Abstract
Objective
Classic determinants of burn mortality are age, burn size, and the presence of inhalation injury. Our objective was to describe temporal trends in patient and burn characteristics, inpatient mortality, and the relationship between these characteristics and inpatient mortality over time.
Methods
All patients aged 18 years or older and admitted with burn injury, including inhalation injury only, between 2004 and 2013 were included. Adjusted Cox proportional hazards regression models were used to estimate the relationship between admit year and inpatient mortality.
Results
5,540 patients were admitted between 2004 and 2013. Significant differences in sex, race/ethnicity, burn mechanisms, total body surface area (TBSA), inhalation injury, and inpatient mortality were observed across calendar years. Patients admitted between 2011 and 2013 were more likely to be women, non-Hispanic White/Caucasian, with smaller burn size, and less likely to have an inhalation injury, in comparison to patients admitted from 2004 to 2010. After controlling for patient demographics, burn mechanisms, and differential lengths of stay, no calendar year trends in inpatient mortality were detected. However, a significant decrease in inpatient mortality was observed among patients with extensive burns (≥75% TBSA) in more recent calendar years.
Conclusions
This large, tertiary care referral burn center has maintained low inpatient mortality rates among burn patients over the past 10 years. While observed reductions in mortality during this time are largely due to changes in patient and burn characteristics, survival among patients with extensive burns has improved.
Keywords: burn centers, burns, mortality, risk factors
Introduction
Classic determinants of burn morbidity and mortality are age, total burn surface area (TBSA), and the presence of inhalation injury. Individuals at the extremes of age, larger sized burns, and with inhalation injury are at increased risk of complications and death. [1–5] These three risk factors are used to calculate the revised Baux score, a tool which predicts the probability of mortality in burn patients. [1] Over the past few decades, there have been numerous improvements in burn treatments, surgical critical care, a multi-disciplinary approach, and surgical interventions. [3, 6, 7] However, there is a paucity of information as to whether improvements in medical and surgical interventions over time have affected patient mortality, and if the effects of burn mechanisms and age have changed. The purpose of this study was to evaluate changes in patient demographics, burn characteristics, and inpatient mortality among adult patients admitted to a single care facility between 2004 and 2013, and the relationship between these characteristics and potential changes in inpatient survival over time.
Methods
Study Design and Population
Our cohort study was conducted using data from the North Carolina Jaycee Burn Center, a large, tertiary care referral burn center. All patients aged 18 years or older and admitted with burn injury, including inhalation injury only, between January 1, 2004 and December 31, 2013 were eligible for inclusion. Only a patient’s first hospitalization, for their first burn, within the time frame was included for analysis. Patients were identified using the Jaycee Burn Center registry, which consists of data collected on all admitted patients in real-time for reporting to the National Burn Repository. Registry data were validated using electronic medical records and manual chart review. Missing and illogical registry data were abstracted using similar methods. Patients were excluded if discharge date could not be determined (n=36). Institutional Review Board (IRB) approval was obtained from the University of North Carolina at Chapel Hill.
Data Analysis
The distribution of demographics, burn characteristics, and inpatient mortality were compared across time, categorized into tertiles by year (2004 – 2007, 2008 – 2010, and 2011 – 2013) using Kruskal Wallis and Chi-square two-tailed tests. Demographics and burn characteristics were also compared across inpatient mortality using Wilcoxon-Mann-Whitney tests and Fisher’s exact tests, where appropriate. A two-sided p-value of <0.05 was used to identify statistically significant differences across categories. Revised Baux scores were calculated using the methods described by Osler et al (2010). [1] Yearly inpatient mortality rates, per 100 hospitalization days, were calculated using Poisson regression. Additionally, 30-day cumulative inpatient mortality was calculated using Kaplan-Meier survival curves. Admit date was used to categorize patients by year.
Cox proportional hazards regression models were used to estimate the relationship between admit year tertile and inpatient mortality. A multivariable model was adjusted for patient age (modeled as a linear spline with knots at 30, 45, 60, and 75 years old), sex, race/ethnicity (non-Hispanic White/Caucasian, non-Hispanic Black/African-American, Hispanic and non-Hispanic other), burn mechanism (flame, scald, contact, and other), total burn surface area (modeled as a linear spline with knots at 20, 35, 50 and 65), and inhalational injury (present and absent). Potential confounding variables were selected based on previous burn research and clinical knowledge. The shape of age and total burn surface area (TBSA) were determined through functional form assessment. Because each component of the revised Baux score was included as a potential confounder, the score itself was not adjusted for in the multivariable models.
