Abstract
Objective
Define the frequency and survival pattern of cardiac arrests in relation to the hospital day of event and etiology of arrest.
Subject and methods
Retrospective cohort study of adult in-hospital cardiac arrests between July 1, 2005, and June 30, 2013, that were classified by etiology of deterioration. Arrests were divided based on hospital day (HD) of event (HD1, HD2–7, HD>7 days), and analysis of frequency was performed. The primary outcome of survival to discharge and secondary outcomes of return of spontaneous circulation (ROSC) and favorable neurological outcomes were compared using multivariable logistic regression analysis.
Results
A total of 627 cases were included, 193 (30.8%) cases in group HD1, 206 (32.9%) in HD2–7, and 228 (36.4%) in HD>7. Etiology of arrest demonstrated variability across the groups (p < 0.001). Arrests due to ventilation issues increased in frequency with longer hospitalization (p < 0.001) while arrests due to dysrhythmia had the opposite trend (p = 0.014). Rates of survival to discharge (p = 0.038) and favorable neurological outcomes (p = 0.002) were lower with increasing hospital days while ROSC was not different among the groups (p = 0.183). Survival was highest for HD1 (HD1: 38.9% [95% CI, 32.0–45.7%], p = 0.002 vs HD2–7: 34.0% [95% CI, 27.5–40.4%], p < 0.001 vs HD>7: 27.2% [95% CI, 21.4–33.0%], p < 0.001).
Conclusions
The etiology of cardiac arrests varies in frequency as length of hospitalization increases. Survival rates and favorable neurological outcomes are lower for in-hospital arrests occurring later in the hospitalization, even when adjusted for age, sex, and location of event. Understanding these issues may help with focusing therapies and accurate prognostication.
Keywords: In-hospital cardiac arrest, Cardiopulmonary resuscitation, Return of spontaneous circulation, Outcome assessment, Adult, Hospitalization
Introduction
Survival from in-hospital cardiac arrest has been historically low with reported rates of success varying across hospitals from 15% to 40% but with the most common estimate around 20%.1–7 Well-established prognostic parameters for a favorable outcome have been identified, including witnessed events, short time between collapse and arrival of the resuscitation team, short duration of CPR, and ventricular fibrillation as the first recorded rhythm.4,7–9 However, there are few studies dedicated to evaluating the cause of the cardiac arrest and its relationship to the outcome of in-hospital cardiac arrests. Wallmuller et al. found that 63% of arrests were due to a cardiac etiology which had a significantly better outcome than those who had a non-cardiac cause of arrest (44 vs 23%); the majority of non-cardiac causes were attributed to pulmonary causes.10 However, this prior study was designed to evaluate in-patient cardiac arrests within an emergency room equipped with ICU beds.
Our study aims to evaluate the outcome of in-hospital cardiac arrests, focusing on the relationship between etiology and outcome and, in particular, in relation to the length of hospitalization prior to the cardiac arrest. We sought to test the hypothesis that cardiac arrests occurring after longer hospitalizations were associated with lower survival rates and worse neurological outcomes compared to shorter hospitalizations.
Methods
Study design and setting
This is a retrospective cohort study that assessed all adult patients admitted to University of California, San Diego (UCSD), a tertiary referral center. Cardiac arrests from two hospitals were included in the study, including the UCSD Hillcrest Medical Center and Thornton Hospital which are comprised of a total of 530 beds of which 74 are licensed ICU beds. The study included all patients who were admitted to the hospital and had a cardiac arrest between July 1, 2005, and June 30, 2013. Resuscitation attempts are conducted by a multidisciplinary team, who have been certified in Advanced Resuscitation Training (ART) and include residents, attending physicians, nurses, pharmacists, and respiratory therapists. ART is a resuscitation management program designed for inpatient cardiopulmonary arrests, which is used as an alternative to advanced cardiac life support (ACLS) at UCSD.11
Inclusion and exclusion criteria
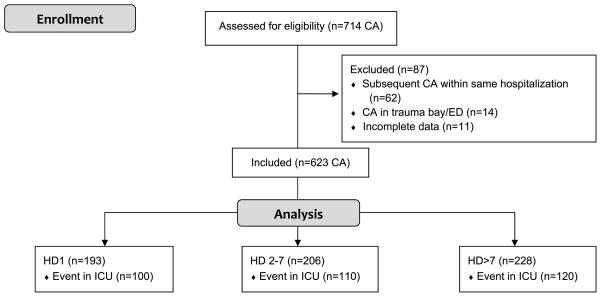
Patients who were 18 years or older and experienced a cardiac arrest (defined as the lack of a palpable central pulse, apnea, and unresponsiveness), requiring cardiopulmonary resuscitation (CPR) or defibrillation, were included in the analysis. Only index events, defined as the first arrest for patients having more than 1 arrest during the same hospitalization, were included. Exclusion criteria included all cardiac arrests in which resuscitation was initiated out of the hospital, in the emergency department, in the trauma bay, or if the patient had an active do-not-attempt resuscitation order (Fig. 1).
