Abstract
PURPOSE
We assess the financial implications for primary care practices of participating in patient-centered medical home (PCMH) funding initiatives.
METHODS
We estimated practices’ changes in net revenue under 3 PCMH funding initiatives: increased fee-for-service (FFS) payments, traditional FFS with additional per-member-per-month (PMPM) payments, or traditional FFS with PMPM and pay-for-performance (P4P) payments. Net revenue estimates were based on a validated microsimulation model utilizing national practice surveys. Simulated practices reflecting the national range of practice size, location, and patient population were examined under several potential changes in clinical services: investments in patient tracking, communications, and quality improvement; increased support staff; altered visit templates to accommodate longer visits, telephone visits or electronic visits; and extended service delivery hours.
RESULTS
Under the status quo of traditional FFS payments, clinics operate near their maximum estimated possible net revenue levels, suggesting they respond strongly to existing financial incentives. Practices gained substantial additional net annual revenue per full-time physician under PMPM or PMPM plus P4P payments ($113,300 per year, 95% CI, $28,500 to $198,200) but not under increased FFS payments (−$53,500, 95% CI, −$69,700 to −$37,200), after accounting for costs of meeting PCMH funding requirements. Expanding services beyond minimum required levels decreased net revenue, because traditional FFS revenues decreased.
CONCLUSIONS
PCMH funding through PMPM payments could substantially improve practice finances but will not offer sufficient financial incentives to expand services beyond minimum requirements for PCMH funding.
Keywords: primary health care, models, theoretical, capitation fee, fee-for-service plans, patient-centered care
INTRODUCTION
As of 2014 at least 114 distinct initiatives from state, federal, and private payers funded primary care clinics to offer services as patient-centered medical homes (PCMHs)—practices delivering comprehensive care for most health problems; coordinating care among multiple clinicians; and achieving heightened standards for accessibility, quality, and safety.1–4 These initiatives, which now involve at least 21 million patients in the United States,4 intend to improve access and quality while delivering population-based care at lower cost.1–3 To do so amidst workforce constraints, practices face challenges, including adopting process improvement techniques and electronic registries for care management, expanding care teams, offering patients longer in-person visits and access to electronic or telephone visits, and extending night and/or weekend business hours to enhance care access.1,5–8 According to recent national surveys, 3 major payment strategies have dominated PCMH initiatives: increased fee-for-service (FFS) payments, traditional FFS payments with additional per-member-per-month (PMPM) payments, and traditional FFS payments with PMPM and pay-for-performance (P4P) payments.4,7
To date, studies of PCMH performance have tracked patient outcomes and total medical spending, with generally positive quality but mixed cost results.9–19 An unaddressed question, however, is how current PCMH funding models affect the financial sustainability of primary care practices and particularly whether current PCMH payment initiatives provide sufficient incentives for meaningful practice transformation. One emerging concern is that practices may minimally reform delivery in response to PCMH payment requirements while still pursuing a practice model that maximizes traditional FFS revenue.20,21 Here, we estimate the revenue and cost implications to primary care practices of delivering services funded by PCMH payment initiatives.
METHODS
We used a previously validated microsimulation model of primary care practices22,23 to estimate practice-level changes in net annual revenue after PCMH transformation under each of 3 dominant payment approaches supporting PCMH transformation. (increased FFS, PMPM, or PMPM plus P4P).
Microsimulation Model
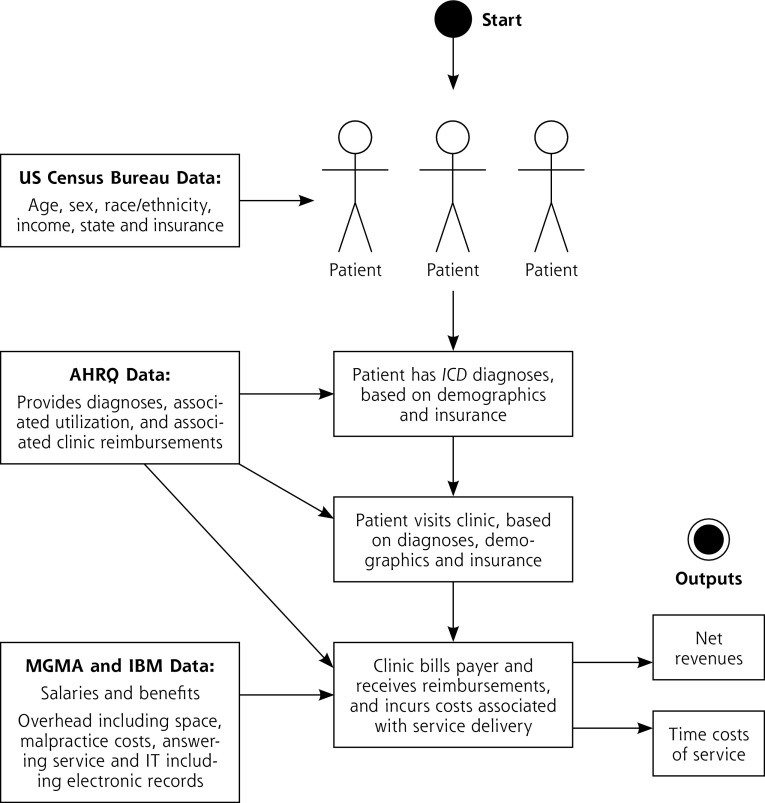
Our model combines (1) a patient-level simulation of patients attending primary care clinics with (2) a practice-level simulation of revenues and costs of service delivery to each clinic (Figure 1). The model was populated by sampling from detailed clinic utilization, revenue, and cost data from national surveys of primary care clinics, including clinics before and after PCMH transformation (Table 1). By structuring the model as a microsimulation, we account for the covariance between practice characteristics and patient characteristics, including billing practice variations. Comprehensive details are provided in the Supplemental Appendix (http://www.annfammed.org/content/14/5/404/suppl/DC1).
Figure 1.
Model flow diagram.
AHRQ = Agency for Healthcare Research and Quality; IBM = International Business Machines; ICD = International Classification of Diseases; IT = information technology; MGMA = Medical Group Management Association.
Table 1.