Additionally, to adjust for potential bias due to differential follow-up/hospitalization time across admit years, the multivariable Cox proportional hazards model described above was weighted using stabilized inverse probability of censor weights. [8] Briefly, the probability of being censored (i.e. discharged alive) was estimated for each patient using a multivariable logistic model, which was adjusted for admit year, patient age, sex, race/ethnicity, burn mechanism, TBSA, and inhalational injury. Weights were stabilized using the marginal (i.e. overall) probability of being censored, dependent on admit year tertile. Weights were truncated at 5% and 95% to adjust for inflated weights. After truncation, weights ranged from 0.93 to 1.06 (compared to 0.03 to 1006.86).
Effect measure modification assessment of the time-mortality relationship by burn size and inhalational injury was also conducted. Wald tests were used to identify significant modification. In order to visualize the estimated, marginal effect of TBSA on survival after adjustment, the predicted probability of 30-day inpatient mortality for each patient was averaged across each reported TBSA, and stratified by admit year tertile and inhalational injury status.
All statistical analyses were performed using SAS 9.4 (SAS Inc., Cary, NC).
Results
Between 2004 and 2013, 5,540 unique patients were admitted to the NC Jaycee Burn Center for burn injuries and included for analysis. Patient ages ranged from 18 to 95 years old. The number of patients treated each year steadily increased during this time, with 354 patients admitted in 2004 and 868 patients admitted in 2013. Significant differences in sex, race/ethnicity, burn mechanism, TBSA, inhalation injury, and revised Baux score were observed across time periods (Table 1). Over time, the admitted patient population has increased in the proportion of women and non-Hispanic White/Caucasians, and decreased in the proportion of flame injuries, inhalation injury, and median TBSA.
Table 1.
Distribution of demographics and burn characteristics among patients 18 years or older admitted to the NC Jaycee Burn Center between January 1, 2004 and December 31, 2013, stratified across time period.
| Patient Characteristics | 2004 – 2007 N=1,509 (27.2) |
2008 – 2010 N=1,591 (28.7) |
2011 – 2013 N=2,440 (44.0) |
p-valuea | |
|---|---|---|---|---|---|
| Sex, n (%) | |||||
| Male | 1,140 (75.6) | 1,141 (71.7) | 1,739 (71.3) | <0.01 | |
| Female | 369 (24.5) | 450 (29.6) | 701 (28.7) | ||
| Race/ethnicity, n (%) | |||||
| African American | 379 (25.1) | 437 (27.8) | 651 (28.4) | 0.07 | |
| Asian | 10 (0.7) | 10 (0.6) | 5 (0.2) | 0.07 | |
| Caucasian | 741 (49.1) | 898 (57.2) | 1,324 (57.7) | <0.01 | |
| Hispanic | 92 (6.1) | 112 (7.1) | 105 (4.6) | <0.01 | |
| Other | 287 (19.1) | 113 (7.2) | 209 (9.1) | <0.01 | |
| Unknown | 0 | 21 | 146 | - | |
| Age, in years, median (IQR) | 42.3 (30 – 54) | 42.5 (30 – 54) | 42.2 (29 – 55) | 0.81 | |
| Burn mechanism, n (%) | |||||
| Flame | 931 (61.2) | 849 (53.7) | 1,167 (47.9) | <0.01 | |
| Scald | 345 (23.0) | 484 (30.6) | 876 (36.0) | <0.01 | |
| Contact | 64 (4.3) | 70 (4.4) | 155 (6.4) | <0.01 | |
| Chemical | 61 (4.1) | 71 (4.5) | 103 (4.2) | 0.84 | |
| Radiation | 3 (0.2) | 5 (0.3) | 6 (0.3) | 0.81 | |
| Electrical | 82 (5.5) | 59 (3.7) | 77 (3.2) | <0.01 | |
| Other burn | 12 (0.8) | 44 (2.8) | 51 (2.1) | <0.01 | |
| Unknown | 11 | 9 | 5 | ||
| TBSA, median (IQR) | 7.0 (3 – 14) | 4.8 (2 – 10) | 3.0 (1 – 7) | <0.01 | |
| Baux score, median (IQR) | 53.2 (40 – 72) | 50.1 (37 – 65) | 47.7 (34 – 62) | <0.01 | |
| Inhalation injury, n (%) | |||||
| Yes | 213 (14.1) | 123 (7.7) | 130 (5.3) | <0.01 | |
| No | 1,296 (85.9) | 1,468 (92.3) | 2,309 (94.7) | ||
IQR=interquartile range, TBSA= Total Burn Surface Area
Chi-square and Kruskal Wallis tests were used to calculate p-values; p<0.05 are in bold
Overall, 4.4% of the cohort (n=243) died during their hospitalization. Crude analysis shows a statistically significant decrease in inpatient mortality rates over time, p=0.009, with an initial 7.3 deaths per 100 patients in 2004 (95% confidence interval [CI] 5.0, 10.8), compared to 3.1 deaths per 100 patients in 2013 (95% CI 2.1, 4.5) (Figure 1a). Inpatient mortality was higher in 2004–2007 compared to both 2008–2010 (hazard ratio [HR] 1.26, 95% CI 0.92, 1.71) and 2011–2013 (HR 1.43, 95% CI 1.05, 1.94) (Figure 1b).