Fig. 1.
Flow diagram illustrating the number cardiac arrests (CA) occurring during the study period (ED = emergency department, HD = hospital day group, ICU = intensive care unit).
Data collection and integrity
Cardiac arrests were identified through a robust review of standardized resuscitation records, “code blue” committee minutes, the continuous quality improvement (CQI) database, and the electronic medical record. Information for each cardiac arrest was entered into a database and cross-referenced to ensure data integrity. Detailed chart review for medical history, clinical presentation, and underlying disease was completed. The project was approved by the University of California, San Diego, Institutional Review Board (IRB 150899).
Advanced Resuscitation Training
Hospital-based resuscitation has unique features related to the etiologies of arrest and the spectrum of deterioration. ART was developed as a comprehensive program involving resuscitation training aimed at not only preventing arrests in critically ill patients but also optimizing the treatment of the cardiopulmonary arrest patient by linking CQI with training and incorporating new understanding of resuscitation science.12 As part of tailoring treatment algorithms and improving recognition of clinical deterioration, the ART Matrix was developed, which represents a taxonomy to describe the various etiologies of cardiopulmonary arrest. The matrix is hierarchical and categorizes resuscitation events as described in Table 1. Patients were designated into one of these groups after review of the medical record, including autopsy reports or imaging studies, if available. ART relies heavily on early recognition and an aggressive rapid response system. Rapid responses can be activated by staff or the patient/family.
Table 1.
Definitions for the etiology of cardiac arrest based on the Advanced Resuscitation Training (ART) Matrix.
| A cardiac arrest is presumed to be of the following aetiology if deterioration can be primarily attributed to the following: | ||
| Ventilation |
|
Intubated |
| Hypoxemia which may be due to known pulmonary disease (pneumonia, chronic obstructive pulmonary disease, asthma, etc.) or with airway obstruction that accompanies a decrease in mental status (due to analgesia/sedation, sleep apnea, hypoglycemia, etc.). Patients are further divided based on airway access prior to the arrest. | Non-intubated | |
| Tracheostomy | ||
| Rapid sequence intubation | ||
| Includes cardiac arrest as a complication following airway management initiation | ||
| Circulation |
|
Sepsis |
| Hypoperfusion which may be due to loss of intravascular volume (including blood loss or fluid shift into the interstitial space), obstruction of forward flow, or secondary to impaired cardiac function. | Clinical syndrome that results from a dysregulated inflammatory response to infection | |
| Hemorrhage | ||
| Includes gastrointestinal bleeding and postoperative blood loss | ||
| Pulmonary embolus | ||
| Cardiac dysfunction | ||
| Includes congestive heart failure and constrictive disease (ie. pericardial effusion) | ||
| Dysrhythmia |
|
Ventricular fibrillation/ventricular tachycardia |
| Abnormality in the rate, regularity, or rhythm of cardiac electrical activity as the primary cause of cardiac arrest. | Vagal | |
| Identified as cardiac arrests preceded by bradycardia in the setting of an identifiable vagal stimulus (i.e. micturation, defecation, deep oral suctioning, position change, etc.) | ||
| Neurological | ||
| Acute neurological deficits or alteration in mental status, not attributable to hypoperfusion, hypoxemia, or hypoglycemia, which may include cerebrovascular accident or intracranial hemorrhage. | ||
| Unknown | ||
| Cause of arrest is not know n or could not be classified as any of the options above. | ||
Outcome
The primary outcome measure was survival to discharge. Secondary outcomes were return of spontaneous circulation (ROSC) for more than 1 h and favorable neurological outcomes. Neurological outcome was determined using the cerebral performance category (CPC) score. A favorable neurological outcome was defined as a cerebral performance score of 1 or 2 (range, 1–5) at the time of discharge.
