Abstract
Multiple sclerosis (MS) is a chronic neurological condition, characterized by recurrent episodes of inflammation and demyelination of the central nervous system called relapsing-remitting episodes, and continuous axonal degeneration that leads to irreversible progressive invalidity.
Patients with multiple sclerosis present a higher mortality rate compared to the general population, and the excess of mortality may be explained by the increased cardiovascular risk and occurrence of cardiovascular disease. However, the exact pathways to cardiovascular dysfunction are not yet completely elucidated.
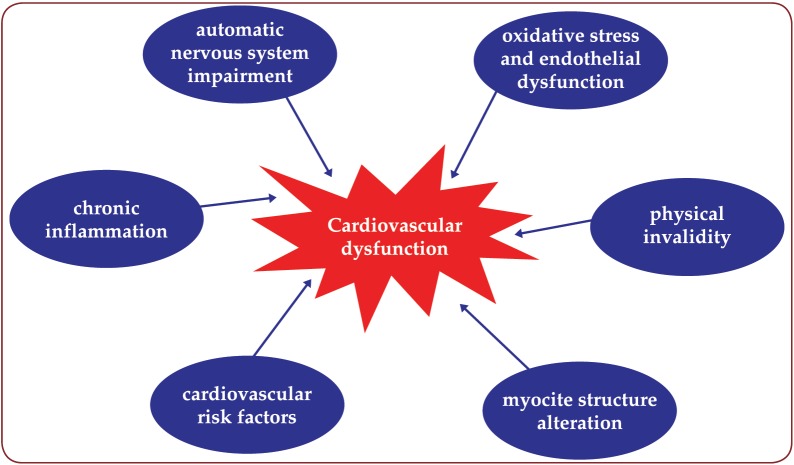
This review focuses on the most important mechanisms of cardiovascular dysfunction in MS, such as the cardiomyocite structure alteration, the cardiovascular autonomous nervous system dysfunction, physical invalidity, oxidative stress and endothelial dysfunction, as well as the impact of cardiovascular risk factors in MS.
The latest evidence about therapeutic approaches for MS, such as immunomodulatory treatment, vitamin D supplementation and statins are also discussed.
There is little knowledge about the cardiovascular dysfunction in MS, and further research is required to improve the understanding of these complex mechanisms.
Keywords:multiple sclerosis, cardiovascular dysfunction, immunonodulatory treatment
INTRODUCTION
Multiple sclerosis (MS) is a chronic neurological condition, characterized by recurrent episodes of inflammation and demyelination of the central nervous system leading to relapsing-remitting episodes and to continuous axonal degeneration with irreversible progressive invalidity (1). MS is the main cause of non-traumatic neurological invalidity in young and middle-aged population, representing a major public health issue. The disease becomes clinically manifest in the early third decade of life, when the individual is economically and socially active, requiring higher costs than stroke or Alzheimer’s disease (2,3). Moreover, patients with MS have a lower life expectancy than normal population, but detailed data on mortality in MS is limited (4). Recent studies show that the median survival time from the onset of the disease is approximately 10 years shorter for these patients. Furthermore, MS is associated with an almost threefold increase in the risk for death, most of the data suggesting that this is due to cardiovascular disease (5, 6). Several large studies reveal the high occurrence of cardiovascular disease in patients with MS, demonstrating that the risk of ischemic heart disease, stroke or heart failure is significantly increased in this population (7). However, recent research shows controversial results regarding the risk of cardiovascular disease occurrence and death in MS people (8).
CARDIOVASCULAR DYSFUNCTION MECHANISMS IN MULTIPLE SCLEROSIS DISEASE
In the next paragraphs we will describe the main mechanisms for cardiovascular dysfunction in MS that have been studied by now: the myocite function alteration, the cardiovascular autonomous nervous system dysfunction, the physical invalidity, oxidative stress and endothelial dysfunction, the impact of cardiovascular risk factors in early atherosclerosis development in MS, like the presence of inflammation, smoking, hypertension, type 2 diabetes mellitus, dyslipidemia, obesity, psychosocial stress and procoagulant status. The main described mechanisms are summarized in Figure 1.
