Abstract
The 2016 WHO-CMP classification proposal defines a broad spectrum of JAK2 V617F mutated MPN phenotypes: normocellular ET, hypercellular ET due to increased erythropoiesis (prodromal PV), hypercellular ET with megakaryocytic-granulocytic myeloproliferation and splenomegaly (EMGM or masked PV), erythrocythemic PV, early and overt classical PV, advanced PV with MF and post-PV MF. ET heterozygous for the JAK2 V617F mutation is associated with low JAK2 mutation load and normal life expectance. PV patients are hetero-homozygous versus homozygous for the JAK2 V617F mutation in their early versus advanced stages with increasing JAK2 mutation load from less than 50% to 100% and increase of MPN disease burden during life long follow-up in terms of symptomatic splenomegaly, constitutional symptoms, bone marrow hypercellularity and secondary MF. Pretreatment bone marrow biopsy in prefibrotic MPNs is of diagnostic and prognostic importance. JAK2 exon 12 mutated MPN is a distinct benign early stage PV. CALR mutated hypercellular thrombocythemia show distinct PMGM bone marrow characteristics of clustered larged immature dysmorphic megakaryocytes with bulky (bulbous) hyperchromatic nuclei, which are not seen in JAK2 mutated ET and PV. MPL mutated normocellular thrombocythemia is featured by clustered giant megakaryocytes with hyperlobulated stag-horn-like nuclei without features of PV in blood and bone marrow. Myeloproliferative disease burden in each of the JAK2, CALR and MPL MPNs is best reflected by the degree of anemia, splenomegaly, mutation allele burden, bone marrow cellularity and myelofibrosis.
Keywords:Myeloproliferative neoplasms; Essential thrombocythemia; Polycythemia vera; Primary megakaryocytic granulocytic myeloproliferation; Myelofibrosis; JAK2V617F mutation; MPL515 mutation; Calreticulin mutation; JAK2 wild type; Bone marrow pathology
INTRODUCTION
Dameshek and Henthell defined in 1940 the clinical characteristics for a definite diagnosis of PV (polycythemia vera): plethoric appearance, splenomegaly, definitely elevated erythrocyte count above 6×1012/L, elevated platelet count, and elevated hematocrit (Ht) (1). The bone marrow is in general highly specific, showing large megakaryocytes and a panmyelosis of increased trilinear erythrocytic-megakaryocytic-granulocytic myeloproliferation (1,2). Blood volume esti mation (red cell mass: RCM) is not required to diagnose PV (1-3). Dameshek (2) considered the majority of PV patients as fundamentally normal and the treatment of PV should be venessection aiming at Ht of 40% resulting in a state of iron deficiency (1-3). In PV in complete remission by phlebotomy alone, red cell count remains elevated above 6×1012/L. Due to microcytosis of red cells, the haemoglobin (Hb) and Ht levels remain low for periods of months to years (1-4). It is possible to relief symptoms and control hypervolemia in PV patients by phlebotomy alone for more than fifteen years. Such PV patient are in as good health as comparable persons of the same age group (3-5).
In 1950, Dameshek (2) (1900-1969, Figure 1) defined PV as a total marrow disorder of trilinear erythrocythemic, thrombocythemic and granulocythemic myeloproliferation (EMGM) with blood erythrocytosis, leukocytosis and thrombocytosis. Dameshek proposed the one cause hypothesis for PV as a trilinear myeloproliferative disease (MPD) due to either the presence of excessive bone marrow stimulation by an unknown factor or the lack or diminution of an inhibitory factor (2,3). The one cause hypothesis of Dameshek for trilinear PV has been confirmed by Vainchenker in France (Figure 1) in 2005 by his discovery of the acquired somatic JAK2 V617F mutation as the cause of erythrocythemic, megakaryocythemic and granulocythemic myeloproliferation (EMGM) associated with three clinical phenotypes of MPN: essential thrombocythemia (ET), PV and myeloid neoplasia of the spleen (MNS) with secondary myelofibrosis (MF) (2,3). In his editorial on some speculations of the myeloproliferative syndromes, Dameshek recognized in 1951 megakaryocyte leukemia (ML) without features of PV. This ML entity has recently been recognized as MPL or CALR mutated thrombocythemia without features of PV (Figure 1) (6- 9).
RCM, RED CELL COUNTS AND BONE MARROW HISTOLOGY IN ET AND PV
The crude PVSG and 2008 WHO criteria of Hb >18.5 g/dL and Ht >60% in men and Hb >16.5 g/dL and Ht >56% in women do need red cell mass (RCM) measurement to distinguish JAK2 V617F mutated ET from PV in cases with Hb and Ht in the upper level of normal (10-12). The 2013-2015 WHO-ECMP criteria used bone marrow histology as a pathognomic clue to distinguish MPN from reactive thrombocytosis and from BCR/ABL positive thrombocythemia in CML and thrombocythemia myelodysplastic syndromes, 5q minus syndrome in particular by the demonstration of clustered mature large megakaryocytes in MPN and small megakaryocytes in CML and MDS (7-9). Megakarycyte morphology are not different in prefibrotic JAK2 V617F mutated ET and PV patients (Figure 2, Tables 1 and 2). The prospective Rotterdam studies assessed the WHO-CMP criteria of PV (Table 2) related to RCM, Hb, Ht and erythrocyte counts in 10 ET and 16 PV patients in whom RCM, peripheral blood and bone marrow data were available (Table 3). The correlation curves between erythrocyte count, Hb or Ht versus RCM showed the best correlation between erythrocyte counts and RCM (Figure 3). At RCM above 30 ml/kg the erythrocytes are above 5.8x1012/L in all 19 WHO-CMP defined PV patients (Table 3, Figure 3). At erythrocyte counts above 5.8x1012/L, the Ht values range from 46% to 72% in WHO-CMP defined PV (Table 3, Figure 3). At erythrocyte counts below 5.8 x1012/L, the Ht values range from 40% to 45% in WHOCMP defined ET who had normal RCM (Figure 3, Table 1). At erythrocytes above 5.8 x1012/L, the Hb values ranged from 15.0 g/dL to 20.9 g/ dL and are below 2008 WHO criteria in 3 females and 2 males (Table 3 in blue), who had increased RCM. At erythrocytes above 5.8 x1012/L, the Ht values ranged from 46% to 72% and are below 2008 WHO criteria but had increased RCM in 7 females and 1 male (Table 3 in blue). Seven ET patients had normal RCM at erythrocyte counts between 4.4 to 5.3 x1012/L of whom 4 had WHO normocellular (<60%) ET and 3 had hypercellular (60-80%) prodromal PV bone marrow histology (Table 3). Increase of erythrocytes counts above 5.8x1012/L for the diagnosis of PV appears to be independent from the iron deficient status and persists in PV in a clinical remission obtained by repeated venesection (Figure 4) thereby confirming the observations of Dameshek (2,3). Erythrocyte count at a cutoff level of the upper limit of normal (5.8 x10/12L in males and 5.6 x10/12L in females) separates JAK2-mutated ET and prodromal PV from classical PV (Figures 3 and 4, Tables 1 and 2) obviating the need to measure RCM in JAK2 V617F and exon 12 mutated MPN patients. It is the degree of erythrocythosis (erythrocyte count above the upper limit of normal) on top of characteristic bone marrow histology, increased LAP score and decreased serum EPO levels that separates WHO JAK2 V617F mutated classical PV from ET and prodromal PV to determine the need of phlebotomy in PV (7-9).The reduction in iron reserve in PV leads to an insufficient amount of iron for the synthesis of hemoglobin in the developing red cells, and as a result that bone marrow iron stain is negative in PV (2,3), but usually present in ET (6-9). As iron deficiency develops in PV on treatment with phlebotomy, the mature red cells produced become smaller (microcytic) than normal and occupy less room in the circulation, which is associated with the relief of hypervolemic symptoms. The Hb and Ht levels remain low at mean red cell volumes (MCV) below 70fl for periods of months to years in PV patients in complete haematological remission by phlebotomy alone, but the erythrocyte count persist to remain above 5.8x1012/L (Figures 4). As the MCV of red cells becomes reduced to levels below 70 cubic micron due to the chronic iron deficiency state, the discrepancy between the high red cell count far above 6x1012/L and low Hb level appears to be a diagnostic clue to PV in remission (2,3,6-9).