In addition, outcome measures were evaluated based on length of hospitalization. Cardiac arrests were divided into three groups based on the hospital day (HD) in which the event occurred. The first group included all arrests that occurred on the first hospital day or within 24 h of the day of admission (HD1), the second group included cardiac arrests on hospital day 2 through 7 (HD2–7), and the third group included all cardiac arrests that occurred after hospital day 7 (HD>7 days). The ranges were chosen to compare three specific cohorts of patients. Given that the average length of hospitalization at UCSD is 4.1 days, HD1 represents the group that had an arrest as an early complication of their hospitalization compared to those with an arrest preceded by an average length of hospital stay (HD2–7) and those with an arrest during a prolonged hospitalization (HD>7).13
Data analysis
Statistical analysis was conducted via SPSS Statistics (IBM Corp., Version 21.0. Armonk, NY). For discrete variables, the number of observations was calculated for each level or outcome and tested for significant differences between groups with the chi-squared test. Continuous variables are reported as medians and interquartile ranges. Percentages were determined for dichotomous variables and are presented with 95% confidence intervals (95% CI). To examine the association between hospital day and survival to discharge, multivariable logistic regression analyses were used with hospital day as the exposure variable. The model included clinically important confounders, including age, sex, and event location (ICU vs non-ICU inpatient ward). Using this model, analyses were also performed to determine the effect of hospital day on return of spontaneous circulation and favorable neurological outcome. All p values represent 2-sided hypothesis tests. The significance level for all tests was α < 0.05.
Results
There were 627 cases of in-hospital, index event, cardiac arrests that occurred during the 8-year study period, including 193 (30.8%) cases in group HD1, 206 (32.9%) in HD2–7, and 228 (36.4%) in HD>7 (Fig. 2). Patient characteristics are shown in Table 2. Event location was determined by whether the arrest occurred in the intensive care unit or not. The distribution of age, sex, and event location were similar among the three groups, as noted with non-significant p values. The incidence of all in-hospital CA during the study period was 3.39 CA/1000 patient discharge, and the median day of arrest was on hospital day 4. The incidence of CA in the ICU was 1.78 CA/1000 patient discharges during the study period.
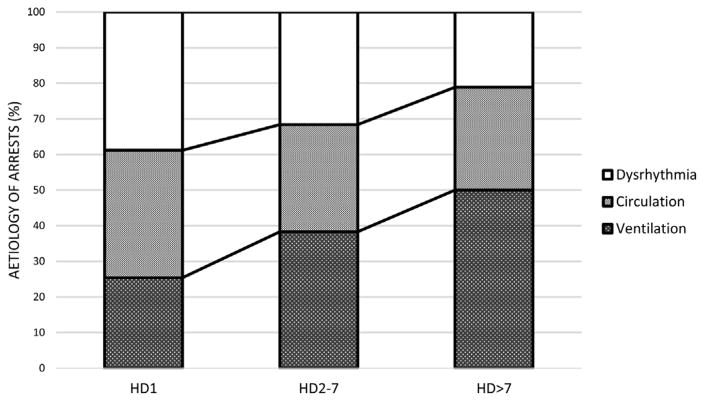
Fig. 2.
Trend in cardiac arrests based on etiology of arrests within each hospital day group (left) for three main etiologies of arrest (ventilation, circulation, and dysrhythmia).
Table 2.
