quadratic change coefficients (blinear time = −21.08, 95% CI −8.88 to −33.27, p < 0.02; bquadratic time = 2.99, 95% CI 0.99 to 4.97, p < 0.020). As depicted in Figure 2, this pattern of change was associated with large decreases that decelerated over time, with a very slight increase in symptoms during the follow-up period. The effect size estimates indicated a large size decrease from pretreatment to 15 weeks (d = −1.23). Although there was a slight increase between week 15 and 2 months post-treatment, the pretreatment to 2-month follow-up decrease was still large (d = −1.04).
FIG. 2.
Change in Davidson Trauma Scale (DTS). Estimates derived from the hierarchical linear modeling (HLM) analysis conducted to evaluate change in DTS. x-Axis: assessment; y-axis: PTSD (DTS—self-report).
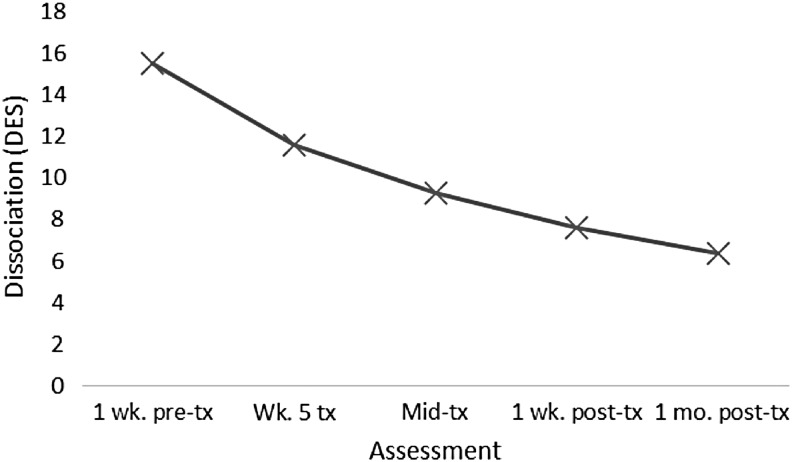
The HLM analysis examining the DES as the outcome variable suggested that the natural log change model fit the data best, with a statistically significant linear change coefficient (btime = −5.69, 95% CI −3.73 to −7.44, p < 0.001), indicating statistically significant decreases. The effect size estimate indicated a large size decrease from pretreatment to 15 weeks (d = −1.41; see Fig. 3).
FIG. 3.
Change in dissociation. Estimates derived from the HLM analysis conducted to evaluate change in Dissociative Experiences Scale (DES). x-Axis: assessment; y-axis: dissociation (DES).
To compare the 10-week treatment18 and 20-week treatment study outcomes, the projected percent drop and associated confidence intervals for the CAPS, DES, and DTS were examined (see Table 2). The percent drops for CAPS and DES in the 10-week treatment study were less than the lower threshold of the 95% CI of the 20-week treatment study reported in the present paper. Estimated mean scores based on these models are also presented in Table 1. These estimates suggest that the overall sample evidenced a 64% reduction in mean CAPS scores between pretreatment (1 week before treatment began) and 2-month follow-up assessments, a 47.4% drop in mean DTS score, and a 59% reduction in mean DES scores between the 1-month pretreatment and the 2-month follow-up assessments.
Table 2.
Percent Drop and Confidence Intervals
| 10-week treatment study pretreatment–post-treatmenta | 20-week treatment (current study) pretreatment–post-treatmentb | 20-week treatment (current study) pretreatment–2-month follow-upc | |
|---|---|---|---|
| PTSD (CAPS) | 33.1% (22%, 44.2%) | 50.6% (43.4%, 69.8%) | 63.8% (39.5%, 88.5%) |
| Dissociation (DES) | 16.0% (–0.6%, 32.6%) | 59.1% (38.7%, 74.9%) | |
| PTSD (DTS)* | 21.0% | 56.3% | 47.4% |
For both studies, DTS was modeled using linear and time coefficients. Therefore, 95% confidence intervals could not be calculated.
Percentage drop for all outcomes measured between 1 week pretreatment and post-treatment (week 10) assessments; 10-week study did not complete follow-up assessments.
Percentage drop for CAPS and DTS measured between 1 week pretreatment and 1 week post-treatment assessments; percentage drop for DES not available in this time frame.
