Introduction
Patients are at increased risk of cutaneous and systemic fungal infections when immunocompromised secondary to chemotherapy administration, hematopoietic and solid organ transplantation, diabetes, and AIDS. Those infections caused by Candida species are increasing in severity and frequency.1 Yarrowia lipolytica, formerly termed Candida lipolytica, has only recently been implicated as an offending organism and is now believed to exist as normal flora in the mouth, gut, and pulmonary tree.2 Most infections present as sepsis and, because the organism is considered of low virulence, are not necessarily treated with antifungal medications. A cutaneous infection has only been reported once previously.3
Case report
A 63-year-old white woman with a history of chronic obstructive pulmonary disease and hypertension presented to the Vanderbilt University Medical Center Emergency Department with a nonhealing wound on the tip of her right third finger. She had pierced the end of this finger on a rose bush thorn 6 weeks prior. An orthopedic surgeon removed the thorn under local anesthesia and prescribed a course of an unknown antibiotic. Her chronic obstructive pulmonary disease subsequently worsened, and she was hospitalized for pneumonia and treated with ceftriaxone and azithromycin. Systemic corticosteroids were not administered. At hospital discharge, amoxicillin-clavulanate and azithromycin were prescribed. Because the finger wound failed to heal, her family physician suggested she go to the emergency department.
On the tip of her right third finger was a 1.5-cm brown-black, well-demarcated eschar with minimal surrounding erythema or swelling (Fig 1). Satellite lesions and lymphadenopathy were absent. Her white blood cell count, sedimentation rate, and C-reactive protein values were all elevated. Given the concern for an infectious process from microbes such as Sporothrix schenkii and Candida parapsilosis, a punch biopsy was performed, tissue cultures submitted, and she was empirically begun on ciprofloxacin and itraconazole. The histopathology findings showed epidermal necrosis and minimal inflammation (Fig 2) and fungal hyphae on Gomori methenamine silver staining (Fig 3). The tissue culture grew Yarrowia lipolytica. Her antibiotic regimen was subsequently changed to fluconazole. A computed tomography examination of the finger found osteomyelitis, and at the suggestion of the plastic surgery department, the patient underwent a distal interphalangeal joint amputation of the affected finger. The surgical pathology report from this procedure noted the presence of fungal organisms. Her postoperative course was unremarkable, and she was discharged on a 14-day course of oral fluconazole. To date, her infection has not recurred.
Fig 1.
A well-demarcated eschar on the right third finger of the patient.
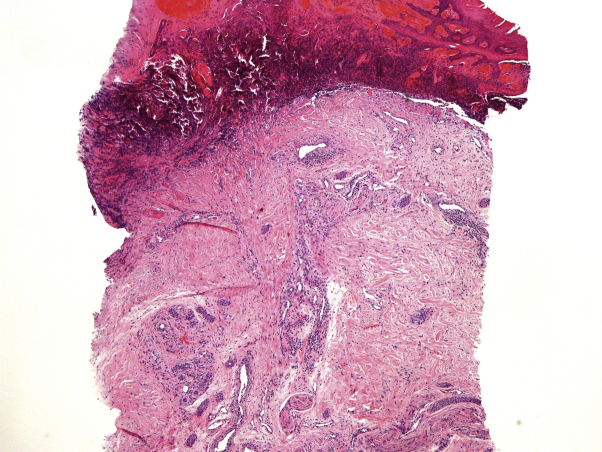
Fig 2.
Low-power microscopy shows epidermal necrosis, mild dermal fibroplasia, and minimal dermal inflammation. (Hematoxylin-eosin stain; original magnification: ×40.)
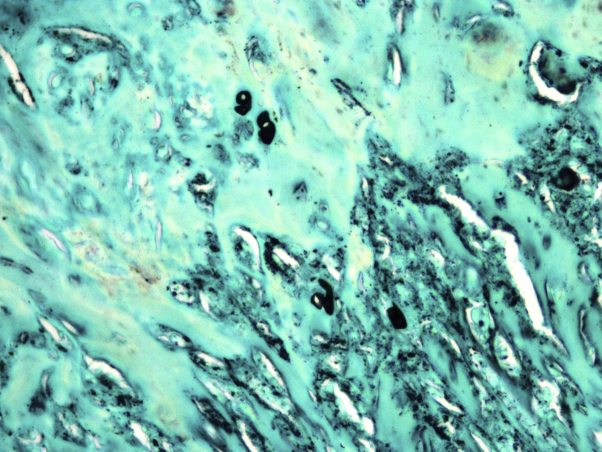
Fig 3.
High-power microscopy shows scattered fungal hyphae within the dermis. (Gomori methenamine silver stain; original magnification: ×900.)