Patient characteristics.
| No. (%)
|
p value | ||||
|---|---|---|---|---|---|
| HD1 (n = 193)a | HD2–7 (n = 206)a | HD>7 (n = 228)a | Total (n = 627) | ||
| Age at event, median (25–75%), year | 58 (49–69) | 61 (52–74) | 59 (47–67) | 60 (50–70) | 0.076 |
| Male sex | 123 (63.7) | 129 (62.6) | 156 (68.4) | 408 (65.1) | 0.402 |
| Event location in ICU | 100 (51.8) | 110 (53.4) | 120 (52.6) | 330 (52.6) | 0.951 |
HD1 was defined as cardiac arrest event occurring on hospital day 1, HD2–7 as event on days 2–7, and HD>7 as event after 1 week of hospitalization.
Causes of cardiac arrest
Cardiac arrests were classified into the ART Matrix based on etiology of deterioration and hospital day of event as shown in Table 3. The majority of cases were classified in the ventilation group (38.6%); of which, the largest subgroup included the patients who were not intubated prior to the cardiac arrest (28.9%). The circulation group was composed of mainly arrests secondary to sepsis (17.5%), and the dysrhythmia group was largely represented by ventricular fibrillation/ventricular tachycardia (VF/VT, 17.5%) arrests. The remaining cardiac arrests were classified into the neurological group, which included 17 arrests (2.7%), and 24 (3.8%) cardiac arrests which were unknown. Perhaps due to the limited number of cases, the neurological group did not have statistically significant findings.
Table 3.
Etiology of cardiac arrests by hospital day.
| No. (%)
|
p value | ||||
|---|---|---|---|---|---|
| HD1 (n = 193)b | HD2–7 (n = 206)b | HD>7 (n = 228)b | Total (n = 627) | ||
| Ventilation | 49 (25.4) | 79 (38.3) | 114 (50) | 242 (38.6) | <0.001 |
| Intubated | 6 (3.1) | 11 (5.3) | 18 (7.9) | 35 (5.6) | 0.044 |
| Non-intubated | 40 (20.7) | 62 (30.1) | 79 (34.6) | 181 (28.9) | 0.002 |
| Tracheostomy | 1 (0.5) | 4 (1.9) | 9 (3.9) | 14 (2.2) | 0.03 |
| Rapid sequence intubation | 2 (1) | 2 (1) | 8 (3.5) | 12 (1.9) | 0.05 |
| Circulation | 69 (35.8) | 62 (30.1) | 66 (28.9) | 197 (31.4) | 0.829 |
| Sepsis | 37 (19.2) | 36 (17.5) | 37 (16.2) | 110 (17.5) | 0.991 |
| Hemorrhage | 13 (6.7) | 10 (4.9) | 14 (6.1) | 37 (5.9) | 0.704 |
| Pulmonary embolus | 7 (3.6) | 6 (2.9) | 4 (1.8) | 17 (2.7) | 0.662 |
| Cardiac dysfunction | 12 (6.2) | 10 (4.9) | 11 (4.8) | 33 (5.3) | 0.913 |
| Dysrhythmia | 65 (33.7) | 45 (21.8) | 37 (16.2) | 147 (23.4) | 0.014 |
| VF/VTa | 44 (22.8) | 40 (19.4) | 26 (11.4) | 110 (17.5) | 0.087 |
| Vagal | 21 (10.9) | 5 (2.4) | 11 (4.8) | 37 (5.9) | 0.005 |
| Neurological | 6 (3.1) | 9 (4.4) | 2 (0.9) | 17 (2.7) | 0.113 |
| Unknown | 4 (2.1) | 11 (5.3) | 9 (3.9) | 24 (3.8) | 0.197 |
VF/VT, ventricular fibrillation/ventricular tachycardia.
HD1 was defined as cardiac arrest event occurring on hospital day 1, HD2–7 as event on days 2–7, and HD>7 as event after 1 week of hospitalization.