Percentage drop for CAPS and DTS measured between 1 week pretreatment and 2-month follow-up assessments; percentage drop for DES measured between 1 month pretreatment and 2-month follow-up assessments.
Discussion
The current study examined the effectiveness of an extended 20-week TCTSY treatment by examining its impact on PTSD symptomatology in a sample of women with chronic and treatment-resistant PTSD. Unlike previously studied yoga treatments, the yoga offered in the current study was of a long duration and involved highly monitored at-home yoga practice. Results suggest that the current sample experienced significant PTSD and dissociation symptom reduction based on self-report and clinical interview data. Importantly, improvement in the current study was above and beyond that of a 10-week TCTSY in a similar sample examined in a RCT by van der Kolk et al.18 Specifically, 83% (n = 5) of treatment completers no longer met the criteria for PTSD 1 week after treatment ended, while only 52% of women in the trial of 10-week TCTSY lost their diagnosis. In addition, the overall sample experienced a 51% reduction in PTSD symptoms at the 1-week post-treatment assessment, while participants in van der Kolk et al. only exhibited a 33% reduction. While data limitations preclude an assessment of a statistically significant change between post-treatment and follow-up assessments, it is important to note that women in the current study exhibited a 64% reduction in PTSD at the 2-month follow-up, suggesting that they continued to improve after treatment completion. As such, it appears that longer-term treatment is more advantageous for women with severe and chronic PTSD. These findings are consistent with previous research on yoga, suggesting that longer duration of practice (i.e., weeks of practice) is associated with a variety of positive physical and mental health outcomes.20,f Research on evidence-based PTSD treatment (e.g., PE) also suggests that longer-term treatment is more beneficial for some individuals with PTSD.26,27 The variability in necessary treatment duration is consistent with current study findings wherein three women elected to discontinue treatment at the 10-week interval after experiencing a 59% decrease in PTSD symptoms as measured by the CAPS. Finally, it is possible that the robust findings in the current study reflect the maximum benefit of TCTSY for female civilian trauma survivors who are open to yoga treatment. Given the chronic natures of the PTSD experienced by the women in this study, it is possible that yoga may serve as a primary vehicle for PTSD resolution for some individuals. Based on the examination of effect sizes, participants in the current study experienced similar or higher levels of symptom reduction compared to other trauma-focused treatments (e.g., EMDR, PE, cognitive processing therapy),50,51 making this one of the first studies of a non-trauma-focused intervention that evidences symptom improvement comparable to that of evidence-based trauma-focused treatments.
The significant effects of yoga on PTSD symptomatology in the current study are particularly noteworthy given the significant level and range of distress experienced by many women in the present sample (see Table 1). The present sample included women who experienced clinically significant dissociation, an experience that is typically predictive of poor treatment outcomes.52 This suggests that TCTSY may be more tolerable for women with high levels of dissociation. Importantly, women in the present sample experienced significant reductions in dissociation, while participants in the shorter-term yoga treatment study did not experience significant improvement.18 As such, it may be that longer-term treatment is more beneficial for women with dissociative symptoms. The current study results also suggest that women who self-select to receive yoga have high expectations for its effectiveness, which is congruent with other research indicating that expectancies are related to outcome.53 Given the self-selected nature of the current sample, it is also possible that women's intentionality for behavior change (i.e., attending yoga classes, practicing yoga outside of class) affected outcomes above and beyond practice duration and frequency.54 Such findings suggest that trauma survivors may greatly benefit from being referred to TCTSY classes.
Limitations and future directions
It is hypothesized that the impressive symptom reductions documented in the current study, which were larger than previously published studies, were due to the long duration of yoga treatment and the increased home practice promoted by the current intervention. However, several methodological limitations prevent the role of homework and frequency of practice from being adequately testing with the current data. First, the frequency and number of yoga sessions, as well as the amount of home practice, was not experimentally manipulated. In this context, there are numerous potentially confounding variables that are likely to be associated with both amount of practice and treatment outcome. Second, the small sample size precluded these potential confounds from being investigating and accounting for, rendering any associations that might emerge with practice amount or frequency ambiguous as best. Future research that systematically varies amount of home practice, as well as frequency and number of yoga sessions, via experimental manipulation are needed to explore fully the impact of these variables in an unambiguous manner. While the present study did not have an adequate sample size to investigate between-subjects effects, the sample size was sufficient to document statistically significant and large decreases in symptoms, as the power to detect these effects benefited from the multiple assessments. Finally, though the sample in the current study was distinguished due to its wide symptom and severity representation, future studies would benefit from analyzing a similar treatment protocol with a larger and more diverse sample to examine the generalizability of the present results.
