Abstract
PURPOSE
Postnatal depression affects 10% to 15% of new mothers, and approximately 90% of cases are managed in primary care. Antidepressants are effective, but adherence is poor; therefore, psychological interventions must be investigated. In this systematic review, we assessed the efficacy of psychological therapies for postnatal depression in primary care.
METHODS
We undertook a systematic search to identify articles published in English between 2000 and 2014 that reported studies meeting our eligibility criteria: (1) had a randomized controlled trial design; (2) assessed psychological interventions for postnatal depression against any other treatment or a wait-list control; (3) recruited patients in primary care; and (4) enrolled mothers with a diagnosed depressive episode or a score of at least 12 on the Edinburgh Postnatal Depression Scale or at least 10 on the Beck Depression Inventory at baseline who had a child younger than 12 months. Quality was assessed using an adapted Cochrane Collaboration Depression, Anxiety, and Neurosis (CCDAN) quality rating scale, and meta-analysis was carried out using RevMan 5.3 (The Cochrane Collaboration).
RESULTS
Screening of 5,919 articles identified 10 studies that met inclusion criteria. These studies reported on 14 psychological intervention arms: 7 using cognitive behavioral therapy, 2 using interpersonal therapy, 2 using counseling, and 3 using other interventions. Psychological interventions resulted in lower depressive symptomatology than control both immediately after treatment (standardized mean difference = −0.38; 95% CI, −0.49 to −0.27) and at 6 months of follow-up (standardized mean difference =−0.21; 95% CI, −0.37 to −0.05). We did not find any significant differences between the various types of therapy. Compared with control, the interventions also led to improvements in adjustment to parenthood, marital relationship, social support, stress, and anxiety.
CONCLUSIONS
Psychological interventions deliverable in the primary care setting are associated with a significant improvement in depressive symptomatology both immediately after completion and for up to 6 months of follow-up.
Keywords: postnatal depression, psychological intervention, psychotherapy, primary care, general practice, systematic review
INTRODUCTION
About 13% of mothers experience postnatal depression during the first year after delivery.1 If left untreated, this condition can have an extensive negative impact on women, children, and wider society. A recent report found that the annual cost to UK society of perinatal depression was £73,822 ($104,574) per case, of which 70% was due to adverse impacts on the child.2 Effects on the child can arise because of impaired maternal-infant bonding, maternal withdrawal, disengagement, hostility, and shortening of the duration of breastfeeding.3–12 Other consequences of postnatal depression include marital difficulties and an increased risk of future depression, with affected mothers twice as likely to experience further episodes of depression in the subsequent 5 years.13 Research has shown that early identification and treatment of postnatal depression can reduce negative impacts on women, children, and families14; therefore, finding suitable and acceptable treatments is vital.15
Management of Postnatal Depression
Antidepressant medication is commonly used as a first-line treatment for postnatal depression, and selective serotonin reuptake inhibitors are likely to be effective16; however, potential medication adverse effects are worrisome to both mothers and clinicians.17 Transmission through breast milk is a concern.18 For this reason, mothers are often reluctant to take medication, with poor adherence seen in those prescribed antidepressants.19 Consequently, it is important to evaluate the efficacy of nonpharmacologic therapies in this setting.
A range of psychological interventions have been developed for postnatal depression. They include support groups, counseling,20 cognitive behavioral therapy (CBT),21,22 interpersonal therapy (IPT),23–25 and psychodynamic therapy.26 Many women with postnatal depression show a strong preference for psychological treatments, and research supports their use as a preventive measure. Reviews have reported that psychological interventions can be an effective means of reducing the risk of developing postnatal depression27 as well as an effective treatment option.28
The Role of Primary Care
In the United Kingdom, and other countries with strong primary health care, the majority of cases of postnatal depression are identified and managed in community settings,29 and fewer than 10% are referred to secondary care.2 The primary objective of this systematic review was to assess the effectiveness of psychological interventions in women with postnatal depression who were recruited and treated in primary care settings. Secondary aims included examining the effectiveness of specific types of psychological interventions (eg, CBT, IPT), comparing the effectiveness of individual vs group intervention, and assessing the impact on secondary outcomes such as the couple’s relationship and adjustment to parenthood.
METHODS
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and Cochrane Collaboration recommendations for the reporting of this review.
Search Methods
A systematic search of MEDLINE, EMBASE, Psyc-INFO, CINAHL, and Web of Science was conducted to identify articles published in English between January 1, 2000, and December 31, 2014. We used a predefined search strategy (Supplemental Appendix 1, http://www.annfammed.org/content/14/5/463/suppl/DC1). The results were imported into EndNote X7 (Thomson Reuters), duplicates were removed, and an initial title assessment was carried out. We then reviewed abstracts and retrieved the full text of relevant studies. Two authors (S.S., E.F.) evaluated the full text of studies together to determine whether they met inclusion criteria, described below.
Inclusion Criteria
Trials were eligible for inclusion if they had a randomized controlled design; assessed the effectiveness of psychological interventions for postnatal depression, comparing them with any other treatment or a wait-list control; enrolled participants recruited from either primary care or via community screening; and delivered their intervention in community settings. Participants had to have met the diagnostic criteria for a depressive episode determined by clinical interview or by an Edinburgh Postnatal Depression Scale (EPDS) score of 12 or higher, or Beck Depression Inventory (BDI) score of 10 or higher at baseline, and had to have a child younger than the age of 12 months at recruitment.