Frequency in relation to hospital day
Etiology of cardiac arrests demonstrated significant variability across the hospital day groups (p < 0.001). Specifically, cardiac arrests due to ventilation issues increased in frequency with longer duration of hospitalization (p < 0.001) while arrests due to dysrhythmia had the opposite trend (p = 0.014). As the length of hospitalization increased, the proportion of all arrests due to ventilation etiologies increased from 20.2% on the first hospital day to 47.1% after the first week of hospitalization while 44.2% of all dysrhythmic arrests occurred on hospital day 1 and tapered to 25.2% after hospital day 7. The circulation group had an overall downward trend across the hospital days when compared with all cardiac arrests, but the frequency of arrests within the circulation group was similar (p = 0.829). Fig. 2 depicts the trend in cardiac arrests based on etiology as the frequency within the hospital day groups.
The trend in the ventilation group continues to be statistically significant even with the division into the subgroups (intubated: p = 0.044, non-intubated: p = 0.002, tracheostomy: p = 0.030, and rapid sequence intubation: p = 0.05). Analysis of the dysrhythmia subgroups revealed a significant trend in vagal arrests (p = 0.005), and although the subgroup VF/VT did not reach statistical significance alone (p = 0.087), the trend seen in the dysrhythmia group is reflective of the VF/VT subgroup given that the subgroup makes up the majority of the dysrhythmia group. There was no significant difference for the frequency of cardiac arrests within the circulation subgroups.
Outcome in relation to hospital day
Rates of survival to discharge and favorable neurological outcomes were lower with increasing hospital days while ROSC was not different among the groups with increasing length of hospitalization. Patients with cardiac arrests that occurred at the beginning of their hospitalization had a higher survival rate than patients whose arrest occurred later, namely after 1 week of hospitalization (Table 4). A logistic regression was performed to ascertain the effects of day of hospital arrest and the etiology of arrest on the likelihood of patients dying. The logistic regression model was statistically significant, χ2(14) = 82.288, p < 0.001. The model explained 17.1% (Nagelkerke R2) of the variance in survival and correctly classified 69.9% of cases with a sensitivity of 94.3% and specificity of 19.9%. Group day of arrest had no significant effect on survival to discharge (Wald = 4.181, p = 0.124). However, the type of arrest did significantly affect survival to discharge (Wald = 30.865, p < 0.001). Patients having a circulation type of arrest were 11.389 times more likely to die than patients having a dysrhythmia type of arrest (C.I. = 4.805–26.992, p < 0.001) while patients having a respiratory failure type of arrest were 2.477 times more likely to die than patients having a dysrhythmia type of arrest (C.I. = 1.158–5.299, p = 0.019). There was no significant main interaction effect between group day of arrest and type of arrest on survival (Wald = 6.855, p = 0.552). However, patients having a circulation type of arrest during days 2–7 of hospitalization were less likely to die prior to discharge (Wald = 3.899, O.R. = 0.293, C.I. = 0.089–0.991, p = 0.048).
Table 4.
Cardiac arrest outcomes by hospital day.a
| No. (%) [95% confidence interval]
|
Odds ratio (95% confidence interval)
|
p valuee | |||||
|---|---|---|---|---|---|---|---|
| HD1 (n = 193)c | HD2–7 (n = 206)c | HD>7 (n = 228)c | Total (n = 627) | Unadjusted odds ratio (HD1/HD>7) | Adjusted odds ratio (HD1/HD>7)d | ||
| Survival to discharge | 75 (38.9) [32.0–45.7] | 70 (34) [27.5–40.4] | 62 (27.2) [21.4–33.0] | 207 (33.0) [29.3–36.7] | 0.588 (0.391–0.886) | 0.587 (0.386–0.891) | 0.012 |
| Return of spontaneous circulation | 146 (75.6) [69.6–81.7] | 142 (68.9) [62.6–75.3] | 155 (68) [61.9–74.0] | 443 (70) [67.1–74.2] | 0.684 (0.444–1.051) | 0.685 (0.443–1.058) | 0.088 |
| Favorable neurological outcomeb | 67 (34.7) [28.0–41.4] | 55 (26.7) [20.1–32.7] | 45 (19.7) [14.6–24.9] | 167 (26.6) [23.2–30.1] | 0.462 (0.298–0.719) | 0.455 (0.290–0.714) | 0.001 |
p < 0.001 for all HD groups for all 3 outcomes, except survival to discharge for HD1 where p = 0.002.
