Abstract
Salvia miltiorrhiza root (Danshen) is widely used in Asia for its cardiovascular benefits and contains both hydrophilic phenolic acids and lipophilic tanshinones, which are believed to be responsible for its therapeutic efficacy. This review summarized the effects of these bioactive components from S. miltiorrhiza roots on pharmacokinetics of comedicated drugs with mechanic insights regarding alterations of protein binding, enzyme activity, and transporter activity based on the published data stemming from both in vitro and in vivo human studies. In vitro studies indicated that cytochrome P450 (CYP450), carboxylesterase enzyme, catechol-O-methyltransferase, organic anion transporter 1 (OAT1) and OAT3, and P-glycoprotein were the major targets involved in S. miltiorrhiza-drug interactions. Lipophilic tanshinones had much more potent inhibitory effects towards CYPs activities compared to hydrophilic phenolic acids, evidenced by much lower Ki values of the former. Clinical S. miltiorrhiza-drug interaction studies were mainly conducted using CYP1A2 and CYP3A4 probe substrates. In addition, the effects of coexisting components on the pharmacokinetic behaviors of those noted bioactive compounds were also included herein.
1. Introduction
Cardiovascular disease, one of the top leading causes of mortality across the world, is responsible for 31% of deaths in 2012 [1]. Frequently prescribed medications include anticoagulants, calcium-channel blockers, β-blockers, diuretics, and platelet aggregation inhibitors. Moreover, cardiovascular disease is often accompanied by obesity and/or diabetes. Polypharmacology, which describes multitargets with multiple-medications exemplified by herbs, has suggestive superior efficacy and safety and is less liable to adverse effects compared to single-medication [2]. Herbal medicines usually have a variety of constituents exerting polypharmacological roles against multiple targets. As high as 80% of the population in Africa and Asia [3] and 4–61% cardiac patients [4] take traditional medicines for health benefits. Patients seek herbs for boosting pharmacologic effects, relieving unwanted adverse syndromes caused by western drugs, and reducing economic burden [5, 6]. Salvia miltiorrhiza root (Danshen) is widely used, alone or coprescribed with other herbs or conventional drugs, by patients with angina pectoris and myocardial infarction in Asia [7, 8]. A meta-analysis of sixty randomized clinical trials indicated that Danshen Dripping pill, consisting of S. miltiorrhiza, Panax notoginseng, and Dryobalanops camphora, showed much more apparent efficacy compared to isosorbide dinitrate [9].
The combination of cardiovascular drugs and S. miltiorrhiza roots highlights potential interactions caused by pharmacokinetic and pharmacodynamic mechanisms. Pharmacokinetic interaction often leads to increased or decreased victim drug systemic levels due to alternation of absorption, distribution, metabolism, and excretion by perpetrator drugs [10, 11]. Underlying mechanisms include but are not limit to protein binding and inhibition and induction of enzyme/transporter activities [12]. These interactions at the end may cause attenuated efficacy or unwanted toxicity, which suggests necessary dose adjustment.
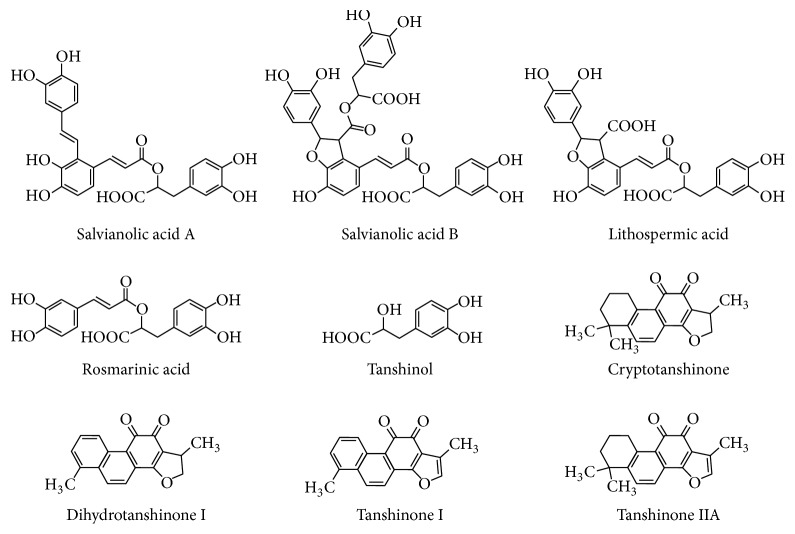
Around one hundred components are found in S. miltiorrhiza roots [13], which are classified into two groups: (1) hydrophilic phenolic acids with tanshinol, rosmarinic acid, lithospermic acid, and salvianolic acids A and B as the major ones; (2) lipophilic tanshinones with tanshinone I, tanshinone IIA, cryptotanshinone, and dihydrotanshinone I as the major ones (Figure 1). The contents of chemicals in S. miltiorrhiza roots vary among aqueous extracts, organic solvent extracts, oral pills, and injections derived from the single herb of S. miltiorrhiza roots or herbal combination, like Fufang prescription in China. These compounds can cause coronary vasodilatation, suppress thromboxane formation, inhibit platelet adhesion and aggregation, and scavenge free radicals [13]. Therefore, roles of S. miltiorrhiza either as a perpetrator or as a victim need to be explored in herb-drug interactions.
Figure 1.
Structures of major constituents from Danshen.
In this review, we mainly focus on pharmacokinetic interaction between S. miltiorrhiza roots and drugs both in human in vitro studies and in clinical trials. Animal in vivo studies are also included when clinical studies are not available. In addition, influence on pharmacokinetics of bioactive constituents from S. miltiorrhiza roots by other combined herbs or drugs is also explored herein.
2. Pharmacokinetic Interaction Caused by Salvia miltiorrhiza
2.1. Protein Binding
After administration, a drug circulates in bloodstream as both free form and protein-drug complex. Acidic and neutral drugs primarily bind to alkalotic albumin and basic drugs tend to bind to α1-acid glycoprotein and lipoproteins [14, 15]. Based on “free drug hypothesis,” free drug concentrations are deemed critical for efficacy/safety since only free drugs can penetrate membrane barriers and have the best correlation with drug response [16]. Pharmacological effect of drugs can be changed when unbound concentration changes while total concentration remains the same [17, 18]. Displacement may occur and lead to elevated unbound fractions in the presence of another drug.
Human serum albumin is the most abundant protein in circulation and bovine serum albumin has a similar structural homology. These two albumins are commonly used for evaluating drugs binding affinities in vitro. Drugs binding constants, the higher values of which indicate more tight binding, determine their unbound concentrations in blood. Salvianolic acid B and rosmarinic acid can bind to bovine serum albumin at site I with binding constants around 105 L/mol [19]. Salvianolic acid B, lithospermic acid, rosmarinic acid, salvianolic acid A, and salvianolic acid C can bind to human serum albumin at sites I and/or II with increasing binding constants at 298 K ranging from 0.18 to 16 × 105 L/mol [20–22]. The binding constant for tanshinone IIA at 303 K was 1.54 × 105 L/mol [23]. The plasma protein binding of salvianolic acid A, salvianolic acid B, and tanshinone IIA was 99.7% [24], 83.8–92.1% [25, 26], and 99.2% [27] while that of tanshinol was 2% [7]. Warfarin, an anticoagulant preventing formation of blood clots, is highly bound (97–99%) with human serum albumin in plasma with selectivity to site I. In the presence of the above-mentioned individual constituent, the human serum albumin binding constant of warfarin decreased by 1.4- to 8.7-fold [20] which may cause increased free warfarin concentrations. Sodium tanshinone IIA sulfonate, a water-soluble derivative of tanshinone IIA used as an injection in China, displaced warfarin from the warfarin-human serum albumin complex, the signal of which can be directly measured by mass spectrum [28]. Therefore, increased levels of free plasma warfarin could be observed when warfarin is combined with Danshen because of replacement of warfarin by its constituents, which may potentiate anticoagulant response of warfarin.
Using an ex vivo study, the effect of coadministration of Danshen-Gegen (Radix Puerariae lobatae) formula on warfarin protein binding was investigated. The rats were orally given the formula at a single dose of 0.15 g/kg or at 0.15 g/kg twice daily for five days. Blood was collected 30 min and 2 h after the single dosing and the last multiple dosing, respectively. By adding warfarin to the freshly obtained plasma, a 12–22% increase of unbound warfarin concentrations was observed. Due to the highly bound fraction of warfarin in rat plasma (92%), the authors recommended that this change of unbound warfarin levels cannot be overlooked and concomitant use of Danshen-Gegen and warfarin for treating cardiovascular disease should be avoided [29].