Figure 1.
Figure 1. The 1950 Dameshek one cause hypothesis of trilinear PV (2) has been confirmed by Vainchenker’s discovery in 2005 (13,14) of heterozygous and homozygous JAK2 V617F mutations as the driver cause of the trilinear erythroctic, megakaryocytic granulocytic myeloproliferation (EMGM) myeloproliferative neoplasms polycythemia vera (PV, essential thrombocythemia (ET) and secondary myelofibrosis (MF). In the editorial on speculations of myeloproliferative syndromes in 1951 (5), Dameshek recognized megakaryocytic leukemia (ML) as a distinct entity without features of PV at diagnosis and follow-up. This ML entity has recently be recognized as MPL or calreticulin (CALR) mutated thrombocythemia without features of PV (8,9).
Figure 2.
Figure 2. Translation of the 2008 WHO clinical criteria (11,12) into 2016 WHO-CMP criteria (6-9) for the classification of JAK2 V617F mutated ET, PV and EMGM or masked PV (red), versus CALR mutated primary megakaryocytic granulocytic myeloproliferation (PMGM, blue) and MPL mutated normocellular ET (black). All molecular variants of MPN disease burden is reflected by the degree of anemia, myeloid neoplasia of the spleen (splenomegaly), bone marrow cellularity and secondary myelofibrosis.
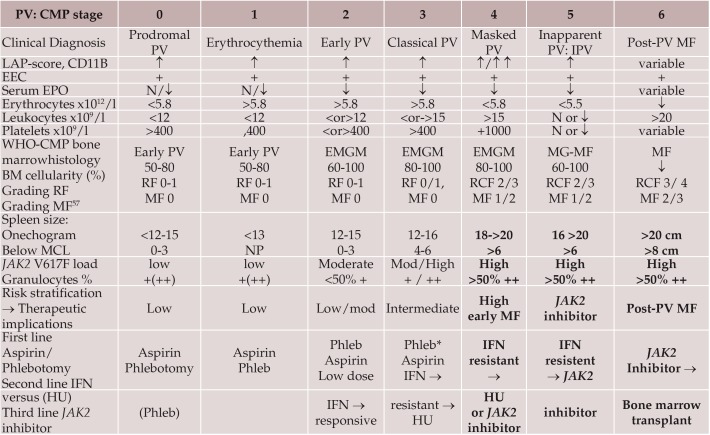
Table 1.
Table 1. 2016 WHO Clinical Molecular and Pathobiological (2016 WHO-CMP) criteria for diagnosis of JAK2 V617F mutated essential throbocythemia (ET) (6-9).
Table 2.
Table 2. 2016 WHO Clinical Molecular andPathological (2016 WHO-CMP) criteria for the diagnosis of prodromal, masked and classical JAK2 mutated polycythemia vera (PV) versus primary or secondary erythrocytoses (6-9).
2014 WHO-CMP criteria for staging of prodromal, erythrocythemic, and advanced PV
A2 + B1 + P1 establish early PV (mimicking ET) prodromal PV CMP stage 0
A1 + A2 + A3 + P1and none of B establish idiopathic erythrocythemia (IE) or stage 1 PV
A1 + A2 + A3 + P1 and one or more of B establish classic stages of PV stage 2 and 3
A2 + B3 + P1 detect masked cases of PV with splenomegaly and hypersplenism to be labelled as Inapparent PV (IPV) frequently seen Budd-Chiari syndrome or splanchnic vein thrombosis
Figure 3.
Figure 3. Erythrocyte counts x1012/L vertical axis versus red cell mass (RCM) horizontal axis according to Michiels et al. (6-9,52,53).
At erythrocyte values below 5.8 x1012/L the red cell mass (RCM) values are between 25 and 30 ml/kg in essential thrombocythemia (ET). At erythrocyte values above 5.7x1012/L all values of RCM area bove 30/kg in all polycythemia vera (PV) cases indicating that the erythrocyte cut-off level of 5.7 x1012/L dicriminates between ET and PV The numbers in the blue line are erythrocyte counts x1012/l.
Table 3.
Table 3. The relation between RCM, erythrocyte count and bone marrow histology findings at time of diagnosis in 26 MPN patients: 10 ET and 14 PV and in 2 ET cases at time of evolution into PV as compared to the 2008 WHO cut-of levels of hemoglobin (Hb) and hematocrit (Ht) for PV: Hb >18.5 g/dl and Ht >0.60 in men and Hb >16.5 and Ht >0.56 in women for the diagnosis of PV.
At RCM above 30 ml/kg (Red) the erythrocytes are above 5.7 x1012/L = PV (Red).
Of 10 ET cases 7 had ET and 3 had PV with erythrocytes above 5.7x1012/L (Bold)
At erythrocytes above 5.7 x1012/L Hb ranges from 15.0 to 20.9 and are below WHO criteria in 3 females and 2 males (Blue)
At erythrocytes above 5.7 x1012/L the Ht ranges from 0.46 to 0.72 and are below WHO criteria in 7 females and 1 male (Blue)
For further interpretation of these data see figure 1.
Figure 4.
Figure 4. Clinical course in a casewith idiopathic erythrocythemia (IE) or erythrocythemic polycythemia vera treated with venesections (arrows). The development of microcytic hypochromic erythrocytes due to iron deficiency was associated with persistent increased red cell count (>6x1012/L), which is diagnostic for PV. Phlebotomy on top of low dose aspirin induces iron deficiency with microcytic erythrocytes (MCV around 65 fL), normal values for haemoglobin (Hb) and hematocrit (Ht) and relief of hypervolumic symptoms.
Table 4.