Data Inputs to the Model
| Parameter | Details | Source |
|---|---|---|
| Population demographics within each state population | ||
| Age, y | Cohorts of <5, 5–13, 14–17, 18–24, 25–44, 45–64, 65–84, and >84 y | US Census Bureau24 |
| Sex | Cohorts of male or female | |
| Race/ethnicity | Cohorts of non-Hispanic white, non-Hispanic black, Hispanic, and other | |
| Income | Housing income relative to household size, expressed relative to federal poverty level | |
| Insurance status | Cohorts of private, Medicare, Medicaid/CHIP, or self-pay | |
| Patient features | ||
| Diagnoses among each demographic group | International Classification of Disease, Ninth Revision | Agency for Healthcare Research and Quality25 |
| Per-person utilization of primary care clinics | Visits per person per year, conditional on demographics, diagnoses, and state of residence | |
| Practice features | ||
| Reimbursement for each primary care visit | Specific to diagnoses and payer | Agency for Healthcare Research and Quality25 |
| Productivity of primary care physicians and midlevel clinicians | Encounters and empanelment per clinician per year, by clinician type (physician, NP, PA) | Medical Group Management Association26 |
| Utilization changes associated with changes in staff | Changes in encounters and empanelment given levels of support staffa | |
| Staffing ratios of midlevel clinicians and support staff per full-time physician | Including NPs, PAs, RNs, LPNs, and MAs | |
| Overhead costs | Including staff benefits, building and occupancy, information technology, drug and medical supply, equipment and administrative supplies, liability insurance and fees, laboratory and imaging fees, and other ancillary service costs | |
| Compensation costs for clinician | Salary per full-time physician or midlevel clinician per year | Bureau of Labor Statistics27 |
| Compensation costs for support staff | Salary per full-time worker per year, by worker type | IBM Kenexa Compensation Analysis28 |
| New financing approaches | ||
| Increased FFS payment rates | Median increase of 12% above current CPT codes (95% CI, 10%–14%)b | CareFirst BlueCross BlueShield29 |
| PMPM payment rates | Median of $4.90 per empaneled patient per month (95% CI, $3.00–$8.00) | Survey of patient-centered medical home initiatives4 |
| P4P payment rates | Median receipt rate of $2.63 per empaneled patient per annum (95% CI, $1.08–$4.17)c | National Academy for State Health Policy1 |
| Empanelment rate among new patient encounters (to charge new PMPM fees during panel expansion) | Median of 53% of new encounters (95% CI, 42%–64%) who become additional panel members | Medical Group Management Association26 |
| Reimbursement codes for electronic and telephone visits | 99444 for electronic, 99441 for telephone, varied by state and payer | Center for Connected Health Policy30 |
| Additional infrastructure costs for electronic visits | $240 per year (95% CI, $0–$360) | Telehealth Resource Center31 |
| Encounter rate per extended business hour | Regression model of utilization per extended hourd | Agency for Healthcare Research and Quality25 |
CHIP = Children’s Health Insurance Program; CPT = Current Procedural Terminology; FFS = fee for service; IBM =International Business Machines; LPN = licensed practical nurse; MA = medical assistant; NP = nurse practitioner; PA = physician assistant; P4P = pay for performance; PMPM = per-member-per-month; RN = registered nurse.
Note: See Supplemental Appendix Tables 1 and 2 and Supplemental Appendix Figure 1 for full parameter values, http://www.annfammed.org/content/14/5/404/suppl/DC1.
See the Supplemental Appendix Figure 1, http://www.annfammed.org/content/14/5/404/suppl/DC1.
Confidence intervals are estimates of the distribution of input data, not the results of a model of population data estimates, and are used to construct normal probability distributions from which to perform repeated sampling in our probabilistic uncertainty analyses.
Receipt rate incorporates the observed rate of performance target achievement, which we varied in sensitivity analyses from a baseline estimate of 10% to a lower and upper bound of 0% to 100%.32
See the Supplemental Appendix, http://www.annfammed.org/content/14/5/404/suppl/DC1.
At the patient level, the model simulates representative populations of each state and Washington, DC,24 and insurance coverage estimates among each population subsequent to the Patient Protection and Affordable Care Act33 (Supplemental Appendix Table 1, http://www.annfammed.org/content/14/5/404/suppl/DC1). Based on age, sex, race/ethnicity, income, and insurance status, the model assigns diagnoses to each individual (by International Classification of Disease-Ninth Revision) to reflect the distribution of diagnoses (including comorbidities) across demographic groups,25 then estimates the number of outpatient visits and payments to clinics associated with these visits.25 Payment estimates account for geographic variations in billing and reimbursement by clinician and payer.
At the practice level, the model estimates visits and payments to primary care practices per year using national survey data.26 The model calculates practice costs for both personnel (staffing ratios and staff salaries per full-time physician)28 and overhead expenditures (staff benefits, building/occupancy, information technology, medical supply equipment, administrative supplies, liability insurance and fees, laboratory and imaging fees, and other ancillary service costs)34 (Supplemental Appendix Table 2, http://www.annfammed.org/content/14/5/404/suppl/DC1). All revenues and costs are expressed in 2015 US dollars using the Consumer Price Index to adjust for inflation.35
For validation, we ensured our model’s estimates of utilization, cost, and revenue were within 5% error of independent survey data36 and revenue and cost data among both pretransformation37 and posttransformation38 primary care clinics (Supplemental Appendix Figure 2, http://www.annfammed.org/content/14/5/404/suppl/DC1).
