Abstract
Background
The prevalence of chronic opioid use among non-cancer patients presenting with acute abdominal pain (AAP) is unknown. The aim was to characterize opioid use, constipation, diagnoses, and risk factors for surgical diagnoses among non-cancer patients presenting with AAP to an emergency department (ED).
Methods
We performed a retrospective, observational cohort study of all (n=16,121) adult patients (88% from Minnesota, Iowa and Wisconsin) presenting during 2014 with AAP. We used electronic medical records, and focused on 2352 adults with AAP who underwent abdominal CT scan within 24 hours of presentation. We determined odds ratios of association with constipation and features predicting conditions that may require surgery (surgical diagnosis).
Key Results
There were 2,352 eligible patients; 18.8% were opioid users. Constipation was more frequent in opioid (35.1%) compared to non-opioid users [OR 2.88 (95% CI 2.28, 3.62)]. Prevalence of surgical diagnosis in the opioid and non-opioid users was 35.3% and 41.7% respectively (p=0.019). By univariate analysis, age and neutrophil count independently predicted increased risk, and chronic opioid use decreased risk of surgical diagnosis. Internal validation of logistic models using a randomly selected validation subset (25% of entire cohort, 587/2352) showed receiver operating characteristic (ROC) curves for the validation and full cohorts were similar.
Conclusions & Inferences
Approximately 19% of adults presenting with AAP were opioid users; constipation is almost 3 times as likely in opioid users compared to non-opioid users presenting with AAP. Factors significantly associated with altered risk of surgical diagnoses were age, opioid use, and neutrophil count.
Keywords: emergency, CT, abdominal pain, opioids, constipation
Graphical Abstract
INTRODUCTION
Abdominal pain is a frequent presentation of patients attending emergency departments (ED); some patients are also constipated at the time of presentation. In the U.S., the prevalence of constipation and the associated costs of ED visits for constipation have increased by 121.4%, from ~$733 million in 2006 to $1.62 billion in 2011 (1). Elderly people or those with risk factors for vascular disease frequently present with acute abdominal pain. The differential diagnosis includes potentially fatal conditions such as mesenteric ischemia, dissecting or leaking abdominal aortic aneurysm, or more common surgical emergencies such as intestinal obstruction, perforation or acute appendicitis. Therefore, these patients frequently undergo imaging studies including emergency CT scans or ultrasonography (2–5).
The widespread use of opiates in the U.S. is associated with fatalities (6); 4% of adults in the U.S. are receiving opioid drugs for chronic, non-cancer pain (7), with prevalence of constipation from 41 to 81% (8,9). Constipation may cause acute abdominal pain. In patients receiving long-term opioid therapy who presented with opioid overdose, 41% were receiving opioids for the indication of abdominal pain (10). The prevalence of chronic opioid use among patients presenting to ED with acute abdominal pain is unclear. Based on the prevalence of chronic opioid use for non-cancer pain (4%), a conservative estimate would be that the prevalence of chronic opioid use among patients presenting to ED with acute abdominal pain would be 4%. On the other hand, patients on opioid therapy may also suffer other abdominal pathology. There are several possible causes of the acute abdominal pain in patients on chronic opioid therapy: first, the original indication for treatment with opioids; second, a result of constipation associated with opioid; and third, other abdominal pathology. Assuming the cause is related to the etiology of chronic pain or the constipation resulting from opioid use may lead to a failure to diagnose the emergency condition presenting as acute abdominal pain and this assumption may thus prove fatal. Based on these considerations, there is need to understand, in patients receiving opioids for non-cancer pain for at least 3 months, the relationships of acute abdominal pain presenting to EDs, the concomitant presence of constipation, and the diagnosis of the cause of the pain. In addition, analysis of the medical records could provide clues regarding the presently unknown predictors of surgical diagnoses in patients receiving chronic opioid treatment.
Our overall aim was to characterize clinical features and factors associated with surgical diagnoses among adult patients who presented with acute abdominal pain to the ED and underwent abdominal and/or pelvic CT scan within 24 hours of presentation. We appraised all the electronic medical records of adults who presented with acute abdominal pain at Mayo Clinic Hospital ED over one calendar year (2014). Our specific aims were to appraise: the prevalence of opioid use for non-cancer pain; the demographic features among the entire group of patients; the nature of “surgical” and “non-surgical” diagnoses among the opioid and non-opioid users; risk factors for vascular emergencies.
MATERIALS AND METHODS
Study Design
We conducted a medical records-based, observational cohort study. A search was conducted using a natural language processing method [Advanced Cohort Explorer (ACE) tool developed by Mayo Clinic] using the terms “abdominal pain” and “Emergency Department” for all records during the calendar year 2014 which at the time of starting the study was the calendar year with complete data for ED presentation.
ACE is a clinical data repository which contains patient demographics, clinical notes, diagnoses, hospital records, laboratory and pathology results obtained from multiple clinical and hospital source systems within Mayo Clinic Rochester. If the patient presented on more than one occasion, we only analyzed the presentation that was associated with abdominal CT scan. We did not analyze any follow-up visits.
The study was reviewed and approved by Mayo Clinic Institutional Review Board (IRB #15-005454).
From the analyzed data, we used regression analysis, based on commonly available clinical and laboratory parameters, to predict the presence of surgical diagnoses and to propose a guidance to enhance the care of adult non-cancer patients presenting to the ED with acute abdominal pain.