A cerebral performance category score of 1 or 2 (range, 1–5).
HD1 was defined as cardiac arrest event occurring on hospital day 1, HD2–7 as event on days 2–7, and HD>7 as event after 1 week of hospitalization.
Regression adjusted for sex, age, and event location.
p value for adjusted odds ratio.
Discussion
This study defines the frequency and outcome of patients suffering from in-hospital cardiac arrests in relation to the hospital day of event and etiology of arrest. Specifically, as ventilation arrests increased, dysrhythmic arrests decreased. In addition, survival to discharge is inversely proportional to the length of hospitalization prior to the cardiac arrest. This trend is likely a reflection of multiple factors related to patient characteristics, pre-arrest conditions, etiology of arrest, and complications of prolonged hospitalization. This trend has been noted in previous studies of rapid response teams that have found that late deterioration (>7 days after admission) is associated with a higher incidence of respiratory distress and worse outcomes.14,15 Few studies have evaluated time of day as a predictor of survival and have noted that survival rates for cardiac arrests during the night was lower than during the day.16–19
Factors which have been associated with death after in-hospital arrest include pre-arrest morbidity, specifically, with clinical diagnoses of sepsis, renal failure, and cancer. Not surprisingly, average length of hospitalization is longest for each of these diagnoses.20–24 In 2009–2010, the average length of hospitalization for septicemia, cancer, and kidney disease was 9.3 days, 6.4 days, and 6.2 days, respectively, for the age group of 65–74 years.25 The worst survival outcome in our cohort is found in the group with the longest hospitalization prior to the arrest which likely has a higher population of patients with these co-morbidities.
Several studies have identified parameters predictive of a favorable outcome in patients with in-hospital cardiac arrests and found that VF/VT arrests have been consistently shown to have better outcomes compared to non-VF/VT rhythms.1,4,26 This finding is confirmed by the better outcomes in our patients in the first hospital day group, which has the highest percentage of arrests with a shockable dysrhythmia. Carr et al. studied early cardiac arrest in patients hospitalized with pneumonia and found that the majority of patients had an arrhythmia in the absence of concurrent hypotension or respiratory distress.27 However, their group found that the most common initial arrest rhythms were PEA and a systole and not shockable rhythms. Although this finding is not reflective of the higher proportion of VF/VT in our HD1 group, some episodes of PEA or a systole that were found may represent late detection of pulselessness and subsequent degeneration from a shockable arrest rhythm.28 The absence of respiratory distress is consistent with our data in that lower rates of cardiac arrest due to ventilation were found in the first two hospital day groups.
Our findings should be interpreted in light of the following potential limitations. This study suffers from a low sample size in some subgroups, which increases the risk of type II errors. The study was performed at a single, academic institution, and the results of the paper may not be generalizable for other institutions. A cause–effect relationship between hospital day and etiology of arrest cannot be inferred due to the nature of our study design. Measures of severity of illness and complexity of co-morbidity are not provided. In addition, CPC score was not evaluated on admission which may have led to an underestimation of favorable neurological outcome (i.e., categorizing patients with no change in neurological status from admission to discharge as having a poor neurological outcome).
Lastly, the observation that return of spontaneous circulation is not affected by hospital day is important. In large part, at UCSD, ART has improved immediate success rates with cardiac arrest. ART relies heavily on early recognition and prevention and has an active rapid response system. In 2012–13 the RRT rate was 31.4 events/1000 patient discharges and just over 50% of those patients are transferred to a higher level of care as a result of the rapid response. We are unable to examine the impact of rapid response on day of arrest, but have shown a decrease in incidence with our system.11 On a national level, both survival and neurological outcomes after in-hospital cardiac arrest have improved over the last decade, likely due to earlier recognition and improved resuscitation care. Cardiac arrests can be avoided with early recognition and should be part of protocols implemented in order to intervene at earlier clinical time points before progression to a cardiac arrest.29,30 Considering that the morbidity associated with cardiac arrests is high, a resuscitation program geared toward early detection of deterioration is crucial in avoiding preventable arrests.