PCMH Simulation
We first calculated the changes in costs and revenues per full-time equivalent (FTE) physician if practices changed minimally to meet criteria for new PCMH funding (base case), then estimated what changes to service delivery would maximize net revenues under the new PCMH funding approaches. To provide optimistic financial sustainability estimates for PCMHs, we did not include highly variable up-front costs of transformation in our base-case simulation,39 only the costs to maintain PCMH functions after transformation. Furthermore, we defined the minimum criteria to match the standards accepted for PCMH financing by payers responding to a previous national PCMH survey,4 which included basic (level 1) PCMH standards for accreditation by the National Committee for Quality Assurance (NCQA) and accreditation by other major agencies, including the Utilization Review Accreditation Commission and the Joint Commission. The criteria were not limited to NCQA level 3 recognition because many PCMH payment initiatives have been funding practices as PCMHs despite not meeting level 3 criteria; with the more inclusive definition, our results favor PCMH maintenance (ie, does not inflate our cost estimates). Typical staff ratios among practices meeting PCMH criteria were obtained from a survey of 502 practices in 7 regions.40
Minimum costs of PCMH maintenance included physical infrastructure charges for patient tracking, quality improvement, communications, and related infrastructure, averaging in 2015 US dollars $2.51 per patient per month (95% CI, $0.95–$4.57) estimated from a national survey of 1,009 practices38 (updated from $2.26 in 2009 dollars using the Consumer Price Index, not significantly different from the estimate of $2.08, 95% CI, $0.58–$4.83, from a more limited survey of 20 practices, excluding one-time transformation costs,39 and estimates from smaller surveys in Utah [8 practices, $3.85] and Colorado [12 practices, $4.83]).41 Salaries and overhead costs incurred for support staff were incorporated into all cost tabulations (Supplemental Appendix and Table 1), whereas the effects of support staff on clinic efficiency and productivity (eg, through extended team roles) were incorporated by Monte Carlo sampling from the probability distribution of encounters and revenue associated with different staffing ratios26 (Supplemental Appendix Figure 1, http://www.annfammed.org/content/14/5/404/suppl/DC1). As an additional check of face validity, our estimates for PCMH monthly maintenance costs per 1 FTE physician were approximately $70,750 (95% CI, $10,670–$51,320), not significantly different from the independent estimate of $64,768 per year (95% CI, 18,585–$83,856) from a recent survey of 12 practices.39
FFS revenues were assigned for each visit according to Table 1. Median PMPM rates, obtained from a national survey of PCMH funding initiative participants (Table 1),4 were multiplied by the number of empaneled patients, estimated as the number of encounters multiplied by the ratio of empaneled patients to encounters (median of 53% of visits are empaneled, 95% CI, 42% to 64%, per national practice surveys [Table 1], and increased in sensitivity analyses).26 P4P bonuses (Table 1) were distributed at the mean achievement rate of approximately 10% (also increased in sensitivity analyses).32
We next estimated changes in revenues and costs if practices offered PCMH functionality beyond minimum levels required for funding by increasing the staffing ratios above the minimum levels observed in a survey of 502 transforming practices across the nation40 and by altering visit templates and service hours as anticipated under the PCMH model. Visit template alterations included (1) extending visit length by 5 minutes, lowering overall visit volume per day but using higher billing codes that reflected more time spent per patient; or (2) converting 10% of routine follow-up visits to electronic or telephone visits (reimbursed per payer-specific rates for CPT [Current Procedural Terminology] code 99444 for 10-minute electronic visits, or 99441 for 10-minute telephone visits), and adding 5 minutes documentation time and infrastructure costs (Table 1).30,31,42 Shifting established patients to electronic or telephone visits enabled practices to open appointment slots for new and established patients. We distributed the open slots among new vs established patients in the same ratio as existing visit ratios at each clinic. Extended service hours included evening and weekend business hours during which the typical number of visits per hour was estimated from the Medical Expenditure Panel Survey (Table 1)25; costs of extending service hours included staff compensation for a physician or nurse practitioner, plus hourly overhead costs including support staff for the clinician, building space, and utility costs (Supplemental Appendix Table 2).26
Optimization
We performed an optimization analysis to identify what changes to support staff, visit templates, and service delivery hours would maximize net revenue before and after PCMH transformation. A generalized pattern search algorithm was used to repeatedly run the model across all possible combinations of staff, visit, and delivery hour changes to maximize net revenue per FTE physician under each payment approach.43
Break-Even Analysis
We estimated the probability that a PCMH would maintain positive net revenue after several possible service delivery changes: if adding 1 FTE for each type of support staff (care coordinator, registered nurse [RN], licensed practical nurse [LPN], or medical assistant [MA]) if adding 5 minutes to each visit (with coding also increased 1 level for these longer visits), if converting 10% of in-person visits to telephone or electronic visits, or if adding 1 business day equivalent (8 hours of evening/weekend service) per week in a practice of 5 FTE physicians (the median practice size). The probability was calculated by running the model 10,000 times, drawing repeatedly from the range of each input parameter (Supplemental Appendix Table 2 and Supplemental Appendix Figure 1) to estimate the frequency with which the clinic achieved positive net revenues after each service delivery change.44
Sensitivity Analyses
In sensitivity analyses, we varied the P4P bonus achievement rate (to 100%). We also varied PCMH payment rates, service delivery costs, and patient utilization rates from 80% to 120% of their base-case values (Table 1). We further investigated whether PCMH transformation produced such clinical efficiency that costs of PCMH maintenance became negative (a net cost savings) at up to $5 saved per patient per month. We explored the impact of risk-adjusting PMPM rates using the algorithm utilized by the Centers for Medicare and Medicaid Services.45 Finally we performed subgroup analysis by state to identify geographic variations in net revenue (Supplemental Appendix).
All analyses were performed in R (v. 3.1.2, The R Foundation for Statistical Computing).
RESULTS
In the primary data sources used to populate the model, median gross annual revenues among primary care practices were $487,390 per year from standard FFS payments (95% CI, $205,231–$955,765) from a total of $871,069 in charges (95% CI, $365,54–$1,749,134) per FTE physician.26 Based on these gross revenues, costs of clinic operations per FTE physician, including physician and support staff salaries and benefits, material costs, and overhead expenditures, totaled $443,569 (95% CI, $182,882–$876,449) per year.26
Financial Outcomes Before Medical Home Transformation
Before PCMH transformation, practice revenue optimization did not require major modifications to baseline support staffing ratios, visit templates, or service delivery hours to maximize net annual revenues from traditional FFS payments. The staffing ratios that maximized net revenues included 0 FTEs for a care coordinator, 0.45 FTEs for RNs, 0.78 FTEs for LPNs, and 1.25 FTEs for MAs per 1 FTE physician (Supplemental Appendix). Visit duration did not increase, nor were electronic or telephone visits included (because of lost FFS revenue from routine office visit volume; Table 2). Evening and weekend business hours increased slightly (to 2.7 evening or weekend hours per week), beyond which overhead and staffing costs exceeded expected revenues from extended business hours.
Table 2.