Table 4. Staging of JAK2 V617F positive prodromal PV, erythrocythemic PV, classical PV, early MF, inapparent PV, spent phase PV and post-PV myelofibrosis (MF) according to 2016 WHO-CMP criteria related to therapy (6-9,52,53).
*↑ = increased, ↓ = decreased, N = normal, + = present or heterozygous; ++ = homozygous
JAK2 V617F mutated trilinear PV and ET: Vainchenker’s Disease
The JAK2 V617F mutated trilinear MPN is featured by erythrocytic, megakaryocytic and granulocytic myeloprolifeation (EMGM) with a broad spectrum of variable clinical manifestations including normocellular ET, prodromal PV, erythrocythemic PV with normal platelet and leukocyte count, classical PV, masked PV and various degrees of myeloid neoplasia of the spleen and secondary MF (13,14). The morphology of clustered medium to large megakaryocytes in bone marrow smears and biopsies were not different in JAK2 V617F mutated ET and PV patients (Figure 5, Tables 1 and 2). Detection of JAK2 V617F has become the first intention diagnostic test to differentiate between PV and erythrocythemic (IE) from erythrocytosis with a sensitity of 95% and specificity of 100% (15-26). The prevalence of the JAK2 V617F mutation in PVSG defined PV is 95% and about 50% in ET and MF7 (15,16). The majority of ET patients are heterozygous for the JAK2 V617F mutation with a JAK2 mutation load of less than 10% to 50% of the granulocytes. Early stage PV patients are hetero-homozygous for the JAK2 V617F mutation with a JAK2 mutation load of less than 50%, whereas PV patients with advanced MPN disease burden are homozygous for the JAK2 mutation with increased JAK2 burden between 50% to 100% of the granulocytes (Figure 6) (17-21). A group of JAK2 V617F positive normocellular ET with a very low percentage of heterozygous mutant JAK2 can maintain as a non-progessive subpopulation in the bone marrow without a tendency to evolve into prodromal PV or hypercellular ET during long term follow-up (22). Patients with hypercellular ET and PV homozygous for the JAK2 V617F mutation patients are at high risk for anemia and myeloid metaplasia of the spleen (splenomegaly) with secondary myelofibrosis (19). Two studies demonstrated that so-called heterozygous PV with allele load less than 50% are hetero/homozygous at the EEC level in blood and bone marrow for the JAK2 V617F mutation, whereas ET patients are heterozygous reflecting a maximal JAK2 V617F mutation load of 50% (20,21). Homozygosity for JAK2 V617F results from mitotic recombination. Homozygous-mutant BFU-E were present in most patients with PV but not in those with ET. According to Michiels & Vainchenker in 2006, the heterozygous status for JAK2 V617F mutation is enough to constitutively activate megakaryocytes, due to increased sensitivity to TPO, in order to induce the clinical ET phenotype (26-29). The JAK2 mutated platelets are constitutively activated, hypersensitive and sticky platelets as the cause of platelet-mediated aspirin-responsive Sticky Platelet Syndrome (Table 4) (23-25). According to the “dosage” hypothesis the level and duration of JAK2 V617F directly contribute to the phenotypic diversity of JAK2 V617F mutated EMGM manifestations (Table 4). This hypothesis is based on different densities of TPO receptors (TPOR) and EPO receptors (EPOR) on hematopoietic progenitor cells and on differences of response of TPOR and EPOR to various levels of JAK2 V617F activity (26,27). MPL is expressed at high levels in megakaryocytic cells where it controls physiological TPO levels. It is possible that activation of TPO receptors by low levels of heterozygous JAK2 V617F is sufficient to send a signal to megakaryocytic cells (13,16,28) (Table 4). Conversely, EPOR is expressed at low levels on hematopoietic progenitor cells and therefore high levels of JAK2 V617F in homozygous mutated progenitor cells is required to spontaneously activate EPOR and generate a PV-like phenotype with increased erythrocytes above the limit of normal (Table 4) (25-28).
Sustained high levels of homozygous JAK2 V617F mutation during long-term follow-up subsequently does lead to a high spontaneous activation level EPOR and GCSF receptor (GCSFR), which is associated with to extramedullary myeloid neoplasia in the spleen (MNS), splenomegaly and cytokine mediated secondary myelofibrosis (Table 4). The percentage of JAK2 V617F positivity and progression from heterozygous to homozygous is strongly correlated with the ability to form spontaneous EEC formation (the hallmark of PV) and with progressive post-PV myelofibrosis (Figure 6) (21,28,29).
Godfrey et al studied in more detail the genotype of individual BFU-E in 29 JAK2 V617F mutated ET and 30 JAK2 V617F mutated PV patients expressed as percentage (%) of EEC colonies genotyped as homozygous (red), heterozygous (purple) or wild type (white in Figure 7) (30). All 29 JAK2 V617F positive ET patients have heterozygous JAK2 mutated EEC colonies and a low percentage less than 10% homozyous colonies in 9 and 20% in 1 of them. Out of 30 JAK2 V617F positive PV patients 8 have heterozygous JAK2 mutated EEC, 13 have homozygous EEC colonies of more than 50% and 7 of less than 50% (Figure 7). To determine whether JAK2 V617F homozygous colonies were part of a single clone or reflected recurrent acquisition of loss of heterozygosity (LOH), breakpoints for chromosome 9p LOH were mapped using fluorescence microsatellite PCR in 576 homozygous mutant colonies from 10 patients (8 PV and 2 ET). Homozygous mutant colonies were absent or present in low percentages in heterozygous ET, but prevalent and common in patients with JAK2 V617F -positive PV (30). In this small number of patients, PV patients harbored a major homozygous-mutant clone that was 8-85 times the size of minor subclones in the same patient. This observation demonstrates that the large numbers of homozygous mutant colonies present in most PV patients do not reflect accumulation of numerous independent subclones but rather the expansion of one dominant clone. The selective expansion of one dominant homozygous subclone is likely to reflect additional cytogenetic (31), genetic or epigenetic alterationsin ET, PV and MF patients (32,33). Such acquired additional epigenetic background biological factors on top of the JAK2, MPL and CALR driver mutations of MPN are associated with impaired prognosis and will become of huge importance for the understanding of differences in biology, prognosis and outcome (34,35).