Figure 1.
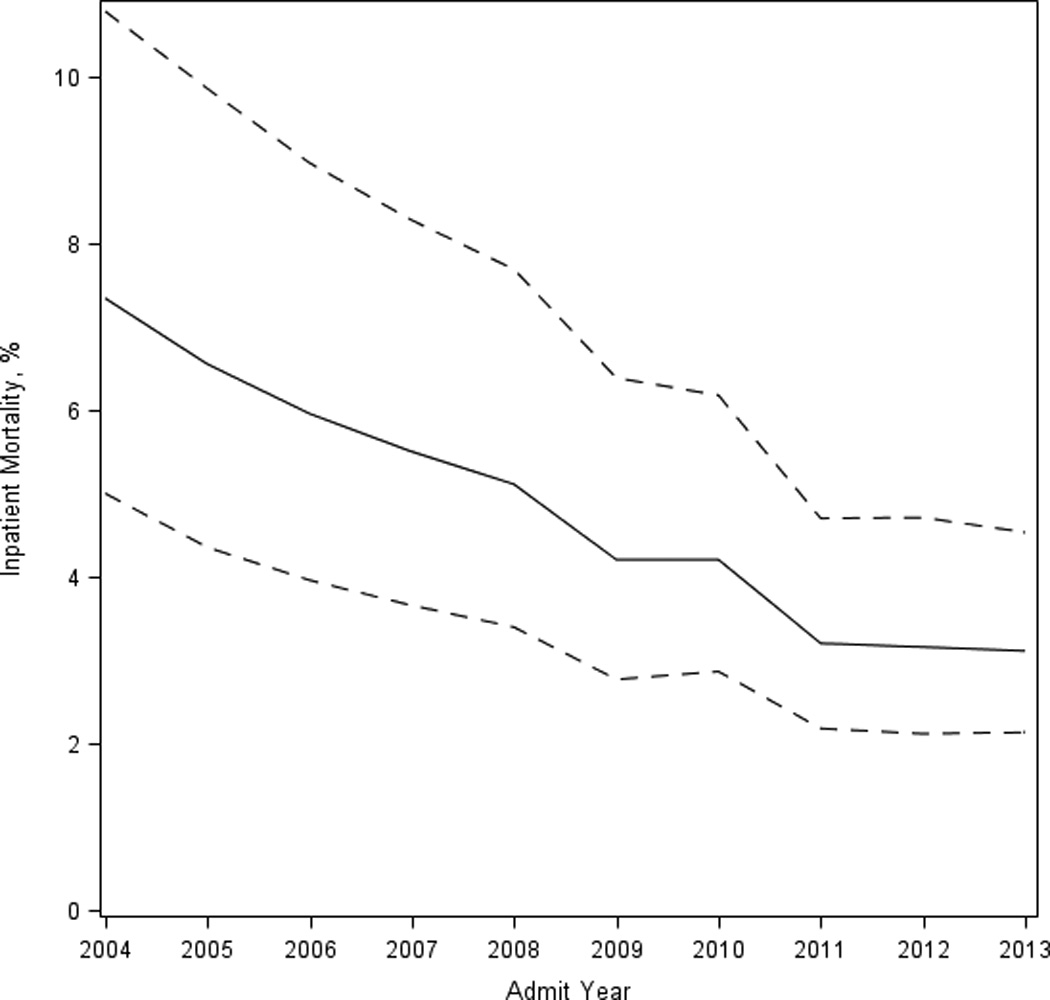
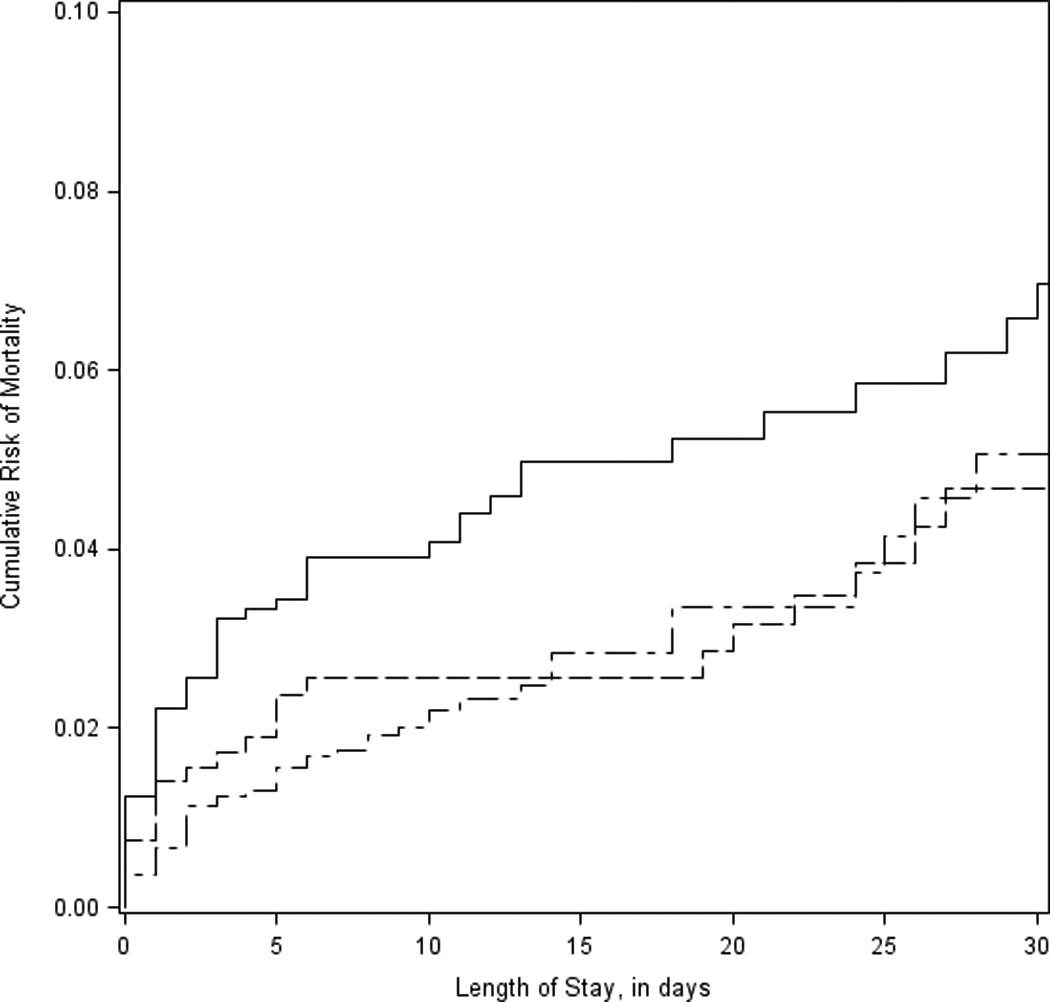
a. Unadjusted mortality rate per 100 patients and 95% confidence interval across admit year.
b. 30-day cumulative incidence of inpatient mortality during 2004–2007 (solid line), 2008–2010 (dashed line), and 2011–2013 (long-dashed line).
Mortality was significantly associated with admit year tertile, patient demographics, and burn characteristics (Table 2). Patients who died during hospitalization were more likely to be female, and older. Additionally, patients who died were more likely to have flame injuries, have more extensive burns, and have inhalation injury. While the median TBSA among patients that died was 34 (interquartile range [IQR] 17 – 64), deaths were observed across the entire spectrum of burn sizes (range 0 – 100). Twenty-five patients (10.3%) that died had a TBSA <6. Similarly, deaths were also observed across the entire age range of the cohort, 18 to 95 years old, and patients who died had a median age of 64 years old (IQR 51 – 77). Seventeen patients (7.0%) who died were under the age of 30, and 19.8% of deaths (n=43) were among patients ≥80 years old.
Table 2.
Distribution of demographics, burn characteristics, and length of stay, stratified across inpatient mortality.