The trials could have used any psychological therapy, including CBT, IPT, counseling, and support groups. The interventions must have used a standardized number of sessions, and must have been delivered by specifically trained personnel (eg, general practitioners, therapists, or health visitors, and not peer support) in the community.
Quality Assessment
We used an adapted version of the Cochrane Collaboration Depression, Anxiety, and Neurosis (CCDAN) Quality Rating Scale30,31 to assess the quality of included studies (Supplemental Appendix 2, http://www.annfammed.org/content/14/5/463/suppl/DC1). The Quality Rating Scale consists of 23 items, including questions on sample size, allocation, use of diagnostic criteria, adherence, attrition, and statistical analysis, of which we used 20 items in this study. Each item was scored from 0 to 2 with a possible total of up to 40 points on the adapted version of this scale. We required a score of greater than 20 to be included in the analysis (adjusted from the 23 points required by Bower and Rowland30) and considered a score of greater than 30 to indicate a study of high methodologic quality.
Data Extraction and Analyses
We extracted the following relevant information from the selected studies: study characteristics (author, year of publication, country), number of participants, details of the intervention and control condition, age of participants, duration of follow-up, measurement tool, scores for depression and other outcomes, and attrition. Meta-analysis was carried out using RevMan 5.3 (The Cochrane Collaboration).
Outcomes Reviewed
Depression scores were reported using the EPDS20 and the Beck Depression Inventory, either the original version (BDI) or second version (BDI-II).32,33 Where studies reported both, we used the EPDS in analysis. To estimate the overall treatment effect, we calculated the standardized mean difference (SMD) for each study with 95% confidence intervals (CIs). The same method was applied to other continuous outcomes, including measures of stress and anxiety. For dichotomous outcomes, such as the number of women who fell below the diagnostic threshold for depression postintervention, we calculated odds ratios. A fixed effect model was used for all analyses. A random effects model was used for further verification of the findings, but results were similar and are therefore not reported. To assess heterogeneity, we calculated the I2 statistic for each outcome; a value of 25% indicates a lower degree of heterogeneity, 50% a moderate degree, and 75% a high degree.34 We carried out a sensitivity analysis to test the robustness of the findings by comparing the overall effect sizes after excluding studies with a quality score of less than 30.
RESULTS
Search Results
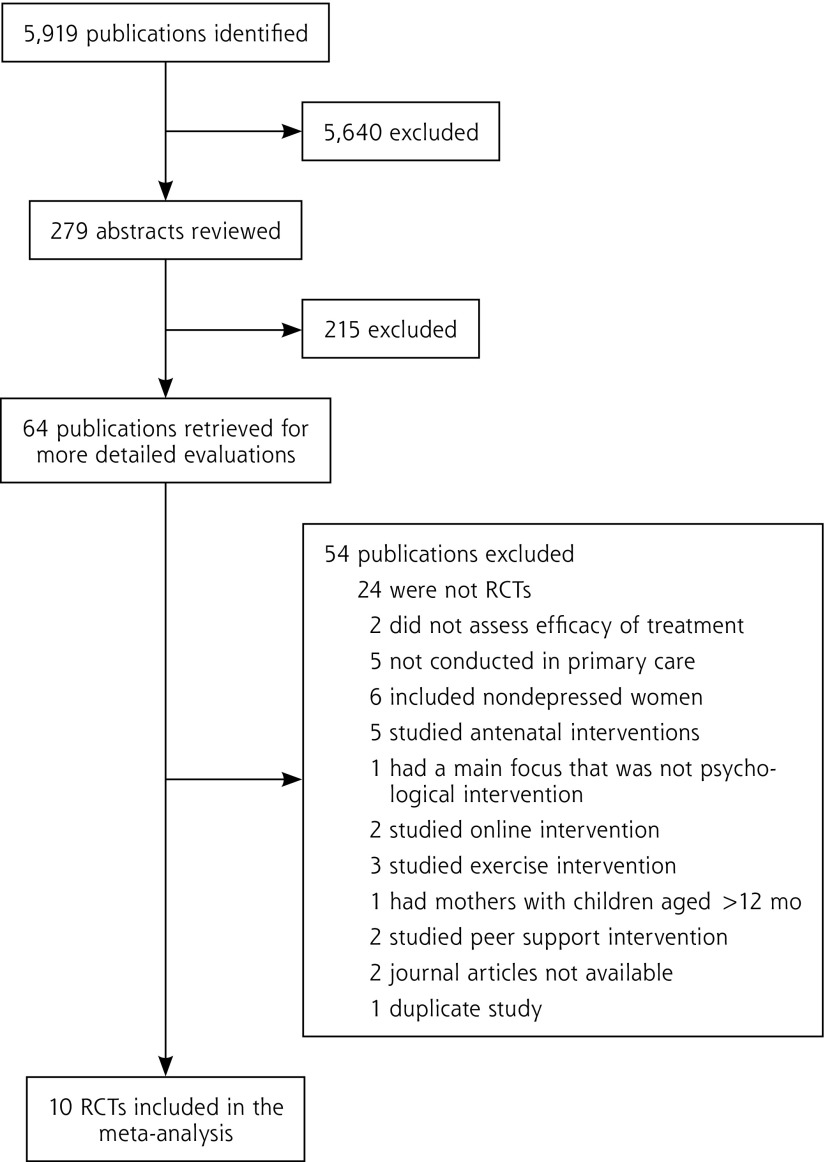
Our database search identified a total of 5,919 publications reporting potentially eligible studies, of which 10 studies, published between 2000 and 2013, ultimately met the inclusion criteria and were included in the meta-analysis (Figure 1).35–44 Of these, 4 were conducted in Australia,35–38 3 in the United Kingdom,39–41 2 in the United States,42,43 and 1 in Taiwan.44
Figure 1.
