Abstract
Background
The current functional guidelines recommend the shuttle walk test (SWT) as an initial screening tool to identify candidates for lung resection without requiring cardiopulmonary exercise testing. This study aims to: (I) assess the use of the SWT in predicting postoperative cardiopulmonary complications; and (II) determine whether the recommended 400 m cut-off is an appropriate distance.
Methods
We retrospectively analysed 101 patients that had performed a SWT prior to surgery. Univariate and multivariate regression analyses were used to test associations between patient variables [demographics, pre-existing conditions, pulmonary function, oxygen desaturation during the SWT, shuttle walk distance (SWD)] and post-operative cardiopulmonary complications.
Results
Patients without cardiopulmonary complications walked longer distance compared to those with complication (417.3 vs. 348.6 m, P=0.01. Fifty two patients walked less than 400 m and 16 less than 250 m. Only 10% of patients who walked at least 400 m had cardiopulmonary complications compared to 33% of those who did not reach this distance (P=0.008). Half of the patients who walked less than 400 m and desaturated during the exercise developed cardiopulmonary complications. A SWD shorter than 400 m remained the only factor significantly associated with cardiopulmonary complications (P=0.009, OR: 4.3) after logistic regression analysis.
Conclusions
Our results support the use of the SWT as an initial screening tool in all patients prior to lung resection. Patients walking longer than 400 m experienced very low incidence of complications and would not need further testing prior to proceed to lung resection.
Keywords: Shuttle walk test (SWT), exercise test, lung surgery, lung cancer, complications
Introduction
Exercise testing is frequently used during the functional assessment of the lung resection candidate.
The cardiopulmonary exercise test (CPET) is considered the gold standard assessment tool in the most recent guidelines (1,2). This refined physiological test is capable to determine the patient’s maximum oxygen uptake (VO2max) and to precisely assess the cardiovascular and respiratory systems, identifying the nature of any present deficits.
However, the resources and trained professionals required to perform CPET are not always readily available and the test is time-consuming and expensive. Therefore, other simpler screening exercise tests have been considered such as the stair climbing test and shuttle walk test (SWT) (3). In particular, there has been an emphasis on walking tests that more naturally reflect an individual’s daily activity. These tests require considerably less technical expertise and equipment than the CPET.
The SWT was developed in 1992 and found to be effective at assessing functional capacity in individuals with chronic airway obstruction. The test was considered reproducible and valid (4). The SWT requires the patient to walk between two cones 10 m apart at an incrementally increasing pace (5). The test is considered easy to perform in any environment, requiring little equipment and minimal staff training (6).
Recent European and American guidelines (1,2) have included the SWT in their functional algorithms to evaluate the lung cancer candidates prior to radical treatment. In general these guidelines state that SWT can be used as a screening low technology exercise test in all patients with abnormal pulmonary function [either forced expiratory volume in one second (FEV1) or carbon monoxide lung diffusion capacity (DLCO) <80% predicted value or predicted postoperative FEV1 or DLCO <60%]. If the distance walked during SWT is shorter than 400 m then the patient should be referred for a formal CPET to detect the deficit in their oxygen transport system.
In this context, the primary aims of this study were to: (I) assess the use of the SWT in predicting postoperative cardiopulmonary complications; and (II) determine whether the recommended 400 m cut-off value is an appropriate distance to be used to select those patients who will not need additional testing prior to lung resection.
Methods
Patient selection
We retrospectively reviewed the electronic medical records of 707 patients who had undergone anatomic pulmonary resection for the treatment of lung cancer in the Leeds Teaching Hospital Trust from April 2014 to July 2016. One hundred and eighteen patients were identified as having performed a SWT within 4 months of surgery as part of their preoperative assessment. Unlike pulmonary function test, SWT is not performed routinely in our center and is generally requested at the discretion of the chest physicians at the referring hospitals. This explains the low proportion of patients with this test available amongst those operated during the same period.
In accordance with Win et al. (5), patients with recent myocardial infarction (within 6 weeks), unstable angina, and musculoskeletal conditions that might physically impede their performance were excluded (n=8) from the study. In addition, we also excluded patients that had terminated their SWT due to other musculoskeletal reasons such as abnormal gait (n=9). A total of 101 patients (mean 65.5 years; range, 19–85 years) were analysed. The study was reviewed by the Research and Innovation Department of our hospital, which waived NHS Research Ethics Committee and classified it as service evaluation.