Model-Based Estimates of Changes in Net Revenue per Full-Time Physician for Primary Care Clinics Delivering PCMH Services Compared With the Net Revenue in the Traditional FFS Clinic Before PCMH Transformation
| Change in Net Revenue ($/FTE physician/year) | Traditional FFS $ (95% CI) | Increased FFS $ (95% CI) | PMPM $ (95% CI) | PMPM plus P4P Bonuses $ (95% CI) | Maximizing Net Revenues Under PCMH Payment Initiatives |
|---|---|---|---|---|---|
| Minimum required changes for PCMH fundinga | N/A | −53,464 (−69,725 to −37,203) |
103,835 (24,462 to 183,208) |
113,343 (28,511 to 198,176) |
N/A |
| Service delivery enhancements | |||||
| Optimize staff ratiob | 46,722 (25,737 to 155,577) |
−53,464 (−69,725 to −37,203) |
103,835 (24,462 to 183,208) |
113,343 (28,511 to 198,176) |
FTEs: 0.23 CC, 0.31 RN, 0.53 LPN, 1.11 MA |
| Extend visit length by 5 minc | −119,092 (−170,874 to −83,002) |
−184,925 (−255,049 to −149,057) |
−62,771 (−156,974 to −57,134) |
−55,390 (−152,320 to −52,719) |
Not in optimal result |
| Replace 10% of visits with electronic visitsd | −16,175 (−17,134 to −15,165) |
−71,497 (−83,935 to −59,960) |
80,427 (11,394 to 145,836) |
89,610 (15,611 to 159,704) |
Not in optimal result |
| Replace 10% of visits with telephone visitsd | −16,151 (−17,107 to −15,144) |
−71,473 (−83,915 to −59,931) |
80,451 (11,413 to 145,868) |
89,634 (15,629 to 159,736) |
Not in optimal result |
| Extend evening/weekend hourse | 380 (373 to 386) | −52,959 (−69,227 to −36,692) |
104,781 (25,402 to 184,160) |
114,321 (29,482 to 199,159) |
3.0–3.8 h/wk |
| Net revenue-maximizing combinationf | 47,101 (26,110 to 155,963) |
−52,959 (−69,227 to −36,692) |
104,781 (25,402 to 184,160) |
11,4321 (29,482 to 199,159) |
FTEs: 0.23 CC, 0.31 RN, 0.53 LPN, 1.11 MA + 3.0–3.8 h/wk evening/weekend service |
CC = care coordinator; FFS = fee for service; FTE = full-time equivalent; LPN = licensed practical nurse; MA = medical assistant; P4P = pay for performance; PCMH = patient-centered medical home; PMPM = per member per month; RN = registered nurse.
Note: Revenues include 4 funding scenarios: traditional FFS, increased FFS, PMPM, and PMPM plus P4P bonus. Confidence intervals in parentheses are from probabilistic sensitivity analyses in which the model was rerun 10,000 times while sampling from the probability distributions of all input parameters to generate confidence intervals around model results.
Meets basic criteria of PCMH funding initiatives, cataloged previously,4 incorporating changes in communication, care management, external coordination, patient tracking, test/referral tracking, and quality improvement at an inflation-adjusted cost of $2.51 per patient per month (95% CI, $0.95–$4.57).35 Staffing ratios include a minimum of 0.23 FTE for a CC (0.21–0.25), 0.31 FTE for an RN (0.28–0.34), 0.53 FTE for an LPN (0.50–0.56), and 1.11 FTE for an MA per FTE physician (1.09–1.13).40 Probabilistic sensitivity and uncertainty analyses performed across the listed CIs through repeated sampling from corresponding normal distributions of minimum staffing levels to assess robustness of results. All costs expressed in 2015 US dollars.
Adjusted support staff (CC, RN, LPN, and MA) levels per full-time physician, determined by repeated sampling from observed joint probability distributions linking staffing levels across clinicians and support staff to encounters and empanelment (Supplemental Appendix Figure 1, http://www.annfammed.org/content/14/5/404/suppl/DC1), then detecting which combinations of staffing levels maximized net revenue while still meeting the minimum PCMH funding requirements. Note that maximum net revenue was achieved by minimum staffing in all PCMH funding scenarios.
Increasing visits by 5 minutes each from the baseline length at each simulated clinic.
Simulated as replacing 10% of regular in-person encounters.
Optimization involved finding the number of evening or weekend hours per week that would maximize net revenues for the clinic, calculating medical revenue from each additional business hour of providing service availability during nights and weekends via a midlevel practitioner, and subtracting the costs of compensation and overhead expenditure for those hours.
Includes optimized clinic activities in all above-mentioned domains.
Financial Outcomes After Medical Home Transformation
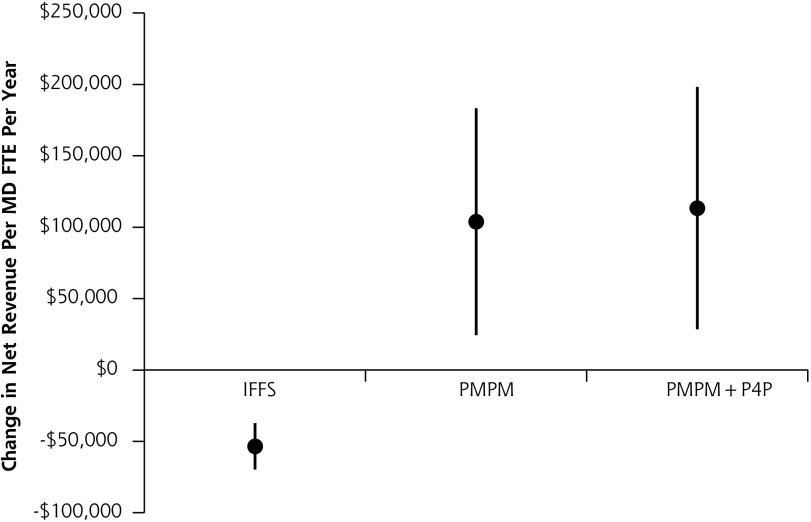
Under current types of PCMH funding initiatives, practices experienced increases in gross annual revenue of $55,700 to $222,500 when only minimally reforming their staffing ratio and infrastructure to meet funding requirements (Table 2). At piloted rates of reimbursement, increased FFS financing generated the least revenue compared with PMPM or PMPM plus P4P. Net revenue under increased FFS financing was lower after PCMH transformation than under traditional FFS payments before PCMH transformation ($53,464 lost per FTE physician per year, 95% CI, $37,203–$69,725 lost). PMPM and PMPM plus P4P, by contrast, always resulted in net revenue gains compared with traditional FFS (Table 2 and Figure 2).