Conclusions
The original RCT18 provided concrete empirical support for the utility of TCTSY as an auxiliary component of “phase one intervention” (i.e., regulation and stabilization based treatment) for adult trauma survivors with chronic, treatment-resistant PTSD. Van der Kolk et al. found clinically significant but modest reductions in PTSD symptoms for participants randomized to the yoga protocol. Results from the present study revealed that participants achieved more substantial reductions in PTSD severity, including loss of diagnosis and attainment of asymptomatic status, as well as clinically significant decreases in dissociation symptoms at levels comparable to those established for bona fide trauma-focused psychotherapies (e.g., measured by treatment effect sizes).55
In both studies, participants presented with chronic treatment-resistant PTSD, despite index traumas at least 12 years prior to intake and receipt of at least 3 years of psychotherapy. While clinically significant but overall modest treatment gains were observed from a brief yoga protocol in the RCT, the current non-randomized sample evidenced reductions in PTSD that were notably more robust. In addition, the current study's effect sizes were comparable to those often observed in studies of bona fide trauma-focused interventions. This raises the question of whether TCTSY plays a more prominent role in the treatment of adult trauma survivors exhibiting chronic-treatment resistant PTSD.
While verification of this plausible conclusion requires further study, its practical implications are noteworthy. First, it suggests the potential for more widespread, cost-effective dissemination of effective interventions and community practice, as TCTSY is designed to be delivered in a group format by certified yoga instructors who are not required to be licensed psychotherapists, though they must receive extensive training and supervision in trauma theory and its role in TCTSY. Second, it offers a compelling alternative approach to symptom resolution for the subset of chronic trauma survivors who are uncomfortable with, unwilling to engage in, or have responded negatively to other trauma-focused interventions predicated around recollection, communication, and processing of traumatic memories and narratives. In conclusion, despite its limitations in sample composition, this study has generated intriguing data that, if replicated within a more controlled study design, could challenge long-held assumptions about the essential components of intervention necessary resolve symptoms of traumatic stress and associated conditions.
Vignette.
Many women in this study described yoga as an empowering practice due to feeling more regulated and in touch with their bodies. Ms. S., a 42-year-old Latina married social worker, had been physically and sexually abused by her father from middle school through late high school. She entered the study after 5 years of trauma-focused talk therapy and had a CAPS score of 60 and a DES score of 10 at the baseline assessment. During the course of the study, she attended 16/20 yoga classes and practiced an average of 43 min per day at home, even practicing while away on vacation. She mentioned that her husband commented on her “Zen-like” ability to maintain focus during her yoga practice. Ms. S. was able to use this skill in other aspects of her life, as she indicated in a note on her homework sheet: “The yoga has helped me be able to pay attention to the rhythm of my breathing, which has helped me be able to run, which I have never been able to do before. I ran for 2¼ miles for the first time in my life.” At the post-treatment assessment, her CAPS score was 25, and at the 1-month follow-up assessment, her CAPS score was 14, indicating that she was asymptomatic and experienced >50% reduction in reported symptoms.
Appendix: 20-Week TCTSY Treatment Protocol
Foundational protocol
| Chair practicea: | Mat practice: |
| Seated mountain pose | Seated: |
| Head drop/flexion/head rolls | Easy pose-torso circles |
| Shoulder rolls with elbows on shoulders | Head to knee form |
| Breathing and moving: 3 way (hands raise, hands open and close, sun breath) | Sage twist |
| Twist | Seated forward fold |
| Sun breath + twist | Prone: |
| Seated cat and dog | Knees-to-belly |
| Leg raise (twice on each side) | Extension (arms overhead, legs extended) |
| Forward fold | Knees side-to-side |
| Standing practice: | Reclining leg stretch (knee-to-chest) |
| Mountain | Mat-based relaxationb |
Sessions 11–19 begin with mat-based rather than chair-based practice.