All patients were operated by Board certified thoracic surgeons either through a muscle sparing thoracotomy or video-assisted thoracoscopic approach.
Patients were selected for operation according to current functional guidelines and after discussion during a multidisciplinary tumour board meeting (1). All patients in this series were judged to be in haemodynamically stable conditions before surgery. No patient underwent prophylactic invasive cardiologic procedures before surgery. After surgery, patients were cared in a high dependency unit for the first 24 hours and then transferred to a dedicated thoracic surgery ward unless clinically contraindicated. Patients were managed according to standardized pathways of care including early as possible mobilization, venous thromboembolic prophylaxis, physical rehabilitation. Surgical pain was managed with a combination of intravenous patient controlled and local paravertebral analgesia.
The SWT
Singh et al. outlined how to perform the SWT in their study (4). Patients walked at an incrementally increasing pace between two cones placed 10 m apart with each speed increment signalled by a “beep” from a fully calibrated audiocassette. The end point was reached when the patient could no longer maintain the required speed or became too breathless to proceed further. A pulse oximeter was used to record oxygen saturation and heart rate every 30 seconds throughout the test.
Data analysis
Data extraction
Patient data was extracted from the electronic records, anonymised and collated in a new dataset. Patient variables included in the dataset were: age, gender, type of lung resection, pre-existing medical conditions, shuttle walk distance (SWD), degree of desaturation during SWT, pre-operative FEV1, pre-operative DLCO% and major postoperative complications. In accordance with the joint definition of terminology and variables agreed by the Society of Thoracic Surgeons and the European Society of Thoracic Surgeons (7), the following major cardiopulmonary complications that had occurred within 30 days post-operatively were considered: pneumonia, respiratory failure requiring at least 24 hours mechanical ventilation, atelectasis requiring bronchoscopy, adult respiratory distress syndrome (ARDS), acute myocardial ischemia (MI) and atrial fibrillation (AF) requiring medical therapy or electric cardioversion, pulmonary embolism, pulmonary edema, stroke. Due to small numbers of events (only one case in this series), 30-day mortality was not analysed separately but instead grouped together with major cardiopulmonary complications.
Statistical analysis
Several patient-related and surgical variables were tested for possible association with the occurrence of cardiopulmonary complications. Numeric variables were compared by means of unpaired t test or Mann Whitney test in case of non-normal distribution. Categorical variables were tested by means of the Chi-squared test or Fisher’s exact test (in case the number of observations was less than 10 in at least one cell).
The following variables were initially screened by univariable analysis: age, gender, FEV1%, DLCO%, history of coronary artery disease (CAD), previous stroke or TIA [cerebrovascular disease (CVD)], presence of diabetes mellitus, pneumonectomy (vs. lesser resections), video assisted thoracoscopic surgery (VATS) (as opposed to thoracotomy), and SWD. SWD was classified according to cut off values reported in the literature (<250 and <400 m) (1,2,5,8). In addition, an exercise oxygen desaturation of greater than or equal to 4% was also used as a further factor in combination with the distinct SWD classes. In this way, the following SWD categories were used as patient variables: “SWD <250 m”; “SWD <400 m”; “SWD <250 m and desaturated”; “SWD <400 m and desaturated”.
Variables with P<0.1 at univariable analysis were subsequently used as independent variables in a stepwise logistic regression analysis (dependent variable: major cardiopulmonary complications). Highly correlated variables were not used in the same model to prevent problems of multicollinearity. In this regard, the different SWD categories were tested in separate regression analyses. Stepwise regression was performed with backward elimination of variables. Variables with P<0.1 were retained in the final model. ROC analysis was then used to test which variable had the highest association with an outcome of major cardiopulmonary complications.
All statistical analysis was performed using SPSS Statistics for Windows (SPSS Statistics version 22, SPSS Lead Technologies, Chicago, IL, USA).
Results
The patients’ baseline characteristics are shown in Table 1.