Figure 2.
Net revenue changes per full-time physician per year from clinics meeting minimum requirements to receive PCMH funding, as compared with the clinic operating under traditional fee-for-service payments.
IFFS = increased fee for service; P4P = pay for performance; PCMH = patient-centered medical home; PMPM = per-member-per-month.
Note: The PCMH funding approaches include IFFS rates, PMPM funding, and PMPM plus P4P bonuses (Table 1). The uncertainty ranges portrayed incorporate 3 sets of uncertainty through repeated sampling from the probability distributions of the input parameters: uncertainty in levels of utilization and associated revenue, cost to the practice including staff compensation and other practice costs, and payments through the new PCMH financing approaches (eg, level of payment increase from IFFS).
Altered Staffing Ratios
As shown in Table 2, increasing staff beyond the minimum required for PCMH funding reduced net revenue under all scenarios. The costs of salary, benefits, and overhead for staff exceeded the revenue benefits from increased efficiency and support from a greater number of staff members. Probabilistic sensitivity and uncertainty analyses across the range of observed minimum staffing levels (Table 1) did not alter this outcome.
Altered Visit Templates
Extending visit length or offering electronic or telephone visits reduced net revenue because of the staffing costs of implementation (Table 2). In the most revenue-generating scenario, where clinics adopted the PMPM plus P4P payment model, no new revenues were produced, but new annual costs of $168,700 were incurred from extending visit length by 5 minutes (as a result of lost FFS revenue from forfeited visits).
Extended Business Hours
By contrast, extended business hours increased net revenues for practices. Under the increased FFS approach, net revenue was maximized by extending evening or weekend hours to 3.0 hours per week (95% CI, 2.7–3.2 hours), whereas under both the PMPM and PMPM plus P4P approaches, net revenue was maximized by increasing hours to 3.8 hours per week. At these levels, net revenues increased marginally by between $500 and $1,000 per year per FTE physician (Table 2). Beyond these extended hours levels, salary and overhead costs of each additional hour exceeded anticipated revenues.
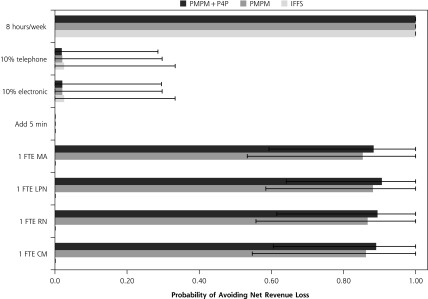
Break Even Analysis
Figure 3 illustrates the probability that a clinic, after meeting minimum practice transformation requirements, would maintain positive net revenues after increasing support staff, altering visit templates, or extending service hours under the new PCMH financing approaches. The probability that the new PCMH funding could support the addition of 1 FTE care coordinator for a median practice size of 5 FTE physicians ranged from 0% under increased FFS to 89% (95% CI, 55%–100%) under PMPM plus P4P bonuses. The probability was low for supporting routine electronic or telephone visits (less than 5%), and high for supporting extended business hours (100% in all simulation scenarios).
Figure 3.
Break even analysis, which identified the probability with which key medical home services could be supported by a clinic without achieving negative net revenue.
CC = care coordinator; FTE = full-time equivalent; IFFS = increased fee for service; LPN = licensed practical nurse; MA = medical assistant; P4P = pay for performance; PMPM = per member per month; RN = registered nurse.
Note: We specifically calculated the probability that a clinic would not lose net revenue through the addition of 1 FTE for each type of support staff (CC, RN, LPN, and MA); when adding 5 minutes to each visit; when converting 10% of routine visits to electronic or telephone visits; or when adding 1 full business day (8 evening/weekend business hours) per week in a median practice size of 5 FTE physicians.
Sensitivity Analyses
Sensitivity analyses did not produce significant changes to the staffing ratios, visit templates, or business hours that maximized net revenues for clinics. Increasing the P4P bonus success rate from 10% to 100% (Supplemental Appendix Table 3, http://www.annfammed.org/content/14/5/404/suppl/DC1) increased net revenues by $88,900 per FTE physician per year under the PMPM funding approach plus P4P bonuses. Varying payment rates in each PCMH financing approach minimally changed the optimal number of extended business hours (Supplemental Appendix Tables 4–5, http://www.annfammed.org/content/14/5/404/suppl/DC1). Under higher payment rates, altering visit templates to extend visit length or adding telephone or electronic visits generated greater losses to clinics than in the base case, because lost in-person visit revenue was greater. Varying service delivery costs and patient utilization rates produced minimal changes to revenue-maximizing number of extended business hours without otherwise altering the optimization results (Supplemental Appendix Tables 6–9, http://www.annfammed.org/content/14/5/404/suppl/DC1). The optimization result also did not change whether PCMH maintenance produced net savings instead of costs, or whether PMPM rates were risk-adjusted (Supplemental Appendix Tables 10 and 11, http://www.annfammed.org/content/14/5/404/suppl/DC1). Variations in patient population, billing behavior, and reimbursement rates by state did not change practice optimization, but they did produce as much as a $76,400/year per FTE physician difference in net revenue after PCMH transformation in different states (Supplemental Appendix Table 12, http://www.annfammed.org/content/14/5/404/suppl/DC1).
DISCUSSION
Although investments in the PCMH should be informed by benefits to patient care, the decision at a practice level remains influenced by financial outcomes, particularly given the tenuous financial sustainability of many primary care practices. The goal of primary care practice is to improve patient care. PCMH transformation has the additional goal of increasing general investment in primary care. Achieving these goals requires financial sustainability over the near-term, but the costs of these goals have been prohibitive, and providing high-value care has in turn been limited.
Our model-based analyses suggest that if PCMH funding initiatives were expanded through current PMPM-based funding approaches (but not increased FFS at currently-piloted rates), primary care practices could expect to gain net revenue by participating in the initiatives. Although clinics under the traditional FFS payment system are operating near their revenue-maximizing levels of staffing and service delivery—suggesting that clinics are highly responsive to financial incentives—they would not gain additional revenues by investing incremental PCMH payments in increasing staff or altering visit templates beyond the minimally required levels to meet PCMH funding requirements. The costs of hiring additional clinic staff were not offset by increased clinic efficiency or workflow. Extending in-person visits or offering minimally or unreimbursed telephone or electronic visits resulted in lost revenue generated by traditional FFS office-based visits.