Sessions 1–10 include 3 min of relaxation, sessions 11–20 include 5 min of relaxation.
TCTSY, Trauma Center Trauma-Sensitive Yoga.
Techniques added
| Session | Technique(s) |
|---|---|
| 2 | Standing sun breath and prone figure four |
| 3 | Introduce awareness of breath in seated mountain |
| 5 | Elongate inhalation, Warrior 1, bridge, and knee-down-twist |
| 6 | Warrior 2 |
| 7 | Elongate inhalation and exhalation; Tree |
| 9 | Alternate nostril breath |
| 11 | Begin mat-based practice only (no chair-based practice) |
| 12 | Alternate arm/leg balance in table, triangle |
| 14 | Belly-based techniques (baby cobra, variations on boat) |
| 17 | Wide angle-forward fold |
| 20 | Begin with chair-based practice (like sessions 1–10) and notice how range of forms have changed over practice |
TCTSY practice builds on itself, and thus when a technique is added, it is subsequently incorporated into all future sessions.
Themes of sessions 2–9
| Session | Theme |
|---|---|
| 2, 5–6 | Yoga is an opportunity to practice making choices |
| 3–4 | Yoga is an opprotunity to practice being in the present moment |
| 7–8 | Yoga is an opportunity to practice taking effective action |
| 9 | Yoga is an opportunity to practice moving in rhythm with others |
Author Disclosure Statement
No competing financial interests exist.
Mueller B. The effects of bikram-style hot yoga on posttraumatic stress and depressive symptoms in a military population [dissertation]. California: Alliant University; 2010.
Moliver N. Psychological wellness, physical wellness, and subjective vitality in long-term yoginis over 45 [dissertation]. Scottsdale, AZ: Northcentral University; 2010.
Mueller B. The effects of bikram-style hot yoga on posttraumatic stress and depressive symptoms in a military population [dissertation]. California: Alliant University; 2010.
Moliver N. Psychological wellness, physical wellness, and subjective vitality in long-term yoginis over 45 [dissertation]. Scottsdale, AZ: Northcentral University; 2010.
West JI. Moving to heal: Women's experiences of therapeutic yoga after complex trauma [dissertation]. Chestnut Hill, MA: Boston College; 2011.
Moliver N. Psychological wellness, physical wellness, and subjective vitality in long-term yoginis over 45 [dissertation]. Scottsdale, AZ: Northcentral University; 2010.
References
- 1.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report 2008;1–23 [PubMed] [Google Scholar]
- 2.Khalsa SB. Yoga as a therapeutic intervention. In: Lehrer PM, Woolfolk RL, Sime WE, eds. Principles and Practice of Stress Management. 3rd ed. New York: Guilford Press, 2007:449–462 [Google Scholar]
- 3.Ross A, Thomas S. The health benefits of yoga and exercise: A review of comparison studies. J Altern Complement Med 2010;16:3–12 [DOI] [PubMed] [Google Scholar]
- 4.Emerson D, Sharma R, Chaudhry S, et al. Trauma-sensitive yoga: Principles, practice, and research. Int J Yoga Therap 2009;19:123–128 [Google Scholar]
- 5.Bluhm RL, Frewen PA, Coupland NC, et al. Neural correlates of self-reflection in post-traumatic stress disorder. Acta Psychiatr Scand 2012;125:238–246 [DOI] [PubMed] [Google Scholar]
- 6.Fonzo GA, Simmons AN, Thorp SR, et al. Exaggerated and disconnected insular-amygdalar blood oxygenation level-dependent response to threat-related emotional faces in women with intimate-partner violence posttraumatic stress disorder. Biol Psychiatry 2010;68:433–441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Emerson D, Hopper E. Overcoming Trauma through Yoga: Reclaiming Your Body. Berkeley, CA: North Atlantic Books, 2011 [Google Scholar]
- 8.Descilo T, Vedamurtachar A, Gerbarg PL, et al. Effects of a yoga breath intervention alone and in combination with an exposure therapy for post-traumatic stress disorder and depression in survivors of the 2004 South-East Asia tsunami. Acta Psychiatr Scand 2010;121:289–300 [DOI] [PubMed] [Google Scholar]
