The recent update of the guidelines for asymptomatic primary hyperparathyroidism includes recommendations around using the urinary calcium clearance to creatinine clearance ratio (UCCR) (1, 2). UCCR is a calculation that has helped distinguish typical primary hyperparathyroidism (PHPT) from familial hypocalciuric hypercalcemia (FHH) (2–5). An empirical cutoff at 0.01 helps separate these diagnoses. A low value recommends further evaluations about FHH. Both diagnoses show overlaps around the cutoff (2–4). The gold standard for diagnosis of FHH is mutation in CASR, APP2S1, or GNA11 (2, 6, 7).
Distinction between typical PHPT and FHH is important because patients with undiagnosed FHH might be referred for parathyroidectomy. However, the mild consequences of FHH rarely require intervention. Furthermore, parathyroidectomy in FHH is usually followed by persistent hypercalcemia (2, 5, 6).
The article includes a flow diagram, highlighting UCCR to help distinguish typical PHPT from FHH among cases with asymptomatic hyperparathyroidism; a separate diagram guides genetic testing in the minority with likely syndromal hyperparathyroidism (2). In the subset with UCCR below 0.01, the main flow diagram depicts greater than 95% likelihood of FHH and indicates that DNA testing can be considered next. However, the depicted value of 95% for likelihood of FHH in the subset group below 0.01 is incorrect; thus, its attached suggestion is incomplete.
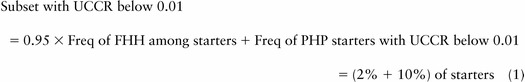
The frequency (Freq) of FHH in the subset with UCCR below 0.01 can be estimated (equation 1 and equation 2):
 |
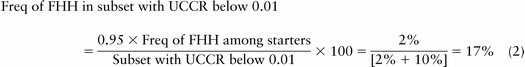 |
The indication that typical FHH is a minority in the subset below the cutoff of 0.01 is similar, using other estimates about the three contributing frequencies. First, 95% of FHH cases have a UCCR below 0.01 (3, 4). Second, the frequency of FHH among tested PHPT cases is estimated as 2%, from its prevalence of 9%–10% among unsuccessful parathyroidectomies before the recognition of FHH (6, 8). Third, UCCR below 0.01 among cases with typical PHPT is estimated as 10% from past reports (4%–23%) (3, 4, 9).
A lower value than cited for likelihood of FHH in this subset has several implications about testing and about management. First, about testing, the UCCR alone does not give as powerful a separation between PHPT and FHH as suggested. Second, the physician may still consider DNA testing in this subset. The cutoff has enriched FHH by approximately 8-fold, although it still remains a minority diagnosis; serum calcium tests in first-degree relatives, especially young relatives, also assist the diagnosis of FHH in a proband (2, 5). Third, the physician also should manage for most likely PHPT in this subset, particularly if the family and DNA testing for FHH is not diagnostic, as is likely to occur.
This work was supported by the intramural program of the National Institute of Diabetes and Digestive and Kidney Diseases and the National Human Genome Research Institute.
Disclosure Summary: The author has nothing to disclose.
The authors of the original article have chosen not to comment on this letter.
Stephen J. Marx
Genetics and Endocrinology Section
National Institute of Diabetes and Digestive and Kidney Diseases
National Institutes of Health, Bethesda
Maryland 20892
e-mail: marxs@mail.nih.gov.
Footnotes
- FHH
- familial hypocalciuric hypercalcemia
- Freq
- frequency
- PHPT
- primary hyperparathyroidism
- UCCR
- urinary calcium clearance to creatinine clearance ratio.
References
- 1. Bilezikian JP, Brandi ML, Eastell R, et al. . Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99:3561–3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eastell R, Brandi ML, Costa AG, D'Amour P, Shoback DM, Thakker RV. Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99:3570–3579. [DOI] [PubMed] [Google Scholar]
- 3. Marx SJ, Spiegel AM, Brown EM, et al. . Divalent cation metabolism: familial hypocalciuric hypercalcemia versus typical primary hyperparathyroidism. Am J Med. 1978;65:235–242. [DOI] [PubMed] [Google Scholar]
- 4. Christensen SE, Nissen PH, Vestergaard P, Heickendorff L, Brixen K, Mosekilde L. Discriminative power of three indices of renal calcium excretion for the distinction between familial hypocalciuric hypercalcemia and primary hyperparathyroidism: a follow-up study on methods. Clin Endocrinol (Oxf). 2008;69:713–720. [DOI] [PubMed] [Google Scholar]
- 5. Arnold A, Marx SJ. Familial hyperparathyroidism (Including MEN, FHH, and HPT-JT). In: Rosen C, Bouillon R, Compston JE, Rosen V, eds. Primer on the Metabolic Bone Diseases and Mineral Metabolism. 8th ed John Wiley, Sons, Inc; Hoboken, NJ: 2013:553–561. [Google Scholar]
- 6. Marx SJ, Stock JL, Attie MF, et al. . Familial hypocalciuric hypercalcemia: recognition among patients referred after unsuccessful parathyroid exploration. Ann Int Med. 1980;92:351–356. [DOI] [PubMed] [Google Scholar]
- 7. Nesbit MA, Hannan FM, Howles SA, et al. . Mutations affecting G-protein subunit a11 in hypercalcemia and hypocalcemia. N Engl J Med. 2013;368:2476–2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Heath H., 3rd Familial benign (hypocalciuric) hypercalcemia. A troublesome mimic of mild primary hyperparathyroidism. Endocrinol Metab Clin North Am. 1989;18:723–740. [PubMed] [Google Scholar]
- 9. Jayasena C, Mahmud M, Palazzo F, Donaldson M, Meeran K, Dhillo WS. Utility of the urine calcium-to-creatinine ratio to diagnose primary hyperparathyroidism in in asymptomatic hypercalcemic patients with vitamin D deficiency. Ann Clin Biochem. 2011;48:126–129. [DOI] [PubMed] [Google Scholar]