In addition to warfarin, there are other drugs that can be affected by displacement of protein binding by constituents from Danshen. Ethyl acetate extract of Danshen, 50–70% of which bound to albumin, can displace salicylate in serum resulting in as high as 1.6-fold increase in free salicylate concentration [30]. Lipophilic constituents were responsible for the effect since they were more easily extracted by ethyl acetate than hydrophilic phenolic acids occurring in Danshen.
2.2. Metabolic Enzyme Activity
Most drugs undergo metabolism by enzymes in different tissues after they enter the body and produce metabolites with or without pharmacological activities. Regulation of enzyme activities can alter the systemic exposure and eventually the efficacy of a drug. Cytochromes P450 (CYP450) enzyme-mediated drug interaction is one of the most popular research topics due to well-known specific inhibitors and probe substrates for CYP isozymes.
Using human liver microsomes (HLMs) and recombinant CYP isozymes, different inhibitory potency against various CYPs have been observed for Danshen extract and its individual constituents [7, 31–39] (Table 1). Water-soluble constituents from Danshen tend to exert little or weak inhibitory effect on CYPs activities except for tanshinol and salvianolic acid B. Tanshinol inhibited CYP1A2, CYP2C8, CYP2C9, and CYP2C19 activities with IC50 of 110, 34, 99, and 67 μM, respectively [7, 37]. Salvianolic acid B inhibited CYP1A2 with IC50 of 105 μM and protocatechuic aldehyde suppressed CYP3A4 activity with IC50 of 130–160 μM [37]. An IC50 value of 51 μg/mL against CYP3A4 was found when testing the inhibitory roles of a Danshen extract, in which the content of tanshinones was approximately two orders of magnitude less than that of water soluble phenolic acids [35]. Salvianolate, a highly purified aqueous extract from Danshen, consists of salvianolic acid B (≥85%), rosmarinic acid (≥10.1%), and lithospermic acid (≥1.9%). Salvianolate can inhibit CYP3A4 using HLMs with Ki value of 2.27 μg/mL and using recombinant CYP3A4 with IC50 value of 3.58 μg/mL, whereas the other CYPs were hardly affected by this extract indicated by the IC50 values higher than 100 μg/mL [32]. Using HepG2 cells, salvianolic acid B at 1 and 10 μM downregulated CYP3A4 mRNA expression with or without induction by rifampicin. Meantime, decrease of CYP1A2 mRNA expression was also observed at the same concentration of salvianolic acid B [40]. However, CYP3A4 and CYP1A2 protein levels and activities were not evaluated.
Table 1.
Inhibitory effects of Danshen extract and its bioactive constituents towards enzyme and transporter activities.
| Extract/constituent | Enzyme/transporter | Substrate | K i (μM) | Reference | ||
|---|---|---|---|---|---|---|
| HLMs | Purified | Inhibition type | ||||
| Tanshinone I | CYP1A1 | 7-Ethoxyresorufin | 0.75∗ | [39] | ||
| CYP1A2 | 7-Ethoxyresorufin | 0.19∗ | [39] | |||
| CYP1A2 | Phenacetin | 0.48–2.16 | 0.11 | com | [36, 37] | |
| CYP2C9 | Tolbutamide | 51.2 | 73.4 | com | [36] | |
| Diclofenac | >200∗ | [37] | ||||
| CYP2D6 | Dextromethorphan | 120∗ | [37] | |||
| CYP2E1 | Chlorzoxazone | 3.67 | ND | non | [36] | |
| CYP3A4 | Testosterone | 86.9 | 92.5 | com | [36] | |
| Testosterone | >200∗ | [37] | ||||
| Midazolam | >200∗ | [37] | ||||
| CE1 | o-Nitrophenyl acetate | 26.3 | [44] | |||
| CE2 | o-Nitrophenyl acetate | 14.6 | [44] | |||
| Irinotecan | 1.4 | [44] | ||||
| P-gp | Digoxin | 0.53∗ (Caco-2 cells) | [60] | |||
|
| ||||||
| Tanshinone IIA | CYP1A | 7-Ethoxyresorufin | 0.2∗ | [39] | ||
| CYP1A | 7-Methoxyresorufin | 0.38∗ | [39] | |||
| CYP1A1 | 7-Ethoxyresorufin | 4.3∗ | [39] | |||
| CYP1A2 | 7-Ethoxyresorufin | 0.09∗ | [39] | |||
| CYP1A2 | Phenacetin | 1.0–1.45 | 0.05 | com | [36, 37] | |
| CYP2C9 | Diclofenac | >200∗ | [37] | |||
| CYP2C9 | Tolbutamide | 61.6 | 88.6 | com | [36] | |
| CYP2D6 | Dextromethorphan | >200∗ | [37] | |||
| CYP2E1 | Chlorzoxazone | — | — | [36] | ||
| CYP3A4 | Midazolam | >200∗ | [37] | |||
| Testosterone | >200∗ | [37] | ||||
| Testosterone | 219 | 141 | com | [36] | ||
| CE1 | o-Nitrophenyl acetate | 6.9 | [44] | |||
| CE2 | o-Nitrophenyl acetate | 2.5 | [44] | |||
| Irinotecan | 0.07 | [44] | ||||
|
| ||||||
| Cryptotanshinone | CYP1A1 | 7-Ethoxyresorufin | 2.2∗ | [39] | ||
| CYP1A2 | 7-Ethoxyresorufin | 0.56∗ | [39] | |||
| CYP1A2 | Phenacetin | 0.68∗ | com | [38] | ||
| Phenacetin | 0.45–1.88 | 0.27 | com | [36, 37] | ||
| CYP2C9 | Diclofenac | 8 | mixed | [37] | ||
| Tolbutamide | 22.9 | 9.90 | com | [36] | ||
| CYP2D6 | Dextromethorphan | 68 | mixed | [37] | ||
| CYP2E1 | Chlorzoxazone | 10.87 | ND | com | [36] | |
| CYP3A4 | Midazolam | >200∗ | [37] | |||
| Testosterone | >200∗ | [37] | ||||
| Testosterone | 120 | 59.9 | com | [36] | ||
| CE1 | o-Nitrophenyl acetate | 0.54 | [44] | |||
| CE2 | o-Nitrophenyl acetate | 0.14 | [44] | |||
| Irinotecan | 0.29 | [44] | ||||
|
| ||||||
| Dihydrotanshinone I | CYP1A2 | Phenacetin | 0.53 | 0.02 | com | [36] |
| CYP2C9 | Tolbutamide | 1.92 | 3.14 | com | [36] | |
| CYP2E1 | Chlorzoxazone | — | ND | un | [36] | |
| CYP3A4 | Testosterone | 2.11 | 2.98 | non | [36] | |
| Midazolam | 1.2∗ | [33] | ||||
| CE1 | o-Nitrophenyl acetate | 0.40 | [44] | |||
| CE2 | o-Nitrophenyl acetate | 0.12 | [44] | |||
| CE2 | Irinotecan | 1.83 | [44] | |||
|
| ||||||
| Miltirone | CE1 | o-Nitrophenyl acetate | 2.53 | [44] | ||
| CE2 | o-Nitrophenyl acetate | 0.04 | [44] | |||
| CE2 | Irinotecan | 0.08 | [44] | |||
|
| ||||||
| Tanshinone IIA sulfonate | CYP2A6 | Coumarin | >100∗ | [31] | ||
| CYP2C9 | Tolbutamide | >100∗ | ||||
| CYP2C19 | s-mephenytoin | >100∗ | ||||
| CYP2D6, | Metoprolol | >100∗ | ||||
| CYP2E1 | Chlorzoxazone | >100∗ | ||||
| CYP3A4 | Midazolam | 3.2 | com | |||
| CE1 | o-Nitrophenyl acetate | >100 | [44] | |||
| CE2 | o-Nitrophenyl acetate | 3.9 | ||||
| CE2 | Irinotecan | 28.8 | ||||
|
| ||||||
| Tanshinol | CYP1A2 | Phenacetin | 110∗ | [37] | ||
| CYP2C9 | Diclofenac | 35 | com | |||
| CYP2D6 | Dextromethorphan | >200∗ | ||||
| CYP3A4 | Midazolam | >200∗ | ||||
| Testosterone | >200∗ | |||||
| OAT1 | p-Aminohippuric acid | 40.4 | [54] | |||
| 98∗ | [56] | |||||
| OAT2 | Prostaglandin F2α | 1528∗ | [56] | |||
| OAT3 | Estrone sulfate | 8.6 | [54] | |||
| 2803∗ | [56] | |||||
| OAT4 | Estrone sulfate | 4079∗ | [56] | |||
|
| ||||||
| Protocatechuic aldehyde | CYP1A2 | Phenacetin | >200∗ | [37] | ||
| CYP2C9 | Diclofenac | >200∗ | ||||
| CYP2D6 | Dextromethorphan | >200∗ | ||||
| CYP3A4 | Midazolam | 130∗ | ||||
| Testosterone | 160∗ | |||||
|
| ||||||
| Protocatechuic acid | CYP1A2 | Phenacetin | >200∗ | [37] | ||
| CYP2C9 | Diclofenac | >200∗ | ||||
| CYP2D6 | Dextromethorphan | >200∗ | ||||
| CYP3A4 | Midazolam | >200∗ | ||||
| Testosterone | >200∗ | |||||
|
| ||||||