Study selection flow diagram.
RCT = randomized controlled trial.
Study Characteristics
Population
The 10 eligible studies had a total of 1,324 participants, with an overall mean age of 29.95 years (SD 1.95); characteristics of these studies are summarized in Table 1. Slightly more than one-half the participants were primiparous (mean = 51.9%, SD 17.2%; reported in 6 studies) and most participants were married or cohabiting (mean = 88.9%, SD 7.9%; reported in 7 studies). Cases of depression were defined variably in the studies using an EPDS score of 12 or higher39–41; an EPDS score of 10 or higher, or of 12 or higher plus a positive diagnostic interview35,36,38,43; a BDI score of 10 or higher44; and a Hamilton Rating Scale for Depression score of 14 or higher plus a diagnostic assessment.37,42 All studies reported EPDS scores, BDI scores, or both at baseline; the mean EPDS score was 15.9 (SD 2.1; 7 studies) and the mean BDI score was 21.5 (SD 7.5; 5 studies).
Table 1.
Characteristics of the 10 Included Studies
| Study, Year, and Country | Sample Size | Intervention (No.) | Control (No.) | Age, Mean (SD), y | Follow-up | Measurement Tool | Attrition, % | Quality Scorea |
|---|---|---|---|---|---|---|---|---|
| Horowitz et al,43 2013, USA | 134 | Communicating and Relating Effectively (CARE) (66) | Treatment as usual (68) | 31.0 (5.7) | 3, 6, and 9 mo | EPDS | 6 | 36 |
| Milgrom et al,36 2011, Australia | 68 | General practitioner management with adjunctive CBT with nurse (22) General practitioner management with adjunctive CBT with psychologist (23) |
General practitioner management (23) | 31.5 (4.7) | 3 and 8 wk | BDI-II | 28 | 32 |
| Mulcahy et al,37 2010, Australia | 57 | Group IPT (29) | Treatment as usual (28) | 32.2 (3.4) | 4 and 8 wk | EPDS, BDI-II, DAS, ISEL, MAI | 12 | 30 |
| Morrell et al,40 2009, UK | 418 | CBT/person-centered therapy (271) | Treatment as usual (147) | 30.9 (5.4) | 6, 12, and 18 mo | EPDS, STAI, PSI | 28 | 34 |
| Milgrom et al,38 2005, Australia | 192 | CBT (46) Group-based counseling (47) Individual counseling (66) |
Treatment as usual (33) | 29.7 (5.4) | 12 wk and 12 mo | BDI, BAI, SPS | 70 | 33 |
| Cooper et al,41 2003, UK | 193 | CBT (43) Psychodynamic therapy (50) Counseling (48) |
Treatment as usual (52) | 27.7 (5.4) | 4.5, 9, and 18 mo, and 5 y | EPDS | 12 | 35 |
| Honey et al,39 2002, UK | 45 | CBT (23) | Treatment as usual (22) | 27.9 (5.5) | 8 wk and 6 mo | EPDS, DAS | – | 21 |
| Prendergast and Austin,35 2001, Australia | 37 | CBT (17) | Ideal standardized care (20) | 32.2b | 6 wk and 6 mo | EPDS | 10 | 23 |
| O’Hara et al,42 2000, USA | 120 | IPT (60) | Wait-list control (60) | 29.6 (4.7) | 4, 8, and 12 wk | BDI | 18 | 26 |
| Chen et al,44 2000, Taiwan | 60 | Support group (30) | Treatment as usual (30) | 29.1 (4.2) | 4 wk | BDI, PSS, ISEL, SEI | – | 24 |
BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory, original version; BDI-II = Beck Depression Inventory, second version; DAS = Dyadic Adjustment Scale; EPDS = Edinburgh Postnatal Depression Scale; ISEL = Interpersonal Support Evaluation List; MAI = Maternal Attachment Inventory; PSI = Parenting Stress Index; PSS = Perceived Stress Scale; SEI = Coopersmith Postnatal Self-Esteem Inventory; SPS = Social Provisions Scales; STAI = State-Trait Anxiety Inventory.
On the modified Quality Rating Scale. Possible scores range from 0 to 40, where higher scores indicate higher quality.
SD not given.
Recruitment and Interventions
Four studies recruited participants using health visitors (UK community nurses specialized in maternal and child heath),35,36,38,39 1 using general practitioners (family physicians),40 and 1 using any health care professional in primary care.37 Another 4 studies recruited using researchers.41–44
The 10 studies had a total of 14 psychological intervention arms—6 used CBT (2 in a single study), 2 used IPT, 2 used counseling, and 3 used other interventions—and 10 control arms. Interventions were provided in group settings (5 intervention arms) or individual settings (9 intervention arms). Sessions lasted between 30 minutes and 2 hours, and the intervention duration ranged from 4 weeks to 8 months. The interventions were delivered by nurses (research nurses,43,44 health visitors,39–41 early childhood nurses,35 or therapists with a nurse background36,38), psychologists,36,38,41,42 or trained researchers.37
Control Conditions
Seven studies used treatment as usual—antidepressant medication, referral to a specialist, or use of preexisting counseling service—for their control arm. Two studies used enhanced standardized care, and the tenth study used a wait-list control group. Four studies allowed use of antidepressants in both study arms,36,37,39,40 but only 1 of them reported on use: 46 of 125 control participants (37%), and 61 of 214 intervention participants (29%) used antidepressants.40
Effects of Interventions
Depressive Symptomatology
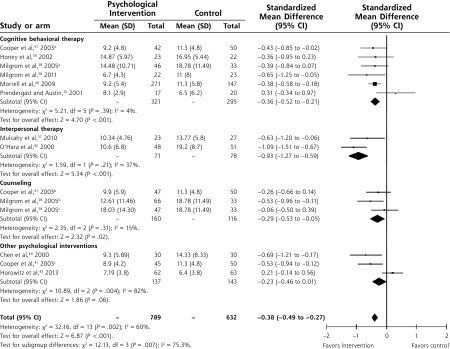
All 10 studies (14 intervention arms) reported on the level of depressive symptomatology immediately postintervention using either the EPDS (6 studies) or the BDI (5 studies), with results showing a significant benefit in favor of the psychological intervention (SMD = −0.38; 95% CI, −0.49 to −0.27) (Figure 2).