| Patient Characteristics | Died N=243 (4.4) |
Survived N=5,297 (95.6) |
p-valuea | |
|---|---|---|---|---|
| Hospitalization year, n (%) | ||||
| 2004–2007 | 95 (39.1) | 1,414 (26.7) | <0.01 | |
| 2008–2010 | 71 (29.2) | 1,520 (28.7) | 0.86 | |
| 2011–2013 | 77 (31.7) | 2,363 (44.6) | <0.01 | |
| Gender, n (%) | ||||
| Male | 156 (64.2) | 3,864 (73.0) | <0.01 | |
| Female | 87 (35.8) | 1,433 (27.1) | ||
| Race/ethnicity, n (%) | ||||
| Caucasian | 121 (53.5) | 2,842 (55.3) | 0.62 | |
| African American | 60 (26.6) | 1,407 (27.3) | 0.79 | |
| Hispanic | 8 (3.5) | 301 (5.9) | 0.14 | |
| Asian | 0 (0) | 25 (0.5) | 0.62 | |
| Other | 37 (16.4) | 572 (11.1) | 0.01 | |
| Unknown | 17 | 150 | ||
| Age, in years, median (IQR) | 64.1 (51 – 77) | 41.4 (29 – 54) | <0.01 | |
| Burn mechanism, n (%) | ||||
| Flame | 212 (87.6) | 2,735 (51.9) | <0.01 | |
| Scald | 10 (4.1) | 1,695 (32.1) | <0.01 | |
| Contact | 6 (2.5) | 283 (5.4) | 0.05 | |
| Chemical | 1 (0.4) | 234 (4.4) | <0.01 | |
| Radiation | 0 (0) | 14 (0.3) | 0.99 | |
| Electrical | 6 (2.5) | 212 (4.0) | 0.23 | |
| Other burn | 7 (2.9) | 100 (1.9) | 0.24 | |
| Unknown | 1 | 24 | ||
| TBSA, median (IQR) | 34.0 (17 – 64) | 4.0 (2 – 9) | <0.01 | |
| Revised Baux score, median (IQR) | 109.7 (90 – 132) | 48.9 (35 – 63) | <0.01 | |
| Inhalation injury, n (%) | ||||
| Yes | 110 (45.5) | 356 (6.7) | <0.01 | |
| No | 132 (54.6) | 4,941 (93.3) | ||
| Length of stayb, median (IQR) | 8 (1 – 50) | 8 (2 – 14) | 0.01 | |
IQR=interquartile range, TBSA= Total Burn Surface Area
Fisher’s exact and Wilcoxon-Mann-Whitney tests were used to calculate p-values; p<0.05 are in bold
In days
After adjusting for patient characteristics, burn characteristics, and differential follow-up, there were no significant differences seen in mortality across admit tertiles, p=0.56 (Table 3). Patient characteristics that were significantly associated with mortality included race/ethnicity (p=0.005) and age (p<0.0001). The hazard of inpatient mortality among other race patients was almost 2 times higher (HR 1.68, 95% CI 1.12, 2.52) compared to non-Hispanic White/Caucasian patients. Older patients were more likely to die, with the likelihood increasing as patient age increased. Specific age comparisons are described in Table 3.
Table 3.
Estimated effect of admit year, patient demographics, and burn characteristics on inpatient mortality.
| Patient Characteristics |
Hazard Ratioa |
95% CI | p-value | |
|---|---|---|---|---|
| Admit year | ||||
| 2004 – 2007 | 1.21 | 0.85, 1.73 | 0.29 | |
| 2008 – 2010 | 1.15 | 0.79, 1.67 | 0.48 | |
| 2011 – 2013 | ref | - | ||
| Gender | ||||
| Male | 0.78 | 0.57, 1.06 | 0.11 | |
| Female | ref | - | ||
| Race/Ethnicity | ||||
| Caucasian | ref | - | ||
| African American | 0.78 | 0.56, 1.09 | 0.15 | |
| Hispanic | 1.66 | 0.79, 3.49 | 0.18 | |
| Other | 1.68 | 1.12, 2.52 | 0.01 | |
| Age, in yearsb | ||||
| 20 years old | ref | - | ||
| 30 years old | 0.86 | 0. 30, 2.46 | 0.77 | |
| 40 years old | 1.32 | 0.60, 2.91 | 0.49 | |
| 50 years old | 2.64 | 1.24, 5.63 | 0.01 | |
| 60 years old | 6.84 | 3.10, 15.11 | <0.0001 | |
| 70 years old | 12.12 | 5.61, 26.15 | <0.0001 | |
| Burn mechanism | ||||
| Flame | ref | - | ||
| Scald | 0.36 | 0.18, 0.72 | 0.004 | |
| Contact | 0.95 | 0.40, 2.30 | 0.91 | |
| Other burn | 1.53 | 0.85, 2.76 | 0.16 | |
| TBSAb | ||||
| 0% | ref | - | ||
| 20% | 3.44 | 1.73, 6.84 | 0.0004 | |
| 40% | 8.63 | 4.91, 15.17 | <0.0001 | |
| 60% | 19.62 | 10.79, 35.68 | <0.0001 | |
| Inhalation injury | ||||
| Yes | 1.53 | 1.12, 2.09 | 0.008 | |
| No | ref | - | ||
CI=Confidence interval, TBSA= Total burn surface area
All estimates are adjusted for patient and burn characteristics, including gender, race/ethnicity, age, burn mechanism, TBSA, and inhalation injury; stabilized inverse probability of censor weights were used to control differential follow-up/hospitalization time
Both age and TBSA were modeled as continuous variables
Burn mechanism (p=0.01), TBSA (p<0.0001), and inhalation injury (p=0.008) were also significantly associated with mortality (Table 3). Specifically, scald burns were associated with significantly lower hazard of mortality (HR: 0.36, 95% CI 0.18, 0.72) compared to flame burns, and neither contact nor other burn mechanisms (chemical, electrical, radiation, ‘other burn’) had significant differences in mortality compared to flame burns. Increases in TBSA increased inpatient mortality. For example, compared to a 0% burn size, a 20% TBSA increased mortality almost 3 times (HR 3.44, 95% CI 1.73, 6.84), a 40% TBSA increased mortality almost 9 times (HR 8.63, 95% CI 4.91, 15.17), and a 60% TBSA increased mortality almost 20 times (HR 19.62, 95% CI 10.79, 35.68) (Table 3). Patients with inhalational injury were 50% more likely to die during their inpatient hospitalization (HR 1.53, 95% CI 1.12, 2.09).