Discussion
More than 200 species of the Candida genus are reported, although only about a dozen are agents of significant toxicity.1 Most species are ubiquitous, growing on substrates rich in organic matter including vegetables, food, and debris. Approximately half of candidemia cases are caused by nonalbicans species.4 Risk factors include use of broad-spectrum antibiotics, hemodialysis/renal failure, major abdominal operations, immunosuppression secondary to transplantation or chemotherapy, AIDS, and chronic corticosteroid administration.4
Yarrowia lipolytica is the only member of the Yarrowia genus. A strictly aerobic organism, it is found in refrigerated meat products, agricultural processing plants, petroleum products, and soil.2 This organism is known for its slime production in culture material, which might be responsible for its ability to adhere to intravenous catheters.5 Efficient at using and breaking down hydrophobic substrates, it is capable of accumulating large amounts of lipid intracellularly.6 Y lipolytica was found to be a nonpathogenic resident on the combs of chickens7 and as skin lesions on 2 harbor seals kept in captivity.8
The first report of human infection with Y lipolytica was in 1985 from a blood culture.9 Infections from this microbe have also been reported as postoperative/postsurgical ocular infections, sinusitis, and wounds, but most have presented as sepsis.4, 10 Over an 18-month period, 55 of 77 patients in a Tunisian hospital with a positive blood culture for yeast were infected with Y lipolytica.2 Most were related to infected vascular catheters, although the organism was found on the hands of a hospital worker and in infusion pumps. Isolates were typically responsive to fluconazole and amphotericin. Over a 10-year period in which all surgical specimens submitted for pathologic analysis were cultured for fungus and bacteria, Irby et al11 noted 24 positive cultures. None were pathogenic, and 17 came from lung tissue and were often associated with a granulomatous tissue response. Two cutaneous specimens described as a “cutaneous nodule” and “toe lesions” were noted, but additional clinical information was not provided. A fatal case of a Y lipolytica–induced subcapsular abscess in a liver transplant patient has been reported.4 The only previous case of cutaneous infection with this yeast occurred in a 39-year-old Chinese national man with a 2-year history of malar nodules after a traumatic event.3 He had been treated with numerous modalities including cyclophosphamide, steroids, and antibiotics to no avail. Follow-up was not discussed in that report.
The presence of fungal hyphae in the dermis engenders a differential diagnosis including aspergillosis, fusariosis, alternariosis, and mucormycosis. The hyphae of mucor organisms show relatively unique features, but often a culture is the only means for elucidating the offending organism. Cryptococcosis, blastomycosis, histoplasmosis, candidiasis and phaeohyphomycoses would be expected to demonstrate almost exclusively spores and not hyphae. Sporotrichosis is probably the closest mimic to our patient's condition in that few fungal organisms would be expected on histologic evaluation, the infection is associated with rose thorn sticks, and the infection is usually seen in otherwise healthy people. Given that patients with deep fungal infections are often gravely ill, systemic antifungal medications are almost always indicated, including aggressive agents such as amphotericin B, voriconazole, and posaconazole.
Treatment of Y lipolytica infections is somewhat controversial given the few cases reported and lack of any clear-cut evidence for appropriate antimicrobial therapy. Because many cases are associated with infected intravenous catheters, simply removing these devices may prove sufficient to clear the infection.2 However, therapy with oral or intravenous azole antifungals, as in our patient, is typically curative.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Lopez-Martinez R. Candidosis, a new challenge. Clin Dermatol. 2010;28(2):178–184. doi: 10.1016/j.clindermatol.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 2.Trabelsi H., Chtara K., Khemakhem N. Fungemia caused by Yarrowia lipolytica. Mycopathologia. 2015;179(5-6):437–445. doi: 10.1007/s11046-015-9859-4. [DOI] [PubMed] [Google Scholar]
- 3.Zheng Y.C., Zeng J.S., Li J.W., Wang D.J., Wu Y.Q., Wu Y. Granuloma caused by Candida lipolytica in China: first case report. J Clin Dermatol. 2009;38(1):9–11. [Google Scholar]
- 4.Mazumder S.A., Todd W.A., Cleveland K.O. Fatal Yarrowia lipolytica intra-abdominal abscess with persistent fungemia in a liver transplant recipient. Infect Dis Clin Pract. 2015;23(5):273–275. [Google Scholar]
- 5.D'Antonio D., Romano F., Pontieri E. Catheter-related candidemia caused by Candida lypolytica in a patient receiving allogenic bone marrow transplantation. J Clin Microbiol. 2002;40:1381–1386. doi: 10.1128/JCM.40.4.1381-1386.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beopoulos A., Cescut J., Haddouche R., Uribelarrea J.L., Molina-Jouve C., Nicaud J.M. Yarrowia lipolytica as a model for bio-oil production. Prog Lip Res. 2009;48(6):375–387. doi: 10.1016/j.plipres.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Grunder S., Mayser P., Redmann T., Kaleta E.F. Mycological examinations on the fungal flora of the chicken comb. Mycoses. 2005;48(2):114–119. doi: 10.1111/j.1439-0507.2004.01074.x. [DOI] [PubMed] [Google Scholar]
- 8.Pollock C.G., Rorhbach B., Ramsay E.C. Fungal dermatitis in captive pinnepeds. J Zoo Wild Med. 2000;31(3):374–378. doi: 10.1638/1042-7260(2000)031[0374:FDICP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Wehrspann P., Fullbrandt U. Report of a case of Yarrowia lipolytica (Wickerman et al.) editors van der Walt and von Arx isolated from a blood culture. Mycoses. 1985;28(5):217–222. [PubMed] [Google Scholar]
- 10.Lai C.C., Lee M.R., Hsiao C.H. Infections caused by Candida lipolytica. J Infect. 2012;65(4):372–374. doi: 10.1016/j.jinf.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Irby R.F., Kandula M., Zadikany R., Sandin R.L., Greene J.N. Yarrowia lipolytica as normal human flora; a case series of 24 patients with positive cultures and no attributable disease. Infect Dis Clin Pract. 2014;22(4):207–209. [Google Scholar]