Figure 2.
Forest plot of scores comparing psychological interventions vs control conditions immediately postintervention, fixed effects analysis.
aCognitive behavioral therapy arms of those trials.
bCounseling arm (Cooper et al) or individual counseling arm (Milgrom et al).
cGroup counseling arm (Milgrom et al) or psychodynamic therapy arm (Cooper et al).
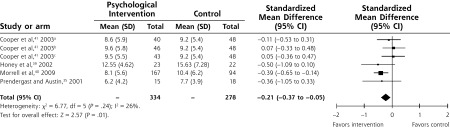
The psychological interventions also resulted in significantly lower levels of depressive symptomatology in the longer term (Figure 3). The timing of the final assessment varied from immediately postintervention (4 studies)36,37,42,44 to 5 years (1 study).41 The level of attrition during the course of the interventions ranged from 6% to 70% (mean = 23%). Six intervention arms reported self-reported scores for depression between 4 and 6 months postintervention, showing a significant improvement in the intervention arm compared with the control arm (SMD = −0.21; 95% CI, −0.37 to −0.05), although this finding was highly influenced by a single study.40
Figure 3.
Forest plot of scores comparing psychological interventions vs control conditions at longer-term follow-up (median time 6 mo), fixed effects analysis.
aCognitive behavioral therapy arms of those trials.
bCounseling arm.
cPsychodynamic therapy arm.
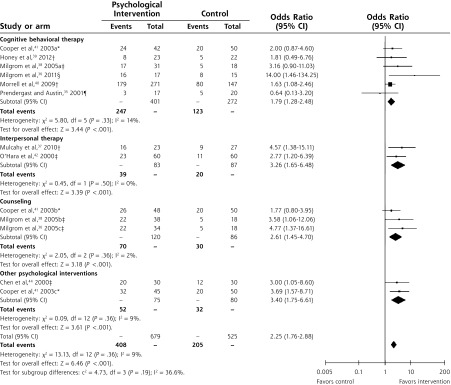
Number of Women Below Diagnostic Threshold
Nine studies (13 intervention arms, 1,190 women) reported on the number of women who fell below the diagnostic threshold for postnatal depression immediately after the intervention, established using cut-off scores on the BDI (score ≥10), the BDI-II (score ≥14), the EPDS (score ≥ 12), or structured clinical interviews. All participants were above the threshold at baseline. The psychological interventions were significantly better than the control conditions for reducing symptoms to below threshold (odds ratio = 2.25; 95% CI, 1.76 to 2.88) (Figure 4).
Figure 4.
Forest plot of the odds ratio of patients being above diagnostic threshold (variously defined) comparing psychological interventions with control conditions, fixed effects analysis.
aCognitive behavioral therapy arms of those trials.
bCounseling arm (Cooper et al) or individual counseling arm (Milgrom et al).
cGroup counseling arm (Milgrom et al) or psychodynamic therapy arm (Cooper et al).
* Diagnostic threshold: clinical interview.
† Diagnostic threshold: Edinburgh Postnatal Depression Scale score ≥12.
‡ Diagnostic threshold: Beck Depression Inventory score ≥10.
§ Diagnostic threshold: Beck Depression Inventory, second version score ≥14.
¶ Diagnostic threshold: Edinburgh Postnatal Depression Scale score ≥10.
