Abstract
Introduction:
According to the Romanian Renal Registry (RRR), only 8% of patients on renal replacement therapy (RRT) in 2012 received a kidney transplant (KTx). As not all transplant centers report to RRR, the outcome of transplanted patients in Romania is not known. Therefore, we aimed to evaluate the outcome in patients grafted in one of the largest transplant center in the country as compared to hemodialysis (HD) and peritoneal dialysis (PD) patients recorded by the RRR.
Method:
In an intention-to-treat analysis using Kaplan-Meier and Cox proportional hazard (CPH) models, survival was compared between 8050 incident HD, 1000 PD and 490 KTx patients treated between 2008 and 2011. The patients were stratified by modality at day 90 of therapy.
Results:
As compared to HD and PD patients, the KTx recipients were younger, more often of male gender, and had glomerulonephritis as primary renal disease (PRD) more frequently. KTx patients had a higher mean survival time (57.68 [56.95-58.42] months) than HD (45.55 [45.04- 46.06] months) or PD patients (46.33 [45.01-47.65] months). In the multivariate CPH model, higher age (OR=1.03 (1.02-1.03), p<0.01) at RRT initiation, HD (OR=5.60 (3.16-9.94), p<0.01) and PD (OR=5.62 (3.14-10.08), p<0.01) as RRT and diabetic nephropathy (p<0.01) as PRD were associated with a poorer survival.
Conclusion:
The present study is the first to provide representative information about the outcome of the KTx patients in Romania. We found that patient survival after KTx is markedly better than either HD or PD. Urgent implementation of a KTx registry is needed in order to improve the national transplantation program.
Keywords:kidney transplantation, hemodialysis, peritoneal dialysis, survival
INTRODUCTION
End stage renal disease (ESRD) incidence and prevalance is rapidly increasing worldwide in the context of improved diagnostic and treatment capabilities of chronic kidney disease, and diabetes mellitus type 2 global epidemic (1,2). Thus, renal replacement therapy (RRT) is emerging as one of the most difficult challenges for health care systems in both developed and developing countries. Kidney transplantation (KTx) is considered to offer durable survival benefit, better quality of life and increased cost efficiency over dialysis (3-5). However, important differences exists between countries in approaches and practices of KTx. For example, within the European Union (EU) only about one third of the RRT patients are living on a functional graft (6). Furthermore, with the notable exception of Norway, the number of KTx had not parallel the increasing number of patients in need for RRT (2,6).
Romania, with a population of 20 121 641 and 14 879 ESRD patients (739 per million population) on 31 December 2012, is the seventh largest country in the EU. According to the Romanian Renal Registry (RRR), only 8% of the patients in need for RRT received a KTx in 2012 (7). As not all transplant centers report to RRR, the outcome of transplanted patients in Romania is not known. Therefore, we aimed to evaluate the survival and identify the risk factors associated with mortality in patients grafted in one of the largest transplant center in the country as compared to hemodialysis (HD) and peritoneal dialysis (PD) patients recorded by the RRR.
METHODS
Patients
We retrospectively examined the outcome on December 31, 2012 of the incident dialysis patients registred by the RRR and those who recieved a kidney graft at “Fundeni Clinical Institute” between January 1, 2008 and December 31, 2011. The patients were stratified by modality at day 90 of therapy: KTx, HD or PD. We excluded patients younger than 18 years, those who had recovery of renal function or were lost to follow up during the first 90 days.
Data collection
The data available for analyses were: age, gender, primary renal disease (PRD), date of first RRT and history of RRT, date and cause of death. The RRT modality was classified as HD (home hemodialysis, center hemodialysis and hemodiafiltration), PD (continuous ambulatory peritoneal dialysis and automated peritoneal dialysis) and KTx (preemptive and non-preemptive transplantation). The primary renal diagnosis was summarized in six categories: glomerulonephritis (GN), renovascular disease (RVD), tubulointerstitial disease (TID), diabetic nephropathy (DN), familial or hereditary nephropathies (HN) and other or unknown renal diagnosis.