Table 1. Baseline characteristics of the patients included in the analysis (101 patients).
| Variables | Values |
|---|---|
| Gender, male (n) | 38 |
| Age (years) | 65.4 (11.6) |
| Diabetes (n) | 8 |
| COPD | 9 |
| CAD (n) | 9 |
| FEV1 | 90.8 (21.8) |
| DLCO% | 73.3 (17.2) |
| Distance at SWT (m) | 402.4 (155.0) |
| Pneumonectomy (n) | 12 |
| VATS | 79 |
Results are expressed as means and standard deviations for numeric variables and as count for categorical variables. COPD, chronic obstructive pulmonary disease; CAD, coronary artery disease; FEV1, forced expiratory volume in one second; DLCO%, carbon monoxide lung diffusion capacity; SWT, shuttle walk test; VATS, video assisted thoracoscopic surgery.
The overall rate of postoperative cardiopulmonary complications was 21.8% (n=22). Pneumonia (14.9%) and atelectasis requiring bronchoscopy (5.9%) were the two most common complications in this series. There was only one case of mortality (Table 2).
Table 2. Breakdown of the different major cardiopulmonary complications that occurred within 30 days post-operatively.
| Outcomes | N (%) |
|---|---|
| Any major complication | 22 (21.8) |
| Death | 1 (1.0) |
| Pneumonia | 15 (14.9) |
| Atelectasis | 6 (5.9) |
| AF | 5 (5.0) |
| Respiratory failure | 2 (2.0) |
| MI | 1 (1.0) |
| ARDS | 2 (2.0) |
Percentages are from the total 101 patients used in the study. AF, atrial fibrillation; MI, myocardial infarction; ARDS, acute respiratory distress syndrome.
The mean distance walked by patients who did not develop any major cardiopulmonary complications was 417.3 m (95% CI: 385–450). This value was on average 69 m longer than the distance achieved by patients who developed complications [348.6 m (95% CI: 268–429), P=0.01].
The incidence of complications was inversely related to the distance walked during SWT (Figure 1).
Figure 1.
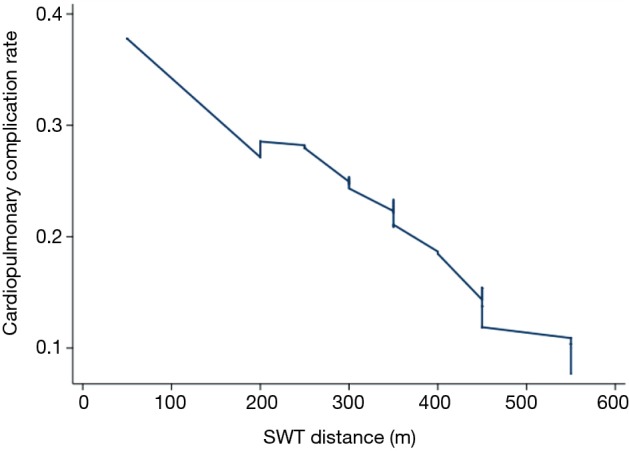
Lowess smoothing plot of the incidence of cardiopulmonary complications with the patients ordered by distance walked during shuttle walk test (SWT).
Table 3 describes the results of the univariable comparison of variables between patients with and without complications. The presence of diabetes was associated with a higher rate of major complications (P=0.07). Indeed, 50% of patients with diabetes experienced complications in this series. There was no significant relationship between major complications and gender, CAD, CVD, extent of operation, surgical approach or desaturation upon SWT (all comparisons had a P value greater than 0.1).
Table 3. Results of the univariable comparison between complicated and non-complicated patients.
| Variables | Complicated (22 patients) | Non-complicated (79 patients) | P values |
|---|---|---|---|
| Age | 70.7 (10.5) | 64.0 (11.6) | 0.008 |
| Male gender (n, %) | 8 (36.0) | 30 (38.0) | 0.900 |
| FEV1% | 90.8 (23.2) | 90.8 (21.7) | 0.900 |
| DLCO% | 70.8 (20.0) | 73.9 (16.6) | 0.500 |
| Diabetes (n, %) | 4 (18.0) | 4 (5.0) | 0.070 |
| CAD (n, %) | 3 (14.0) | 5 (6.3) | 0.400 |
| CVD (n, %) | 0 | 2 (2.5) | 1.000 |
| SWD (m) | 348.6 (182.0) | 417.3 (145.0) | 0.010 |
| Pneumonectomy (n, %) | 3 (14.0) | 9 (11.0) | 0.700 |
| Thoracotomy (n, %) | 5 (23.0) | 17 (22.0) | 0.900 |
Results are expressed as means and standard deviations for numeric variables and as number and percentages for categorical ones. FEV1, forced expiratory volume in one second; CAD, coronary artery disease; CVD, cerebrovascular disease; DLCO%, carbon monoxide lung diffusion capacity; SWD, shuttle walk distance.