- 9.Carter JJ, Brown RP, Ware RS, et al. Multi-component yoga breath program for Vietnam veteran post traumatic stress disorder: Randomized controlled trial. J Trauma Stress Disord Treat 2013;2:1–10 [Google Scholar]
- 10.Staples JK, Hamilton MF, Uddo M. A yoga program for the symptoms of post-traumatic stress disorder in veterans. Mil Med 2013;178:854–860 [DOI] [PubMed] [Google Scholar]
- 11.Johnston JM, Minami T, Greenwald D, et al. Yoga for military service personnel with PTSD: A single arm study. Psychol Trauma Theory, Res Pract Policy 2015;7:555–562 [DOI] [PubMed] [Google Scholar]
- 12.Franzblau SH, Smith M, Echevarria S, et al. Take a breath, break the silence: The effects of yogic breathing and testimony about battering on feelings of self-efficacy in battered women. Int J Yoga Therap 2006;16:49–57 [Google Scholar]
- 13.Spinazzola J, Rhodes AM, Emerson D, et al. Application of yoga in residential treatment of traumatized youth. J Am Psychiatr Nurses Assoc 2011;17:431–444 [DOI] [PubMed] [Google Scholar]
- 14.Shannahoff-Khalsa DS. Kundalini Yoga Meditation: Techniques Specific for Psychiatric Disorders, Couples Therapy, and Personal Growth. New York: W. W. Norton & Co., Inc., 2006 [Google Scholar]
- 15.Shannahoff-Khalsa DS. Sacred Therapies: The Kundalini Yoga Meditation Handbook for Mental Health. New York: W. W. Norton & Co., Inc., 2012 [Google Scholar]
- 16.Mitchell KS, Dick AM, DiMartino DM, et al. A pilot study of a randomized controlled trial of yoga as an intervention for PTSD symptoms in women. J Trauma Stress 2014;27:121–128 [DOI] [PubMed] [Google Scholar]
- 17.Jindani F, Turner N, Khalsa SBS. A yoga intervention for posttraumatic stress: A preliminary randomized control trial. Evid Based Complement Altern Med 2015;2015:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van der Kolk B, West J, Rhodes A, et al. Yoga as an adjunctive treatment for posttraumatic stress disorder: A randomized controlled trial. J Clin Psychiatry 2014;75:1–7 [DOI] [PubMed] [Google Scholar]
- 19.Bradley R, Greene J, Russ E, et al. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry 2005;162:214–227 [DOI] [PubMed] [Google Scholar]
- 20.Kiecolt-Glaser JK, Christian LM, Andridge R, et al. Adiponectin, leptin, and yoga practice. Physiol Behav 2012;107:809–813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daubenmier JJ. The relationship of yoga, body awareness, and body responsiveness to self-objectification and disordered eating. Psychol Women Q 2005;29:207–219 [Google Scholar]
- 22.Rice Cucci L, Williams JS. Practice variables as predictors of stress and relaxation dispositions for yoga and meditation. Adv ABC Relax Appl Invent 2001;193–196 [Google Scholar]
- 23.Dale LP, Carroll LE, Galen GC, et al. Yoga practice may buffer the deleterious effects of abuse on women's self-concept and dysfunctional coping. J Aggress Maltreat Trauma 2011;20:90–102 [Google Scholar]
- 24.Ross A, Friedmann E, Bevans M TS. Frequency of yoga practice predicts health: Results of a national survey of yoga practitioners. Evid Based Complement Alternat Med 2012;2012:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schottenbauer MA, Glass CR, Arnkoff DB, et al. Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry 2008;71:134–168 [DOI] [PubMed] [Google Scholar]
- 26.Galovski TE, Blain LM, Mott JM, et al. Manualized therapy for PTSD: Flexing the structure of cognitive processing therapy. J Consult Clin Psychol 2012;80:968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. J Consult Clin Psychol 2005;73:965. [DOI] [PubMed] [Google Scholar]
- 28.Kazantzis N, Deane FP, Ronan KR. Homework assignments in cognitive and behavioral therapy: A meta-analysis. Clin Psychol Sci Pract 2000;7:189–202 [Google Scholar]
- 29.Vaughan K, Tarrier N. The use of image habituation training with post-traumatic stress disorders. Br J Psychiatry. 1992;161:658–664 [DOI] [PubMed] [Google Scholar]
- 30.van Minnen A, Hagenaars M. Fear activation and habituation patterns as early process predictors of response to prolonged exposure treatment in PTSD. J Trauma Stress 2002;15:359–367 [DOI] [PubMed] [Google Scholar]