Patient Eligibility Criteria
Presentation to the ED with chief complaint of abdominal/flank pain.
Adult patients (≥ 18 years).
CT of the abdomen or abdomen and pelvis within 24 hours of presentation to ED; CT scans were performed as a part of the work-up to diagnose the abdominal pain by the emergency department health care providers. The CT scans were reported blind to information on opioid use.
Absence of malignancy, except non-melanoma skin cancer.
Patients were excluded if their chief complaint at the time of presentation to the ED was not abdominal pain, or if they had past history of malignancy (as above), or if they did not undergo CT scan within 24 hours of presentation to the ED.
Search Strategy for Electronic Medical Records
From electronic medical records, we extracted information on age, gender, body mass index, chronic opioid use for chronic pain (≥ 3 months), history of constipation, laxative use, final diagnoses, use of μ-opioid receptor antagonists, contraindication to μ-opioid receptor antagonists, laboratory tests including hemoglobin, total white blood cell count, neutrophil count, serum levels of amylase and lipase (as screens for acute pancreatitis), total bilirubin, circulating liver enzymes, and creatinine, and reports of CT scans.
Since four investigators participated in data collection, this may have introduced observer bias. However, one investigator trained and demonstrated methods to be used to the team in order to assure consistency in the method of data collection. Most of the data collected in this study were dichotomous (Y or N, present or absent), demographic (age, gender, BMI), or diagnoses recorded in the medical record. The data collection by 4 investigators did not involve complex measurements or interpretations, which may have potential for bias. Therefore, there was low (if any) potential for bias in the data collection.
Patient Involvement
The retrospective observational study involved patients who had provided consent for using information in their electronic medical records for research purposes. We did not involve patients in the design, recruitment or conduct of this study. The results of this study will not be disseminated to the study population.
The development of the research question was based on the high prevalence of opioid use (~4%) for chronic non-cancer pain among adults in the United States and the clinical observation that such patients present with acute abdominal pain, increasing health care burden and costs. However, there is to date no information on the prevalence of chronic opioid use among non-cancer patients presenting for emergency medical care and no data on their diagnosis and risk factors for surgical conditions.
Definitions
Abdominal pain
This was defined as recorded in the medical history and included pain that was located in the abdomen or flank in the information provided by the patient.
Constipation
The presence of constipation was based on documentation by the health care provider in the medical history and/or evidence reported in the radiology records of colonic loading with fecal material on CT of the abdomen or abdomen and pelvis.
Chronic opioid analgesic use
Chronic opioid use for chronic non-cancer pain (≥3 months) was based on documentation in the medical record (provider note, medication list). If patients also received opioid medication in the ED, they were not excluded, as long as they fulfilled the eligibility criterion on chronic opioid use.
Final diagnoses
Final diagnoses were based on the diagnosis made by the health care provider and documented in the medical record during the acute presentation. Furthermore, the diagnoses were sub-classified for the purpose of this study as conditions that potentially required surgical intervention (summarized as “surgical diagnoses”) and those that did not (summarized as “non-surgical diagnoses”).
The list of conditions included as surgical diagnoses are shown partly in Table 1 and in the Supplemental Material. The non-surgical diagnoses are also detailed in Supplemental Material. Renal and ureteric calculi (summarized as kidney stones in the remainder of the manuscript) were classified as potentially requiring surgery.
Table 1.
Demographics and Surgical Diagnoses in Patients Presenting to ED with Non-Cancer Abdominal Pain in 2014, Based on Opioid Use
| Opioid users | Non-opioid users | |
|---|---|---|
| Number (N) | 442 | 1910 |
| Age, years (mean ± SEM) | 51.2 ± 0.9 | 50.1 ± 0.4 |
| Gender (female: male, %) | 65:35 | 56:44 |
| Constipation (%) | 35.1 | 15.8 |
| Diagnoses potentially requiring surgery$, N (%) | 156 (35.3) | 796 (41.7) |
| Vascular emergencies#, N (%) | 4 (0.9) | 21 (1.1) |
| Perforation, N (%) | 5 (1.1) | 33 (1.7) |
| Biliary pathology^, N (%) | 14 (3.2) | 69 (3.6) |
| Acute appendicitis, N (%) | 7 (1.6) | 113 (5.9) |
| Obstruction, N (%) | 38 (8.6) | 185 (9.7) |
| Renal stones, N (%) | 53 (12.0) | 261 (13.7) |
| Other Surgical diagnoses (N=149) (ovarian torsion, ovarian cystic hemorrhage, incarcerated hernia, incisional hernia, renal colic, anastomotic leak after end-colostomy, epiploic appendagitis, hepatic abscess, GI bleed, ischemic colitis) | 35 (7.9) | 114 (25.8) |
Vascular emergencies included abdominal aortic aneurysm (e.g. dissection), superior mesenteric artery pathology (occlusion or dissection), and thrombosis of superior mesenteric, ovarian or renal veins
Biliary pathology = acute cholecystitis or cholelithiasis
OR 0.77; 95% CI: 0.62, 0.96 (p=0.019)
Outcomes of Interest
The primary outcomes were:
prevalence of opioid analgesic use in the eligible patients with acute abdominal pain and
prevalence of constipation in opioid users or non-users at the time of presentation with acute abdominal pain.
The secondary outcomes were demographic features, surgical and non-surgical diagnoses, risk factors for vascular emergencies, and identification of factors that were associated with surgical diagnoses.