Patients with complications were older than those without (P=0.008). However, pulmonary function (FEV1 and DLCO%) was similar between patients with and without complications in this series (FEV1, P=0.9; DLCO%, P=0.5).
In total 52 patients (51%) walked less than 400 m and 16 less than 250 m (16%).
Patients who walked less than 250 m had a 2.5-fold higher rate of major cardiopulmonary complications than patients who were able to walk at least 250 m (44% vs. 18%, P=0.04). Patients who were able to achieve at least 400 m at SWT had a 10% incidence of cardiopulmonary complications. This incidence was 3-fold lower than in patients who walked shorter than 400 m (33%, P=0.008).
Thirty patients experienced an oxygen desaturation greater than 4% during SWT. Desaturation alone was not associated with significantly increased incidence of complications (30% vs. 18%, P=0.2). However, when analysed in combination with the distance walked during the test it became a strong risk factor. Half of the patients who were not able to walk at least 400 m and desaturated during the exercise developed cardiopulmonary complications. This rate was significantly higher than any other combination of distance with or without desaturation (16%, P=0.006). For instance, 14 of the 49 patients who walked at least 400 m desaturated more than 4%, but only 1 of them developed complications, a proportion similar to the one observed in patients without desaturation and who walked at least 400 m or longer (7.1% vs. 11.4%, P=0.9).
Patients who had a “SWD <250 m and desaturated” (n=4) had the highest rate of a major cardiopulmonary complication (75%) in comparison to all other patient variables analysed. These patients also had a 55.4% higher rate of major complications when compared to patients that had a “SWD ≥250 m and/or no desaturation” (n=97, 19.6% had major complications, P=0.009).
Stepwise logistic regression analysis
The two SWD cut off values of 400 and 250 m were used as independent predictors in separate stepwise logistic regression analyses along with those factors selected from univariable analysis (age and diabetes).
A SWD less than 250 m did not remain significantly associated with cardiopulmonary complications after adjusting the analysis for the other confounders.
On the other hand, a SWD shorter than 400 m remained the only factor significantly associated with cardiopulmonary complications (P=0.009, OR: 4.3, 95% CI: 1.4–12.7).
Finally, we tested the variable SWD less than 400 m combined with oxygen desaturation in a regression analysis. This factor remained significantly associated with outcome (OR: 4.7, 95% CI: 1.4–15.9, P=0.01) along with age (OR: 1.05, 95% CI: 0.99–1.1, P=0.06) and diabetes (OR: 4.6, 95% CI: 0.94–22.3, P=0.06).
ROC analysis revealed that the best model associated with cardiopulmonary complications was then one containing the variable “SWD <400 m and desaturation” (AUC 0.67).
Among the patients with SWT and included in this study, 25 patients underwent CPET as part of their pre-operative evaluation. Eight patients had a VO2max<15 mL/kg/min and 17 patients achieved a VO2max>15 mL/kg/min. Ninety one percent of the patients with a VO2max >15 mL/kg/min also achieved a SWD >400 m. Of the patients who had a lower VO2max, only one actually walked longer than 400 m at SWT.
Discussion
Background
SWT is one of the low technology tests that has been recommended as first line exercise screening test in the most recent functional guidelines (1,2). In particular, the recent ACCP guidelines recommend the use of SWT or stair climbing test in patients with ppoFEV1 or ppoDLCO lower than 60% of predicted values (1). If the distance walked at SWT is less than 400 m then a formal CPET is recommended to detect the cause of the poor performance. However, this recommendation is based on few and contradictory studies.