| Salvianolic acid B | CYP1A2 | Phenacetin | 105∗ | [37] | ||
| CYP2C9 | Diclofenac | >200∗ | ||||
| CYP2D6 | Dextromethorphan | >200∗ | ||||
| CYP3A4 | Midazolam | >200∗ | ||||
| Testosterone | >200∗ | |||||
| OAT1 | p-Aminohippuric acid | 22.2 | [54] | |||
| OAT3 | Estrone sulfate | 19.8 | ||||
|
| ||||||
| Salvianolic acid A | OAT1 | p-Aminohippuric acid | 5.6 | [54] | ||
| OAT3 | Estrone sulfate | 0.16 | ||||
|
| ||||||
| Lithospermic acid | OAT1 | p-Aminohippuric acid | 20.8 | [54] | ||
| OAT3 | Estrone sulfate | 0.59 | ||||
|
| ||||||
| Rosmarinic acid | OAT1 | p-Aminohippuric acid | 0.35 | [54] | ||
| OAT3 | Estrone sulfate | 0.55 | ||||
|
| ||||||
| Danshen extracta | CYP1A2 | Phenacetin | 190# | [64] | ||
|
| ||||||
| Danshen extractb | CYP3A4 | Testosterone | 51# | com | [35] | |
|
| ||||||
| Danshen ethanol extractc | CYP1A2 | Phenacetin | 3.4# | com | [34] | |
| CYP3A4 | Testosterone | 11.9# | com | |||
|
| ||||||
| Danshen ethanol extractd | CYP3A4 | Midazolam | 8.6# | [33] | ||
|
| ||||||
| Salvianolatee | CYP1A2, | Phenacetin | >100∗# | [32] | ||
| CYP2A6 | Coumarin | >100∗# | ||||
| CYP2C9 | Tolbutamide | >100∗# | ||||
| CYP2C19 | s-mephenytoin | >100∗# | ||||
| CYP2D6, | Metoprolol | >100∗# | ||||
| CYP2E1 | Chlorzoxazone | >100∗# | ||||
| CYP3A4 | Midazolam | 2.27# | 3.58# | non | ||
com, competitive; non, noncompetitive; un, uncompetitive.
∗, IC50 (μM).
#, μg/mL.
aContaining tanshinol 3.1, salvianolic acid B 37.3, rosmarinic acid 1.8 and protocatechuic aldehyde 0.16 mg/g, and dihydrotanshinone I 12.7, cryptotanshinone 34.6, tanshinone I 10.4, and tanshinone IIA 22.6 μg/g.
bContaining tanshinol 31, salvianolic acid B 41, rosmarinic acid 6.1, and protocatechuic aldehyde 2.8 mg/g, dihydrotanshinone I 98, cryptotanshinone 70, tanshinone I 32, and tanshinone IIA 21 μg/g.
cContaining tanshinol 2.68, salvianolic acid B 209, rosmarinic acid 14.9, and protocatechuic aldehyde 0.64, dihydrotanshinone I 9.3, cryptotanshinone 36.8, tanshinone I 17.9, and tanshinone IIA 118 mg/g.
dContaining tanshinone IIA 106.2, cryptotanshinone 88.0, tanshinone I 53.1, and dihydrotanshinone I 13.5 mg/g.
eContaining salvianolic acid B (≥85%), rosmarinic acid (≥10.1%), and lithospermic acid (≥1.9%).
Compared to hydrophilic constituents, lipophilic tanshinones tend to have much more potent inhibitory effects towards CYPs activities. Tanshinone I, tanshinone IIA, cryptotanshinone, and dihydrotanshinone I inhibited CYP1A2 with IC50 values ranging from 0.02 to 3.0 μM using either HLMs or recombinant CYP1A2 [36, 39, 41]. Similarly, tanshinone I, cryptotanshinone, and dihydrotanshinone I inhibit CYP2E1 with IC50 values ranging from 0.7 to 10 μM. Cryptotanshinone and dihydrotanshinone I inhibit CYP2C9 with IC50 values ranging from 7.5 to 33 μM. Tanshinone I, tanshinone IIA, and cryptotanshinone were weak inhibitors (IC50 > 75 μM) towards CYP2D6 and CYP3A4 [41]. However, dihydrotanshinone I exerted a potent inhibitory role against CYP3A4 with IC50 at 1.2–3.2 μM [33, 36]. Because of more potent inhibitory effect of tanshinones than phenolic acids, ethanol extract which usually contained mainly tanshinones exerted much lower IC50 and Ki values compared to aqueous extract. It was reported that ethanol extract could inhibit CYP1A2 and CYP3A4 in HLMs with IC50 or Ki values of 3.4 and 8.6–12 μg/mL, respectively [32, 33]. Sodium tanshinone IIA inhibited CYP3A4 with Ki value of 3.2 μM in HLMs, whereas it had little inhibitory effect on CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, and CYP2E1, supported by much higher IC50 values (>100 μM) [31].
Besides inhibition, Danshen ethanol extract, tanshinone IIA, and cryptotanshinone could induce CYP3A4 via activating human pregnane X receptor and, to a less extent, constitutive androstane receptor and glucocorticoid receptor in HepG2 cells [42]. Tanshinone I, tanshinone IIA, cryptotanshinone, and dihydrotanshinone I were reported to induce CYP1A1/2 via aryl hydrocarbon receptor in the human HepG2 cells and lead to 2- to 14-fold increase of CYP1A1/2 activity with concentration of individual component at 5 μM [43].
In addition, UDP-glucuronosyltransferases (UGTs) as well as CYP3A4 are targets of pregnane X receptor. Therefore, it is possible that Danshen could induce UGTs expression levels [33]. Meanwhile, salvianolic acid B at 1 and 10 μM increased glutathione S-transferase protein levels in HepG2 cells [40]. Using o-nitrophenyl acetate and irinotecan as substrates of human carboxylesterase (CE) enzyme 2, miltirone and cryptotanshinone had the most potent inhibition demonstrated with Ki values of 0.04 and 0.08 μM, 0.14 and 0.29 μM, respectively. Tanshinone IIA and tanshinone I only exhibited potent inhibitory effect towards irinotecan metabolism with Ki value of 0.07 and 0.14 μM, respectively, and dihydrotanshinone I only inhibited o-nitrophenyl acetate metabolism with Ki value of 0.12 μM. Unlike CE2, the inhibitory effects of tanshinones against CE1 were modest with cryptotanshinone and dihydrotanshinone as exceptions, evidenced by Ki values of 0.54 and 0.40 μM, respectively [44]. Compared to CYP enzymes, more studies are necessary for investigating the effect of Danshen on non-CYP enzymes.
Collectively, hydrophilic phenolic acids and lipophilic tanshinones have exerted different inhibitory potency for various CYPs, the latter of which are more likely to cause Danshen-drug interactions. Among hydrophilic constituents from Danshen, tanshinol had the highest bioavailability (40% in dogs and 30% in rats) while other phenolic acids were slightly or not detected in human and dogs after oral administration [7, 45]. The oral bioavailability of salvianolic acid B and lithospermic acid in rats was only 0.02% [46] and 1.15% [47]. After oral administration of cardiotonic pills containing 4.8 mg of tanshinol, the maximum plasma concentration (Cmax) of tanshinol was only 20–30 ng/mL [45]. Meanwhile, tanshinones tend to have Cmax in the nanomolar to lower micromolar range [48] due to their low contents in commonly used aqueous Danshen extract and poor bioavailability. For example, the oral bioavailability of cryptotanshinone was 2.1% in rats [49]. Therefore, there is minor possibility that traditional oral medication of aqueous Danshen extract-derived products can cause CYP-mediated Danshen-drug interaction. However, it is probable for Danshen-derived injections or other formulations with high content tanshinones to lead to Danshen-drug interactions. Furthermore, all the reported data on enzyme inhibition and induction by Danshen were based on liver. High exposure of intestinal enzymes to herbal constituents in the intestine is also a critical factor contributing to herb-drug interactions [50]. Therefore, further investigations concerning gut enzyme modulation by Danshen are necessary in the future.