Statistical Analysis
Multivariate analyses were assessed using logistic regression (surgical emergency vs. non-surgical emergency) as the dependent variable, and, separately, constipation (no vs. yes) as the dependent variable. A further logistic model incorporating “just being constipated at presentation” and “opioid use” was also assessed. The overall odds ratio [OR (95% CI)] of being constipated at presentation with abdominal pain in chronic opioid users vs. non-opioid users was calculated. The univariate association with surgical diagnoses (Table 2) identified factors to be included in a logistic model adjusted for age and gender, since these were significantly associated with several other factors (see Results section) using features in the clinical history and laboratory tests: history of opioid use, presence of constipation, total white blood cell count, neutrophil count, and serum lipase. A separate logistic model was used to estimate the odds for acute appendicitis (in the surgical emergency subset) for opioid use adjusted for age and gender. Sensitivity analyses were performed with exclusion of kidney stones from the “surgical diagnosis” category.
Table 2.
Univariate Associations with Surgical Diagnoses
| Predictor | Number | Odds Ratio (95% CI)† | p-value |
|---|---|---|---|
| Age | 2352 | 1.01 (1.01,1.02) | <0.0001 |
| Gender | 2352 | 1.74 (1.47,2.06) | <0.0001 |
| Total WBC Count, thousands/μL | 2263 | 1.07 (1.05,1.09) | <0.0001 |
| Neutrophil Count, thousands/μL | 891 | 1.05 (1.02,1.09) | 0.003 |
| (log) Lipase, i.u/L | 1543 | 0.87 (0.78,0.98) | 0.023 |
| Chronic Opioid Use | 2352 | 0.78 (0.63,0.98) | 0.031 |
| Constipation | 2352 | 0.86 (0.69,1.06) | 0.164 |
| Body Mass Index, kg/m2 | 2096 | 1.00 (0.99,1.01) | 0.919 |
| Hemoglobin, g/dL | 2263 | 0.96 (0.92,1.01) | 0.114 |
| C-Reactive Protein, mg/dL | 140 | 1.00 (1.00,1.01) | 0.168 |
| Bilirubin, mg/dL | 448 | 0.99 (0.87,1.12) | 0.855 |
| Alanine Transaminase, iu/L | 406 | 1.00 (1.00,1.00) | 0.234 |
| Aspartate Transaminase, iu/L | 371 | 1.00 (1.00,1.00) | 0.232 |
| Serum Creatinine, mg/dL | 2126 | 1.03 (0.91,1.18) | 0.606 |
| Amylase, iu/L | 92 | 1.00 (0.99,1.01) | 0.485 |
Adjusted for age and gender using all subjects (N=2352); WBC= white blood count; values refer to measurements in blood or serum
The final models in the total cohort (overall and excluding those with renal stones) were applied to randomly selected subsets (overall and excluding renal stones) stratified on surgical emergency (vs. non-surgical emergency) and chronic use of opioids (no vs. yes).
In addition, a logistic model also examined the association of chronic opioid use and constipation to predict those with surgical diagnoses (vs. non-surgical diagnoses) overall and after excluding patients with a diagnosis of kidney stones.
Receiver operating characteristic (ROC) curves were plotted using the entire cohort to assess sensitivity and specificity for surgical (vs. non-surgical) diagnoses and, separately, for the model using just constipation and history of chronic opioid use, as well as a validation subset (25% of the entire cohort).
The Pearson goodness-of-fit statistic was used to assess the goodness of fit of the univariate association models assessing association of each parameter (adjusted for age and gender) with surgical diagnosis.
All analyses were done using SAS® software (Version 9.3, SAS, Inc., Cary, NC).
All authors had access to the study data and reviewed and approved the final manuscript.
RESULTS
Patient Identification, Demographics of Cohort
The natural language process search identified 16,121 patients during the year 2014. Of these patients, 2,354 met the eligibility criteria. Two patients with extra-abdominal cause of abdominal pain (epididymal cysts and pericardial effusion) were excluded; thus, there were 2,352 patients in the cohort studies. Mean age of patients was 50.1 years, with 57.6% (95% CI: 55.6 – 59.6) females and 42.4% males (95% CI: 40.4 – 44.4); 80.6% of the patients were from Minnesota, and 88.3% from Minnesota, Wisconsin or Iowa.
The demographic features of the two groups (Table 1) showed similar age, but higher proportion of females in each group. Age was significantly associated with hemoglobin, (log) lipase, AST (aspartate aminotransferase), bilirubin, and creatinine (all p<0.002). Gender was associated with chronic opioid use, hemoglobin, creatinine, total white blood cell (WBC) count, (log) lipase (all<0.001), and neutrophil count (p=0.001).
Indications for Opioid Use
Indications for chronic opioid use were: musculoskeletal pain (n=189), abdominal pain (n=93), others (n=160) including chronic pain syndromes, connective tissue disease, renal calculi. We found 0.9% (4/442) of patients with recurrent renal stones in the opioid users group. In this group of 4 patients, the diagnosis reached for the acute abdominal pain leading to ED visit was exclusively kidney stones.
Among the 442 opioid users, 3 patients were diagnosed with narcotic bowel syndrome, in addition to the other diagnoses revealed on CT scan. Of these 3 patients diagnosed with narcotic bowel syndrome, 2 were receiving opioids for the indication “abdominal pain”.