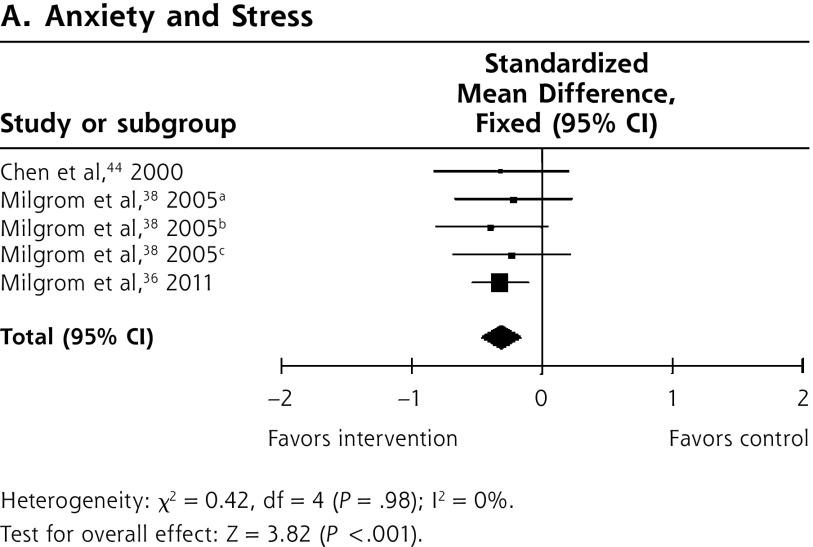
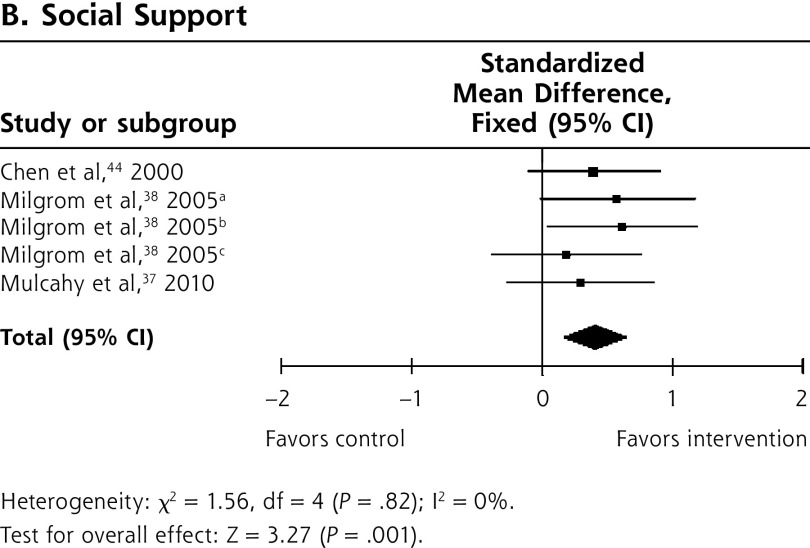
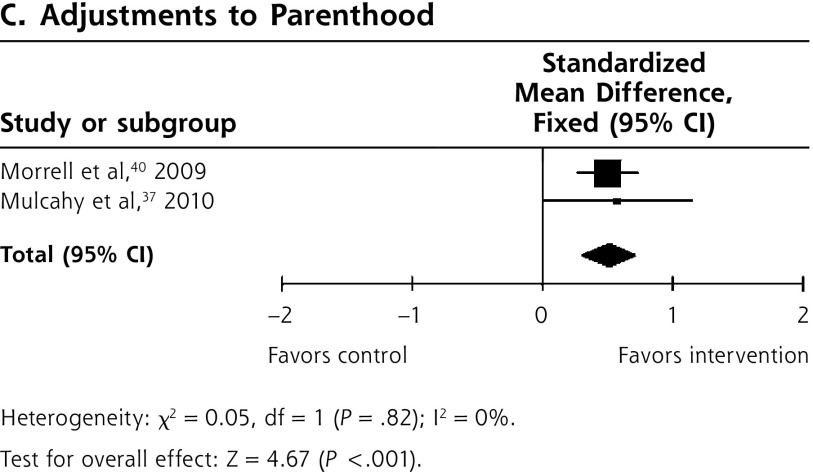
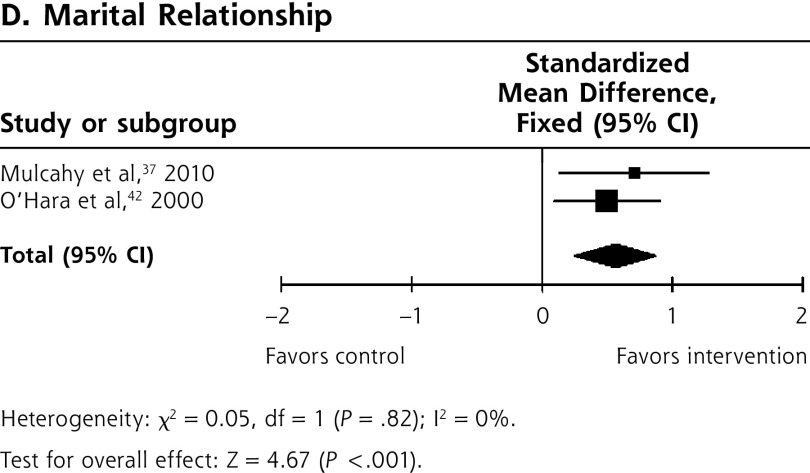
Other Outcomes
The psychological interventions additionally resulted in lower levels of stress and anxiety compared with control (SMD = −0.30; 95% CI, −0.45 to −0.15) (3 studies, 5 intervention arms) (Figure 5). Women in the psychological intervention arms also reported significantly higher levels of social support (SMD = 0.42; 95% CI, 0.17 to 0.42) (3 studies, 5 intervention arms); improved marital relationships as measured by the Dyadic Adjustment Scale (SMD = 0.57; 95% CI, 0.25 to 0.90) (2 studies); and better adjustment to parenthood (SMD = 0.52; 95% CI, 0.30 to 0.74) (2 studies).
Figure 5.
Forest plots of data comparing psychological and psychosocial interventions vs control conditions for anxiety and stress, social support, adjustment to parenthood, and marital relationship, fixed effects analysis.
Note: Scales used: (A) anxiety and stress: Perceived Stress Scale,44 Beck Anxiety Inventory,38 Depression Anxiety and Stress Scales36; (B) social support: Interpersonal Support Evaluation List,37,44 Social Provisions Scale38; (C) adjustment to parenthood: Parenting Stress Index - short form,40 Maternal Attachment Inventory37; (D) marital relationship: Dyadic Adjustment Scale.37,45
aCognitive behavioral therapy arms of those trials.
bIndividual counseling arm.
cGroup counseling arm.