2.3. Transporter Activity
Uptake and efflux transporters, as well as enzymes, are critical determinants of drug systemic exposures and efficacies. Modulation of transporters functions can lead to altered drug pharmacological effects [51–53]. Lithospermic acid, rosmarinic acid, salvianolic acid A, salvianolic acid B, and protocatechuic acid were reported to have inhibitory effects towards human organic anion transporter 1 (OAT1) and OAT3 with Ki values of 20.8 and 0.59, 0.35 and 0.55, 5.6 and 0.16, 22.2 and 19.8, and 13.4 and 81.8 μM, respectively [54, 55]. Tanshinol exhibited weak inhibitory potency towards human OAT1, OAT2, OAT3, and OAT4 with IC50 values of 98, 1528, 2803, and 4079 μM, respectively, using transfected HEK293 cells. However, tanshinol at 1 mM did not inhibit human organic anion transporting polypeptide 4C1 (OATP 4C1), organic cation transporter 2 (OCT2), organic cation/carnitine transporter 1 (OCTN1), multidrug and toxin extrusion protein 1 (MATE1), and MATE2-K in transfected HEK293 cells or P-glycoprotein (P-gp), multidrug resistance-associated protein 2 (MRP2), MRP4, and breast cancer resistance protein (BCRP) in inside-out membrane vesicles that expressed specific transporter [7, 56]. In addition, treatment with salvianolic acid A at 3, 6, and 12 μM for 48 h in MCF-7/PTX cells significantly downregulated both gene and protein expression of P-gp, MRP1, and BCRP [57]. After intravenous administration of a Danshen injection to healthy subjects, the unbound Cmax for rosmarinic acid, salvianolic acid B, and tanshinol were 0.53, 0.39, and 18 μM, respectively [54, 58]. Considering unbound plasma concentration/Ki (or IC50) ratios caused by potent inhibitory effect of rosmarinic acid and high plasma concentration of tanshinol after administration of Danshen injections, OAT1 and OAT3 mediated Danshen-drug interactions possibly take place during the clinical practice.
Cryptotanshinone and dihydrotanshinone I inhibited P-gp indicated by decreased efflux ratio of digoxin (a cardiac glycoside) transport across Caco-2 monolayer in the presence of these two components compared to baseline. The inhibitory effect was due to downregulated P-gp mRNA and protein expression. P-gp protein levels in P-gp overexpressing SW620 Ad300 cells decreased by 40% after incubation with 12.5 μM of individual cryptotanshinone and dihydrotanshinone I for 24 h. Miltirone failed to inhibit the P-gp mediated transport of digoxin in Caco-2 cells [59]. Reports on effects of tanshinone I and tanshinone IIA towards P-gp function were controversial. Hu et al. found little inhibitory effect [59], whereas Li et al. [60] and Yu et al. [61] reported significant inhibitory effects of tanshinone I (IC50 = 0.53 μM) and tanshinone IIA (IC50 = 2.6 μM) on P-gp activity, respectively.
Since Danshen ethanol extract, tanshinone IIA, and cryptotanshinone could activate human pregnane X receptor [42], via which P-gp can be induced, it is hypothesized that Danshen lipophilic constituents might induce P-gp. Indeed, treatment of tanshinone IIA and cryptotanshinone at 10 μM for 72 h exerted comparable inductive effects on P-gp mRNA with rifampin at 25 μM using primary human hepatocytes [62]. Upregulation of mRNA levels of BCRP, human peptide transporter 1 (hPepT1), monocarboxylate transporter (MCT), and MRP1-6 in Caco-2 cells were also found after treatment by tanshinone IIA at 0.01 or 1 μM for 24 h [63]. The low bioavailability of tanshinones restrained them from entering the liver at high concentrations. Therefore, it is probable that tanshinones might cause P-gp mediated interactions with a much greater extent in the gut than in the liver after oral administration of Danshen products.
2.4. Clinical Studies
Clinical studies on pharmacokinetic Danshen-drug interactions are listed in Table 2. Two-week treatment with Danshen extract tablets had no effect on the pharmacokinetics of theophylline that metabolized predominantly by CYP1A2 and, to a less extent, CYP2E1 [65], which was due to low bioavailability of tanshinones and weak inhibitory potency of hydrophilic constituents [37]. Following this study, Qiu et al. reported [67] that two-week treatment of the same Danshen extract tablets caused 31% and 27% decrease of midazolam Cmax and AUC0–∞, respectively, in volunteers. It has been confirmed that tanshinones had inductive effects on CYP1A, CYP2C, and CYP3A in mice while aqueous extract of Danshen did not [69]. Therefore, the decreased midazolam levels may be due to both hepatic and intestinal CYP3A4 induction by lipophilic constituents [33, 42]. Ten-day treatment of Danshen ethanol extract, which contained 26- to 85-fold higher tanshinones compared to the above mentioned Danshen extract tablets, decreased the midazolam AUC0–12 h and Cmax values by 80% and 66%, respectively, accompanied by a 3.0-fold increase of the AUC ratio of 1-hydroxymidazolam/midazolam [33]. Inductive effect of Danshen towards CYP3A4 was dependent on tanshinones dose although not proportionally, which was indicated by the extent of pharmacokinetic change of midazolam. As discussed earlier, tanshinones could induce P-gp in vitro. Importantly, consistent findings were observed in humans. Using the p-gp substrate fexofenadine as a probe, ethanol extract of Danshen for ten days can significantly decrease fexofenadine AUC0–24 h and Cmax by 45% and 35%, respectively [62].
Table 2.
Clinical trials on pharmacokinetic Danshen-drug interactions.
| Dose regimen | Effect and ratio (treatment/control) | Reference | |||
|---|---|---|---|---|---|
| Danshen | Daily dose (mg/day) | Victim drug | |||
| Four Danshen extract tablets (each tablet contained an extract of 1 g Danshen), p.o., three times daily for 14 days (days 2–15) | Cryptotanshinone, tanshinone, tanshinone IIA, tanshinol, protocatechuic acid, salvianolic acid B |
3.0 6.0 4.2 19.2 2.4 156 |
A single oral dose of theophylline at 100 mg on days 1 and 15. | No effect | [65] |
| Sodium tanshinone IIA sulfonate injections, i.v., 60 mg/day for 13 days | Baseline and a single oral dose of caffeine at 100 mg on day 13 after injection of placebo or sodium tanshinone IIA sulfonate. | CYP1A2 activity (ratio of paraxanthine to caffeine at 6 h in plasma) ratio 1.41; caffeine AUC ratio 0.87, paraxanthine AUC ratio 1.17 |
[66] | ||
| Four Danshen extract tablets (each tablet contained an extract of 1 g Danshen), p.o., three times daily for 14 days (days 2–15) | Cryptotanshinone tanshinone I, tanshinone IIA, protocatechuic aldehyde, tanshinol, salvianolic acid B |
3.12 6.0 4.44 8.04 20.4 162 |
A single oral dose of midazolam at 15 mg on days 1 and 16. | Midazolam AUC ratio 0.74, Cmax ratio 0.69, CL/F ratio 1.35. No effect on Cmax and AUC ratios of midazolam to 1-hydroxymidazolam |
[67] |
| Ethanol extract of Danshen at 1 g, p.o., a single dose | Tanshinone IIA, cryptotanshinone, tanshinone I, dihydrotanshinone I |
106.2 88.0 53.1 13.5 |
Baseline and a single oral dose of midazolam at 15 mg 0.5 h after administration of 1 g Danshen extract. | Midazolam Cmax ratio 1.87; 1-hydroxymidazolam Cmax ratio 1.68 |
[33] |
| Ethanol extract of Danshen at 1 g, p.o., three times a day for 10 days (days 2–11) | Tanshinone IIA, cryptotanshinone, tanshinone I, dihydrotanshinone I |
318.6 264.0 159.3 40.5 |
A single oral dose of midazolam at 15 mg of on days 1 and 12 (0.5 h after administration of 1 g Danshen extract). | Midazolam AUC0–12 h ratio 0.20, Cmax ratio 0.34, and t1/2 ratio 0.56, CL/F ratio 6.0; 1-hydroxymidazolam AUC0–12 h ratio 0.55; AUC1-hydroxymidazolam/AUCmidazolam ratio 3.0 |
|
| T89 (225 mg, twice daily, p.o.) and warfarin were given simultaneously for one-week after reaching warfarin steady state | Warfarin dose to maintain international normalized ratio at 1.3–1.9 was selected. | T89 has no effect on the steady‐state PK of warfarin | [68] | ||
| Ethanol extract of Danshen at 1 g, p.o., three times a day for 10 days (days 2–11) | Tanshinone IIA, cryptotanshinone, tanshinone I |
318.6 264.0 159.3 |
A single oral dose of fexofenadine at 60 mg on days 1 and 12. |
C
max ratio 0.65, AUC0–24 h ratio 0.55, CL/F ratio 2.11. Induction of intestinal P-glycoprotein |
[62] |
p.o., oral.
i.v., intravenous.