Statistical analysis
Continuous variables are presented as mean or median and 95% confidence intervals, according to their distribution, and categorical variables as percentages. Comparisons between groups were done with Student T test or Kruskal-Wallis test, as appropriate. The statistical analysis was conducted using an intention to treat approach – multiple switches between RRT methods were ignored.
Survival analyses were conducted with the Kaplan-Meier method, and the log rank test was used for comparison. The intent-to-treat analysis used the Cox proportional hazard (CPH) model to estimate hazard ratio (HR) and 95 % CI for the three RRT modalities. The analysis of the variables related to survival was carried out using the multivariate CPH model. A p .0.05 was considered statistically significant. Statistical analyses were performed with SPSS (SPSS Inc., Chicago, IL) and Analyse-it (Analyse-it Software, Ltd., Leeds, UK) packages.
RESULTS
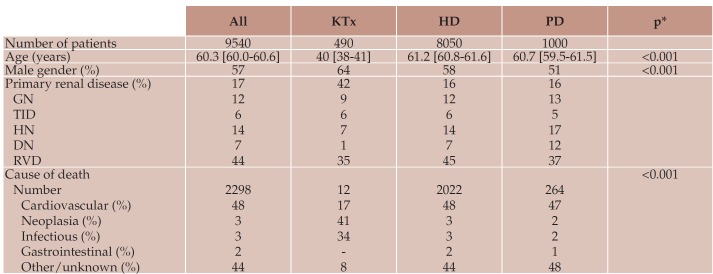
A total of 9540 patients started RRT and fulfilled the study criteria. The median age of the entire cohort was 60.3 [60.0-60.6] years; 57% were male. The main primary renal diseases were GN, DN and TID (17%, 14% and 12%, respectively). However, the primary diagnosis was unknown in a large proportion of patients (44%) (Table 1).
Of the patients included in the study, 8050 (84%) were incident on HD, 1000 (10%) on PD and 490 (6%) on KTx. Most transplantations were non-preemptive (81%) with a median dialysis time before procedure of 15.5 [12-18] months; 64% were living donor grafts. As compared to HD and PD patients, the KTx recipients were younger, more often of male gender, and had GN as primary renal disease more frequently (Table 1).
A total of 2298 patients died during the period of the study. The leading causes of death were cardio-vascular in HD and PD patients, while neoplasms and infections dominated in KTx recipients (Table 1). The mean survival time for the entire cohort was 46.21 [45.76- 46.67] months. The cumulative chances of survival at 12, 24, 36 and 48 months were 83.5%, 78.2%, 74.2% and 72.3%, respectively. KTx recipients had a higher mean survival time (57.68 [56.95-58.42] months) than HD (45.55 [45.04-46.06] months) and PD patients (46.33 [45.01-47.65] months) (Figure 1). No difference in survival was observed between HD and PD patients (p=0.63; log-rank test).
In the multivariate CPH model, higher age at RRT initiation, HD and PD as RRT and DN as PRD were associated with a poorer survival (Table 2).
Table 1.
Table 1. Patient characteristics.
DN diabetic nephropathy, GN glomerulonephritis, HD hemodialysis, HN hereditary nephropathies, KTx kidney transplant, PD peritoneal dialysis, RVD renovascular disease, TID tubulointerstitial disease. * KTx versus HD versus PD.
DISCUSSION
In contrast to dialysis, the renal transplantation program made only marginal contribution to the RRT progress in Romania. Although increasing from 2% in 2007 to 8% in 2012, the number of patients in need of RRT that received a KTx is still alarmingly low when compared with the EU mean (7). However, these data are not accurate, since are based on estimates from one of the largest national KTx centers and the non-preemptive KTx reports of the dialysis centers. The present study is the first to provide representative information about the outcome of the KTx patients in Romania. We found that patient survival after KTx is markedly better than either HD or PD.