These findings contribute important new insights to the literature on PCMHs, explaining why some previous evaluations of PCMH demonstrations have shown mixed impact. Studies have not clearly established what factors determine whether PCMH transformations are financially sustainable for practices. Our model suggests that although PCMH transformation initiatives have adopted a team-based delivery approach,14,15,46 more radical payment reforms may be required to adequately fund these changes at the practice level. Phrased differently, practices must receive more robust non–visit-based payment mechanisms to provide an incentive to sustain transformation. The recently announced Comprehensive Primary Care Plus model aims to promote this type of payment reform in its Track 2, which incorporates higher PMPM amounts, larger performance bonuses, and perhaps most importantly, upfront per capita population-based payments that offset gradual reductions in FFS reimbursements.47
Our study fills an important gap in the literature because existing demonstration-project evaluation efforts have focused on system-level cost savings (eg, through fewer emergency department or specialty visits), which have been inconsistently observed.10,14–16,18,48–62 For many practices, revenue gains must be observed at the practice level to justify practice-level workforce and time use changes. Another key advantage is that our modeling allows us to compare different reforms in the same practices, unlike demonstration projects for which it is unclear whether differences in outcomes are due to differences in the PCMH funding program itself or preexisting practice differences.
Our findings were robust to wide variations in levels of payment, cost, and clinic performance but have some important limitations. There are insufficient or no publicly available data on some new PCMH funding strategies, such as fully capitated payment, shared-savings programs, and the alternative payment model from Medicare. Our model will have to be extended as new payment strategies emerge with large-scale data. The number of staff required to meet PCMH requirements in the model was also based on a pilot study involving a limited sample size of practices that elected into transformation40; nationwide, less ambitious or PCMH-ready clinics may require even more staff to assist in transformation, rendering our results conservative. Our results are also conservative because we examined the net revenue after transformation, not the costs of transformation itself, which remains highly variable.
Some clinics may choose to lose revenue in the interest of service enhancement, as long as they remain financially sustainable. Hence, we examined what levels of service would permit clinics to break even. Expanding business hours would be among the most revenue-generating strategies for delivering PCMH services, consistent with earlier findings,63 and could be adopted sustainably under any of the PCMH funding initiatives. Notably, however, the current level of incentivized extended business hours were limited to about 3 hours per week, which may not be of important clinically.
Our model does not provide an answer to what practices should do, only what fiscal outcomes may occur after different decisions. We cannot predict health or experiential changes, which can be more directly assessed through traditional evaluation methods3,6,64–72; hence, we focused on the financial implications of practice-level management decisions, which are often assessed through modeling.
In a microsimulation model of primary care practices, current PMPM-based funding for patient-centered medical homes may enhance finances for practices but offers only minimal incentives to change staffing ratios and service delivery strategies. Achieving goals of the PCMH will likely require more radical payment reforms specifically to target funding toward the delivery of desired services.
Footnotes
Conflicts of interest: Asaf Bitton serves part-time as a senior advisor to the Comprehensive Primary Care initiative at the Center for Medicare and Medicaid Innovation (CMMI).
Disclaimer: The ideas expressed herein are solely the authors’ and do not represent any official position of the Center for Medicare and Medicaid Innovation.
Supplementary materials: Available at http://www.AnnFamMed.org/content/14/5/404/suppl/DC1/.
References
- 1.National Academy for State Health Policy. Medical Home & Patient-Centered Care Database. Portland, OR: NASHP; 2014. [Google Scholar]
- 2.Rittenhouse DR, Shortell SM. The patient-centered medical home: will it stand the test of health reform? JAMA. 2009;301(19): 2038–2040. [DOI] [PubMed] [Google Scholar]
- 3.Ferrante JM, Balasubramanian BA, Hudson SV, Crabtree BF. Principles of the patient-centered medical home and preventive services delivery. Ann Fam Med. 2010;8(2):108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Edwards ST, Bitton A, Hong J, Landon BE. Patient-centered medical home initiatives expanded in 2009–13: providers, patients, and payment incentives increased. Health Aff (Millwood). 2014;33(10):1823–1831. [DOI] [PubMed] [Google Scholar]
- 5.Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med. 2008;21(5): 427–440. [DOI] [PubMed] [Google Scholar]
- 6.Jackson GL, Powers BJ, Chatterjee R, et al. Improving patient care. The patient centered medical home. A Systematic Review. Ann Intern Med. 2013;158(3):169–178. [DOI] [PubMed] [Google Scholar]
- 7.Bitton A, Martin C, Landon BE. A nationwide survey of patient centered medical home demonstration projects. J Gen Intern Med. 2010;25(6):584–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel MS, Arron MJ, Sinsky TA, et al. Estimating the staffing infrastructure for a patient-centered medical home. Am J Manag Care. 2013;19(6):509–516. [PubMed] [Google Scholar]
- 9.Nelson KM, Helfrich C, Sun H, et al. Implementation of the patient-centered medical home in the Veterans Health Administration: associations with patient satisfaction, quality of care, staff burnout, and hospital and emergency department use. JAMA Intern Med. 2014;174(8):1350–1358. [DOI] [PubMed] [Google Scholar]
- 10.DeVries A, Li C-HW, Sridhar G, Hummel JR, Breidbart S, Barron JJ. Impact of medical homes on quality, healthcare utilization, and costs. Am J Manag Care. 2012;18(9):534–544. [PubMed] [Google Scholar]
- 11.Alexander JA, Bae D. Does the patient-centred medical home work? A critical synthesis of research on patient-centred medical homes and patient-related outcomes. Health Serv Manage Res. 2012;25(2):51–59. [DOI] [PubMed] [Google Scholar]
- 12.Hebert PL, Liu C-F, Wong ES, et al. Patient-centered medical home initiative produced modest economic results for Veterans Health Administration, 2010–12. Health Aff (Millwood). 2014;33(6):980–987. [DOI] [PubMed] [Google Scholar]
- 13.Han E, Hudson Scholle S, Morton S, Bechtel C, Kessler R. Survey shows that fewer than a third of patient-centered medical home practices engage patients in quality improvement. Health Aff (Millwood). 2013;32(2):368–375. [DOI] [PubMed] [Google Scholar]
- 14.Bielaszka-DuVernay C. Vermont’s Blueprint for medical homes, community health teams, and better health at lower cost. Health Aff (Millwood). 2011;30(3):383–386. [DOI] [PubMed] [Google Scholar]
- 15.Harbrecht MG, Latts LM. Colorado’s Patient-Centered Medical Home Pilot met numerous obstacles, yet saw results such as reduced hospital admissions. Health Aff (Millwood). 2012;31(9):2010–2017. [DOI] [PubMed] [Google Scholar]
- 16.Raskas RS, Latts LM, Hummel JR, Wenners D, Levine H, Nussbaum SR. Early results show WellPoint’s patient-centered medical home pilots have met some goals for costs, utilization, and quality. Health Aff (Millwood). 2012;31(9):2002–2009. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal MB, Friedberg MW, Singer SJ, Eastman D, Li Z, Schneider EC. Effect of a multipayer patient-centered medical home on health care utilization and quality: the Rhode Island chronic care sustainability initiative pilot program. JAMA Intern Med. 2013;173(20):1907–1913. [DOI] [PubMed] [Google Scholar]
- 18.Friedberg MW, Schneider EC, Rosenthal MB, Volpp KG, Werner RM. Association between participation in a multipayer medical home intervention and changes in quality, utilization, and costs of care. JAMA. 2014;311(8):815–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schneider EC. Strengthening Primary Care Amid the Hype. The Commonwealth Fund. http://www.commonwealthfund.org/publications/blog/2015/jun/strengthening-primary-care-amid-the-hype. Published Jun 1, 2015 Accessed Jul 15, 2015.