Prevalence of Opioid Use and Constipation
Of the 2,352 patients, 18.8% was opioid users. Constipation was more frequent in opioid (35.1%) compared to non-opioid (15.8%) users. The presence of constipation [19.4% (95% CI: 17.8, 21.1)] in non-cancer patients presenting to ED with acute abdominal pain was more frequent in opioid users [35.1% (95% CI: 30.6, 39.7)] compared to non-opioid users [OR 2.88 (95% CI: 2.28, 3.62); p<0.0001].
Surgical Diagnoses among Opioid and Non-opioid Users with Acute Abdominal Pain
Prevalence of surgical diagnosis in the opioid and non-opioid users was 35.3% and 41.7% respectively, and chronic opioid use significantly (p=0.019) was associated with lower risk of surgical diagnosis (OR 0.77; 95% CI: 0.62, 0.96).
The numbers of patients in the two groups (opioid users and non-opioid users) and the final diagnoses that were potential indications for surgery are shown in Table 1. Among the surgical diagnoses (n=952), the following 6 categories were observed in 803 patients: vascular emergencies, perforation, appendicitis, obstruction, biliary pathology, and renal stones (Table 1). Kidney stones were the most common surgical diagnosis (~13% in both opioid and non-opioid users). Vascular emergencies were observed with similar frequency (~1%) among opioid and non-opioid users (Table 1). Typically, at least one risk factor was associated with vascular emergencies in 23/25 patients: tobacco dependence (n=10), oral contraceptive treatment (n=1), obesity (n=4), diabetes mellitus (n=5), hypertension (n=16), hyperlipidemia (n=10), and coronary artery disease (n=5).
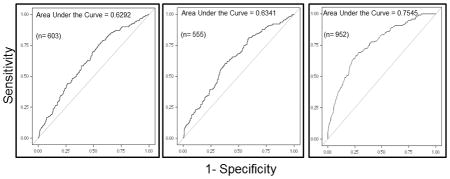
Although there were slightly lower percentages of all surgical diagnoses among opioid users compared to non-opioid users, the only significant association between opioid users and non-opioid users was a lower prevalence of acute appendicitis (Figure 2, right panel) (OR 0.33; 95% CI: 0.15, 0.74; p=0.007).
Figure 2.
Odds ratios (OR) with 95% Wald confidence intervals (CIs) for entire cohort showing factors associated with all surgical diagnoses (left), excluding kidney stones (middle), and only acute appendicitis (right).
In a similar model, after excluding renal stones among the diagnoses potentially requiring surgery in the remaining 2038 patients, chronic opioid use was also significantly associated with a lower likelihood of surgical diagnosis (OR 0.72; 95% CI: 0.56, 0.92; p=0.020).
Non-Surgical Diagnoses among Opioid and Non-opioid Users with Acute Abdominal Pain
Table 3 lists the categories of non-surgical diagnoses in patients presenting with acute abdominal pain. In 48%, the CT scan did not provide a diagnostic finding for the pain.
Table 3.
Non-Surgical Diagnoses in Opioid and Non-Opioid Users in Order of Frequencies
| N | Opioid Users | Non-Opioid Users | |
|---|---|---|---|
| Non-Surgical Diagnoses | 1400 | 285 | 1115 |
| Unexplained abdominal or flank pain; incidental CT findings | 401 | 91 | 310 |
| Negative CT scans | 277 | 63 | 214 |
| GI etiology (mesenteric and retroperitoneal lymphadenopathy, constipation, acute on chronic pain, peptic ulcer disease, IBS, hernia, hematoma) | 192 | 36 | 156 |
| Diverticulitis/Diverticulosis | 115 | 13 | 102 |
| Renal etiology (pyelonephritis, renal insufficiency, acute renal failure, urinary tract infection, hydronephrosis, renal cyst, hematuria, ureteritis, urosepsis) | 90 | 20 | 70 |
| Pancreatic pathology (pancreatitis, pancreatic cyst, pseudocyst, atrophy, cystic lesion, IPMN, pancreatic mass) | 87 | 22 | 65 |
| Infectious GI etiology (acute enteritis, ascites, colitis, C. Difficile colitis, colostomy infection, duodenitis, infectious diarrhea, ileitis, mesenteric adenitis, gastroenteritis, spontaneous bacterial peritonitis, pancolitis, gastroenteritis, gastritis, abscess, proctitis) | 86 | 10 | 76 |
| Reproductive organs (ovarian cyst, fallopian tube cyst, PID, uterine fibroids, corpus luteal cyst, adnexal mass, adnexal cyst, uterine infection, endometritis) | 55 | 4 | 51 |
| Post-operative/post-procedural pain | 42 | 12 | 30 |
| Inflammatory Bowel Diseases: | |||
| Crohn’s Disease | 27 | 7 | 20 |
| Ulcerative Colitis | 6 | 0 | 6 |
| Liver etiology (hepatic cyst, liver hemangioma, PSC, NASH) | 12 | 3 | 9 |
| Other causes (rib fracture, sickle cell crisis, costochondritis, Still’s disease, infectious mononucleosis, splenomegaly, splenic cyst) | 10 | 4 | 6 |
In thirty-five patients, constipation was considered to be the cause of their abdominal pain in the final diagnoses, based on the CT report and the medical records. Of these 35 patients, 6 were chronic opioid users.