Injection of sodium tanshinone IIA sulfonate at 60 mg/day for 13 days increased CYP1A2 activity (ratio of paraxanthine to caffeine at 6 h in plasma) by 41% and decreased caffeine AUC by 13%, suggesting induction of CYP1A2 activity [66]. Cmax of sodium tanshinone IIA sulfonate in human was around 2 μM after one-hour intravenous infusion at the dose of 40 mg [70]. Considering Ki value of 3.2 μM towards hepatic CYP3A4 inhibition [31], interactions of tanshinone IIA sulfonate and CYP3A4 substrate drug would take place if they are administered simultaneously.
Danshen is often in combined use with other herbs in China. T89 consists of Danshen, Sanqi (Radix Notoginseng), and Borneol. The main components from Danshen in T89 are hydrophilic phenolic acids. After warfarin, which was metabolized primarily by CYP2C9, CYP1A2, and CYP2C19 [71], reached steady-state in healthy volunteers, T89 was added in combination with warfarin for another week. T89 had no significant effect on total concentration and pharmacodynamic effect of warfarin [68]. This nonsignificant change in warfarin pharmacokinetics is consistent with the in vitro finding that hydrophilic phenolic acids exhibited high IC50 values against CYP450 activities (Table 1), which cannot be reached after regular dose of Danshen. However, Danshen was reported to cause potentiation of anticoagulation of warfarin in patients in three case reports [72–74] and a clinical study [75]. The difference of effect of Danshen on warfarin pharmacodynamic effect among these studies may be due to differences of dosage of Danshen and heath conditions. Since no warfarin levels were detected in the above-mentioned patients, the existence of pharmacokinetic interaction between Danshen and warfarin was unclear and the underlying mechanisms still need to be explored.
Collectively, clinical studies mainly focused on influence of Danshen on substrate drugs of CYP450 or P-gp due to extensively published data regarding potent modulatory effects of its ingredients. After oral administration of Danshen products enriched in tanshinones, CYP1A2, CYP3A4, and P-gp mediated Danshen-drug interactions were observed. Clinical interactions of Danshen and cardiovascular drugs focused on Danshen-warfarin interactions with unclear mechanisms.
3. Pharmacokinetic Alterations of Danshen Bioactive Constituents due to Coexisting Components
Danshen is prescribed for cardiovascular protection either alone or in combination with other herbs such as Fufang Danshen in China. Since Danshen itself is a cardiovascular protective herb, the pharmacokinetics of its bioactive constituents, which can be affected by coexisting components from Danshen extract, other herbs, and drugs, is important for evaluating the efficacy and toxicity. Recently, studies in this field are mainly conducted using animal models.
When Danshen injection was coadministered to rats with pure tanshinol, protocatechuic aldehyde, salvianolic acid A, or salvianolic acid B at 10-fold of their corresponding levels in Danshen injection, a 27–83% increase in the AUC of tanshinol, salvianolic acid A, and salvianolic acid B was observed compared to control group due to pharmacokinetic interactions [76]. Intravenous injection of tanshinones and polyphenolic extracts caused 2- to 14-fold change in the AUC of tanshinone IIA and salvianolic acid B compared to dosing either tanshinones or polyphenolic extract alone [77]. Metabolism-based interactions could be the underlying mechanism. Tanshinones are a class of compounds that has low bioavailability due to poor absorption and P-gp mediated intestinal efflux [49, 60, 61]. Similarly to intravenous injection, oral administration of tanshinones extract could result in 4- to 18-fold increase in the systemic exposure of cryptotanshinone and tanshinone II A compared to that of oral administration of pure cryptotanshinone or tanshinone II A [78]. This might be partly due to the inhibition of p-gp mediated efflux during absorption. It was reported that coexisting components from Danshen enhanced intestinal absorption of cryptotanshinone by 30–40% via inhibiting efflux transport of cryptotanshinone by P-gp using a rat gut sac model [79].
The coadministration of Danshen and Sanqi significantly improved intestinal absorption (2-fold) of the bioactive component salvianolic acid B in rats compared to administration of Danshen alone, suggesting synergistic effect of these two herbs [80]. However, another rat study reported oral administration of Fufang Danshen preparation or salvianolic acid B extract alone or in the presence of Sanqi, Borneol, and tanshinones extract had the same salvianolic acid B pharmacokinetics. Similar results were found for tanshinone IIA [81]. Using Guinea pigs as the animal model, the values of Cmax and AUC of salvianolic acid B in plasma decreased by 35% and 37%, respectively, and the corresponding values of tanshinone IIA decreased by 91% and 84%, respectively, after intratympanic administration of Danshen and Sanqi. Interestingly, 5.7- and 7.7-fold increase in AUC of salvianolic acid B and tanshinone IIA were found in cerebrospinal fluid [82]. This effect might be due to a different dosing route applied in guinea pigs.
To improve the absorption of tanshinol and salvianolic acid B, sodium caprate was dosed with Danshen tablet. Cmax and AUC values of tanshinol increased by 1.8-fold and the AUC value of salvianolic acid B increased by 1.4-fold due to improved intestinal permeability with addition of sodium caprate [83]. In addition, a single dose of rifampin caused 2.6- to 7.0-fold and 1.9- to 2.7-fold increase in salvianolic acid B AUC and Cmax values compared to baseline [84], respectively, the reason of which is partly due to inhibition of OATP-mediated elimination. Tanshinol was metabolized by methylation and, to a less extent, by sulfation into inactive metabolites. The metabolites and parent tanshinol were then subjected to OATs-mediated renal elimination both in human and in rat model [85]. Impairment of tanshinol methylation by entacapone, a potent catechol-O-methyltransferase inhibitor, caused 35% and 43% increase of tanshinol AUC with oral and intravenous administration of tanshinol to rats, respectively [7]. Blockage of tanshinol renal excretion by probenecid, an inhibitor of multiple OATs, led to 3.3-fold increase of tanshinol AUC in rats after intravenous administration of tanshinol [56]. Since tanshinol had a wide therapeutic effect window, the presence of catechol-O-methyltransferase and OATs inhibitors, from either herbs or comedicated drugs, might improve Danshen efficacy in cardiovascular treatment without causing unwanted adverse effects.
4. Conclusions
This review summarized pharmacokinetic Danshen-drug interactions in vitro and in vivo. In vitro studies indicated that lipophilic tanshinones tend to have more potent modulatory effects on enzyme and transporter activities than hydrophilic phenolic acids. Whether phenolic acids or tanshinones would cause significant in vivo pharmacokinetic Danshen-drug interactions depends not only on their intrinsic potency but also on their dosages. Different extraction methods and administration routs for Danshen products make the dosages of major bioactive components vary largely and cause difficulties in comparing those published research data among different labs. Information on dosages and pharmacokinetics of the major bioactive components from Danshen would help understand in vivo herb-interaction results. Therefore, it is highly recommended that researchers provide extraction details, contents of constituents in dosing formulations, and pharmacokinetics of major herbal components in the future research. Additionally, effects of coexisting components on pharmacokinetics of bioactive ingredients from Danshen were investigated mainly using animal models nowadays and further clinical studies are necessary for better disclosing underlying mechanisms of the therapeutic effect of this herb.
Acknowledgments
This work was supported by Specialized Research Fund for the Doctoral Program of Hainan Medical College and the National Natural Science Foundation of China (Grants nos. 81573828 and 81460629).
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
All authors contributed equally to this work.