In 2004, Win and colleagues analyzed 111 patients submitted to lung resection and who had SWT prior to surgery. They found that 66% of those walking less than 250 m developed poor postoperative outcome defined as death or major complications. On the other hand, only 29% of those walking more than 400 m developed poor outcome. Nevertheless the average distance walked by those with poor outcome did not differ from the one walked by those with good outcome. For this reason the authors concluded that SWT was not a useful test to select patients for operation (5). The same group published another study comparing the distance walked at SWT with the oxygen consumption measured during CPET (8). They found that all 55 patients who walked more than 400 m had a VO2max greater than 15 mL/kg/min at CPET. However, only 31% of patients who did not reach at least 400 m at SWT had a VO2max <15 mL/kg/min. In addition, 53% of the patients who were not able to walk at least 250 m had VO2max >15 mL/kg/min and 94% of them had a VO2max >10 mL/kg/min. The authors concluded that although SWT appears to be correlated with VO2max, this test tends to underestimate exercise capacity at the lower range compared with VO2max. Therefore, in patients who fail to reach 400 m a CPET would be recommended to assess their functional reserve before operation. On the other hand they confirmed the safety threshold of 400 m to proceed directly to surgery without further testing.
In a more sophisticated study, Benzo and colleagues (9) measured the expired gases and metabolic response during SWT in 50 patients with COPD. They found that VO2 increased linearly at every level of SWT. The positive predictive value for walking 25 shuttles (predicting a VO2max <15 mL/kg/min) was 90% and the negative predictive value was 90%. Accordingly, the false-positive rate of detecting VO2max <15 mL/kg/min decreased to 0% if the patient walked at least 380 m.
The main objective of our study was therefore to verify in a modern group of candidates to lung resection whether the thresholds used in previous studies and guidelines were associated with postoperative outcome.
Main findings
Although we found that the cut off value of 250 m was associated with a very high incidence of postoperative cardiopulmonary complications (44%), this value did not remain significantly associated with outcome after logistic regression. This was likely due to the small number of patients walking less than 250 m. The high incidence of complications in patients walking less than 250 m confirmed previous investigations (5).
On the other hand we found that walking less than 400 m was significantly associated with complications even after adjusting the analysis for other confounders using logistic regression. In particular, walking less than 400 m increased the risk of developing complications four times. Notably, only 10% of patients walking at least 400 m developed complications. This corroborates previous findings of a high measured VO2max associated with this distance (9) and which represents a safety criteria to proceed directly to lung resection without further testing as recommended also by recent guidelines (1,2).
Previous British guidelines recommended classifying individuals who experienced more than a 4% oxygen desaturation during the SWT as high risk for surgery (10). However, this was not included in the updated guidelines (11) as a study found oxygen desaturation of 4% or over to not be predictive of surgical outcome (5). Our results concur that oxygen desaturation alone is not predictive of postoperative cardiopulmonary complications. However, we found that measuring oxygen desaturation during the SWT is of benefit when combined with the SWD. Seventy-five percent of the individuals who could not achieve 250 m and who experienced oxygen desaturation of 4% or greater suffered from a complication. However, only four patients in our group showed the two characteristics associated (<250 m and desaturation >4%). On the other hand, 14 patients walked less than 400 m and desaturated at least 4%. Walking less than 400 m combined with oxygen desaturation remained significantly associated with cardiopulmonary complications after logistic regression and increased 5 times the risk of a poor outcome after resection.
Our results seem to support existing guidelines recommending CPET in patients walking less than 400 m particularly in those who desaturated more than 4% during exercise.
Limitations
We recognise that there are a number of limitations in our study.
Firstly, the patients included in the present analysis and performing SWT prior to lung resection represented only a minority of all patients undergoing to lung resection during the same period at our institution (14%). The SWT was generally prescribed by the referring chest physicians according to their individual preferences and selection criteria. Although the characteristics of the patients who performed the SWT were similar to those who did not perform it, the presence of unaccounted or unknown factors influencing the outcome differing between the two groups cannot be completely excluded. Therefore generalizability of the present findings needs to be verified in larger populations.
Secondly, the time frame differed between when the SWT was performed and the date of surgery. To minimise the effect this had on the results we only included patients who had a SWT performed within 4 months of their operation.