The risk of mortality over time was significantly modified by TBSA, p<0.001. Specifically, a decrease in risk in recent years was observed among patients with extensive burns (Figure 2). For example, compared to patients treated between 2011 and 2013 with 75% TBSA, patients treated between 2004 and 2007 with 75% TBSA were over 3 times more likely to die (HR 3.69, 95% CI 1.35, 10.16), and patients treated between 2008 and 2010 with 75% TBSA were over 2.5 times more likely to die (HR 2.82, 95% CI 0.9899, 8.14). While inhalational injury did not significantly modify the effect of admit year on survival, p=0.07, the results suggest that improvements in inpatient mortality only occurred among patients without an inhalational injury (Figure 2).
Figure 2.
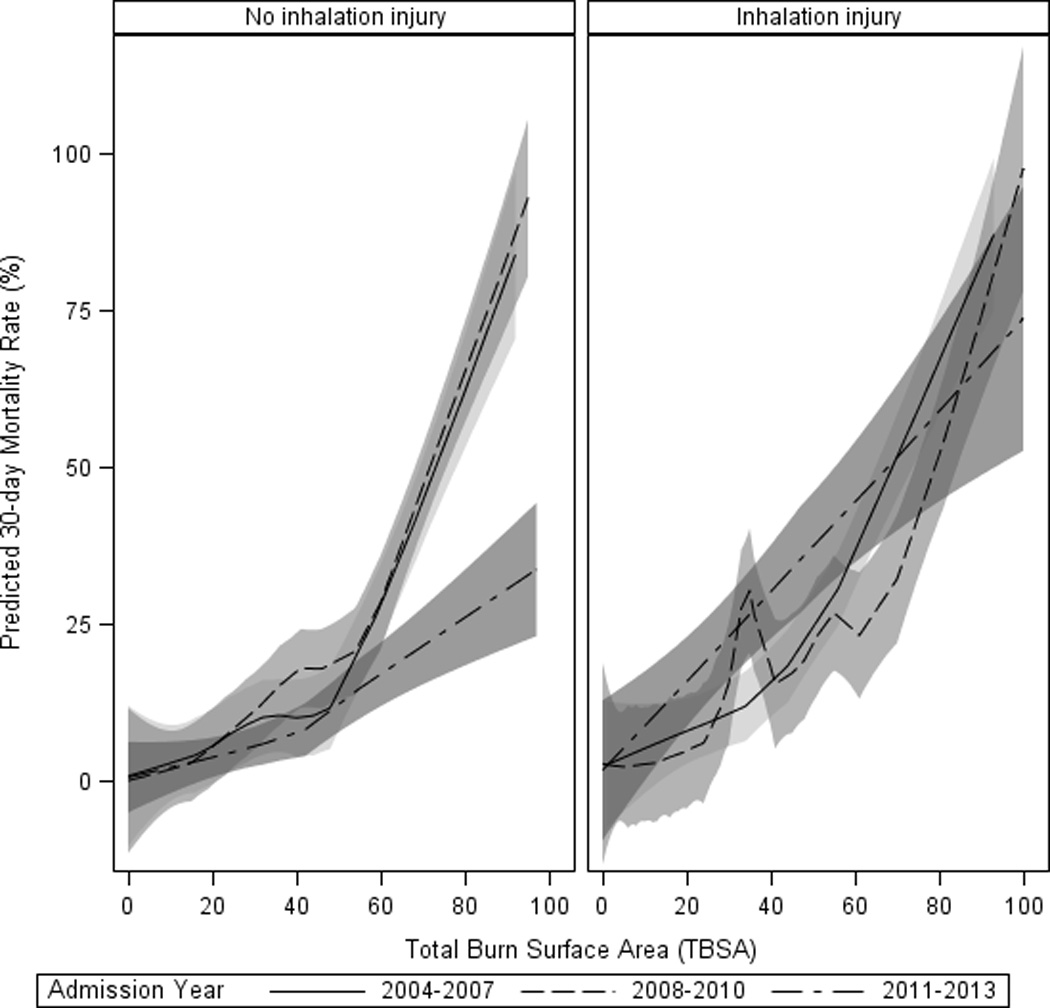
Predicted 30-day inpatient mortality rate (%) and 95% confidence interval in 2004–2007 (solid line), 2008–2010 (dashed line), and 2011–2013 (long-dashed line), across total burn surface area and stratified by inhalational injury status.