References
- 1.World Health Organization. Cardiovascular Diseases (CVDs) 2014. http://www.who.int/mediacentre/factsheets/fs317/en/ [Google Scholar]
- 2.Peters J.-U. Polypharmacology—foe or friend? Journal of Medicinal Chemistry. 2013;56(22):8955–8971. doi: 10.1021/jm400856t. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Traditional Medicine. 2008. http://www.siav-itvas.org/images/stories/doc/agopuntura_scientifica/WHO_Traditional_medicine_2008.pdf. [Google Scholar]
- 4.Grant S. J., Bin Y. S., Kiat H., Chang D. H.-T. The use of complementary and alternative medicine by people with cardiovascular disease: a systematic review. BMC Public Health. 2012;12, article 299 doi: 10.1186/1471-2458-12-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brantley S. J., Argikar A. A., Lin Y. S., Nagar S., Paine M. F. Herb-drug interactions: challenges and opportunities for improved predictions. Drug Metabolism and Disposition. 2014;42(3):301–317. doi: 10.1124/dmd.113.055236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu W. I., Lu D. P. Impact of chinese herbal medicine on american society and health care system: perspective and concern. Evidence-based Complementary and Alternative Medicine. 2014;2014 doi: 10.1155/2014/251891.251891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tian D.-D., Jia W.-W., Liu X.-W., et al. Methylation and its role in the disposition of tanshinol, a cardiovascular carboxylic catechol from Salvia miltiorrhiza roots (Danshen) Acta Pharmacologica Sinica. 2015;36(5):627–643. doi: 10.1038/aps.2015.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ji X.-Y., Tan B. K.-H., Zhu Y.-Z. Salvia miltiorrhiza and ischemic diseases. Acta Pharmacologica Sinica. 2000;21(12):1089–1094. [PubMed] [Google Scholar]
- 9.Jia Y., Huang F., Zhang S., Leung S.-W. Is danshen (Salvia miltiorrhiza) dripping pill more effective than isosorbide dinitrate in treating angina pectoris? A systematic review of randomized controlled trials. International Journal of Cardiology. 2012;157(3):330–340. doi: 10.1016/j.ijcard.2010.12.073. [DOI] [PubMed] [Google Scholar]
- 10.Ma B.-L., Ma Y.-M. Pharmacokinetic herb-drug interactions with traditional Chinese medicine: progress, causes of conflicting results and suggestions for future research. Drug Metabolism Reviews. 2016;48(1):1–26. doi: 10.3109/03602532.2015.1124888. [DOI] [PubMed] [Google Scholar]
- 11.Tian D. D., Hu Z. Y. CYP3A4-mediated pharmacokinetic interactions in cancer therapy. Current Drug Metabolism. 2014;15(8):808–817. doi: 10.2174/1389200216666150223152627. [DOI] [PubMed] [Google Scholar]
- 12.Zhao Y.-S., Chen F., Li L. Are circulating metabolites important in pharmacokinetic drug-drug interactions? A retroanalysis of clinical data. Current Drug Metabolism. 2014;15(8):767–790. doi: 10.2174/1389200216666150223152113. [DOI] [PubMed] [Google Scholar]
- 13.Su C.-Y., Ming Q.-L., Rahman K., Han T., Qin L.-P. Salvia miltiorrhiza: traditional medicinal uses, chemistry, and pharmacology. Chinese Journal of Natural Medicines. 2015;13(3):163–182. doi: 10.1016/s1875-5364(15)30002-9. [DOI] [PubMed] [Google Scholar]
- 14.Hochman J., Tang C., Prueksaritanont T. Drug-drug interactions related to altered absorption and plasma protein binding: theoretical and regulatory considerations, and an industry perspective. Journal of Pharmaceutical Sciences. 2015;104(3):916–929. doi: 10.1002/jps.24306. [DOI] [PubMed] [Google Scholar]
- 15.Liu X., Wright M., Hop C. E. C. A. Rational use of plasma protein and tissue binding data in drug design. Journal of Medicinal Chemistry. 2014;57(20):8238–8248. doi: 10.1021/jm5007935. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt S., Gonzalez D., Derendorf H. Significance of protein binding in pharmacokinetics and pharmacodynamics. Journal of Pharmaceutical Sciences. 2010;99(3):1107–1122. doi: 10.1002/jps.21916. [DOI] [PubMed] [Google Scholar]
- 17.Musteata F. M. Monitoring free drug concentrations: challenges. Bioanalysis. 2011;3(15):1753–1768. doi: 10.4155/bio.11.187. [DOI] [PubMed] [Google Scholar]
- 18.Persky A. M., Pollack G. M. Foundations in Pharmacokinetics (Enhanced Edition) Eshelman School of Pharmacy, University of North Carolina at Chapel Hill; 2017. [Google Scholar]
- 19.Peng X., Qi W., Huang R., Su R., He Z. Elucidating the influence of gold nanoparticles on the binding of salvianolic acid B and rosmarinic acid to bovine serum albumin. PLoS ONE. 2015;10(4) doi: 10.1371/journal.pone.0118274.e0118274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shao X., Ai N., Xu D., Fan X. Exploring the interaction between Salvia miltiorrhiza and human serum albumin: insights from herb-drug interaction reports, computational analysis and experimental studies. Spectrochimica Acta Part A: Molecular and Biomolecular Spectroscopy. 2016;161:1–7. doi: 10.1016/j.saa.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 21.Chen T., Cao H., Zhu S., et al. Investigation of the binding of Salvianolic acid B to human serum albumin and the effect of metal ions on the binding. Spectrochimica Acta—Part A: Molecular and Biomolecular Spectroscopy. 2011;81(1):645–652. doi: 10.1016/j.saa.2011.06.068. [DOI] [PubMed] [Google Scholar]
- 22.Peng X., Wang X., Qi W., Su R., He Z. Affinity of rosmarinic acid to human serum albumin and its effect on protein conformation stability. Food Chemistry. 2016;192:178–187. doi: 10.1016/j.foodchem.2015.06.109. [DOI] [PubMed] [Google Scholar]
- 23.Li J. H., Wang S. M. Application of molecular modelling and spectroscopic approaches for investigating the binding of tanshinone IIA to human serum albumin. The Journal of Chemical Thermodynamics. 2013;58:206–210. doi: 10.1016/j.jct.2012.11.009. [DOI] [Google Scholar]
- 24.Chen D., Tu X., Zhang Y. Determination of plasma protein binding rate of salvianol acid a by ultrafiltration. Yao Xue Xue Bao. 2012;2 [Google Scholar]
- 25.Wu Y.-T., Chen Y.-F., Hsieh Y.-J., Jaw I., Shiao M.-S., Tsai T.-H. Bioavailability of salvianolic acid B in conscious and freely moving rats. International Journal of Pharmaceutics. 2006;326(1-2):25–31. doi: 10.1016/j.ijpharm.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Jing C.-J., Chen X.-H., Liu X., Bi K.-S., Guo D.-A. Determination of the binding rate of rat plasma protein with salvianolic acid B. Yaoxue Xuebao. 2010;45(3):343–346. [PubMed] [Google Scholar]
- 27.Hao H., Wang G., Cui N., Li J., Xie L., Ding Z. Pharmacokinetics, absorption and tissue distribution of tanshinone IIA solid dispersion. Planta Medica. 2006;72(14):1311–1317. doi: 10.1055/s-2006-951698. [DOI] [PubMed] [Google Scholar]
- 28.Liu J., Wang X., Cai Z., Lee F. S. C. Effect of tanshinone IIA on the noncovalent interaction between warfarin and human serum albumin studied by electrospray ionization mass spectrometry. Journal of the American Society for Mass Spectrometry. 2008;19(10):1568–1575. doi: 10.1016/j.jasms.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 29.Zhang Z., Ge B., Zhou L., Lam T.-N., Zuo Z. Induction of liver cytochrome P450s by Danshen-Gegen formula is the leading cause for its pharmacokinetic interactions with warfarin. Journal of Ethnopharmacology. 2014;154(3):672–686. doi: 10.1016/j.jep.2014.04.047. [DOI] [PubMed] [Google Scholar]
- 30.Gupta D., Jalali M., Wells A., Dasgupta A. Drug-herb interactions: unexpected suppression of free Danshen concentrations by salicylate. Journal of Clinical Laboratory Analysis. 2002;16(6):290–294. doi: 10.1002/jcla.10057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen D., Lin X.-X., Huang W.-H., et al. Sodium tanshinone IIA sulfonate and its interactions with human CYP450s. Xenobiotica. 2016;46(12):1085–1092. doi: 10.3109/00498254.2016.1152417. [DOI] [PubMed] [Google Scholar]