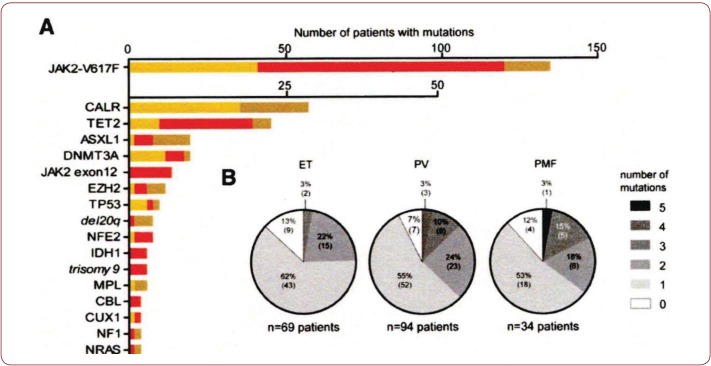
Using next generation sequencing (NGS), Lundberg et al found that 28 of 104 (27%) of genes analyzed were mutated in at least 1 (JAK2 or CALR) of the 197 MPN patients (94 PV, 69 ET, 34 MF) (Figure 8) (35). The JAK2 V617F mutation was recorded in 2008 WHO defined ET, PV and PMF patients and CALR mutation was recorded in ET and PMF patients and not in PV. Seventeen of 69 (25%) ET patients and 11 of 34 (32%) MF patients carried mutations in CALR. After JAK2 V617F and CALR, the most frequently observed mutations affected genes implicated in epigenetic regulation (TET2, ASXL1, DNMT3A, EZH2, and IDH1, Figure 8). JAK2 V617F mutation was recorded in ET, PV and PMF patients and CALR mutation was recorded in ET and PMF patients and not in PV. Rare mutations include NF1, NFE2, and CUX1. Recurrent somatic mutations were observed in the genes TP53, CBL, MPL, and NRAS. Nonrecurrent mutations were detected in 16 other genes. Overall, 20 of 197 patients (10%) had no detectable somatic mutation in any of the genes analyzed (9 ET, 7 PV, and 4 PMF). Besides the JAK2 or CALR mutations, one, two or more somatic mutations were found in 65 of 197 (33%) patients, which appeared to be of impaired prognostic significance (35).
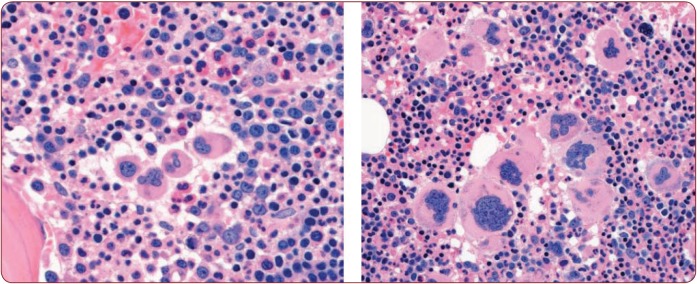
Figure 5.
Figure 5. WHO bone marrow features in JAK2 V617F positive ET cases 2, 3, 4, 5 and 6, and PV case 7.
Case 2. Clinically JAK2 V617F positive ET 2 (low serum EPO) and a normocellular ET (WHO-ET) bone marrow wit pleomorph small and large megakaryocytes and reticulin fibers: RF grade 1.
Case 3 and 4. Clinically JAK2 V617F positive ET 2 with a trilinear hypercellular PV bone marrow and RF 0 in case 2 and increased cellularity due to increased erythropoiesis in case 4, and no increase of reticulin fibers: RF grade 0.
Case 5. Clinically JAK2 V617F positive ET with slight to moderate splenomegaly and a hypercellular megakaryocytic granulocytic myeloproliferation (EMGM = ET 3), with dysmorphic megakaryocytes (not cloud-like) and no increase of reticulin fibers: RF grade 0 in the bone marrow.
Case 6. Clinically JAK2 V617F positive ET 2 with a trilinear hypercellular PV bone marrow picture and no oncrease of reiculinefibers: RF 0.
Case 7. Clinically JAK2 V617F positive PV with a 65% hypercellular ET/PV bone marrow picture in between “normocellular ET” (WHO-ET) and trilinear hypercellular (100%) PV picture.
Table 6.
Table 6. Grading of bone marrow biopsy content of secondary reticulin fibrosis (RF), and WHO grading of myelofibrosis (MF) (6-9,29,50,51).
Figure 6.
Figure 6. Relationship of splenomegaly and MPN disease duration to the JAK2 mutation status of burst forming uniterythropiesis (BFU-E) clonal genotypes in 6 ET, 14 PV and 6 MF patients (21). Progression of heterozygous JAK2 V617F mutation load from about 25% to 100% is seen in ET, PV and MF during longterm follow-up of 10 to 20 years. The mutation load of combined hetero/homozygous JAK2 V617 muated PV in 10 cases of PV was around 25% to 50% in early stage PV and increases to 80% to 100% in advanced myeloproliferative stages (splenomegaly) of PV and post-PV myelofibrosis (21).
Table 7.
Table 7. 2016 WHO-CMP criteria for hypercellular ET associated with primary megakaryocytic, granulocytic myeloproliferation (PMGM) caused by calreticulin (CALR) mutations (8,9).
The combination of A1 + A2 and P1 establishes CALR ET and various clinical stages (C1, C2,C3) related to the degree of myelofibosis (MF).
Figure 7.
Figure 7. Proportions of JAK2 genotypes in BFU-Es from 59 patients with JAK2-mutated essential thrombocythemia (ET) and polycythemia vera (PV) (30). Each vertical bar represents 1 patient, divided according to the proportion of wild-type, heterozygous and homozygous-mutant colonies obtained, with the absolute colony numbers shown above: (wild type white), heterozygous (purple) homozygous (red). Results EEC colony genotypes are presented for 29 JAK2 V617F -positive ET patients (total 2277 colonies; mean 79 per patient) and for 30 JAK2 V617F -positive PV patients (total 2287 colonies; mean 76 colonies per patient) (30). All 29 JAK2 V617F positive ET patients have heterozygous JAK2 mutated EEC colonies and a low percentage less than 10% homozyous colonies in 9 and 20% in 1 of them. Out of 30 JAK2 V617F positive PV patients 8 have heterozygous JAK2 mutated EEC, 13 have homozygous EEC colonies of more than 50% and 7 of less than 50%.
Figure 8.
Figure 8. Distribution of somatic mutations in 197 MPN patients from the study of Lundberg et al. (35). None of 94 (%) PV patients, 17 of 69 (25%) ET patients and 11 of 34 (32%) MF patients carried mutations in the caleticulin (CALR) gene. After JAK2 V617F and CALR, the most frequently observed mutations affected genes implicated in epigenetic regulation (TET2, ASXL1, DNMT3A, EZH2, and IDH1. Rare epigenetic mutations include NF1, NFE2, and CUX1. Recurrent somatic mutations were observed in the genes TP53, CBL, MPL, and NRAS. On top of the JAK2 or CALR mutation one, two or more somatic mutations were found in 65 of 197 (33%) patients, which appeared to be of impaired prognostic significance (35).
Table 8.
Table 8. 2016 WHO Clinical Molecular andPathological (2016 WHO-CMP) criteria for the diagnosis of normocelular ET carrying one of the MPL mutations (8,9).
Figure 9.
Figure 9. Bone marrow histology in PV patients with JAK2 exon 12 mutations meeting the criteria for idiopathic erythrocythemia (IE) and classical PV, showed prominent erythroid hyperplasia and clustered atypical small to medium-sized large megakaryocytes with various degrees of monolobation to hyperlobation and abnormal chromatin distribution (Lakey et al. [40]).
Figure 10.