Figure 1.
Figure 1. Main mechanisms of cardiovascular dysfunction in MS. Adapted after (17,19,30,43,52,69).
Cardiomyopathies in neuromuscular disorders
Cardiomyopathies are generally characterized by abnormal structure, dimension or function of the left or right ventricular myocardium in the absence of arterial hypertension, coronary heart disease, valve abnormalities or congenital heart disease (9). The cause of cardiomyopathies caused by neuromuscular disorders is unknown, but there are indications that isoforms of mutated muscle proteins causing muscle disease are also expressed in the myocardium (10).
MS is a neuromuscular disorder, involving the upper motor neuron with demyelination, accompanied by a disruption in the ability of the nerves to conduct electrical impulses to and from the brain. Until today, there are no studies demonstrating the association between MS and the development of cardiomyopathies, so research in this area should be intensified. Our study group started a protocol to determine the subclinical myocardial dysfunction in MS patients using the newest echocardiography techniques, which concluded that patients with MS, either treated or not, have subclinical biventricular systolic dysfunction with normal vascular function, suggesting an intrinsic myocardial impairment (11).
Cardiovascular autonomous nervous system dysfunction
The autonomous nervous system is affected in the course of MS due to the lesions of the regions responsible for autonomic regulation. Parasympathetic dysfunction is closely related to the progression of disability in patients with MS. In contrast, sympathetic dysfunction was associated to the clinical activity of MS (12). The main tests for diagnosing the cardiovascular autonomous dysfunction are: head up tilt test for assessment of impaired heart rate and blood pressure response to orthostatic challenge, deep breathing test, Valsalva maneuver, handgrip test and baroreflex stimulation (13).
A recent meta-analysis on cardiovascular autonomic dysfunction in multiple sclerosis from 16 studies including 611 patients showed that the proportion of patients with autonomic dysfunction was two-fold higher when using a threshold of one than when using a threshold of two abnormal autonomic tests (42.1% vs. 18.8%, p=0.006). This is why the lack of consensus about the threshold for the diagnosis of autonomic dysfunction in patients with multiple sclerosis may cause problems of comparability in literature, and no threshold is completely acceptable for diagnosing it, although using the definition of at least one abnormal test is the approach that appears to have the greatest sensitivity (13).
Physical invalidity
Sedentary behavior has been associated with increased risk of obesity, metabolic syndrome, type 2 diabetes and cardiovascular disease mortality. (14) Physical invalidity might be an important determinant of cardiovascular dysfunction in MS. MS patients are less physically active compared to healthy people and healthy sedentary individuals (15). Disability status and progression of the disease are associated with reduced physical activity, which, combined with other factors may lead to a higher susceptibility for subclinical atherosclerosis and cardiac dysfunction (16). On the other hand, MS does not prohibit adapted physical activity. Moreover, it has been established that quality of life in MS people is correlated with physical activity level. Studies showed that rehabilitation interventions like exercise training and educational intervention have a stronger effect on severity of patient-reported fatigue compared to the two most commonly prescribed fatigue medications (Amantadine and Modafinil) (17). The results of these studies suggest that rehabilitation interventions should be the initial treatment choice for people with MS who are reporting disabling fatigue. MS women that do low to moderate long-term physical activity have significantly less abdominal fat accumulation, lower levels of triglycerides, and lower levels of glucose. This may improve cardiovascular disease risk and contribute to important health-related benefits (18).
Oxidative stress and endothelial dysfunction
Oxidative stress is defined as an imbalance between oxidants and antioxidants, in favor of the oxidants, leading to molecular damage (19). It increases with the biological aging process, and it independently causes a greater risk of cardiovascular disease. Endothelial cells and vascular smooth muscle cells produce reactive oxygen and nitrogen species which oxidize low-density lipoproteins (LDL). Oxidized LDL enters subendothelial spaces where they initiate atherosclerosis (20). Oxidative stress consequently leads to endothelial dysfunction, the early feature of atherosclerotic vascular di sease, characterized by a decrease in nitric o xide (NO) bioavailability and a concomitant increase in vascular superoxide (O-) formation. Loss of NO bioavailability precedes the development of overt atherosclerosis and is an independent predictor of adverse cardiovascular events (21).