- 32.Qin C.-Z., Ren X., Zhou H.-H., Mao X.-Y., Liu Z.-Q. Inhibitory effect of salvianolate on human cytochrome P450 3A4 in vitro involving a noncompetitive manner. International Journal of Clinical and Experimental Medicine. 2015;8(9):15549–15555. [PMC free article] [PubMed] [Google Scholar]
- 33.Qiu F., Jiang J., Ma Y., et al. Opposite effects of single-dose and multidose administration of the ethanol extract of danshen on CYP3A in healthy volunteers. Evidence-Based Complementary and Alternative Medicine. 2013;2013 doi: 10.1155/2013/730734.730734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang X., Yeung J. H.-K. Investigation of cytochrome P450 1A2 and 3A inhibitory properties of Danshen tincture. Phytomedicine. 2012;19(3-4):348–354. doi: 10.1016/j.phymed.2011.09.075. [DOI] [PubMed] [Google Scholar]
- 35.Wang X., Yeung J. H. K. Effects of Salvia miltiorrhiza extract on the liver CYP3A activity in humans and rats. Phytotherapy Research. 2011;25(11):1653–1659. doi: 10.1002/ptr.3472. [DOI] [PubMed] [Google Scholar]
- 36.Wang X., Cheung C. M., Lee W. Y. W., Or P. M. Y., Yeung J. H. K. Major tanshinones of Danshen (Salvia miltiorrhiza) exhibit different modes of inhibition on human CYP1A2, CYP2C9, CYP2E1 and CYP3A4 activities in vitro. Phytomedicine. 2010;17(11):868–875. doi: 10.1016/j.phymed.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 37.Qiu F., Zhang R., Sun J., et al. Inhibitory effects of seven components of danshen extract on catalytic activity of cytochrome P450 enzyme in human liver microsomes. Drug Metabolism & Disposition. 2008;36(7):1308–1314. doi: 10.1124/dmd.108.021030. [DOI] [PubMed] [Google Scholar]
- 38.He F., Bi H.-C., Xie Z.-Y., et al. Rapid determination of six metabolites from multiple cytochrome P450 probe substrates in human liver microsome by liquid chromatography/mass spectrometry: application to high-throughput inhibition screening of terpenoids. Rapid Communications in Mass Spectrometry. 2007;21(5):635–643. doi: 10.1002/rcm.2881. [DOI] [PubMed] [Google Scholar]
- 39.Ueng Y.-F., Kuo Y.-H., Peng H.-C., et al. Diterpene quinone tanshinone IIA selectively inhibits mouse and human cytochrome P4501A2. Xenobiotica. 2003;33(6):603–613. doi: 10.1080/0049825031000105769. [DOI] [PubMed] [Google Scholar]
- 40.Wang Q.-L., Wu Q., Tao Y.-Y., Liu C.-H., El-Nezami H. Salvianolic acid B modulates the expression of drug-metabolizing enzymes in HepG2 cells. Hepatobiliary and Pancreatic Diseases International. 2011;10(5):502–508. doi: 10.1016/S1499-3872(11)60085-4. [DOI] [PubMed] [Google Scholar]
- 41.Zhou X., Chan K., Yeung J. H. K. Herb-drug interactions with Danshen (Salvia miltiorrhiza): a review on the role of cytochrome P450 enzymes. Drug Metabolism and Drug Interactions. 2012;27(1):9–18. doi: 10.1515/dmdi-2011-0038. [DOI] [PubMed] [Google Scholar]
- 42.Yu C., Ye S., Sun H., et al. PXR-mediated transcriptional activation of CYP3A4 by cryptotanshinone and tanshinone IIA. Chemico-Biological Interactions. 2009;177(1):58–64. doi: 10.1016/j.cbi.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 43.Zhang R., Sun J., Ma L., et al. Induction of cytochromes P450 1A1 and 1A2 by tanshinones in human HepG2 hepatoma cell line. Toxicology and Applied Pharmacology. 2011;252(1):18–27. doi: 10.1016/j.taap.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 44.Hatfield M. J., Tsurkan L. G., Hyatt J. L., et al. Modulation of esterified drug metabolism by tanshinones from Salvia miltiorrhiza (“Danshen”) Journal of Natural Products. 2013;76(1):36–44. doi: 10.1021/np300628a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lu T., Yang J., Gao X., et al. Plasma and urinary tanshinol from Salvia miltiorrhiza (Danshen) can be used as pharmacokinetic markers for cardiotonic pills, a cardiovascular herbal medicine. Drug Metabolism and Disposition. 2008;36(8):1578–1586. doi: 10.1124/dmd.108.021592. [DOI] [PubMed] [Google Scholar]
- 46.Zhang Y., Akao T., Nakamura N., et al. Extremely low bioavailability of magnesium lithospermate B, an active component from Salvia miltiorrhiza, in rat. Planta Medica. 2004;70(2):138–142. doi: 10.1055/s-2004-815490. [DOI] [PubMed] [Google Scholar]
- 47.Wang L., Zhang Q., Li X., et al. Pharmacokinetics and metabolism of lithospermic acid by LC/MS/MS in rats. International Journal of Pharmaceutics. 2008;350(1-2):240–246. doi: 10.1016/j.ijpharm.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 48.Zhang Y., Jiang P., Ye M., Kim S.-H., Jiang C., Lü J. Tanshinones: sources, pharmacokinetics and anti-cancer activities. International Journal of Molecular Sciences. 2012;13(10):13621–13666. doi: 10.3390/ijms131013621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang J., Huang M., Guan S., et al. A mechanistic study of the intestinal absorption of cryptotanshinone, the major active constituent of Salvia miltiorrhiza. Journal of Pharmacology and Experimental Therapeutics. 2006;317(3):1285–1294. doi: 10.1124/jpet.105.100701. [DOI] [PubMed] [Google Scholar]
- 50.Paine M. F., Oberlies N. H. Clinical relevance of the small intestine as an organ of drug elimination: drug-fruit juice interactions. Expert Opinion on Drug Metabolism and Toxicology. 2007;3(1):67–80. doi: 10.1517/17425255.3.1.67. [DOI] [PubMed] [Google Scholar]
- 51.Giacomini K. M., Huang S.-M., Tweedie D. J., et al. Membrane transporters in drug development. Nature Reviews Drug Discovery. 2010;9(3):215–236. doi: 10.1038/nrd3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.König J., Müller F., Fromm M. F. Transporters and drug-drug interactions: important determinants of drug disposition and effects. Pharmacological Reviews. 2013;65(3):944–966. doi: 10.1124/pr.113.007518. [DOI] [PubMed] [Google Scholar]
- 53.Wu X., Ma J., Ye Y., Lin G. Transporter modulation by Chinese herbal medicines and its mediated pharmacokinetic herb–drug interactions. Journal of Chromatography B. 2016;1026:236–253. doi: 10.1016/j.jchromb.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 54.Wang L., Sweet D. H. Competitive inhibition of human organic anion transporters 1 (SLC22A6), 3 (SLC22A8) and 4 (SLC22A11) by major components of the medicinal herb Salvia miltiorrhiza (Danshen) Drug Metabolism and Pharmacokinetics. 2013;28(3):220–228. doi: 10.2133/dmpk.dmpk-12-rg-116. [DOI] [PubMed] [Google Scholar]
- 55.Wang L., Sweet D. H. Potential for food-drug interactions by dietary phenolic acids on human organic anion transporters 1 (SLC22A6), 3 (SLC22A8), and 4 (SLC22A11) Biochemical Pharmacology. 2012;84(8):1088–1095. doi: 10.1016/j.bcp.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 56.Jia W., Du F., Liu X., et al. Renal tubular secretion of tanshinol: molecular mechanisms, impact on its systemic exposure, and propensity for dose-related nephrotoxicity and for renal herb-drug interactions. Drug Metabolism and Disposition. 2015;43(5):669–678. doi: 10.1124/dmd.114.062000. [DOI] [PubMed] [Google Scholar]