Figure 10. Hemorrhagic thrombocythemia in case of JAK2 wild type hypercellular ET associated with prefibrotic primary megakaryocytic and granulocytic myeloproliferation (PMGM, colour picture) in the bone marrow by dual myeloproliferation of granulopoiesis and dense clustered enlarged immature dysmorphic megakaryocytes with bulky (bulbous) hyperchromatic nuclei (arrows), which are never seen in JAK2 wild type MPL mutated ET and also not in the prefibrotic JAK2 V617F mutated ET. During long-term follow-up, reduction of platelet count to normal or near normal by treatment with hydroxyurea in 1994 followed by anagrelide from 1995 to 1998 the bleeding manifestations did not recur. After discontinuation of anagrelide in 1998 the patient remained asymptomatic, the platelet counts were between 600 and 800x109/L, which normalized after 8 years of follow-up. From 2001 to 2005 haemoglobin and hematocrit reached completely normal values.
Prospective evaluation of WHO-CMP criteria in JAK2 V617F mutated MPN
The 2013-2015 WHO-ECMP classifications defined three phenotypes of JAK2 V617F mutated ET: normocellular ET, hypercellular ET due to increased erythropoiesis (prodromal PV) and ET with hypercellular megakaryocyticgranulocytic myeloproliferation (EMGM or masked PV (Table 1) (6-9).The updated 2016 WHO-CMP for the diagnosis of PV (Table 2) and subsequent staging of PV distinguished at least 6 stages that has important therapeutic implications (Table 5) (7-9). Bone marrow cellularity, increased erythropoiesis or granulopoisis and the morphology of pleomorphic megakarocytes are not different in JAK2 V617F mutated ET, prodromal PV, masked PV and classical PV (Figure 5). Normocellular ET had stable ET disease without any progression during life long follow-up. WHO defined ET patients frequently had a typical hypercellular PV bone marrow picture due to increased erythropoiesis similar as observed in newly diagnosed PV patients (Figures 2 and 6) (7-9,21). JAK2 V617F mutated pure erythrocythemia or idiopathic erythrocytosis according to PVSG criteria presented with a typical PV bone marrow histology and persistant increased erythrocyte counts above 6×1012/L (Figure 4). After correction of Hb and Ht to around 40% by repeated venessections (Figure 4), the erythrocyte counts remained above 6×1012/L, whereas the JAK2 V617F mutation load increased in this case rose from heterozygous 25% to homozygous 65% after 5 years follow-up.
Detection of JAK2 V617F mutation and serum EPO measurement have become the first step in the diagnostic work-up of erythrocytosis with erythrocyte counts above the upper limit of normal (>5,6×1012/L) (36-38). Vannucchi et al employed quantitative assays for JAK2 V617F allele levels in granulocytes in a prospective study of 175 PV patients at time of diagnosis (18). The JAK2 mutant allele burden could be quantified as 1-25%, 25% to 50%, 50%-75% and 75%-100% in 57, 50, 34 and 32 PV patients respectively at time of investigation (18). The burden of JAK2 V617F allele was directly correlated with abnormally increased levels of hematocrit, white cell and neutrophil count, LDH and LAP score, spleen size on echogram and with decreased values for serum ferritin, and erythropoietin (18). The JAK2 V617F mutation load correlated with a progressively higher relative risk for aquagenic pruritus, spleen size on echogram, total thrombosis and the need for receiving myelosuppressive agents (hydroxyurea).
Figure 11.
Figure 11. Clinical case of calcireticulin (CALR) positive ET who present with aspirin responsive platelet thrombophilia, normal vlaues for hemogobin, hematocrit and erythrocytes, platelet count of 1352x109/L and slight splenomegaly (16 cm lenght diameter on echogram). Bone marrow histology is hypercellular with relative decrease of erythropoisis, dense cluster of immature megakaryocytes with hypolobulated nu clei consistent, and no increase of reticulin fibrosis consistent with a typical PMGM bone marrow (Table 7).
Figure 12.
Figure 12. Clinical case of CALR positive myelofibrosis (MF): hemoglobin 11.2 g/dL, hematocrit 0.33, leukocytes 9.2x109/L, platelets 347x109/L, LDH 1393 U/l, and the presence of tear drop erythrocytes, poikolocytosis and polychromasie in a peripheral bloodsmear, and hypercellular bone marrow with relative decrease of erythropoisis, dense cluster of immature megakaryocytes with hypolobulated nuclei consistent, and reticulin fibrosis grade 2 consistent with a PMGM bonemarrow (Table 7), clearly distinct from JAK2 V617F mutated ET and PV, and distinct from MPL mutated ET (Figure 13).
JAK2 exon 12 mutations as cause of idiopathic erythrocythemia and PV
The frequency of JAK2 exon 12 mutations among all patients with PV is estimated around 3%(38-40). JAK2 N542-E543del is the most frequent among the different reported exon 12 mutations. The finding of the JAK2 exon 12 mutations in the 5% PV patients negative for JAK2 V617F usually present with early stage PV or idiopathic erthrocytosis (idiopathic erythrocythemia (IE) = increased red cell mass with normal values for leukocytes and platelets and no palpable spleen) with a favourable outcome and normal life expectancy (38-40). In JAK2 exon 12-mutated PV homozygous clone were absent or the sizes were small and very likely explain he benign course of the MPN disease. A low percentage of homozygosity for the exon 12 mutation was observed in both K539L-type and E543del-type mutations. The relative high proportions of heterozygous mutant colonies were stable over time in 16 patients tested on 2 separate occasions. Pre-treatment bone marrow histology in JAK2 exon 12 mutated PV or IE showed characteristic erythroid hyperplasia with minor and distinct histology changes of the megakaryocyte lineage. JAK2 exon 12 mutated PV were frequently diagnosed as IE with increased Hb, Ht and RCM, low serum EPO, but normal Plt and leukocyte counts, no or palpable spleen. The bone marrow histology is hypercellular predominantly due to erythroid hyperplasia and clusters of large megakaryocytes with hyperploid nuclei (38-40). Bone marrow pathology of the JAK2 exon 12 PV cases lacked the prominent clustering of large megakaryocytes and revealed a spectrum of small to medium sized megakaryocyte with a predominance of smaller forms with a varying degree of lobation comprising monolobulated and hyperlobulated forms (Figure 9) (40).
Figure 13.
Figure 13. Comparison of JAK2 V617F mutated ET versus MPL mutated normocellular ET: 65 years old man with RBC 5.37x1012/L, HB 15.8 g/dL, MCV 89, WBC 11.95 x109/L, Plts 517x109/L, LDH 600 UI/L and JAK2 V617F mutation (allele burden: 20% on peripheral blood). Diagnosis JAK2 V617F mutated prodromal PV according WHO-ECMP (left). 55 years old woman with MPL-positive normocellular ET with normal values for hemoglobin, hematocrit, leukocytes and platelet around 1000x109/L associatedwith small medium, large and giant megakaryocytes with staghorn-like hyperlobulated nuclei (right).