Only a small number of patients who performed SWT had also a CPET before surgery. This precluded any reliable correlation analysis between the two tests as performed in previous investigations (8).
Conclusions
This study shows that individuals who walked over 400 m were found to experience a very low rate of postoperative complication. A CPET would be likely of little benefit to this group as we also know from previous studies that nearly all of these patients would have a VO2max >15 mL/kg/min.
In addition, our study has shown the importance of measuring the patient’s oxygen saturation whilst they complete the SWT. We know that walking less than 400 m and having an oxygen desaturation of 4% or over has the strongest association with developing a complication. Finally, we found that 75% of our patients who walked less than 250 m and who had an oxygen desaturation of 4% or over suffered from a postoperative cardiopulmonary complication.
However, we note that patients should not be excluded from lung resection surgery based exclusively on their SWD, regardless of their oxygen desaturation. These high-risk patients should be referred to CPET in order to determine any weak links in the oxygen transport chain, which could be addressed to improve their aerobic reserve to a level that would be considered suitable for surgery.
We believe that this study has several applications to future guidelines and research. Firstly, the guidelines should continue to recommend 400 m as an appropriate cut-off distance in the SWT. Individuals who walk this distance do not require any further investigation to confirm their surgical suitability. Secondly, our findings also suggest that future guidelines could recommend measuring oxygen desaturation during the SWT to identify patients of particular concern. We suggest that future research should focus on the importance of oxygen desaturation during the SWT to validate or reject this recommendation. Our findings warrant the institution of a prospective study aimed at confirming their reliability and generalizability.
Acknowledgements
None.
Ethical Statement: The study was reviewed by the Research and Innovation Department of our hospital, which waived NHS Research Ethics Committee and classified it as service evaluation.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Brunelli A, Kim AW, Berger KI, et al. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e166S-90S. [DOI] [PubMed] [Google Scholar]
- 2.Brunelli A, Charloux A, Bolliger CT, et al. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemo-radiotherapy). Eur Respir J 2009;34:17-41. 10.1183/09031936.00184308 [DOI] [PubMed] [Google Scholar]
- 3.Brunelli A, Pompili C, Salati M. Low-technology exercise test in the preoperative evaluation of lung resection candidates. Monaldi Arch Chest Dis 2010;73:72-8. [DOI] [PubMed] [Google Scholar]
- 4.Singh SJ, Morgan MDL, Scott S, et al. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 1992;47:1019-24. 10.1136/thx.47.12.1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Win T, Jackson A, Groves AM, et al. Relationship of shuttle walk test and lung cancer surgical outcome. Eur J Cardiothorac Surg 2004;26:1216-9. 10.1016/j.ejcts.2004.07.036 [DOI] [PubMed] [Google Scholar]
- 6.Booth S, Adams L. The shuttle walking test: a reproducible method for evaluating the impact of shortness of breath on functional capacity in patients with advanced cancer. Thorax 2001;56:146-50. 10.1136/thorax.56.2.146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernandez FG, Falcoz PE, Kozower BD, et al. The Society of Thoracic Surgeons and the European Society of Thoracic Surgeons general thoracic surgery databases: joint standardization of variable definitions and terminology. Ann Thorac Surg 2015;99:368-76. 10.1016/j.athoracsur.2014.05.104 [DOI] [PubMed] [Google Scholar]
- 8.Win T, Jackson A, Groves AM, et al. Comparison of shuttle walk with measured peak oxygen consumption in patients with operable lung cancer. Thorax 2006;61:57-60 10.1136/thx.2005.043547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benzo RP, Sciurba FC. Oxygen consumption, shuttle walking test and the evaluation of lung resection. Respiration 2010;80:19-23. 10.1159/000235543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.British Thoracic Society. Society of Cardiothoracic Surgeons of Great Britain Ireland Working Party BTS guidelines: guidelines on the selection of patients with lung cancer for surgery. Thorax 2001;56:89-108. 10.1136/thorax.56.2.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim E, Baldwin D, Beckles M, et al. Guidelines on the radical management of patients with lung cancer. Thorax 2010;65:iii1-27. 10.1136/thx.2010.145938 [DOI] [PubMed] [Google Scholar]