Reactive oxygen species and reactive nitrogen species increase several times in MS (22). The central nervous system has a high susceptibility to oxidative stress due to the high rate utilization of the oxygen, the relatively poor antioxidants and the high concentration of polyunsaturated fatty acids. Multiple studies indicate an intense peripheral oxidative stress in MS patients (23). This may lead to endothelial dysfunction, arterial remodeling and stiffness, and at the end at overt atherosclerosis.
Cardiovascular risk factors in multiple sclerosis
The major risk factors that promote the development of atherosclerosis are elevated lowdensity lipoprotein (LDL) cholesterol level, low high-density lipoprotein (HDL) level, cigarette smoking, type 2 diabetes, hypertension and a family history of coronary heart disease, ischemic stroke or peripheral arterial disease. Other conditions thought to increase the risk of atherosclerotic disease include abdominal obesity, hypertriglyceridemia, high plasma levels of lipoprotein (a) and homocysteine, hyperfibrinogenemia, the inflammatory marker C-reactive protein (CRP) and physical inactivity. Other emerging risk factors, including uric acid, psycho- social stress, encompassing external stressors (e.g. job stress life events and financial problems), and reactions to stress (e.g. depression, anxiety, psychosocial distress and sleep disturbances), have as well their contribution (24).
The cardiovascular risk factors are present in MS population and our review discusses the most frequent ones: (a) inflammation status, (b) smoking, (c) arterial hypertension, (d) type 2 diabetes mellitus, (e) dyslipidemia, (f) obesity, (g) psychosocial stress and (h) procoagulant status.
(a) Inflammation. Inflammation is considered to have an important role in atherosclerosis. Evidence indicates that inflammation, both focal and systemic, plays a key role in formation, destabilization and rupture of atherosclerotic plaques, leading to acute cardiovascular events (25).
High levels of CRP are associated with disease activity in MS (26). Cytokines are the principal mediators of immunity. MS is an immune- mediated disease with principal emphasis on the activated inflammatory cells. Studies indicate that pro-inflammatory cytokine levels such as IL-1, IL-6, TNF-ƒÑ or IFN-ƒ× are increased in MS patients. On the other hand, the IL-10, which plays an important role in the regulation of immune responses and is considered the main anti-inflammatory cytokine, was decreased in MS patients when compared with healthy individuals (27).
(b) Smoking. Smoking is one of the major modifiable risk factors for coronary artery disease and the largest risk factor for coronary artery disease for those below the age of 45, especially women (28). Smoking leads to decrease NO levels, increased levels of NO synthase inhibitors, decreased NO synthase expression, increased production of oxygen radicals, and inflammatory reactions, resulting in augmented oxidative stress, endothelial dysfunction, subsequent arterial remodeling and stiffness and overt atherosclerosis (29). It also produces higher plaque instability, faster platelet activation and coagulation and increased mitochondrial damage in heart myocite (29). Smoking significantly accelerates the onset of coronary artery disease presentation. The average smoker develops coronary artery calcification, a sensitive marker for early development of coronary artery disease, 10 years earlier than a non-smoker (30).
Cigarette smoking is one of the most postulated environmental risk factors linked to the onset and clinical course of MS in genetically susceptible individuals, along with the vitamin D level, latitude and Epstein Barr virus infection (31). The incidence of smoking is greater in MS people than in general population, leading to an excess of cardiovascular disease (32).
(c) Hypertension. For all ages and for all ethnic groups, hypertension has a direct relation with the incidence of cardiovascular events like stroke, myocardial infarction, sudden death, heart failure and peripheral artery disease (33). Most of the studies regarding hypertension in patients with MS concluded that incidence is the same as in the general population, 30-45 %. Marrie et al reported that 30% of 8983 patients with MS were hypertensive, percentage similar for the general population (34). Moreover, patients with MS who developed hypertension had a faster progression of the disease and clinical disability (35).