CALR mutated Thrombocythemia and MF
Two MPN research groups independently discovered in 2013 the calreticulin (CALR) mutations in JAK2/MPL wild type MPN patients (41-43). Dr Kralovics and his team in Vienna Austria detected calreticulin (CALR) somatic mutations in 78 of 311 (25%) ET patients and in 72 of 203 (35%) MF patients and in none of 382 PV patients (41). The somatic CALR mutation was not found 45 CML, 73 MDS, 64 chronic myelomonocytic leukemia (CMML) and 24 RARS-T patients except that 3 SF3B1 positive RARS-T patients carried a CALR mutation. Among 1235 ET and MF patients in the Italian-Austrian study, 63.4%, 4.4% and 23.5% carried the JAK2 V617F, MPL and CALR mutations respectively, and in 8.8% none of these clonal markers (triple negative) was detected (42). Evolution into MF during very long term follow up was equallly high in CALR mutated ET as in JAK2 mutated PV (about 20% after 20 years follow up). CALR mutated MPN patients had higher platelet counts, normal to low normal hemoglobin and white blood cells counts and a lower incidence of major thrombotic events simple because it lacks PV features (41,42). The UK study found somatic CALR mutations in 110 of 158 JAK2 and MPL wild type MPN, including 80 of 112 (70%) ET patients, 18 of 32 (56%) MF patients (43). CALR exon 9 mutations were found in 26 of 31 (84%) patients with JAK2/MPL wild type MF. CALR exon 9 mutations were absent in all 120 JAK2 or MPL mutated patients. CALR mutations were present in 10 of 120 (8%) MDS patients (RA in 5 of 53, RARS in 3 of 27 and RAEB-T in 2 of 27), and in one patient each with CMML and atypical CML. No CALR mutations were found in control samples, lymphoid cancers, solid tumors, or cell lines.
In the American study of 254 evaluable WHO-defined MF patients the JAK2-, MPLand CALR-mutations were present in 58%, 8.3% and 25% respectively, and 8.7% were triple negative (44). Median overall survival (OS) durations of 83 CALR-, 21 MPL-, and 147 JAK2-mutated MF cases and in 22 triple negative MF cases were 8.2, 4.1, 4.3 and 2.5 years respectively. As compared to JAK2 mutated MF, CALR-mutated MF patients were younger, had higher platelet count, lower leukocyte count, were less anemic with lower DIPSS-plus score. The median overall survival was 2.3 years in 55 CALR-negative/ASLX1-positive, 5.6 years in 126 CALR-negative/ASXL1-negative MF patients, 7 years in 20 CALR-positive/ASXL1-positive MF patients and 9.6 years in 126 CALRpositive/ ASXL1-negative MF patients (44).
Figure 14.
Figure 14. World Health Organisation (WHO) clinical, molecular and pathological (2016 WHO-CMP) translational states of Myeloproliferative Neoplasms (MPN) Classification of at least four distinct clonal JAK2 V617F, JAK2 exon 12, CALR, MPL mutated MPNs.
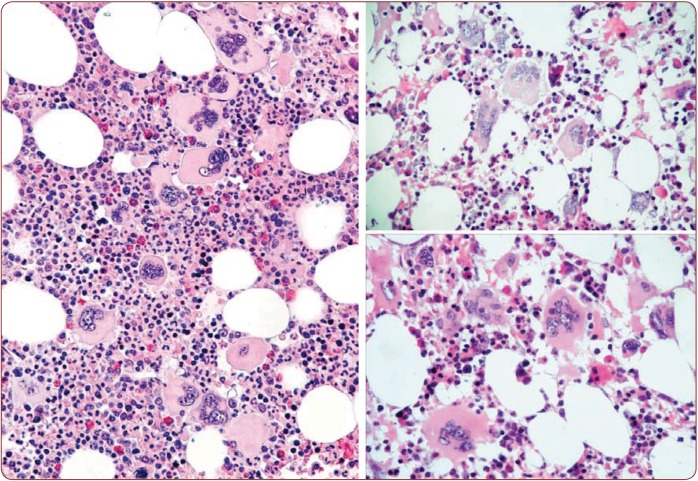
Bone marrow pathology of CALR mutated Thrombocythemia and MF
From 1994 to 2006, we documented a case of JAK2 wild type ET with a PMGM bone marrow (Figure 10) in a 9-year-old boy (referred to us from Basel, Switzerland) with Plt of 1596 to 1946x109/l, no splenomegaly on palpation, white blood differential count (metamyelocytes 0.5%, banded forms 1%, segmented granulocytes 52%, basophiles 2.5%, lymphocytes 35% monocytes 6%), low LAP score, and a hypercellular (80-100%) bone marrow with a predominant prefibrotic primary megakaryocytic and granulocytic myeloproliferation (PMGM, table 7), absence of reticulin fibers, loose to dense clustering of large dysmorphic megakaryocytes variable in size with cloud-like hypoploid nuclei. The dysmorphic megakaryocytes show definite abnormalities of maturation with bulky (bulbous) hyperchromatic nuclei and some disturbances of the nuclear cytoplasmic ratio (Figure 10, arrows), which are not seen in JAK2 V617F mutated ET. The 10 years follow-up from 1994 to 2004 showed normal blood cells counts, absence of the JAK2 V617F mutation, no evidence of myelofibrosis, and no splenomegaly on palpation (Figure 10).
The bone marrow histology in 15 consecutive newly diagnosed CALR mutated ET and early MF in 2014/2015 revealed a typical FIGURE 14. World Health Organisation (WHO) clinical, molecular and pathological (2016 WHO-CMP) translational states of Myeloproliferative Neoplasms (MPN) Classification of at least four distinct clonal JAK2 V617F, JAK2 exon 12, CALR, MPL mutated MPNs. 2016 WHO CLINICAL MOLECULAR AND PATHOLOGICAL CRITERIA FOR CLASSIFICATION AND STAGING OF MYELOPROLIFERATIVE NEOPLASMS 22 Maedica A Journal of Clinical Medicine, Volume 11 No.1 2016 PMGM picture characterized by dysmorphic megakaryocytes with definite abnormalities of maturation with bulky (bulbous) hyperchromatic nuclei (Table7). Representative bone marrow histology findings of typical cases of CALR positive ET (Figure 11) and CALR positive MF (Figure 12) show dense cluster of immature megakaryocytes. The clinical presentation, laboratory and molecular findings has been confirmed in Belgium in 40 of 64 JAK2 wild type MPN (ET or MF) patients (45). This study extends the growing body of evidence that CALR thrombocythemia patients are phenotypically distinct from JAK2 V617F ET and prodromal PV cases with regard to clinical and hematological features at presentation and during follow-up.