Our study approaches the classification of cardiac arrests from a novel perspective, not only in regards to frequency and survival patterns based on a temporal spectrum of hospital days, but also from a functional perspective to guide cardiac arrest prevention and to improve aspects of a resuscitation program. ART was designed to prompt early intervention and to tailor treatment algorithms based on the etiology of deterioration. Thus, characterization of arrest and survival patterns is crucial in improving in-patient resuscitation programs. Moreover, such information can be crucial to providing accurate guidance to patients/families during code status discussions.
Conclusions
The etiology of cardiac arrests as defined by the ART Matrix varies in frequency as length of hospitalization increases. Survival rates and favorable neurological outcomes are lower for in-hospital cardiac arrests occurring later in the hospitalization, even when adjusted for potentially confounding factors. The mechanism for decreased survival is likely multi-factorial, related to patient physiology as well as operational factors. These data suggest the need for further studies aimed to improve resuscitation practices and prognostication. Future studies may examine the impact of increasing hospital stay on etiology of CA and survival. Ultimately interventional strategies could be defined based on the type and pattern of arrest and the associated prognosis.
Footnotes
Work was performed at University of California, San Diego.
No financial support was received for this research article.
A Spanish translated version of the abstract of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2016.07.006.
Conflict of interest statement
The authors have no commercial associations or sources of support that might pose a conflict of interest.
References
- 1.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 2.Rozenbaum EA, Shenkman L. Predicting outcome of in-hospital cardiopulmonary resuscitation. Crit Care Med. 1988;16:583–6. doi: 10.1097/00003246-198806000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Hodgetts TJ, Kenward G, Vlackonikolis I, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation. 2002;13:115–23. doi: 10.1016/s0300-9572(02)00098-9. [DOI] [PubMed] [Google Scholar]
- 4.Cooper S, Janghorbani M, Cooper G. A decade of in-hospital resuscitation: outcomes and prediction of survival? Resuscitation. 2006;68:231–7. doi: 10.1016/j.resuscitation.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 5.Herlitz J, Andreasson AC, Bang A, Aune S, Lindqvist J. Long-term prognosis among survivors after in-hospital cardiac arrest. Resuscitation. 2000;45:167–71. doi: 10.1016/s0300-9572(00)00187-8. [DOI] [PubMed] [Google Scholar]
- 6.Fredriksson M, Aune S, Thorén AB, Herlitz J. In-hospital cardiac arrest: an Utstein style report of seven years experience from the Sahlgrenska University Hospital. Resuscitation. 2006;68:351–8. doi: 10.1016/j.resuscitation.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33:237–45. doi: 10.1007/s00134-006-0326-z. [DOI] [PubMed] [Google Scholar]
- 8.Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010;38:101–8. doi: 10.1097/CCM.0b013e3181b43282. [DOI] [PubMed] [Google Scholar]
- 9.Brady WJ, Gurka KK, Mehring B, Peberdy MA, O’Connor RE American Heart Association’s Get with the Guidelines (formerly, NRCPR) Investigators. In-hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation. 2011;82:845–52. doi: 10.1016/j.resuscitation.2011.02.028. [DOI] [PubMed] [Google Scholar]
- 10.Wallmuller C, Meron G, Kurkciyan I, Schober A, Stratil P, Sterz F. Causes of in-hospital cardiac arrest and influence on outcome. Resuscitation. 2012;83:1206–11. doi: 10.1016/j.resuscitation.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Davis DP, Graham PG, Husa RD, et al. A performance improvement-based resuscitation programme reduces arrest incidence and increases survival from in-hospital cardiac arrest. Resuscitation. 2015;92:63–9. doi: 10.1016/j.resuscitation.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 12. [accessed 16.08.13];UCSD Medical Center advanced resuscitation training manual. Available at: http://www.health.ucsd.edu/medinfo/nursing/edr/education/Documents/ARTMANUAL2012.pdf.