ESRD is progressively becoming a geriatric condition due to increased prevalence of diabetes mellitus type 2 and hypertension, improved life expectancy, and greater access to dialysis of the older patients (8). There is growing evidence that elderly patients, in the absence of contraindication and significant comorbid conditions, have better outcomes after KTx than alternative forms of RRT (9-12). However, the increased number of aged patients on dialysis in Europe and United States is not matched by a proportional growth of KTx in this segment of population (6,8,9). According to the 2012 ERA-EDTA Registry Report, there is a drastically difference between the European and Romanian mean KTx established therapy in the age group 65-74 years – 41% vs. 1%. Furthermore, in the >75 years group the European mean is 14% for KTx, while in Romania there is virtually no patient registred in this age group (2). Our results confirms these figures, renal transplant recipients were significantly younger than the patients on dialysis and only 0.6% were over 65 years old. Different healthcare policies can be used to increase access to KTx of older patients: implementation of expanded criteria for donors (donor age >60 years or 50-59 years with two of the following – hypertension, terminal creatinine level >1.5mg/dL, death from stroke), joining the Eurotransplant Seniors Program (ESP) initiative – which allocates kidneys from donors older than age 65 to recipients of similar age only by blood group and waiting time (9, 13). The ESP age matching seems to be an effective allocation system, since graft and patient survival were not negatively affected when compared to the standard allocation (14).
Among the causes leading to ESRD, GN and DN had similar percentages in the HD and PD groups. Comparable results have been reported in Norway in the dialysis population (16.6% GN and 16.8% DN), but the 14% prevalence of DN in our incident RRT patients remains lower than the 20-30% reported by the West European countries and the 40-45% reported by the United States (2,15). In the KTx group almost half of the patients had GN and only 7% DN. These findings can be explained by the young age of the recipients. Nevertheless, the low percentage of KTx patients with diabetes is worrisome in the context of global DN epidemic. Compared with dialysis, renal transplantation is associated with a better survival and an increase in life expectancy of more than 11 years among ESRD patients due to DN (4, 16). The salutary effect of successful KTx is likely to reflect the reduction in fatal and nonfatal cardiovascular complications in diabetic patients (17-19).
Living donor grafts are related to a better outcome than those from deceased donors. The advantage of living donor kidneys seems to be the same for spousal and unrelated donors (20). The better outcomes are probably due to: high quality renal tissue with an increased nephron mass transplanted, the general benefits of elective as opposed to urgent surgery, avoidance of ischemia-reperfusion injury, shorter time on waiting list, better social suport and a greater sense of obligation to keep medical compliance (21). We found that more than half of the grafts came from living donors, which might have contributed to the better outcome of the KTx recipients. However, these results also reflect an undeveloped national network for cadaveric organ procurement.
Most of our patients were non-preemptively transplanted with a median dialysis time of more than one year. This transplantation timing could be detrimental for the graft survival since data from the United States Renal Data Systems database have shown that pretransplant dialysis duration of six months or more is associated with poor graft outcome (22,23). Furthermore, the risk of death with a functional allograft is also higher in these patients (22,23). In order to increase preemptive KTx, referral to a transplant team for evaluation should take place at an estimated GFR (eGFR) <30 mL/ min/1.73m2 (24). Experts generally agree that transplantation should not be performed until the eGFR is <20 mL/min/1.73m2 and evidence exists of progressive and irreversible decrease in renal function over the previous 6 to 12 months (25). The earlier referral threshold would allow appropriate candidates to be on the waiting list at the time the eGFR declines to 20 mL/min/1.73 m2.
With 50 to 60 percent of deaths, cardiovascular disease is the leading cause of mortality in adult renal graft recipients (26). However, most of the deaths attributable to cardiovascular disease are amongst those with diabetes, whereas infection and malignancy are more commonly in those without diabetes (18). Accordingly, the increased mortality from infection and malignancy observed in our KTx patients could be explained by the low prevalence of DN.