Study Quality and Sensitivity Analysis
The studies’ CCDAN Quality Rating Scale scores ranged from 21 to 36, with only 4 studies scored below 30 (Table 1). Eliminating data from these 4 studies resulted in a reduction of the heterogeneity in the overall depressive symptomatology analysis, from I2 = 60% to I2 = 40%, but a statistically significant result in favor of the psychological interventions was maintained.
Antidepressant Use
Two studies investigated the impact of antidepressant use on outcomes. One found that antidepressant use in the control arm was higher than that in the intervention arm, yet the decrease in depressive symptoms was less in the former.40 One carried out a regression analysis, finding that antidepressant use did not account for the improvement in mood seen with psychological intervention.39
DISCUSSION
This meta-analysis combined the results of 10 RCTs, involving 1,324 depressed new mothers and showed that psychological interventions delivered in community settings are an effective treatment for postnatal depression. Compared with treatment as usual or a wait-list control, psychological interventions resulted in lower levels of depressive symptomatology and higher levels of remission immediately after treatment. Improvements in symptoms at 4 to 6 months of follow-up were still significant but less robust, and levels of remission at follow-up were not assessed. Individual and group-based treatments were equally effective. Statistically significant improvements were also found in anxiety and stress, marital relationships, adjustment to parenthood, and perceived social support. The small number of studies available means that caution is required when interpreting the secondary results and the longer-term follow-up.
By focusing on community studies, we have been able to show that psychological interventions, deliverable in primary care, are effective for reducing symptomatology and caseness of postnatal depression. CBT was the most widely studied treatment in this analysis. It has been extensively investigated46 and shown to be equally as effective for depression as antidepressant medication.47,48 IPT was also found to be an effective therapy. A review of IPT for depression in pregnancy and the postnatal period also found that it led to an overall clinical improvement.49 There is strong evidence that low levels of social support are a key risk factor for postnatal depression, and both attachment and interpersonal models of etiology argue that a perceived lack of or a mismatch between desired and actual levels of support are implicated in its development,1,50,51 suggesting that IPT will be effective in this context.
These findings are consistent with those of the previously published reviews on psychological interventions for postnatal depression28 and on psychological interventions for depression in primary care.52 Our analysis provides an update and new focus compared with the 2007 review by Dennis and Hodnett,28 and only 3 studies overlap with that review. By selecting studies in which participants were both recruited and treated in primary care, we have produced evidence relevant to primary care clinicians for their care of patients as well as for the planning of services.
Delivery of the Interventions
A range of professionals recruited women to the trials and delivered the interventions investigated, but the majority of interventions were conducted by trained community nurses, particularly health visitors. The generalizability of these findings may therefore be limited by the lack of availability of similar personnel in all countries, particularly in the United States, where a health-visiting service may not exist. In such countries, family physicians are well placed to identify women with postnatal depression, and psychological therapists working in the community could deliver the interventions.
There are other logistic implications of delivering psychological interventions to new mothers, such as the time required, accessibility, and availability of childcare. We did not find any difference in efficacy between group and individual therapy. Group therapy may have advantages in that it is less resource intensive to provide, but disadvantages in terms of the inflexibility of timing of sessions and the logistics of childcare provision. A comparison of the adherence to therapies by location and other logistics would help to inform the planning of these treatments.
Clinical Implications
Our results suggest that primary care clinicians need to ensure that psychological therapies are as available as medication to their patients. Psychological services should be commissioned in situations where they do not already exist, and where they do exist, their availability should reflect the prevalence of postnatal depression.
Research regarding the cost-effectiveness of psychological treatments for depression within primary care is inconclusive.53 A recent study suggested, however, that CBT was a cost-effective treatment for depression based on the UK National Institute for Health and Care Excellence criteria.54 Additionally, there is extensive evidence that investment in mental health provision for the postnatal period has a very significant cost-benefit effect for wider society.2
Strengths and Limitations
This meta-analysis is the first to systematically assess the efficacy of psychological interventions for the treatment of postnatal depression solely in the primary care setting. Unlike previous analyses and reviews, it used subanalysis to clarify the effectiveness of different interventions and modes of delivery. Our results are also strengthened by the inclusion of a sensitivity analysis that removed low-quality studies and found no effect on results.
On the other hand, our review of study quality did not weight study components, but treated all of them as equally important; thus, despite scoring higher than 20 on the rating scale, many of the studies had small sample sizes and high attrition, and allowed concomitant use of antidepressant medication. These methodologic limitations weaken the conclusions to be drawn and could have introduced bias. Additionally, the findings regarding long-term effects were weak, looking only at symptom reduction rather than resolution, and the significant finding appeared to be due to a single study. More research is needed on the longer-term effects of these psychological interventions. Attrition rates were variable, but the majority of studies reported no difference in confounders between the groups at completion.
Conclusions
Our review provides evidence for the use of psychological interventions for the treatment of postnatal depression in primary care. No particular type of therapy emerged as the most effective, but IPT showed promising results, and CBT was also beneficial. Future trials should address long-term follow up and minimizing attrition, as well as examine the effects that therapies have on the wider context of the family. Studies should also investigate whether different therapies are valuable for women with differing risk factors or clinical presentations, and explore the effectiveness of psychological interventions in the absence of adjunctive medication, especially if women are reluctant to take antidepressants. Overall, psychological interventions are a valid treatment option for postnatal depression managed in primary care, and provide an important alternative for mothers not wishing to take antidepressant medication.