Diagnoses in Patients Who Received Chronic Opioid Treatment for Abdominal Pain
The following were the diagnoses for the acute abdominal pain among the patients who were receiving chronic opioid treatment for the indication of abdominal pain (Table 4): bowel obstruction, cholecystitis, cirrhosis, colitis, constipation, Crohn’s disease, diverticulitis, enteritis, hiatal hernia, idiopathic abdominal pain, intussusception, ovarian cysts, pancreatic pseudocyst, pancreatitis, renal stones, sickle cell crisis, urinary tract infection and ventral hernia.
Table 4.
Final Diagnoses in Opioid Users based on Indications for Opioid Prescription
| Final Diagnosis | Indication for Chronic Opioid Use, N (%) | p-value | |
|---|---|---|---|
| Abdominal Pain (n=88) | Other Causes* (n=354) | ||
| Vascular emergency | 1 (1.14) | 3 (0.85) | 0.75 |
| Perforation | 0 (0) | 5 (1.41) | - |
| Biliary Pathology | 2 (2.27) | 12 (3.39) | 0.86 |
| Acute Appendicitis | 0 (0) | 7 (1.98) | - |
| Obstruction | 5 (5.68) | 33 (9.32) | 0.87 |
| Renal Stones | 4 (4.55) | 49 (13.84) | 0.92 |
| Other Surgical Diagnoses | 9 (10.23) | 26 (7.34) | 0.74 |
| Non-Surgical Diagnoses | 67 (76.14) | 219 (61.86) | 0.77 |
Chronic pain syndrome, musculoskeletal pain, connective tissue disorders and recurrent renal stones
It is worth noting that the general categories of diagnoses among these 88 patients were not significantly different from those of the other 354 patients who were also chronic opioid users (for the indications musculoskeletal pain, chronic pain syndromes, connective tissue disease, or recurrent renal calculi).
Univariate and Multivariate Models Predicting Surgical Diagnosis
In age- and sex-adjusted univariate logistic models (Table 2), age (p<0.001), gender (p<0.001), neutrophil count (p=0.003), total white blood cell count (WBC) (p<0.001), and (log) lipase (p=0.023) were factors associated with surgical diagnoses among presenters with abdominal pain. The Pearson goodness of fit model was not significant for any of the factors assessed, suggesting internal validity of the data. In the multivariate analyses, gender and total WBC were no longer significant (Figure 2, left panel).
Log lipase level was associated with lower risk of surgical diagnosis, but lipase was measured only in 53.6% (510/952) of the entire surgical diagnosis cohort.
Since kidney stones were the most common condition among the surgical diagnoses, we conducted an additional analysis after excluding subjects with kidney stones in order to appraise risk factors for the other surgical diagnoses. This analysis showed that age, neutrophil count, and (log) lipase were again significant (Figure 2, middle panel), as observed in the entire cohort (Figure 2, left panel).
Mathematical Models Predicting Surgical Diagnosis in Non-Cancer Patients Presenting with Acute Abdominal Pain
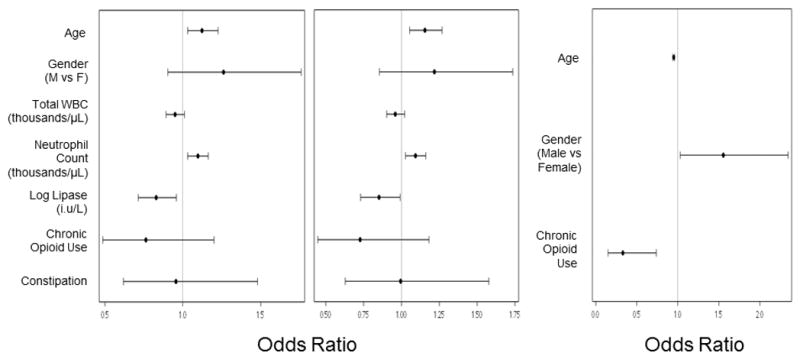
The logistic regression analysis results were used to develop a score that combined the factors to predict a surgical diagnosis, or a surgical diagnosis excluding kidney stones. Figure 3 shows the receiver operating characteristic (ROC) curves based on numbers of patients with complete data for the included parameters in the surgical diagnoses cohort (Figure 3, left panel, n=603), and those with surgical diagnosis excluding those with kidney stones (Figure 3, middle panel, n=555).
Figure 3.
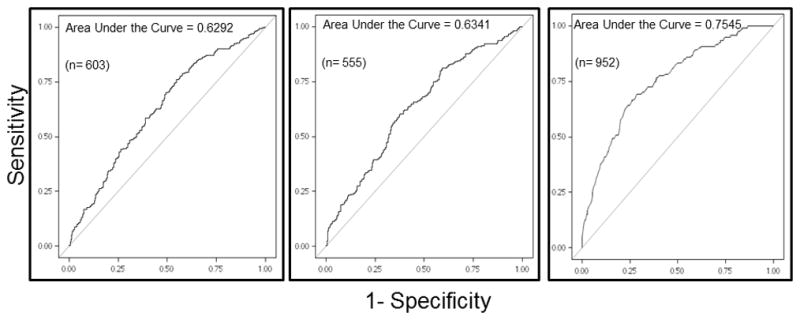
Receiver operating characteristic (ROC) curves from logistic regressions of the full model that included age, gender, total white blood cell count (WBC), neutrophil counts, (log) lipase value, history of opioid use and constipation to appraise risk factors associated with surgical vs. non-surgical diagnoses using entire cohort (left), entire cohort without diagnosis of kidney stones (middle), and the model that included age, gender and chronic opioid use to appraise risk factors associated with acute appendicitis in the group with surgical diagnoses (right).