- 13.UC San Diego Health System, Hillcrest. [accessed 16.08.13];Rating hospital quality in California. Available at: http://www.calhospitalcompare.org.
- 14.Smith RJ, et al. The duration of hospitalization before review by the rapid response team: a retrospective cohort study. J Crit Care. 2015;30:692–7. doi: 10.1016/j.jcrc.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 15.Jones D, et al. The timing of rapid-response team activations: a multicentre study. Crit Care Resusc. 2013;15:15–20. [PubMed] [Google Scholar]
- 16.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785–92. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 17.Herlitz J, Bang A, Alsen B, Aune S. Characteristics and outcome among patients suffering from in hospital cardiac arrest in relation to whether the arrest took place during office hours. Resuscitation. 2002;53:127–33. doi: 10.1016/s0300-9572(02)00014-x. [DOI] [PubMed] [Google Scholar]
- 18.Dumot JA, Burval DJ, Sprung J, et al. Outcome of adult cardiopulmonary resuscitations at a tertiary referral center including results of limited resuscitations. Arch Intern Med. 2001;161:1751–8. doi: 10.1001/archinte.161.14.1751. [DOI] [PubMed] [Google Scholar]
- 19.Jones-Crawford JL, Parish DC, Smith BE, Dane FC. Resuscitation in the hospital: circadian variation of cardiopulmonary arrest. Am J Med. 2007;120:158–64. doi: 10.1016/j.amjmed.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 20.Kazaure HS, Roman SA, Rosenthal RA, Sosa JA. Cardiac arrest among surgical patients: an analysis of incidence, patient characteristics, and outcomes in ACS-NSQIP. JAMA Surg. 2013;148:14–21. doi: 10.1001/jamasurg.2013.671. [DOI] [PubMed] [Google Scholar]
- 21.Ballew KA, Philbrick JT, Caven DE, Schorling JB. Predictors of survival following in-hospital cardiopulmonary resuscitation. A moving target. Arch Intern Med. 1994;154:2426–32. [PubMed] [Google Scholar]
- 22.de Vos R, Koster RW, De Haan RJ, Oosting H, van der Wouw PA, Lampe-Schoenmaeckers AJ. In-hospital cardiopulmonary resuscitation: prearrest morbidity and outcome. Arch Intern Med. 1999;159:845–50. doi: 10.1001/archinte.159.8.845. [DOI] [PubMed] [Google Scholar]
- 23.Ebell MH, Afonso AM. Pre-arrest predictors of failure to survive after in-hospital cardiopulmonary resuscitation: a meta-analysis. Fam Pract. 2011;28:505–15. doi: 10.1093/fampra/cmr023. [DOI] [PubMed] [Google Scholar]
- 24.Khasawneh FA, Kamel MT, Abu-Zaid MI. Predictors of cardiopulmonary arrest outcome in a comprehensive cancer center intensive care unit. Scand J Trauma Resusc Emerg Med. 2013;21:18. doi: 10.1186/1757-7241-21-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Table 97. [accessed 16.08.13];Average length of stay in nonfederal short-stay hospitals, by sex, age, and selected first-listed diagnosis: United States, selected years 1990 through 2009–2010. Available at: http://www.cdc.gov/nchs/hus/contents2012.htm#097.
- 26.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–7. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 27.Carr GE, Yuen TC, McConville JF, et al. Hospital cardiac arrest among patients with coexisting pneumonia: a report from the American Heart Association’s Get with the Guidelines-Resuscitation Program. Chest. 2012;141:1528–36. doi: 10.1378/chest.11-1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tovar OH, Jones JL. Electrophysiological deterioration during long-duration ventricular fibrillation. Circulation. 2000;10223:2886–91. doi: 10.1161/01.cir.102.23.2886. [DOI] [PubMed] [Google Scholar]
- 29.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–20. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith GB. In-hospital cardiac arrest: is it time for an in-hospital ‘chain of prevention’? Resuscitation. 2010;81:1209–11. doi: 10.1016/j.resuscitation.2010.04.017. [DOI] [PubMed] [Google Scholar]