- 31.Bluett EJ, Zoellner LA, Feeny NC. Does change in distress matter? Mechanisms of change in prolonged exposure for PTSD. J Behav Ther Exp Psychiatry 2014;45:97–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychol Assess 1999;11:124–133 [Google Scholar]
- 33.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, 2000 [Google Scholar]
- 34.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. J Trauma Stress 1995;8:75–90 [DOI] [PubMed] [Google Scholar]
- 35.Davidson JRT, Book SW, Colket JT, et al. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med 1997;27:153–160 [DOI] [PubMed] [Google Scholar]
- 36.Weathers FW, Keane TM, Davidson JRT. Clinician-administered PTSD scale: A review of the first ten years of research. Depress Anxiety 2001;13:132–156 [DOI] [PubMed] [Google Scholar]
- 37.Carlson EB, Putnam FW, Ross CA, et al. Validity of the Dissociative for Multiple Personality Scale in screening for multiple personality disorder: A multicenter study. Am J Psychiatory 1993;150:1030–1036 [DOI] [PubMed] [Google Scholar]
- 38.Carlson EB, Putnam FW. An update on the dissociative experiences scale. Dissociation Prog Dissociative Disord 1993;6:16–27 [Google Scholar]
- 39.Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986;174:727–735 [DOI] [PubMed] [Google Scholar]
- 40.Frischholz EJ, Braun BG, Sachs RG. The Dissociative Experiences Scale: Further replication and validation. Dissociation Prog Dissociative Disord 1990;3:151–153 [Google Scholar]
- 41.Steinberg M, Rounsaville B, Cicchetti D. Detection of dissociative disorders in psychiatric patients by a screening instrument and a structured diagnostic interview. Am J Psychiatry 1991;148:1050–1054 [DOI] [PubMed] [Google Scholar]
- 42.Emerson D, West J. Trauma-Sensitive Yoga in Therapy: Bringing the Body into Treatment. New York: W. W. Norton & Co., Inc., 2015 [Google Scholar]
- 43.Raudenbush SW, Bryk AS, Cheong YF, et al. HLM Statistical Software v7. Lincolnwood, IL: Scientific Software International, Inc. 2011 [Google Scholar]
- 44.McCartney K, Burchinal MR, Bub KL. Best Practices in Quantitative Methods for Developmentalists. Hoboken, NJ: Wiley, 2006 [DOI] [PubMed] [Google Scholar]
- 45.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford: Oxford University Press, 2003 [Google Scholar]
- 46.Walker-Barnes CJ, Mason CA. Ethnic differences in the effect of parenting on gang involvement and gang delinquency: A longitudinal, hierarchical linear modeling perspective. Child Dev 2001;72:1814–1831 [DOI] [PubMed] [Google Scholar]
- 47.Evans CH, Ildstad ST. Small Clinical Trials: Issues and Challenges. Washington, DC: National Academy Press, 2001 [PubMed] [Google Scholar]
- 48.Markowitz JC, Petkova E, Neria Y, et al. Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. Am J Psychiatry 2015;172:430–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Farchione TJ, Fairholme CP, Ellard KK, et al. Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behav Ther 2012;43:666–678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schnurr PP, Friedman MJ, Engel CC, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. JAMA 2007;297:820–830 [DOI] [PubMed] [Google Scholar]
- 51.Monson CM, Schnurr PP, Resick PA, et al. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol 2006;74:898. [DOI] [PubMed] [Google Scholar]
- 52.Jaycox LH, Foa EB, Morral AR. Influence of emotional engagement and habituation on exposure therapy for PTSD. J Consult Clin Psychol 1998;66:185. [DOI] [PubMed] [Google Scholar]
- 53.Constantino MJ, Arnkoff DB, Glass CR, et al. Expectations. J Clin Psychol 2011;67:184–192 [DOI] [PubMed] [Google Scholar]
- 54.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. Am Psychol 1992;47:1102. [DOI] [PubMed] [Google Scholar]
- 55.Foa EB, Keane TM, Friedman MJ, et al. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. New York: Guilford Press, 2008 [Google Scholar]