The cumulative chances of survival at 12 and 24 months were similar in our RRT cohort to those reported by the ERA-EDTA Registry for the 2006-2010 cohort (83.5% vs. 83.1% and 78.2% vs. 72.6%) (2). The unadjusted overall survival comparisons between RRT showed markedly improved survival of KTx recipients over HD and PD. Furthermore, the survival advantage remained after adjustments for age, gender and primary renal disease. Our results agree with several studies which examined the survival among patients treated with dialysis versus KTx using similar methodology (27-29). The survival benefit of KTx over dialysis may result from better clearence of uremic toxins. Also, in non-preemptive recipients inflammation seems to be significantly lower post transplantation (30). Moreover, diabetic patients benefit from reduction in the levels of circulating advanced glycosilation end products (31). Interestingly, left ventricular hypertrophy tends to diminish after KTs, which might decrease the mortality from coronary heart disease (32). Due to their comorbidities, a great number of the dialysis population is unsuitable for KTx. Thus, the survival comparisons between renal transplant and dialysis methods are best performed by comparing the survival rates of the patients on waiting list with those who have undergone surgery. Multiple studies from Europe and United States using these two comparative groups showed that patient and graft survivals is better with renal transplantation than with dialysis (4,16,33-35). However, we were not able to conduct such an analysis, since currently there is no national waiting list for KTx in Romania.
In order to improve the KTx program, a unique national database for renal transplantation is urgently needed. The transplantation registry, which will collect information regarding the risk factors of mortality and morbidity, forms the basis for future management of donors and recipients, and provides the support for efficient health-care policy decisions. According to the RRR, HD has the highest estimated cost for one patient per year – 17,000 Euro, followed by PD with 12,500 Euro and KTx with 11,750 Euro (7). The increasing prevalence of ESRD patients on dialysis therapy in the context of a finite health-care budget requires the optimization of patients allocation to renal replacement therapies. In line with this, the RRR proposed a model of economic impact for five yearsin which the increase to 20% in the ratio of incident PD patients and a minimum of 400 kidney grafts per year would allow newly-included patients to be treated without rising the dialysis program budget (7).
Our study has several limitations. First, data on KTx were available only from one national transplant center and the reports of non-preemptive transplants from dialysis centers registred by the RRR. However, currently there are only two large centers that perform renal transplantation, so our results could are representative. Second, the data from RRR, while providing specific clinical and demographic data for a large sample size, do not include information on comorbidities and laboratory tests. Third, our study design used an intention-to-treat censoring strategy, rather than an as-treated one.
CONCLUSION
In conclusion, the present study provides evidence that in the current setting of ESRD in Romania, there is a substantial long-term survival advantage for renal transplantation compared with dialysis. Urgent implementation of a KTx registry is required in order to improve the national transplantation program. Also, improvement in allocation strategies are needed to better match the life expectancy of organs and recipients.
Conflict of interests: none declared.
Financial support: The present study was financed by European Union using Sectoral Operational Program Human Resources Development (POSDRU) program - POSDRU/159/1.5/S/ 133377.
Contributor Information