(d) Type 2 diabetes mellitus. People with type 2 diabetes mellitus (DM) have a 2-3 times higher risk of myocardial infarction or stroke, independent of the association with other cardiovascular risk factors (36). Studies report different results regarding the prevalence of type 2 DM in MS patients. Hussein et al reported a higher prevalence of type 2 DM compared to general population (37), however, Marrie et al found similar prevalence (38). Patients with MS and type 2 DM may have a worse progression of disability compared to people without DM: a 29% increased risk of early gait disability, a 28% increased risk of requiring unilateral assistance and a 56% increased risk of requiring bilateral assistance for walking. However, DM determines increased disability compared to patients with MS without DM (39).
(e) Dyslipidemia. There is a direct relation between serum cholesterol and cardiovascular mortality and morbidity, as shown by important epidemiological studies. The cardiovascular risk grows with 2-3% with every 1% growth of serum cholesterol (40). There is contradictory data regarding the lipid profile in patients with MS. Studies show only slightly elevated total cholesterol, LDL and triglycerides in these patients compared to controls. However, LDL cholesterol has a negative impact on acute inflammatory activity and disease course in MS patients (41). On the contrary, higher levels of HDL have a beneficial effect on course of the disease, which is consistent with the antioxidant and anti-inflammatory properties of HDL. EDSS worsening was associated with higher baseline LDL and total cholesterol levels, with trends for higher triglyceride. Higher HDL levels were associated with lower contrast-enhancing neurological lesion volume in MRI (42). Oxidized LDL was also high in the MS serum, as a marker of early a therosclerosis, and correlated with the disease activity (43).
(f) Obesity. Different methods have been used to quantify obesity, including body mass index, waist circumference, waist-to-hip ratio, waist-to-height ratio, but regardless of the chosen index, overall and central adiposity confer a greater risk for subsequent cardiovascular diseases, both in men and women (44). Approximately 50% of patients with MS are overweight or obese, the same with the general population (45). Recent data suggest that childhood and adolescence obesity increases the risk of MS in females beyond established heritable and environmental risk factors (46).
(g) Psychosocial stress. The lifetime incidence of depression in patients with MS is 50%, nearly three times higher than in the general population (47). The mechanisms of depression are multiple. First, depression can be reactive following the diagnosis and the uncertainties about the prognosis and the future in general. Second, depression may be related to the release of proinflammatory cytokines such as interferon-ƒ×, TNF-ƒÑ or IL-6 that can produce symptoms which reinforce an underlying tendency for depression. Third, structural changes in the brain due to neurodegeneration may contribute to the development of depression (48). By activating the inflammatory mechanisms and consequent acceleration of endothelial dysfunction and early atherosclerosis, patients with depression are at higher risk of developing cardiovascular disease.
(h) Procoagulant status. D-dimer concentrations were raised in MS patients serum, correlated with homocysteine levels. It has been demonstrated that axonal damage in MS lesions is associated with failure of fibrinolysis because of the inhibition of the plasminogen activator system (49). So, in MS patients, the procoagulant system is enhanced, while the fibrinolysis system is reduced. This may also contribute to cardiovascular disease.
THE INFLUENCE OF TREATMENT ON CARDIOVASCULAR DYSFUNCTION
There is no cure in MS, the treatments approved for use focus only on preventing relapses and on slowing down the progression of the disease. The treatment drugs are divided into first-line drugs: interferon beta (Avonex, Rebif, and Betaferon) and glatiramer acetat (Copaxone), injectable disease modifying treatments available for more than 15 years, and teriflunomide (Aubagio) and dimethylfumarate (Tecfidera), newcomer oral disease modifying treatments. The second line agents include fingolimod (Gilenya), natalizumab (Taysabri) and mitoxantrone (Novantrone). A third line is now available with alemtuzumab and some forth class experimental therapies. First class therapies have a good safety profile, but the clinical response is often suboptimal, and there are still unknown issues about the right timing to switch for a second line agent of whether escalation therapy is an appropriate strategy (50). The use of mitoxantrone is limited by the cardiotoxicity effect, first time documented in the cure of cancer, because it may affect the structure of the cardiac myocite and may cause irreversible cardiomyopathy, with reduced left ventricular ejection fraction and congestive heart failure (51). A recent metaanalysis showed that the incidence of significant heart dysfunction was almost 12% under mitoxantrone treatment. This is why recent guidelines recommend assessing cardiac function before each dose of mitoxantrone, regardless of the cumulative dose, and on an annual basis even after discontinuation, given the potential for delayed development of cardiotoxicity (52).