Acquired MPL mutated normocellular ET
Three European studies describe MPL W515L and W515K mutations as the cause of clonal ET and myelofibrosis without features of PV(46-48). Within the JAK2 wild type MPN, the prevalence of the MPL mutations as the cause of ET is 3% in the Vannucchi study(46), and 8.5% in the UK studies (47,48). The clinical presentation in 30 ET patients with acquired MPL mutations (9 males and 21 females, age 22-84 (mean 56 years of whom 18 had the W515L and 12 the W515K) was featured by a high incidence of major arterial event in 23%, venous thrombosis in 10%, aspirin responsive microvessel disturbances in 60%, and major hemorrhage in 7% (46). The only abnormal laboratory finding in MPL mutated ET was increased Plt counts in all and slight splenomegaly in 5 (17%). On the other hand, Teffferi’s group from Mayo Clinic shown recently that MPL-mutated ET patients seem to be prone to secondary MF, on a large cohort of 495 patients with ET with annotated driver mutation status (eg JAK2 V617F, CALR and MPL). They also shown a higher thrombosis risk conferred by the MPL mutations (49). MPL mutated ET patients have no clinical, laboratory and bone marrow features of prodromal PV at diagnosis, do not evolve into overt PV during follow-up, have normal serum EPO, normal ferritin levels, absence of spontaneous endogenous erythroid colonies (EEC). The pretreatment bone marrow at time of diagnosis in a typical case of MPL mutated ET is featured by normocellular ET with pronounced megakaryopoiesis with large and giant megakarocytes and no increase of erythropoiesis (Figure 13). The comparison of bone marrow histopathology findings in patients with normocellular JAK2 V617F mutated ET versus JAK2 wild type ET carrying MPL mutations shown significant differences (8). The megakaryocytes in MPL mutated ET are larger with hyperlobulated staghorn-like nuclei as compared to the pleomorphic megakaryocytes morphology in JAK2 V617F mutated ET and PV (Figure 13, Table 8). There was local increase of erythropoiesis in areas of loose clustered pleiomorphic megakaryoctyes in JAK2 V617F mutated ET, but not in JAK2 wild type PT carrying the MPL mutation.
2016 WHO-CMP classification in the context of new 2016 WHO classification and staging of MPNs: Therapeutic implications
The 2016 WHO new classification of MPN bring some important changes (Barbui et al, 2015; Tefferi, 2016) (50,51). In the case of PV, there are three major criterion: Hb >16.5 g/dL (men) and >16 g/dL (women) or Ht >49% (men) and >48% (women); hypercellular bone marrow with trilineage growth (panmyelosis) with pleomorphic and mature megakaryocytes, and presence of JAK2 V617F mutation. A subnormal serum erythropoietin level represents the only minor criterion. The diagnosis of PV requires all three major criteria or the first two ones plus the minor criterion. The Hg and Ht thresholds were lowered in order to capture cases with masked PV, while subnormal erythropoietin could capture the rare PV cases not showing the JAK2 V617F mutation. In the case of ET, there are major criteria: Plt >450x109/L; bone marrow showing proliferation mainly of the megakaryocytic lineage with increased numbers of enlarged and mature megakaryocytes; no significant increase or left-shift in granulopoiesis or erythropoiesis; minor (grade 1) increase in reticulin fibers; not meeting WHO criteria for chronic myeloid leukemia (CML), PV, PMF, myelodysplastic syndromes (MDS) or other myeloid neoplasm; presence of JAK2, CALR or MPL mutations. There are two minor criteria, namely presence of another clonal marker and absence of evidence for reactive thrombocytosis. The diagnosis of ET requires all four major criteria or first three major criteria and one minor criterion. In the case of PMF, there are three major criteria: bone marrow showing megakaryocytic proliferation and atypia accompanied by reticulinor collagen fibrosis . grade 2; not meeting WHO criteria for CML, PV, PMF, MDS orother myeloid neoplasm; presence of JAK2, CALR or MPL mutations or presence of another clonal marker or absence of evidence for reactive reticulin fibrosis. There are five minor criterion: anemia; leukocytosis >11 x 109/L; palpable splenomegaly; increase in serum lactate dehydrogenase level; leukoerythroblastosis. The 2016 WHO classification establish for the first time separate diagnostic criteria for pre-fibrotic PMF (50,51). The most important difference between PMF and pre-fibrotic PMF is at the bone marrow level; in pre-fibrotic PMF, the bone marrow shows megakaryocytic proliferation and atypia accompanied by reticulin fibrosis . grade 1. It also shows increased marrow cellularity and granulocytic proliferation with often decreased erythropoiesis. The other major and minor criteria are the same as for PMF, except for the leukoerythoblastosis, which is not required to pre-fibrotic PMF. Diagnosing both PMF and pre-fibrotic PMF requires all three major criteria and at least one minor criterion. The new 2016 WHO classification of MPN highlights the importance of bone marrow examination. This becomes most important especially in the following two situations: distinguishing masked PV from ET and distinguishing pre-fibrotic PMF from ET.
The 2016 WHO-CMP classification (6- 9,52,53) matches in general the 2016 WHO new classification of MPN (50,51), but it provides more refined morphological criteria for distinguishing the subtypes and stages of MPN. The 2016 WHO-CMP classification and staging of patients with MPN will be very helpful in predicting and documenting prospectively the natural history of JAK2 V617F mutated ET, prodromal PV and PV patients (Tables 1 and 2), versus CALR mutated thrombocythemia (Table 7) and MPL mutated thrombocythemia (Table 8) (6-9,52,53.The primary involvement of basic researchers, laboratory scientists, molecular biologists and clinicians as well as pathologists are essential to document the natural history at the clinical molecular and bone marrow level to demonstrate that scrutinized and integrated clinical, laboratory, molecular and pathological approaches and intense communications amongst clinicians, molecular biologists and pathologists are warranted in prospective diagnostic and managements studies (Figure 14). The 2016 WHO-CMP criteria surely will have important implications in choosing proper targetedtreatment options for the management and prevention of thrombotic and bleeding complications and serious complications of progressive MPN disease burden in prodromal PV and overt PV (52,53). Proper staging of PV in terms of JAK2 V617F mutation load, and MPN disease burden including splenomegaly, constitutional symptoms including itching, bone marrow histology and grading of myelofibrosis is of huge importance since it has significant implications for a non-leukemogenic or the least potential leukemogenic treatment options in low, intermediate and high risk PV patients (Table 5) (9,52,53). A primary rigid venessection regimen aiming at a hematocrit around and below 40% seems to perform better than the target of <45% in males and <42% in females on top of low dose aspirin for the control of activated platelets in MPN. According to our extended experiences, this strategy in stage zero, 1 and 2 PV patients (Table 5) will reduce the cumulative incidence of minor and major thrombosis from above 50% to less than 2% per patient/year during long-term follow-up (52,53).