The regression equation for predicting any surgical diagnosis from the surgical diagnoses cohort [ROCAUC = 0.629 (95% CI: 0.585, 0.674)] was:
A separate regression equation for predicting surgical diagnosis after excluding kidney stones from the entire cohort [ROC AUC= 0.634 (95% CI: 0.587, 0.681)] was:
Among the 952 patients with surgical diagnoses, information on age, gender and opioid use was available for all patients. In this group, the area under the ROC (Figure 3, right panel) using these three parameters was 0.752, suggesting that they were useful to appraise risk of acute appendicitis.
Validation of Mathematical Model Predicting Surgical Diagnosis
To further appraise the validity of these models for the entire cohort, we applied the models to a randomly selected validation subset (25% of the entire cohort, 587/2352) and generated ROC curves. The values of the ROCAUCs for the validation subset (n=587) were 0.57 with or without exclusion of patients with kidney stones, and these AUCs were not appreciably different from those of the entire abdominal pain cohort (n=2352, AUC-0.63).
DISCUSSION
Our analysis of adults who presented to a single center’s ED with acute abdominal pain and underwent CT of the abdomen or abdomen and pelvis within 24 hours shows that almost 19% of non-cancer patients were chronic opioid users and 35.1% of those patients were constipated. They were, thus, approximately three times as likely to be constipated compared to non-opioid users. Thus, whereas the reported background prevalence of chronic opioid use in the population is ~4%, chronic opioid use is almost 5 times more likely among those presenting with acute abdominal pain.
Opioid users were just as likely as non-opioid users to suffer from abdominal pain due to surgical diagnoses, with the exception of acute appendicitis which is more prevalent among non-opioid users. We did not identify risk factors for the higher prevalence of acute appendicitis in non-opioid users; conversely, we do not perceive (and can find no evidence in the literature) that opioid use protects against development of acute appendicitis. Among the opioid users, 15.4% had surgical diagnoses other than renal stones: vascular emergencies, perforation, acute cholecystitis, acute appendicitis or intestinal obstruction. Therefore, history of opioid use and of constipation does not exclude a surgical diagnosis as a whole category, indicating that it is important to screen patients who are receiving chronic opioid treatment for risk factors of vascular disease, as well as ensuring there are no signs suggesting mechanical intestinal obstruction or peritonitis.
As expected, higher age and neutrophil count (though not total WBC) were significantly associated with surgical emergencies. Nineteen of the 120 patients (15.8%) with acute appendicitis had constipation, suggesting that constipation may be a possible factor predisposing to the development of acute appendicitis, as documented in a few studies in the literature (11,12). Although there was an overall lower prevalence of acute appendicitis in opioid users in the current study, this should be confirmed with further prospective studies.
After excluding from the “surgical diagnoses” group those with renal stones (the vast majority of which were radiopaque and therefore could be identified on plain abdominal radiograph or by ultrasound, irrespective of stone composition), the history of opioid use and identification of constipation (which could be obtained from history or plain abdominal radiograph) predicted absence of surgical emergency with 69% sensitivity.
Almost 19% of eligible patients were on chronic opioid treatment for non-cancer pain. Since opioid use is a risk factor for constipation, our data suggest that the Bowel Function Index (13,14) may be useful to select patients for approved prescription therapies: methylnaltrexone, lubiprostone, combination oxycodone-naloxone, and naloxegol (15,16).
Limitations and Strengths
Limitations in our medical records-based study include: First, the retrospective nature of the study that led to some of the other tests (e.g. serum amylase and lipase) not being performed on all patients. However, the main objective test, which was CT of the abdomen or abdomen and pelvis, was required for eligibility. A second potential limitation was the reliance on the recorded radiological reports for all the 2,352 CT scans. The facts that the study was conducted at a single ED and the CTs were reported by full-time radiologists in a single department provide some measure of consistency of the observations reported. Identification of constipation was based on clinical documentation in the medical history or clinical diagnosis, and reports of CT of the abdomen or abdomen and pelvis provided by staff radiologists. Therefore, the estimated proportion of patients with constipation is regarded as a conservative prevalence estimate. A third potential limitation is that designation of opioid use was based on information in the medical record, since no chemical drug screen of urine was performed in those who were classified as opioid users. The estimate of opioid non-users is, therefore, a conservative estimate. The fact that less than 20% of diagnoses would be indications for emergency surgery (e.g. vascular catastrophe, perforation, intestinal obstruction, acute appendicitis) in the entire cohort selected for CT scan suggests that the cohort is representative of patients presenting with acute abdominal pain. However, it would be ideal, in future studies, to control for this potential bias towards patients who were more acutely unwell by including a comparison cohort of patients with acute abdominal pain who did not undergo CT.
Prior to our study, there was no documentation in the literature on the prevalence of chronic opioid use among non-cancer patients presenting with abdominal pain for emergency medical care. The study strengths include the large number (2,352 patients) evaluated at a single ED, strict eligibility criteria, the generalizability (since 80.6% of the total study population were from Minnesota, and 88.3% from the tri-states of Minnesota, Iowa and Wisconsin), and the use of electronic medical and radiological records. Moreover, the internal validation of the mathematical model to predict surgical diagnosis in a randomly selected subset of patients suggests the model is, indeed, valid, and that age, neutrophil count, lipase, and history of chronic opioid use are significant univariate predictors.