Vitamin D supplementation showed its positive effects in delaying the relapses and in modulation of the immune regulation (53). There is also research on the effect of statins on the course of MS, but the results of the latest metaanalysis (54) concluded that combination therapy of IFN beta plus statin is not able to reduce in a definite way the relapse rate or to prevent progression in MS. The analysis included only a small number of trials, so it is necessary to perform more randomized trials in order to establish the statins’ precise indication.
CONCLUSION
Patients with MS have a higher mortality rate compared to the general population. The excess of mortality could be explained by the increased cardiovascular risk and occurrence of cardiovascular disease. The main mechanisms described so far are cardiomyocite structure alteration, the cardiovascular autonomous nervous system dysfunction, physical invalidity, oxidative stress and endothelial dysfunction and the presence of cardiovascular risk factors in MS.
There is little knowledge about the cardiovascular dysfunction in MS, and subsequent research is required to improve the understanding of these mechanisms. Thus, our research group has started a study to investigate the cardiovascular dysfunction in MS, ongoing at this moment.
Abbreviations
MS = multiple sclerosis;
LDL = low density lipoprotein;
HDL = high density lipoprotein;
EDSS = expanded disability status scale;
NO = nitric oxide;
CRP = C-reactive protein;
hs CRP = high-sensitivity C-reactive protein;
CVD = cardiovascular disease;
TNF = tumor necrosis factor;
IL = interleukine;
IFN = interferon;
DM = diabetes mellitus;
BMI = body mass index;
MRI = magnetic resonance imaging.
Conflict of interests: none declared.
Financial support: This paper is partially supported by the Sectorial Operational Programme Human Resources Development (SOPHRD), financed by the European Social Fund and the Romanian Government under the contract number POSDRU 141531.
Contributor Information
Raluca Ileana Mincu, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Lucia Stefania Magda, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Cardiology, Emergency University Hospital, Bucharest, Romania.
Maria Florescu, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Cardiology, Emergency University Hospital, Bucharest, Romania.
Andreea Velcea, Department of Cardiology, Emergency University Hospital, Bucharest, Romania.
Sorina Mihaila, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Diana Mihalcea, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Bogdan O. Popescu, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
Adela Chiru, Department of Neurology, Colentina Clinical Hospital, Bucharest, Romania.
Cristina Tiu, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Cardiology, Emergency University Hospital, Bucharest, Romania.
Mircea Cinteza, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Cardiology, Emergency University Hospital, Bucharest, Romania.
Dragos Vinereanu, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Cardiology, Emergency University Hospital, Bucharest, Romania.