Gabriel Stefan, Department of Nephrology, “Dr. Carol Davila” University Hospital of Nephrology, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Liliana Garneata, Department of Nephrology, “Dr. Carol Davila” University Hospital of Nephrology, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Dorina Tacu, Center of Uronephrology and Renal Transplantation, Fundeni Clinical Institute, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Cristina Bucsa, Center of Uronephrology and Renal Transplantation, Fundeni Clinical Institute, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Ioanel Sinescu, Center of Uronephrology and Renal Transplantation, Fundeni Clinical Institute, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Gabriel Mircescu, Department of Nephrology, “Dr. Carol Davila” University Hospital of Nephrology, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
REFERENCES
- Collins AJ, Foley RN, Gilbertson DT, et al. - The state of chronic kidney disease, ESRD, and morbidity and mortality in the first year of dialysis. Clin J Am Soc Nephrol. 2009;4Suppl1:S5–11. doi: 10.2215/CJN.05980809. [DOI] [PubMed] [Google Scholar]
- Academic Medical Center, Department of Medical Informatics. ERA-EDTA Registry: ERA-EDTA Registry Annual Report 2012. Amsterdam,The Netherlands: 2014. [Google Scholar]
- Hunsicker LG - A survival advantage for renal transplantation. N Engl J Med. 1999;341:1762–63. doi: 10.1056/NEJM199912023412310. [DOI] [PubMed] [Google Scholar]
- Wolfe RA, Ashby VB, Milford EL, et al. - Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–30. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- Haller M, Gutjahr G, Kramar R, et al. - Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol Dial Transplant. 2011;26:2988–95. doi: 10.1093/ndt/gfq780. [DOI] [PubMed] [Google Scholar]
- Stel VS, Kramar R, Leivestad T, et al. - Time trend in access to the waiting list and renal transplantation: a comparison of four European countries. Nephrol Dial Transplant. 2012;27:3621–31. doi: 10.1093/ndt/gfs089. [DOI] [PubMed] [Google Scholar]
- Romanian Renal Registry 2012 Report. In. Bucharest, Romania: “Dr Carol Davila” Teaching Hospital of Nephrology 2014. [Google Scholar]
- Berger JR, Hedayati SS - Renal replacement therapy in the elderly population. Clin J Am Soc Nephrol. 2012;7:1039–46. doi: 10.2215/CJN.10411011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang E, Segev DL, Rabb H - Kidney transplantation in the elderly. Semin Nephrol. 2009;29:621–35. doi: 10.1016/j.semnephrol.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann EL, Wu C - The evolving challenge of evaluating older renal transplant candidates. Adv Chronic Kidney Dis. 2010;17:358–67. doi: 10.1053/j.ackd.2010.03.012. [DOI] [PubMed] [Google Scholar]
- Dempster NJ, Ceresa CD, Aitken E, et al. - Outcomes following renal transplantation in older people: a retrospective cohort study. BMC Geriatr. 2013;13:79. doi: 10.1186/1471-2318-13-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oniscu GC, Brown H, Forsythe JL - How great is the survival advantage of transplantation over dialysis in elderly patients? Nephrol Dial Transplant. 2004;19:945–51. doi: 10.1093/ndt/gfh022. [DOI] [PubMed] [Google Scholar]
- Rao PS, Merion RM, Ashby VB, et al. - Renal transplantation in elderly patients older than 70 years of age: results from the Scientific Registry of Transplant Recipients. Transplantation. 2007;83:1069–74. doi: 10.1097/01.tp.0000259621.56861.31. [DOI] [PubMed] [Google Scholar]
- Frei U, Noeldeke J, Machold-Fabrizii V, et al. - Prospective age-matching in elderly kidney transplant recipients--a 5-year analysis of the Eurotransplant Senior Program. Am J Transplant. 2008;8:50–7. doi: 10.1111/j.1600-6143.2007.02014.x. [DOI] [PubMed] [Google Scholar]
- Collins AJ, Foley RN, Herzog C, et al. - US Renal Data System 2012 Annual Data Report. Am J Kidney Dis. 2013;61:e1–476. doi: 10.1053/j.ajkd.2012.11.031. [DOI] [PubMed] [Google Scholar]
- Oniscu GC, Brown H, Forsythe JL – Impact of cadaveric renal transplantation on survival in patients listed for transplantation. J Am Soc Nephrol. 2005;16:1859–65. doi: 10.1681/ASN.2004121092. [DOI] [PubMed] [Google Scholar]