- 20.Landon BE. Structuring payments to patient-centered medical homes. JAMA. 2014;312(16):1633–1634. [DOI] [PubMed] [Google Scholar]
- 21.Saultz JW, Jones SM, McDaniel SH, et al. A new foundation for the delivery and financing of American health care. Fam Med. 2015;47(8):612–619. [PubMed] [Google Scholar]
- 22.Basu S, Landon BE, Song Z, Bitton A, Phillips RS. Implications of workforce and financing changes for primary care practice utilization, revenue, and cost: a generalizable mathematical model for practice management. Med Care. 2015;53(2):125–132. [DOI] [PubMed] [Google Scholar]
- 23.Basu S, Phillips RS, Bitton A, Song Z, Landon BE. Medicare chronic care management payments and financial returns to primary care practices. Ann Intern Med. 2015;163(8):580–588. [DOI] [PubMed] [Google Scholar]
- 24.US Census Bureau. Current Population Survey: Annual Social and Economic Supplements. Washington, DC: US Census Bureau; 2013. [Google Scholar]
- 25.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. Washington, DC: AHRQ; 2013. [Google Scholar]
- 26.Medical Group Management Association. DataDive. Englewood, CO: MGMA; 2015. [Google Scholar]
- 27.Bureau of Labor Statistics. Employer Costs for Employee Compensation. http://www.bls.gov/news.release/ecec.toc.htm. Published 2014 Accessed Jul 21, 2013 Updated Jun 9, 2016.
- 28.Kenexa IBM. CompAnalyst Market Data. Armonk, NY: IBM; 2015. [Google Scholar]
- 29.CareFirst BlueCross BlueShield. Patient-Centered Medical Home Program Shows Promising Quality Trends and Continued Savings on Expected Costs. Baltimore: BlueCross BlueShield; 2014. [Google Scholar]
- 30.Center for Connected Health Policy. State Telehealth Policies and Reimbursement Schedules: A Comprehensive Plan of the 50 States and District of Columbia. Sacramento, CA: CCHP; 2014. [Google Scholar]
- 31.Neufeld J. Telehealth Costs, Business Models, Risks, and Savings Strategies. Terra Haute, IN: Upper Midwest Telemedicine Resource Center; 2015. [Google Scholar]
- 32.Scott A, Sivey P, Ait Ouakrim D, et al. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database Syst Rev. 2011; 7(9):CD008451. [DOI] [PubMed] [Google Scholar]
- 33.Congressional Budget Office. Effects of the Affordable Care Act on Health Insurance Coverage - Baseline Projections. Washington, DC: CBO; 2015. https://www.cbo.gov/publication/43900 Accessed Feb 12, 2015. [Google Scholar]
- 34.Basu S, Landon B, Song Z, Bitton A, Phillips R. Implications of workforce and financing changes for primary care practice utilization, revenue, and cost: a generalizable mathematical model for practice management. Med Care. 2015;53(2):125–132. [DOI] [PubMed] [Google Scholar]
- 35.Bureau of Labor Statistics. Consumer Price Index (CPI). http://www.bls.gov/cpi/ Published 2014 Accessed Sep 26, 2013.
- 36.Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey (Namcs). Atlanta, GA: CDC; 2014. [Google Scholar]
- 37.Medical Group Management Association. Cost Survey for Single-Specialty Practices. Englewood, CO: MGMA; 2014. [Google Scholar]
- 38.Nocon RS, Sharma R, Birnberg JM, Ngo-Metzger Q, Lee SM, Chin MH. Association between patient-centered medical home rating and operating cost at federally funded health centers. JAMA. 2012;308(1):60–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martsolf GR, Kandrack R, Gabbay RA, Friedberg MW. Cost of transformation among primary care practices participating in a medical home pilot. J Gen Intern Med. 2016;31(7):723–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peikes DN, Reid RJ, Day TJ, et al. Staffing patterns of primary care practices in the comprehensive primary care initiative. Ann Fam Med. 2014;12(2):142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Magill MK, Ehrenberger D, Scammon DL, et al. The cost of sustaining a patient-centered medical home: experience from 2 states. Ann Fam Med. 2015;13(5):429–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Medicare & Medicaid Services. Summary of policies in the calendar year (CY) 2015 Medicare Physician Fee Schedule (MPFS) final rule and telehealth originating site facility fee payment amount. MM9034. MLN Matters. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM9034.pdf. Revised Jan 18, 2015.