REFERENCES
- Bajenaru O - Ghiduri de diagnostic si tratament in neurologie. Bucuresti: Editura Medicala Almatea. 2010 [Google Scholar]
- Barnes MP, Gilhus NE, Wender M - Task force on minimum standards for health care of people with multiple sclerosis. Eur J Neurol. 2001;8:215–220. doi: 10.1046/j.1468-1331.2001.00194.x. [DOI] [PubMed] [Google Scholar]
- Ropper AH, Samuels MA - Multiple sclerosis and allied demyalinating diseases. In: Adams and Victor’s principles of neurology. New York: McGraw-Hill Medical. 2009;771:796. [Google Scholar]
- Goodin DS - The epidemiology of multiple sclerosis: insights to disease pathogenesis. In: Handbook of Clinical Neurology. Elsevier. 2014;231:266. doi: 10.1016/B978-0-444-52001-2.00010-8. [DOI] [PubMed] [Google Scholar]
- Kang JH, Chen YH, Lin HC - Comorbidities amongst patients with multiple sclerosis: A population-based controlled study. . Eur J Neurol. 2010;17:1215–1219. doi: 10.1111/j.1468-1331.2010.02971.x. [DOI] [PubMed] [Google Scholar]
- Lalmohamed A, Bazelier MT, Van Staa TP, et al. - Causes of death in patients with multiple sclerosis and matched referent subjects: A population- based cohort study. Eur J Neurol. 2012;19:1007–1014. doi: 10.1111/j.1468-1331.2012.03668.x. [DOI] [PubMed] [Google Scholar]
- Jadidi E, Mohammadi M, Moradi T - High risk of cardiovascular diseases after diagnosis of multiple sclerosis. Mult Scler. 2013;19:1336–1340. doi: 10.1177/1352458513475833. [DOI] [PubMed] [Google Scholar]
- Wenz I, Dalgas U, Stenager E, et al. - Risk factors related to cardiovascular diseases and the metabolic syndrome in multiple sclerosis – a systematic review. Mult Scler. 2013;19:1556–1564. doi: 10.1177/1352458513504252. [DOI] [PubMed] [Google Scholar]
- Elliott P, Andersson B, Arbustini E, et al. - Classification of the cardiomyopathies: a position statement from the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29:270–276. doi: 10.1093/eurheartj/ehm342. [DOI] [PubMed] [Google Scholar]
- Finsterer J, Stöllberger C - Primary myopathies and the heart. Scand Cardiovasc J. 2008;42:9–24. doi: 10.1080/14017430701854953. [DOI] [PubMed] [Google Scholar]
- Mincu RI, Magda LS, Velcea A, et al. - Multiple sclerosis determines subclinical biventricular dysfunction. Eur Heart J. 2014;35 (Supplement):1004. [Google Scholar]
- Flachenecker P, Reiners K, Klauser M, et al. - Autonomic dysfunction in multiple sclerosis is related to disease activity and progression of disability. Mult Scler. 2001;7:327–337. doi: 10.1177/135245850100700509. [DOI] [PubMed] [Google Scholar]
- Racosta JM, Sposato LA, Morrow SA, et al. - Cardiovascular autonomic dysfunction in multiple sclerosis: A meta-analysis. Mult Scler Relat Disord. 2015;4:104–111. doi: 10.1016/j.msard.2015.02.002. [DOI] [PubMed] [Google Scholar]
- Matthews CE, George SM, Moore SC, et al. - Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95:437–445. doi: 10.3945/ajcn.111.019620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickmans K, Simoens F, Nijs J, et al. - Recovery of peripheral muscle function from fatiguing exercise and daily physical activity level in patients with multiple sclerosis: A case-control study. Clin Neurol Neurosurg. 2014;122:97–105. doi: 10.1016/j.clineuro.2014.04.021. [DOI] [PubMed] [Google Scholar]
- Ranadive SM, Yan H, Weikert M, et al. - Vascular dysfunction and physical activity in multiple sclerosis. Med Sci Sports Exerc. 2012;44:238–243. doi: 10.1249/MSS.0b013e31822d7997. [DOI] [PubMed] [Google Scholar]
- Asano M, Finlayson ML - Meta-analysis of three different types of fatigue management interventions for people with multiple sclerosis: exercise, education, and medication. Mult Scler Int. 2014;2014:798285. doi: 10.1155/2014/798285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slawta JN, McCubbin JA, Wilcox AR, et al. - Coronary heart disease risk between active and inactive women with multiple sclerosis. Med Sci Sports Exerc. 2002;34:905–912. doi: 10.1097/00005768-200206000-00001. [DOI] [PubMed] [Google Scholar]