Footnotes
Conflicts of interest: authors report none.
Supplemental Materials: Available at http://www.annfammed.org/content/14/5/463/suppl/DC1/.
References
- 1.O’Hara MW, Swain AM. Rates and risk of postpartum depression; a meta-analysis. Int Rev Psychiatry. 1996;8(1):37–54. [Google Scholar]
- 2.Bauer A, Parsonage M, Knapp M, Iemmi V, Adelaja B. The costs of perinatal mental health problems. Centre for Mental Health; https://www.centreformentalhealth.org.uk/costs-of-perinatal-mh-problems. Published Oct 20, 2014 Accessed Aug 8, 2016. [Google Scholar]
- 3.O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013;9:379–407. [DOI] [PubMed] [Google Scholar]
- 4.Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of the literature. Arch Womens Ment Health. 2003;6(4):263–274. [DOI] [PubMed] [Google Scholar]
- 5.Salisbury AL, Lester BM, Seifer R, et al. Prenatal cocaine use and maternal depression: effects on infant neurobehavior. Neurotoxicol Teratol. 2007;29(3):331–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murray L, Sinclair D, Cooper P, Ducournau P, Turner P, Stein A. The socioemotional development of 5-year-old children of postnatally depressed mothers. J Child Psychol Psychiatry. 1999;40(8):1259–1271. [PubMed] [Google Scholar]
- 7.Hall P. Mothers’ experiences of postnatal depression: an interpretative phenomenological analysis. Community Pract. 2006;79(8): 256–260. [PubMed] [Google Scholar]
- 8.Beck CT. Maternal depression and child behaviour problems: a meta-analysis. J Adv Nurs. 1999;29(3):623–629. [DOI] [PubMed] [Google Scholar]
- 9.Hipwell AE, Goossens FA, Melhuish EC, Kumar R. Severe maternal psychopathology and infant-mother attachment. Dev Psychopathol. 2000;12(2):157–175. [DOI] [PubMed] [Google Scholar]
- 10.Martins C, Gaffan EA. Effects of early maternal depression on patterns of infant-mother attachment: a meta-analytic investigation. J Child Psychol Psychiatry. 2000;41(6):737–746. [PubMed] [Google Scholar]
- 11.Murray L, Fiori-Cowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev. 1996;67(5): 2512–2526. [PubMed] [Google Scholar]
- 12.Dennis CL, McQueen K. Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatr. 2007;96(4):590–594. [DOI] [PubMed] [Google Scholar]
- 13.Cooper PJ, Murray L. Course and recurrence of postnatal depression. Evidence for the specificity of the diagnostic concept. Br J Psychiatry. 1995;166(2):191–195. [DOI] [PubMed] [Google Scholar]
- 14.Pilowsky DJ, Wickramaratne P, Talati A, et al. Children of depressed mothers 1 year after the initiation of maternal treatment: findings from the STAR*D-Child Study. Am J Psychiatry. 2008;165(9):1136–1147. [DOI] [PubMed] [Google Scholar]
- 15.Bauer APM, Knapp M, Iemmi V, Adelaja B. Costs of Perinatal Mental Health Problems. London, England: Centre for Mental Health and London School of Economics; 2014. [Google Scholar]
- 16.Molyneaux E, Howard LM, McGeown HR, Karia AM, Trevillion K. Antidepressant treatment for postnatal depression. Cochrane Database Syst Rev. 2014;9(9):CD002018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pearlstein T, Howard M, Salisbury A, Zlotnick C. Postpartum depression. Am J Obstet Gynecol. 2009;200(4):357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pearlstein T. Perinatal depression: treatment options and dilemmas. J Psychiatry Neurosci. 2008;33(4):302–318. [PMC free article] [PubMed] [Google Scholar]
- 19.Boath E, Bradley E, Henshaw C. Women’s views of antidepressants in the treatment of postnatal depression. J Psychosom Obstet Gynaecol. 2004;25(3–4):221–233. [DOI] [PubMed] [Google Scholar]
- 20.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–786. [DOI] [PubMed] [Google Scholar]
- 21.Hollon SD. What is cognitive behavioural therapy and does it work? Curr Opin Neurobiol. 1998;8(2):289–292. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Beck JS. Cognitive Behavior Therapy: Basics and Beyond. 2nd ed. New York, NY: Guilford Press; 2011. [Google Scholar]
- 23.Markowitz JC, Weissman MM. Interpersonal psychotherapy: principles and applications. World Psychiatry. 2004;3(3):136–139. [PMC free article] [PubMed] [Google Scholar]
- 24.Weissman MM, Klerman GL. Interpersonal psychotherapy for depression. In: Wolman BB, Stricker G, eds. Depressive Disorders: Facts, Theories, and Treatment Methods. Oxford, England: John Wiley & Sons; 1990:379–395. [Google Scholar]
- 25.Stuart S, O’Hara MW. Interpersonal psychotherapy for postpartum depression: a treatment program. J Psychother Pract Res. 1995;4(1): 18–29. [PMC free article] [PubMed] [Google Scholar]
- 26.Clark R, Tluczek A, Wenzel A. Psychotherapy for postpartum depression: a preliminary report. Am J Orthopsychiatry. 2003;73(4):441–454. [DOI] [PubMed] [Google Scholar]
- 27.Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2013;2(2):CD001134. [DOI] [PubMed] [Google Scholar]
- 28.Dennis CL, Hodnett E. Psychosocial and psychological interventions for treating postpartum depression. Cochrane Database Syst Rev. 2007;(4):CD006116. [DOI] [PubMed] [Google Scholar]