- Lentine KL, Brennan DC, Schnitzler MA Incidence and predictors of myocardial infarction after kidney transplantation. J Am Soc Nephrol. 2015;16:496–506. doi: 10.1681/ASN.2004070580. [DOI] [PubMed] [Google Scholar]
- Cosio FG, Hickson LJ, Griffin MD, et al. - Patient survival and cardiovascular risk after kidney transplantation: the challenge of diabetes. Am J Transplant. 2008;8:593–99. doi: 10.1111/j.1600-6143.2007.02101.x. [DOI] [PubMed] [Google Scholar]
- Meier-Kriesche HU, Schold JD, Srinivas TR, et al - Kidney transplantation halts cardiovascular disease progression in patients with end-stage renal disease. Am J Transplant. 2004;4:1662–68. doi: 10.1111/j.1600-6143.2004.00573.x. [DOI] [PubMed] [Google Scholar]
- Terasaki PI, Cecka JM, Gjertson DW, et al. - High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med. 1995;333:333–6. doi: 10.1056/NEJM199508103330601. [DOI] [PubMed] [Google Scholar]
- Kaplan B, Srinivas TR, Meier-Kriesche HU - Factors associated with long-term renal allograft survival. Ther Drug Monit. 2002;24:36–9. doi: 10.1097/00007691-200202000-00007. [DOI] [PubMed] [Google Scholar]
- Meier-Kriesche HU, Port FK, Ojo AO, et al. - Effect of waiting time on renal transplant outcome. Kidney Int. 2000;58:1311–17. doi: 10.1046/j.1523-1755.2000.00287.x. [DOI] [PubMed] [Google Scholar]
- Goldfarb-Rumyantzev A, Hurdle JF, Scandling J, et al. - Duration of end-stage renal disease and kidney transplant outcome. Nephrol Dial Transplant. 2005;20:167–75. doi: 10.1093/ndt/gfh541. [DOI] [PubMed] [Google Scholar]
- National Kidney F - K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266. [PubMed] [Google Scholar]
- Knoll G, Cockfield S, Blydt-Hansen T, et al. - Canadian Society of Transplantation: consensus guidelines on eligibility for kidney transplantation. CMAJ. 2005;173:S1–25. doi: 10.1503/cmaj.1041588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojo AO - Cardiovascular complications after renal transplantation and their prevention. Transplantation. 2006;82:603–11. doi: 10.1097/01.tp.0000235527.81917.fe. [DOI] [PubMed] [Google Scholar]
- Vollmer WM, Wahl PW, Blagg CR - Survival with dialysis and transplantation in patients with end-stage renal disease. N Engl J Med. 1983;308:1553–58. doi: 10.1056/NEJM198306303082602. [DOI] [PubMed] [Google Scholar]
- Port FK, Wolfe RA, Mauger EA, et al. - Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. JAMA. 1993;270:1339–43. [PubMed] [Google Scholar]
- Hutchinson TA, Thomas DC, Lemieux JC, et al. - Prognostically controlled comparison of dialysis and renal transplantation. Kidney Int. 1984;26:44–51. doi: 10.1038/ki.1984.132. [DOI] [PubMed] [Google Scholar]
- Cueto-Manzano AM, Morales-Buenrostro LE, Gonzalez-Espinoza L, et al. - Markers of inflammation before and after renal transplantation. Transplantation. 2005;80:47–51. doi: 10.1097/01.tp.0000164348.16689.03. [DOI] [PubMed] [Google Scholar]
- Makita Z, Bucala R, Rayfield EJ, et al. - TheReactive glycosylation endproducts in diabetic uraemia and treatment of renal failure. Lancet. 1994;343:1519–22. doi: 10.1016/s0140-6736(94)92935-1. [DOI] [PubMed] [Google Scholar]
- McGregor E, Jardine AG, Murray LS, et al. - Pre-operative echocardiographic abnormalities and adverse outcome following renal transplantation. Nephrol Dial Transplant. 1998;13:1499–505. doi: 10.1093/ndt/13.6.1499. [DOI] [PubMed] [Google Scholar]
- Rabbat CG, Thorpe KE, Russell JD, et al. - Comparison of mortality risk for dialysis patients and cadaveric first renal transplant recipients in Ontario, Canada. J Am Soc Nephrol. 2000;11:917–22. doi: 10.1681/ASN.V115917. [DOI] [PubMed] [Google Scholar]
- Meier-Kriesche HU, Ojo AO, Port FK, et al. - Survival improvement among patients with end-stage renal disease: trends over time for transplant recipients and wait-listed patients. J Am Soc Nephrol. 2001;12:1239–96. doi: 10.1681/ASN.V1261293. [DOI] [PubMed] [Google Scholar]
- Gill JS, Tonelli M, Johnson N, et al. – The impact of waiting time and comorbid conditions on the survival benefit of kidney transplantation. Kidney Int. 2005;68:2345–51. doi: 10.1111/j.1523-1755.2005.00696.x. [DOI] [PubMed] [Google Scholar]