- 57.Cai J., Chen S., Zhang W., et al. Salvianolic acid A reverses paclitaxel resistance in human breast cancer MCF-7 cells via targeting the expression of transgelin 2 and attenuating PI3 K/Akt pathway. Phytomedicine. 2014;21(12):1725–1732. doi: 10.1016/j.phymed.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 58.Zhang J.-L., Cui M., He Y., Yu H.-L., Guo D.-A. Chemical fingerprint and metabolic fingerprint analysis of Danshen injection by HPLC-UV and HPLC-MS methods. Journal of Pharmaceutical and Biomedical Analysis. 2005;36(5):1029–1035. doi: 10.1016/j.jpba.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 59.Hu T., To K. K. W., Wang L., et al. Reversal of P-glycoprotein (P-gp) mediated multidrug resistance in colon cancer cells by cryptotanshinone and dihydrotanshinone of Salvia miltiorrhiza. Phytomedicine. 2014;21(11):1264–1272. doi: 10.1016/j.phymed.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 60.Li X.-X., Zhou Z.-W., Zhou S.-F. Role of P-glycoprotein in the transport of tanshinone I, one active triterpenoid from Salvia miltiorrhiza. Drug Metabolism Letters. 2008;2(3):223–230. doi: 10.2174/187231208785425746. [DOI] [PubMed] [Google Scholar]
- 61.Yu X.-Y., Lin S.-G., Zhou Z.-W., et al. Role of P-glycoprotein in the intestinal absorption of tanshinone IIA, a major active ingredient in the root of Salvia miltiorrhiza Bunge. Current Drug Metabolism. 2007;8(4):325–340. doi: 10.2174/138920007780655450. [DOI] [PubMed] [Google Scholar]
- 62.Qiu F., Zeng J., Liu S., et al. Effects of danshen ethanol extract on the pharmacokinetics of fexofenadine in healthy volunteers. Evidence-Based Complementary and Alternative Medicine. 2014;2014 doi: 10.1155/2014/473213.473213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yin Y., Yang M., Wang Y., et al. Tanshinone IIA increases mRNA expression of efflux transporters in cultured human intestinal cell. The American Journal of Chinese Medicine. 2010;38(5):995–1004. doi: 10.1142/s0192415x1000841x. [DOI] [PubMed] [Google Scholar]
- 64.Wang X., Yeung J. H. K. Effects of the aqueous extract from Salvia miltiorrhiza Bunge on caffeine pharmacokinetics and liver microsomal CYP1A2 activity in humans and rats. Journal of Pharmacy and Pharmacology. 2010;62(8):1077–1083. doi: 10.1111/j.2042-7158.2010.01127.x. [DOI] [PubMed] [Google Scholar]
- 65.Qiu F., Wang G., Zhao Y., et al. Effect of danshen extract on pharmacokinetics of theophylline in healthy volunteers. British Journal of Clinical Pharmacology. 2008;65(2):270–274. doi: 10.1111/j.1365-2125.2007.03027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen Y., Tu J.-H., He Y.-J., et al. Effect of sodium tanshinone II A sulfonate on the activity of CYP1A2 in healthy volunteers. Xenobiotica. 2009;39(7):508–513. doi: 10.1080/00498250902951763. [DOI] [PubMed] [Google Scholar]
- 67.Qiu F., Wang G., Zhang R., Sun J., Jiang J., Ma Y. Effect of danshen extract on the activity of CYP3A4 in healthy volunteers. British Journal of Clinical Pharmacology. 2010;69(6):656–662. doi: 10.1111/j.1365-2125.2010.03624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang P., Sun H., Yang L., et al. Absence of an effect of T89 on the steady-state pharmacokinetics and pharmacodynamics of warfarin in healthy volunteers. The Journal of Clinical Pharmacology. 2014;54(2):234–239. doi: 10.1002/jcph.209. [DOI] [PubMed] [Google Scholar]
- 69.Kuo Y.-H., Lin Y.-L., Don M.-J., Chen R.-M., Ueng Y.-F. Induction of cytochrome P450-dependent monooxygenase by extracts of the medicinal herb Salvia miltiorrhiza. Journal of Pharmacy and Pharmacology. 2006;58(4):521–527. doi: 10.1211/jpp.58.4.0012. [DOI] [PubMed] [Google Scholar]
- 70.Qin W., Wang B., Lu X., Liu H., Wang L., Qi W. Determination of Sodium Tanshinone IIA Sulfonate in human plasma by LC-MS/MS and its application to a clinical pharmacokinetic study. Journal of Pharmaceutical and Biomedical Analysis. 2016;121:204–208. doi: 10.1016/j.jpba.2016.01.026. [DOI] [PubMed] [Google Scholar]
- 71.Kaminsky L. S., Zhang Z.-Y. Human P450 metabolism of warfarin. Pharmacology and Therapeutics. 1997;73(1):67–74. doi: 10.1016/S0163-7258(96)00140-4. [DOI] [PubMed] [Google Scholar]
- 72.Tam L. S., Chan T. Y. K., Leung W. K., Critchley J. A. J. H. Warfarin interactions with Chinese traditional medicines: danshen and methyl salicylate medicated oil. Australian and New Zealand Journal of Medicine. 1995;25(3):p. 258. doi: 10.1111/j.1445-5994.1995.tb01540.x. [DOI] [PubMed] [Google Scholar]
- 73.Yu C. M., Chan J. C. N., Sanderson J. E. Chinese herbs and warfarin potentiation by ‘danshen’. Journal of Internal Medicine. 1997;241(4):337–339. doi: 10.1046/j.1365-2796.1997.134137000.x. [DOI] [PubMed] [Google Scholar]
- 74.Izzat M. B., Yim A. P. C., El-Zufari M. H. A taste of chinese medicine! Annals of Thoracic Surgery. 1998;66(3):941–942. doi: 10.1016/S0003-4975(98)00624-9. [DOI] [PubMed] [Google Scholar]
- 75.Yan Q., Jiang J. Q. Effect of Danshen tablet on anticogulation of warfarin. Chinese Traditional Patent Medicine. 2008;30(1):19–21. [Google Scholar]
- 76.Chang B.-B., Zhang L., Cao W.-W., et al. Pharmacokinetic interactions induced by content variation of major water-soluble components of Danshen preparation in rats. Acta Pharmacologica Sinica. 2010;31(5):638–646. doi: 10.1038/aps.2010.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Guo Z.-J., Zhang Y., Tang X., Li H., Sun Q.-S. Pharmacokinetic interaction between tanshinones and polyphenolic extracts of Salvia miltinorrhiza Bunge after intravenous administration in rats. Biological and Pharmaceutical Bulletin. 2008;31(8):1469–1474. doi: 10.1248/bpb.31.1469. [DOI] [PubMed] [Google Scholar]
- 78.Song M., Hang T.-J., Zhang Z., Chen H.-Y. Effects of the coexisting diterpenoid tanshinones on the pharmacokinetics of cryptotanshinone and tanshinone IIA in rat. European Journal of Pharmaceutical Sciences. 2007;32(4-5):247–253. doi: 10.1016/j.ejps.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 79.Dai H., Li X., Li X., Bai L., Li Y., Xue M. Coexisted components of Salvia miltiorrhiza enhance intestinal absorption of cryptotanshinone via inhibition of the intestinal P-gp. Phytomedicine. 2012;19(14):1256–1262. doi: 10.1016/j.phymed.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 80.Huang J., Zhang J., Bai J., Xu W., Wu D., Qiu X. LC-MS/MS determination and interaction of the main components from the traditional Chinese drug pair Danshen-Sanqi based on rat intestinal absorption. Biomedical Chromatography. 2016;30(12):1928–1934. doi: 10.1002/bmc.3768. [DOI] [PubMed] [Google Scholar]
- 81.Yang S., Zhang K., Lin X., et al. Pharmacokinetic comparisons of single herb extract of Fufang Danshen preparation with different combinations of its constituent herbs in rats. Journal of Pharmaceutical and Biomedical Analysis. 2012;67-68:77–85. doi: 10.1016/j.jpba.2012.03.058. [DOI] [PubMed] [Google Scholar]
- 82.Long W., Zhang S.-C., Wen L., Mu L., Yang F., Chen G. In vivo distribution and pharmacokinetics of multiple active components from Danshen and Sanqi and their combination via inner ear administration. Journal of Ethnopharmacology. 2014;156:199–208. doi: 10.1016/j.jep.2014.08.041. [DOI] [PubMed] [Google Scholar]
- 83.Zhou L., Chow M. S. S., Zuo Z. Effect of sodium caprate on the oral absorptions of danshensu and salvianolic acid B. International Journal of Pharmaceutics. 2009;379(1-2):109–118. doi: 10.1016/j.ijpharm.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 84.Zhao D., Gao Z.-D., Han D.-E., et al. Influence of rifampicin on the pharmacokinetics of salvianolic acid B may involve inhibition of organic anion transporting polypeptide (Oatp) mediated influx. Phytotherapy Research. 2012;26(1):118–121. doi: 10.1002/ptr.3522. [DOI] [PubMed] [Google Scholar]
- 85.Li M., Wang F., Huang Y., et al. Systemic exposure to and disposition of catechols derived from Salvia miltiorrhiza roots (Danshen) after intravenous dosing danhong injection in human subjects, rats, and dogs. Drug Metabolism and Disposition. 2015;43(5):679–690. doi: 10.1124/dmd.114.061473. [DOI] [PubMed] [Google Scholar]