Summary
In adults without cancer presenting to the ED with acute abdominal pain, almost 19% were opioid users. Factors significantly associated with altered risk of surgical diagnoses are age, opioid use, and neutrophil count. Overall, our data suggest that evaluation of adults presenting to ED with acute abdominal pain should include recording the patient’s age, gender, history of chronic opioid use and constipation, total WBC and neutrophil count (17,18). Acute gastrointestinal surgical emergencies and vascular disease should also be considered in all patients, given that the prevalence of such conditions is similar in opioid and non-opioid users, and may potentially be fatal if unrecognized.
Our study leads to three proposed strategies that will require further prospective studies: first, an abdominal radiograph would be an appropriate first imaging assessment for identification of common conditions such as kidney stones, perforation or intestinal obstruction; second, a bedside ultrasound to rule out kidney stones should be performed; and third, in the absence of perforation or intestinal obstruction on clinical or radiographic assessment, treat the constipation identified by history and confirmed on the abdominal radiograph.
This approach may reduce radiation exposure (19) and health care costs. However, if these initial investigations do not provide a diagnosis, it is clear that some patients (e.g. retroperitoneal perforation, or those unable to stand for an erect abdominal radiograph because of pain) will require more advanced imaging, such as CT, ultrasound, or MRI (20, 21).
Figure 1.
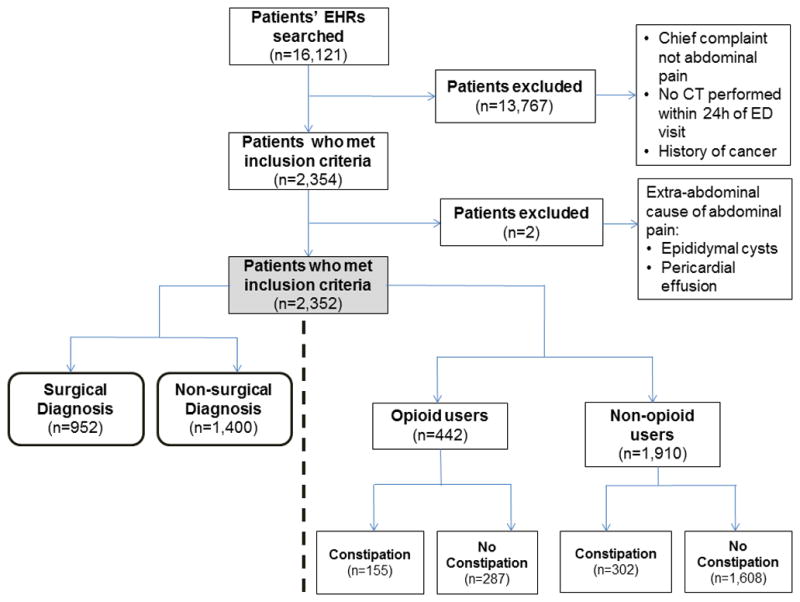
CONSORT flow chart reporting patient eligibility and exclusion.
KEY POINTS.
4% of adult U.S. population uses opioids chronically for non-cancer pain. We evaluated prevalence of chronic opioid use in over 2,300 adult patients who presented to one ED with acute abdominal pain and underwent abdominal CT imaging.
One-fifth were on chronic opioid therapy; constipation was more frequent in opioid vs. non-opioid users. Risk factors for surgical diagnoses among opioid users were identified.
In patients with acute abdominal pain in ED, constipation should be considered in the differential diagnosis.
Acknowledgments
Disclosures:
Dr. Camilleri, in the last two years, has served as a consultant or as an advisory board member or has received research funding as follows:
Dr. Camilleri has received research grants from:
National Institutes of Health, Tsumura, Rhythm, Vibrant, Entera Health, AstraZeneca, NPS Pharmaceuticals, Ferring, NovoNordisk
Dr. Camilleri has consulted for and received consulting fees from:
BioKier, Shionogi, Enterin, Forum
Dr. Camilleri has consulted for the following companies with the consulting fee going to his employer, Mayo Clinic:
Ironwood/Allergan, Takeda, Synergy, AstraZeneca, Shire, NPS Pharmaceuticals, Rhythm, Theravance, Lyric Pharmaceuticals, GlaxoSmithKline, Novartis, Elobix AB, Entera Health, Elira, EA Pharma, Relypsa
Dr. Acosta, in the last two years, has served as an advisory board member for Gila Therapeutics, Inversago, and General Mills. He holds stock in Gila Therapeutics, Inc.
The other authors have no competing interests.
Funding:
None
Abbreviations
- ACE
Advanced Cohort Explorer
- CT
Computed tomography
- ED
emergency department
- OR
Odds Ratio
- PAMORA
peripherally active μ-opioid receptor antagonist
Footnotes
Registration: This study was not a clinical trial; however, a CONSORT flow chart is included as a figure.