- Sies H - Oxidative stress: a concept in redox biology and medicine. Redox Biology. 2015;4:180–183. doi: 10.1016/j.redox.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North BJ, Sinclair DA - The intersection between aging and cardio-vascular disease. Circ Res. 2012;110:1097–1108. doi: 10.1161/CIRCRESAHA.111.246876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osto E, Cosentino F - The Role of Oxidative Stress in Endothelial Dysfunction and Vascular Inflammation. Nitric Oxide. 2010;22:705–754. [Google Scholar]
- Zuliani C, Baroni L - Bioactive Nutraceuticals and Dietary Supplements in Neurological and Brain Disease Prevention and Therapy- Antioxidants for the Prevention and Treatment of Multiple Sclerosis: An Overview. Academic Press. 2015 [Google Scholar]
- Tasset I, Aguera E, Sanchez-Lopez F, et al. - Peripheral oxidative stress in relapsing–remitting multiple sclerosis. Clin Biochem. 2012;45:440–444. doi: 10.1016/j.clinbiochem.2012.01.023. [DOI] [PubMed] [Google Scholar]
- Hansson GK, Hamste A - Atherosclerosis, Thrombosis, and Vascular Biology. Goldman’s Cecil Medicine. 2012;1:409–412. [Google Scholar]
- Madjid M, Willerson JT - Inflammatory markers in coronary heart disease. Br Med Bull. 2001;100:23–38. doi: 10.1093/bmb/ldr043. [DOI] [PubMed] [Google Scholar]
- Soilu-Hanninen M, Koskinen J, Laaksonen M, et al. - High sensitivity measurement of CRP and disease progression in Multiple Sclerosis. J Neurol Sci. 2005;238:S250. doi: 10.1212/01.wnl.0000167129.90918.f5. [DOI] [PubMed] [Google Scholar]
- Polachini CNR, Spanevello RM, Casali EA, et al. - Alterations in the cholinesterase and adenosine deaminase activities and inflammation biomarker levels in patients with multiple sclerosis. Neuroscience. 2014;266:266–274. doi: 10.1016/j.neuroscience.2014.01.048. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Colditz GA, Stampfer MJ, et al. - Smoking cessation and time course of decreased risks of coronary heart disease in middle-aged women. Arch Intern Med. 1999;154:169–175. [PubMed] [Google Scholar]
- Toda N, Tanabe S, Nakanishi S - Nitric oxide-mediated coronary flow regulation in patients with coronary artery disease: recent advances. Int J Angiol. 2011;20:121–134. doi: 10.1055/s-0031-1283220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann N, Mohlenkamp S, Mahabadi AA - Effect of smoking and other traditional risk factors on the onset of coronary artery calcification: results of the Heinz Nixdorf Recall Study. Atherosclerosis. 2014;232:339–345. doi: 10.1016/j.atherosclerosis.2013.11.045. [DOI] [PubMed] [Google Scholar]
- Handel AE, Williamson AJ, Disanto G, et al. - Smoking and multiple sclerosis: an updated meta-analysis. PLoS One. 2011;6:e16149. doi: 10.1371/journal.pone.0016149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundstrom P, Nystrom L, Hallmans G - Smoke exposure increases the risk for multiple sclerosis. Eur J Neurol. 2008;15:579–583. doi: 10.1111/j.1468-1331.2008.02122.x. [DOI] [PubMed] [Google Scholar]
- Lewington S, Clarke R, Qizilbash N, et al. - Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- Marrie RA, Rudick R, Horwitz R, et al. - Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74:1041–1047. doi: 10.1212/WNL.0b013e3181d6b125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almdal T, Scharlng H, Jensen JS, et al. - The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke and death: a population based study of 13000 men and women with 20 years of follow up. Arch Intern Med. 2004;164:1422–1426. doi: 10.1001/archinte.164.13.1422. [DOI] [PubMed] [Google Scholar]
- - Third report of the National Cholesterol Education Program Expert Panel on detection, evaluation and treatment of high blood cholesterol in adults. Circulation. 2002;106:31–43. [PubMed] [Google Scholar]