- 43.Nocedal J, Wright SJ. Numerical Optimization. New York, NY: Springer Science+ Business Media; 2006. [Google Scholar]
- 44.Basu S, Andrews J. Complexity in mathematical models of public health policies: a guide for consumers of models. PLoS Med. 2013;10(10):e1001540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pope GC, Ellis RP, Ash AS, et al. Diagnostic cost group hierarchical condition category models for Medicare risk adjustment. Centers for Medicare and Medicaid Services. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/Downloads/Pope_2000_2.pdf. Published Dec 21, 2000 Accessed Oct 26, 2015.
- 46.Steele GD, Haynes JA, Davis DE, et al. How Geisinger’s advanced medical home model argues the case for rapid-cycle innovation. Health Aff (Millwood). 2010;29(11):2047–2053. [DOI] [PubMed] [Google Scholar]
- 47.Sessums LL, McHugh SJ, Rajkumar R. Medicare’s vision for advanced primary care: New directions for care delivery and payment. JAMA. 2016;315(24):2665–2666. [DOI] [PubMed] [Google Scholar]
- 48.Christensen EW, Dorrance KA, Ramchandani S, et al. Impact of a patient-centered medical home on access, quality, and cost. Mil Med. 2013;178(2):135–141. [DOI] [PubMed] [Google Scholar]
- 49.Coleman K, Reid RJ, Johnson E, et al. Implications of reassigning patients for the medical home: a case study. Ann Fam Med. 2010; 8(6):493–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Driscoll DL, Hiratsuka V, Johnston JM, et al. Process and outcomes of patient-centered medical care with Alaska Native people at Southcentral Foundation. Ann Fam Med. 2013;11(Suppl 1):S41–S49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fillmore H, DuBard CA, Ritter GA, Jackson CT. Health care savings with the patient-centered medical home: Community Care of North Carolina’s experience. Popul Health Manag. 2014;17(3):141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Flottemesch TJ, Anderson LH, Solberg LI, Fontaine P, Asche SE. Patient-centered medical home cost reductions limited to complex patients. Am J Manag Care. 2012;18(11):677–686. [PubMed] [Google Scholar]
- 53.Gilfillan RJ, Tomcavage J, Rosenthal MB, et al. Value and the medical home: effects of transformed primary care. Am J Manag Care. 2010;16(8):607–614. [PubMed] [Google Scholar]
- 54.Maeng DD, Graham J, Graf TR, et al. Reducing long-term cost by transforming primary care: evidence from Geisinger’s medical home model. Am J Manag Care. 2012;18(3):149–155. [PubMed] [Google Scholar]
- 55.Milstein A, Gilbertson E. American medical home runs. Health Aff (Millwood). 2009;28(5):1317–1326. [DOI] [PubMed] [Google Scholar]
- 56.Phillips RL, Jr, Bronnikov S, Petterson S, et al. Case study of a primary care-based accountable care system approach to medical home transformation. J Ambul Care Manage. 2011;34(1):67–77. [DOI] [PubMed] [Google Scholar]
- 57.Reid RJ, Johnson EA, Hsu C, et al. Spreading a medical home redesign: effects on emergency department use and hospital admissions. Ann Fam Med. 2013;11(Suppl 1):S19–S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roby DH, Pourat N, Pirritano MJ, et al. Impact of patient-centered medical home assignment on emergency room visits among uninsured patients in a county health system. Med Care Res Rev. 2010;67(4):412–430. [DOI] [PubMed] [Google Scholar]
- 59.Rosenberg CN, Peele P, Keyser D, McAnallen S, Holder D. Results from a patient-centered medical home pilot at UPMC Health Plan hold lessons for broader adoption of the model. Health Aff (Millwood). 2012;31(11):2423–2431. [DOI] [PubMed] [Google Scholar]
- 60.Steiner BD, Denham AC, Ashkin E, Newton WP, Wroth T, Dobson LA., Jr Community care of North Carolina: improving care through community health networks. Ann Fam Med. 2008;6(4):361–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Takach M. Reinventing Medicaid: state innovations to qualify and pay for patient-centered medical homes show promising results. Health Aff (Millwood). 2011;30(7):1325–1334. [DOI] [PubMed] [Google Scholar]
- 62.Mathematica Policy Research. Evaluation of the Comprehensive Primary Care Initiative: First Annual Report. Princeton, NJ: Mathematica Policy Research; 2015. [Google Scholar]
- 63.Jerant A, Bertakis KD, Fenton JJ, Franks P. Extended office hours and health care expenditures: a national study. Ann Fam Med. 2012;10(5):388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Day J, Scammon DL, Kim J, et al. Quality, satisfaction, and financial efficiency associated with elements of primary care practice transformation: preliminary findings. Ann Fam Med. 2013;11(Suppl 1):S50–S59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fishman PA, Johnson EA, Coleman K, et al. Impact on seniors of the patient-centered medical home: evidence from a pilot study. Gerontologist. 2012;52(5):703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gabbay RA, Bailit MH, Mauger DT, Wagner EH, Siminerio L. Multipayer patient-centered medical home implementation guided by the chronic care model. Jt Comm J Qual Patient Saf. 2011;37(6): 265–273. [DOI] [PubMed] [Google Scholar]
- 67.Lee K, Palacio C, Alexandraki I, Stewart E, Mooradian AD. Increasing access to health care providers through medical home model may abolish racial disparity in diabetes care: evidence from a cross-sectional study. J Natl Med Assoc. 2011;103(3):250–256. [DOI] [PubMed] [Google Scholar]
- 68.Meyer H. Group Health’s move to the medical home: for doctors, it’s often a hard journey. Health Aff (Millwood). 2010;29(5):844–851. [DOI] [PubMed] [Google Scholar]
- 69.Rankin KM, Cooper A, Sanabria K, Binns HJ, Onufer C. Illinois medical home project: pilot intervention and evaluation. Am J Med Qual. 2009;24(4):302–309. [DOI] [PubMed] [Google Scholar]
- 70.Reid RJ, Coleman K, Johnson EA, et al. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood). 2010;29(5):835–843. [DOI] [PubMed] [Google Scholar]
- 71.Solberg LI, Asche SE, Fontaine P, Flottemesch TJ, Anderson LH. Trends in quality during medical home transformation. Ann Fam Med. 2011;9(6):515–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Solimeo SL, Hein M, Paez M, Ono S, Lampman M, Stewart GL. Medical homes require more than an EMR and aligned incentives. Am J Manag Care. 2013;19(2):132–140. [PubMed] [Google Scholar]