- Disha Khemani: data retrieval from electronic medical records, authorship
- Michael Camilleri: concept, design, interpretation, authorship of manuscript
- Ana Roldan: data retrieval from electronic medical records, authorship
- Alfred D. Nelson: data retrieval from electronic medical records, authorship
- Seon-Young Park: data retrieval from electronic medical records
- Andrés Acosta: data interpretation, authorship
- Alan R. Zinsmeister: biostatistics analysis
References
- 1.Sommers T, Corban C, Sengupta N, Jones M, Cheng V, Bollom A, Nurko S, Kelley J, Lembo A. ED Burden of constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110:572–9. doi: 10.1038/ajg.2015.64. [DOI] [PubMed] [Google Scholar]
- 2.Spangler R, Van Pham T, Khoujah D, Martinez JP. Abdominal emergencies in the geriatric patient. Int J Emerg Med. 2014;7:43. doi: 10.1186/s12245-014-0043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gardner JB, Fruauff AM, Bhalla S, Katz DS. Computed tomography of nontraumatic thoracoabdominal aortic emergencies. Semin Roentgenol. 2014;49:143–56. doi: 10.1053/j.ro.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Rubano E, Mehta N, Caputo W, Paladino L, Sinert R. Systematic review: ED bedside ultrasonography for diagnosing suspected abdominal aortic aneurysm. Acad Emerg Med. 2013;20:128–38. doi: 10.1111/acem.12080. [DOI] [PubMed] [Google Scholar]
- 5.Saini DK, Chaudhary P, Durga CK, Saini K. Role of multislice computed tomography in evaluation and management of intestinal obstruction. Clin Pract. 2013;3:e20. doi: 10.4081/cp.2013.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363:1981–5. doi: 10.1056/NEJMp1011512. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. [Accessed on Feb 26, 2016];CDC Vitalsigns - Opioid Painkiller Prescribing. 2014 at http://www.cdc.gov/vitalsigns/opioid-prescribing/.)
- 8.Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European Patient Survey (PROBE 1) Pain Med. 2009;10:35–42. doi: 10.1111/j.1526-4637.2008.00495.x. [DOI] [PubMed] [Google Scholar]
- 9.Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 2004;112:372–80. doi: 10.1016/j.pain.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, Wharam JF. Opioid prescribing after nonfatal overdose and association with repeated overdose: A cohort study. Ann Intern Med. 2016;164:1–9. doi: 10.7326/M15-0038. [DOI] [PubMed] [Google Scholar]
- 11.Arnbjornsson E. Acute appendicitis related to faecal stasis. Ann Chir Gynaecol. 1985;74:90–3. [PubMed] [Google Scholar]
- 12.Raahave D. Faecal retention: a common cause in functional bowel disorders, appendicitis and haemorrhoids--with medical and surgical therapy. Dan Med J. 2015;62 pii:B5031. [PubMed] [Google Scholar]
- 13.Argoff CE, Brennan MJ, Camilleri M, Davies A, Fudin J, Galluzzi KE, Gudin J, Lembo A, Stanos SP, Webster LR. Consensus recommendations on initiating prescription therapies for opioid-induced constipation. Pain Med. 2015;16:2324–37. doi: 10.1111/pme.12937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rentz AM, Yu R, Muller-Lissner S, Leyendecker P. Validation of the Bowel Function Index to detect clinically meaningful changes in opioid-induced constipation. J Med Econ. 2009;12:371–83. doi: 10.3111/13696990903430481. [DOI] [PubMed] [Google Scholar]
- 15.Camilleri M, Drossman DA, Becker G, Webster LR, Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary working group consensus statement on opioid-induced constipation. Neurogastroenterol Motil. 2014;26:1386–95. doi: 10.1111/nmo.12417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nelson AD, Camilleri M. Chronic opioid induced constipation in patients with nonmalignant pain: challenges and opportunities. Therap Adv Gastroenterol. 2015;8:206–20. doi: 10.1177/1756283X15578608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khemani D, Roldan A, Nelson AD, Park S-Y, Acosta A, Camilleri M. Prevalence of opioid analgesic use among patients presenting to emergency department with abdominal pain that is investigated with emergent abdominal CT scan. Gastroenterology. 2016;150:S192–3. [Google Scholar]
- 18.Khemani D, Camilleri M, Roldan A, Nelson AD, Park S-Y, Acosta A, Zinsmeister AR. Risk factors among patients presenting with acute abdominal pain at a single center and prediction score of surgical emergencies. Neurogastroenterol Motil. 2016;28(Suppl 1):39. doi: 10.1111/nmo.13000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cartwright S, Knudson M. Diagnostic imaging of acute abdominal pain in adults. Am Fam Physician. 2015;91:452–9. [PubMed] [Google Scholar]
- 20.Gangadhar K, Kielar A, Dighe MK, O’Malley R, Wang C, Gross JA, Itani M, Lalwani N. Multimodality approach for imaging of non-traumatic acute abdominal emergencies. Abdom Radiol (NY) 2016;41:136–48. doi: 10.1007/s00261-015-0586-6. [DOI] [PubMed] [Google Scholar]
- 21.Smith MP, Katz DS, Lalani T, Carucci LR, Cash BD, Kim DH, Piorkowski RJ, Small WC, Spottswood SE, Tulchinsky M, Yaghmai V, Yee J, Rosen MP. ACR Appropriateness Criteria® Right Lower Quadrant Pain--Suspected Appendicitis. Ultrasound Q. 2015;31:85–91. doi: 10.1097/RUQ.0000000000000118. [DOI] [PubMed] [Google Scholar]