- Hussein WI, Reddy SS - Prevalence of diabetes in patients with multiple sclerosis. Diabetes Care. 2006;29:1984–1985. doi: 10.2337/dc06-0811. [DOI] [PubMed] [Google Scholar]
- Marrie RA, Yu BN, Leung S, et al. - Rising prevalence of vascular comorbidities in multiple sclerosis: validation of administrative definitions for diabetes, hypertension, and hyperlipidemia. Mult Scler. 2012;18:1310–1319. doi: 10.1177/1352458512437814. [DOI] [PubMed] [Google Scholar]
- Wong E, Backholer K, Gearon E, et al. - Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1:106–114. doi: 10.1016/S2213-8587(13)70046-9. [DOI] [PubMed] [Google Scholar]
- Rosengren A, Perk J, Dallongeville J - ESC Textbook of Cardiovascular Medicine. . Oxford University Press. 2009 [Google Scholar]
- Tettey P, Simpson S Jr, Taylor BV, et al. - Vascular comorbidities in the onset and progression of multiple sclerosis. J Neurol Sci. 2014;347:23–33. doi: 10.1016/j.jns.2014.10.020. [DOI] [PubMed] [Google Scholar]
- Weinstock-Guttman B, ZivadinovR, Mahfooz N, et al. - Serum lipid profiles are associated with disability and MRI outcomes in multiple sclerosis. J Neuroinflammation. 2011;8:127. doi: 10.1186/1742-2094-8-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palavra F, Marado D, Mascarenhas- Melo F, et al. - New markers of early cardiovascular risk in multiple sclerosis patients: oxidized-LDL correlates with clinical staging. Dis Markers. 2013;34:341–348. doi: 10.3233/DMA-130979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rebecca P, Gelber, J. Michael Gaziano, et al. - Measures of Obesity and Cardiovascular Risk Among Men and Women. JACC. 2008;52:605–615. doi: 10.1016/j.jacc.2008.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana SR, DiGiacomo AM, Rohini V, et al. - Prevalence of overweight and obesity among Veterans with multiple sclerosis. Int J MS Care. 2006;8:59. [Google Scholar]
- Gianfrancesco MA, Acuna B, Shen L, et al. - Obesity during childhood and adolescence increases susceptibility to multiple sclerosis after accounting for established genetic and environmental risk factors. Obesity Research and Clinical Practice. 2014;8:e435–e447. doi: 10.1016/j.orcp.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman Consensus Group - The Goldman Consensus statement on depression in multiple sclerosis. Mult Scler. 2005;11:328–338. doi: 10.1191/1352458505ms1162oa. [DOI] [PubMed] [Google Scholar]
- Ziemssen T - Multiple sclerosis beyond EDSS: depression and fatigue. J Neurol Sci. 2009;277:S37–S41. doi: 10.1016/S0022-510X(09)70011-5. [DOI] [PubMed] [Google Scholar]
- Gveric D, Herrera BM, Cuzne ML - tPA Receptors and the Fibrinolytic Response in Multiple Sclerosis Lesions. Am J Pathol. 2005;166:1143–1151. doi: 10.1016/S0002-9440(10)62334-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michel L, Larochelle C, Prat A - Update on treatments in multiple sclerosis. La Presse Médicale. 2015;44:e137–e151. doi: 10.1016/j.lpm.2015.02.008. [DOI] [PubMed] [Google Scholar]
- Joyce E, Mulroy E, Scott J, et al. - Subclinical Myocardial Dysfunction in Multiple Sclerosis Patients Remotely Treated With Mitoxantrone; Evidence of Persistent Diastolic Dysfunction. J Card Fail. 2013;19:571–576. doi: 10.1016/j.cardfail.2013.06.003. [DOI] [PubMed] [Google Scholar]
- Marriott JJ, Miyasaki JM, Gronseth G, et al. - Evidence Report: The efficacy and safety of mitoxantrone (Novantrone) in the treatment of multiple sclerosis: Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2010;74:1463–1470. doi: 10.1212/WNL.0b013e3181dc1ae0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correale J, Ysrraelit MC, Gaitan MI - Vitamin D-mediated immune regulation in multiple sclerosis. J Neurol Sci. 2011;311:23–31. doi: 10.1016/j.jns.2011.06.027. [DOI] [PubMed] [Google Scholar]
- Wang J, Xiao Y, Luo M, et al. - Statins for multiple sclerosis. Cochrane Database Syst Rev. 2011;7(12):CD008386. doi: 10.1002/14651858.CD008386.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]