- 29.Wittchen H-U, Mühlig S, Beesdo K. Mental disorders in primary care. Dialogues Clin Neurosci. 2003;5(2):115–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bower P, Rowland N. Effectiveness and cost effectiveness of counselling in primary care. Cochrane Database Syst Rev. 2006;(3):CD001025. [DOI] [PubMed] [Google Scholar]
- 31.Moncrieff J, Churchill R, Drummond DC, McGuire H. Development of a quality assessment instrument for trials of treatments for depression and neurosis. Int J Methods Psychiatr Res. 2001;10(3):126–133. [Google Scholar]
- 32.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. [DOI] [PubMed] [Google Scholar]
- 33.Steer RA, Ball R, Ranieri WF, Beck AT. Dimensions of the Beck Depression Inventory-II in clinically depressed outpatients. J Clin Psychol. 1999;55(1):117–128. [DOI] [PubMed] [Google Scholar]
- 34.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prendergast J, Austin M-P. Early childhood nurse-delivered cognitive behavioural counselling for postnatal depression. Australas Psychiatry. 2001;9(3):255–259. [Google Scholar]
- 36.Milgrom J, Holt CJ, Gemmill AW, et al. Treating postnatal depressive symptoms in primary care: a randomised controlled trial of GP management, with and without adjunctive counselling. BMC Psychiatry. 2011;11(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mulcahy R, Reay RE, Wilkinson RB, Owen C. A randomised control trial for the effectiveness of group interpersonal psychotherapy for postnatal depression. Arch Womens Ment Health. 2010;13(2):125–139. [DOI] [PubMed] [Google Scholar]
- 38.Milgrom J, Negri LM, Gemmill AW, McNeil M, Martin PR. A randomized controlled trial of psychological interventions for postnatal depression. Br J Clin Psychol. 2005;44(Pt 4):529–542. [DOI] [PubMed] [Google Scholar]
- 39.Honey KL, Bennett P, Morgan M. A brief psycho-educational group intervention for postnatal depression. Br J Clin Psychol. 2002;41(Pt 4):405–409. [DOI] [PubMed] [Google Scholar]
- 40.Morrell CJ, Slade P, Warner R, et al. Clinical effectiveness of health visitor training in psychologically informed approaches for depression in postnatal women: pragmatic cluster randomised trial in primary care. BMJ. 2009;338:a3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of postpartum depression. I. Impact on maternal mood. Br J Psychiatry. 2003;182:412–419. [PubMed] [Google Scholar]
- 42.O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry. 2000;57(11):1039–1045. [DOI] [PubMed] [Google Scholar]
- 43.Horowitz JA, Murphy CA, Gregory K, Wojcik J, Pulcini J, Solon L. Nurse home visits improve maternal/infant interaction and decrease severity of postpartum depression. J Obstetric Gynecol Neonatal Nurs. 2013;42(3):287–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen C-H, Tseng Y-F, Chou F-H, Wang S-Y. Effects of support group intervention in postnatally distressed women. A controlled study in Taiwan. J Psychosom Res. 2000;49(6):395–399. [DOI] [PubMed] [Google Scholar]
- 45.Grekin R, O’Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. 2014;34(5):389–401. [DOI] [PubMed] [Google Scholar]
- 46.Hofmann SG, Asnaani A, Vonk IJJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2012;36(5):427–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.DeRubeis RJ, Gelfand LA, Tang TZ, Simons AD. Medications versus cognitive behavior therapy for severely depressed outpatients: mega-analysis of four randomized comparisons. Am J Psychiatry. 1999;156(7):1007–1013. [DOI] [PubMed] [Google Scholar]
- 48.Dobson KS. A meta-analysis of the efficacy of cognitive therapy for depression. J Consult Clin Psychol. 1989;57(3):414–419. [DOI] [PubMed] [Google Scholar]
- 49.Miniati M, Callari A, Calugi S, et al. Interpersonal psychotherapy for postpartum depression: a systematic review. Arch Womens Ment Health. 2014;17(4):257–268. [DOI] [PubMed] [Google Scholar]
- 50.Beck CT. Theoretical perspectives of postpartum depression and their treatment implications. MCN Am J Matern Child Nurs. 2002;27(5):282–287. [DOI] [PubMed] [Google Scholar]
- 51.Cooper PJ, Murray L, Hooper R, West A. The development and validation of a predictive index for postpartum depression. Psychol Med. 1996;26(3):627–634. [DOI] [PubMed] [Google Scholar]
- 52.Bortolotti B, Menchetti M, Bellini F, Montaguti MB, Berardi D. Psychological interventions for major depression in primary care: a meta-analytic review of randomized controlled trials. Gen Hosp Psychiatry. 2008;30(4):293–302. [DOI] [PubMed] [Google Scholar]
- 53.Bosmans JE, van Schaik DJ, de Bruijne MC, et al. Are psychological treatments for depression in primary care cost-effective? J Ment Health Policy Econ. 2008;11(1):3–15. [PubMed] [Google Scholar]
- 54.Wiles N, Thomas L, Abel A, et al. Clinical effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: the CoBalT randomised controlled trial. Health Technol Assess. 2014;18(31):1–167, vii–viii. [DOI] [PMC free article] [PubMed] [Google Scholar]