Discussion
This large, tertiary care referral burn center has maintained a low inpatient mortality rate for at least a decade. Moreover, a significant reduction in inpatient mortality among patients with extensive burns (≥75%) was observed in recent years (2011–2013). Despite this, the observed decrease in mortality between 2004 and 2013 was mostly explained by significant changes in the patient and burn characteristics of admitted individuals. In the past decade, adult patients admitted for burns are, on average, younger, have smaller burns, and present with fewer inhalational injuries, all of which are still significant predictors of mortality.
At least one other burn center has found similar findings in regards to low, but overall, unchanging mortality rates among their burn patients. Tompkins recently reviewed 70 years of burn center records from Massachusetts General Hospital, and found that among both adults and children, no significant reduction in mortality has been observed since 1984. [7] He further suggests that if survival rates have been maximized among this population, future research should turn its attention to the quality of life after survival from these injuries instead of mortality.
Determinants of mortality remain related to severity of injury, with larger burns and inhalational injury being significant factors, and increased age, even after adjusting patient characteristics and time. However, while both age and TBSA are assumed to be linear in their relationship to mortality (e.g. the change in risk between a TBSA of 20 and 40 is assumed to be the same as the change in risk between a TBSA of 60 and 80) when calculating the revised Baux score [1], we determined linear splines were a better fit for both age and TBSA on the risk of mortality. These findings suggest that more revisions to the revised Baux score are needed in order to improve predictability.
Advances in critical care, including early goal directed therapies, balanced fluid resuscitation, and early excision and grafting, have revolutionized burn care and improved survival. [9–12] Between 2004 and 2013, a significant reduction in inpatient mortality was observed among patients with extensive burns, and most at risk for morbidity and mortality. Extensive burns often lead to a profound and persistent hypermetabolic, hypercatabolic state, and patients are immunocompromised, at increased risk for infection, sepsis and multi-system organ failure. [13–15] However, these patients do not represent the majority of cases seen, and no changes in inpatient mortality were observed among patients with smaller burns. Further improvements in burn care may have little impact on those patients already likely to survive (i.e. those that require little if any resuscitation, those with very small burns, and those with no comorbidities). Other quality measures will need to be investigated for small burn injury survivors to discover ways to improve outcomes (i.e. scar satisfaction, quality of life, functional outcomes).
Our study suggests that improvements in inpatient mortality only occurred among patients without inhalational injury. The fact remains that inhalation injury increases the risk of mortality, whether or not one has a cutaneous injury, and there is no consensus across burn centers on the management of inhalation injury. While the pathophysiology of inhalation injury is better understood today, the clinical impact of a particular inhalation injury cannot be prognosticated based on the diagnosis or severity of injury found on admission. Inhalational injury increases the risk of pneumonia, which is the leading cause of death among burns patients. [16, 17]
The significant changes in “other” race are likely due to changes in race/ethnicity coding over time. That being said, further investigation is needed to account for the 2-fold increase in mortality in patients with “other” race compared to non-Hispanic White/Caucasian patients, even after other demographic and burn characteristic changes had been accounted for.
This study has a few limitations. First, only inpatient mortality was able to be analyzed in this study and represents only a portion of all deaths caused by burn injury. Future studies should focus on long-term morbidity and mortality outside of the initial hospitalization. Second, patients were observed for differing lengths of time, dependent on their inpatient length of stay, which is directly related to burn severity and year of admit, and could affect the results. However, inverse probability-of-censor weighting was used to account for the differential follow-up between patients in order to minimize potential bias.
Third, analyses were not adjusted for comorbidities, as they were not included in the burn registry until 2008. Studies have found that both the presence of comorbidities and the Charlson comorbidity score are associated with burn patient mortality.[18–20] Future research should both look into whether the number of comorbidities or specific comorbidity (e.g. diabetes) increases the risk of mortality. Finally, this analysis only includes one large, tertiary care facility and results may not be applicable to all burn hospitals, particularly if the patient population and burn characteristics differ.
Overall, this analysis presents insight into the changing demographics and burn characteristics among burn injury patients over the past decade. Significant reductions in mortality were only observed among patients with very large burns. This study provides further evidence that burn injury research should shift from inpatient mortality to long-term outcomes and quality of life measures, as survival is no longer the exception but the standard.
Acknowledgments
The authors would also like to thank Ali Fokar for his assistance with data management.
This project was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR001111. SWJ is supported by K08GM109106-02 (NIGMS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1.Osler T, Glance LG, Hosmer DW. Simplified estimates of the probability of death after burn injuries: extending and updating the baux score. J Trauma. 2010;68(3):690–697. doi: 10.1097/TA.0b013e3181c453b3. [DOI] [PubMed] [Google Scholar]
- 2.Ryan CM, Schoenfeld DA, Thorpe WP, et al. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338(6):362–366. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 3.Santaniello JM, Luchette FA, Esposito TJ, et al. Ten year experience of burn, trauma, and combined burn/trauma injuries comparing outcomes. J Trauma. 2004;57(4):696–700. doi: 10.1097/01.ta.0000140480.50079.a8. discussion 700–691. [DOI] [PubMed] [Google Scholar]
- 4.Miller SF, Bessey PQ, Schurr MJ, et al. National Burn Repository 2005: a ten-year review. J Burn Care Res. 2006;27(4):411–436. doi: 10.1097/01.BCR.0000226260.17523.22. [DOI] [PubMed] [Google Scholar]
- 5.Palmieri TL, Przkora R, Meyer WJ, 3rd, et al. Measuring burn injury outcomes. Surg Clin North Am. 2014;94(4):909–916. doi: 10.1016/j.suc.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 6.Pereira C, Murphy K, Herndon D. Outcome measures in burn care. Is mortality dead? Burns. 2004;30(8):761–771. doi: 10.1016/j.burns.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Tompkins RG. Survival from burns in the new millennium: 70 years' experience from a single institution. Ann Surg. 2015;261(2):263–268. doi: 10.1097/SLA.0000000000000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cole SR, Hernan MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–664. doi: 10.1093/aje/kwn164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenhalgh DG. Burn resuscitation: the results of the ISBI/ABA survey. Burns. 2010;36(2):176–182. doi: 10.1016/j.burns.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Janzekovic Z. A new concept in the early excision and immediate grafting of burns. J Trauma. 1970;10(12):1103–1108. [PubMed] [Google Scholar]
- 11.Lu J, Wang X, Chen Q, et al. The effect of early goal-directed therapy on mortality in patients with severe sepsis and septic shock: a meta-analysis. J Surg Res. 2016;202(2):389–397. doi: 10.1016/j.jss.2015.12.048. [DOI] [PubMed] [Google Scholar]
- 12.Tricklebank S. Modern trends in fluid therapy for burns. Burns. 2009;35(6):757–767. doi: 10.1016/j.burns.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Herndon DN, Tompkins RG. Support of the metabolic response to burn injury. Lancet. 2004;363(9424):1895–1902. doi: 10.1016/S0140-6736(04)16360-5. [DOI] [PubMed] [Google Scholar]
- 14.Jeschke MG, Chinkes DL, Finnerty CC, et al. Pathophysiologic response to severe burn injury. Ann Surg. 2008;248(3):387–401. doi: 10.1097/SLA.0b013e3181856241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kraft R, Herndon DN, Al-Mousawi AM, et al. Burn size and survival probability in paediatric patients in modern burn care: a prospective observational cohort study. Lancet. 2012;379(9820):1013–1021. doi: 10.1016/S0140-6736(11)61345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGwin G, Jr, George RL, Cross JM, et al. Improving the ability to predict mortality among burn patients. Burns. 2008;34(3):320–327. doi: 10.1016/j.burns.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Pham TN, Kramer CB, Klein MB. Risk factors for the development of pneumonia in older adults with burn injury. J Burn Care Res. 2010;31(1):105–110. doi: 10.1097/BCR.0b013e3181cb8c5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heng JS, Clancy O, Atkins J, et al. Revised Baux Score and updated Charlson comorbidity index are independently associated with mortality in burns intensive care patients. Burns. 2015;41(7):1420–1427. doi: 10.1016/j.burns.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Lundgren RS, Kramer CB, Rivara FP, et al. Influence of comorbidities and age on outcome following burn injury in older adults. J Burn Care Res. 2009;30(2):307–314. doi: 10.1097/BCR.0b013e318198a416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thombs BD, Singh VA, Halonen J, et al. The effects of preexisting medical comorbidities on mortality and length of hospital stay in acute burn injury: evidence from a national sample of 31,338 adult patients. Ann Surg. 2007;245(4):629–634. doi: 10.1097/01.sla.0000250422.36168.67. [DOI] [PMC free article] [PubMed] [Google Scholar]