The rational for using IFN-Ą as the first-line treatment option in newly diagnosed PV-patients include its effectiveness to abate constitutional symptoms and to induce a complete remission (Table 5), thereby avoiding phlebotomy, iron deficiency and macrocytosis associated with hydroxyurea (52,53). Clinicians will be reluctant to postpone the use of hydroxyurea as long as possible or even life long in early stage PV (9,53). Two studies show IFN-induced complete hematological responses (CHR) within one year, and major molecular responses (MMR) were reached after a follow-up of 2 to 3 years in PV and ET patients (54,55). The cumulative incidence of MMR was 14% at 2 years and 30% at 4 years follow-up in one prospetive study (54). Peglyated IFN Ą-2a (PegasysR) reduced the median JAK2-allele burden from 45% to 5% in 37 PV patients in one study (54) and from 64% to 12% in a second study of 79 PV and ET patients (55). A complete molecular response (CMR) may be reached, which was associated with normalization of bone marrow histology (56). MPN patients and their physicians should be cautious and attentive since the use of pegylated IFN Ą-2a or2b may be associated with significant side effects in about one third of PV patients (54). Kiladjian and his team of investigators reported in 2015 on the response to pegylated IFN in 31 CALR mutated ET patients during a mean follow-up of 11.8 years (57,58). A hemotological response was achieved in all patients and the median CALR mutation allele burden significantly decreased from 41% at baseline to 26% after treatment. Only 2 CALR ET patients achieved a complete molecular response. In contrast, the percentage of CALR mutation was not significantly modified in CALR ET patients treated with hydroxyurea or aspirin only. The presence of additional mutations (TET2, ASXL1, IDH2 and TP53) was associated with only minor or no molecular resonses on CALR mutant clones. MPN patients on-responsive to IFN with progressive myeloproliferative disease, splenomegaly and constitutional symptoms are candidates for myelosuppressive (hydroxyurea) or myeloreductive (JAK2 inhibtors) treatment (Table 5). MF transformation of thrombocythemia in MPN of various molecular etiology has to be distinguished from the expansion of one dominant homozygous subclone, the selective advantage of which is likely to reflect additional cytogenetic, genetic or epigenetic lesions (Figure 8). Such additional, acquired background biological factors on top of the JAK2, MPL and CALR driver causes of MPN will become of huge importance for the understanding of differences in prognosis, evolution and treatment outcome of thrombocythemia and polycythemia patients.
Conflict of interests: none declared.
Financial support: none declared.
Contributor Information
Jan Jacques Michiels, International Hematology and Bloodcoagulation Research Center, Goodheart Institute and Foundation in Nature Medicine, and International Collaboration and Research on Myeloproliferative Neoplasms: ICAR.MPN, Rotterdam, The Netherlands; Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
Mihaela Tevet, Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
Adrian Trifa, Department of Medical Genetics, “Iuliu Hatieganu”, University of Medicine and Pharmacy, Cluj-Napoca, Romania; Department of Genetics, “Ion Chiricuta” Cancer Institute, Cluj-Napoca, Romania.
Emilia Niculescu-Mizil, Provita Diagnosis and Treatment Center, Bucharest, Romania.
Anca Lupu, Department of Hematology, “Carol Davila” University of Medicine, Coltea Clinical Hospital, Bucharest, Romania.
Ana Maria Vladareanu, Department of Hematology, “Carol Davila” University of Medicine, Emergency Hospital, Bucharest, Romania.
Horia Bumbea, Department of Hematology, “Carol Davila” University of Medicine, Emergency Hospital, Bucharest, Romania.
Anca Ilea, Ritus Biotec Laboratory, Codlea, Brasov, Romania.
Camelia Dobrea, Department of Hematology, “Carol Davila” University of Medicine, Fundeni.
Daniela Georgescu, Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
Oana Patrinoiu, Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
Mihaela Popescu, Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
Meilin Murat, Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
Cornel Dragan, Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
Felicia Mihai, Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
Sabina Zurac, Department of Pathology, “Carol Davila” University of Medicine, Colentina Hospital, Bucharest, Romania.
Silvana Angelescu, Department of Hematology, “Carol Davila” University of Medicine, Coltea Clinical Hospital, Bucharest, Romania.
Anamaria Iova, Morphology Laboratory, Gral Laboratory, Bucharest, Romania.
Alina Popa, Morphology Laboratory, Gral Laboratory, Bucharest, Romania.
Rodica Gogulescu, Morphology Laboratory, Gral Laboratory, Bucharest, Romania.
Violeta Popov, Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania.
REFERENCES
- Dameshek W, Henstell HH - The diagnosis of polycythemia. Ann Intern Med. 1940;13:1360–1387. [Google Scholar]
- Dameshek W - Physiopathology and corse of polycythemia vera as related to therapy. JAMA. 1950;142:790–797. doi: 10.1001/jama.1950.02910290018005. [DOI] [PubMed] [Google Scholar]
- Michiels JJ - Physiopathology, etiologic factors, diagnosis and course of polycythemia vera as related to therapy according to William Dameshek 1940-1950. Turkish J Hematol. 2013;30:102–110. doi: 10.4274/Tjh.2013.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dameshek W - The treatment of Polycythemia. Blood. 1946;1:256. [Google Scholar]
- Dameshek W - Some speculations on the myeloproliferative syndromes. Blood. 1951;6:372–375. [PubMed] [Google Scholar]
- Michiels JJ, Berneman Z, Schroyens W, et al. - PVSG andWHO vs European Clinical, Molecular andPathological (ECMP) criteria for prefibrotic myeloproliferative neoplasms. World J Hematol. 2013;2:71–88. [Google Scholar]
- Michiels JJ, Ten kate F, Lam KH, et al. - The European clinical, molecular and Pathological (ECMP) criteria and the 2007/2008 revision of the worldHealth Organization fort he diagnosis, classfication and staging of prefibrotic myeloprloiferative neoplasms carryig the V617F mutation. Turk J Hematol. 2014;31:239–254. [Google Scholar]
- Michiels JJ, Berneman Z, Schroyens W, et al. - Changing concepts of diagnostic criteria of myeloproliferative disorders and the molecular etiology and classification of myeloproliferative neoplasms: From Dameshek 1950 to Vainchenker 2005 and beyond. Acta Haematol. 2015;133:71–86. doi: 10.1159/000358580. [DOI] [PubMed] [Google Scholar]
- Michiels JJ, Valster F, Wielenga J, et al. - European vs 2015 World Health Organization clinical molecular and pathological classification of myeloproliferative neoplasms. World J Hematol. 2015;4:16–53. [Google Scholar]
- - 2001 WHO classification of the chronic myeloproliferative diseases (CMPD) polycythemia vera, chronic idiopathic myelofibrosis essential thrombocythemia and cMPD unclassifiable. In: Jaffe SS, Harris NL, Stern A, Vardiman JW eds. WHO classification of Tumours of haematopoiesis and lymphoid tissues. Lyon, France IARC; 2001;31:42. [Google Scholar]
- Tefferi A, Thiele J, Orazi A, et al. - Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood. 2007;110:1092–1097. doi: 10.1182/blood-2007-04-083501. [DOI] [PubMed] [Google Scholar]
- - 2008 WHO criteria for polycthemia vera, primary myelofibrosis and essential thrombocythemia. Thiele et al In: Swerdlow SH, Campo E, Harris NL et al: WHO Classification of Tumours of Haematopoietic and Lympoid Tissues. Lyon France IARC Press. 2008;40:50. [Google Scholar]
- James C, Ugo V, Le Couédic JP, et al. - A unique clonal JAK2 mutation leading to constitutive signalling causes polycythemia vera. Nature. 2005;434:1144–1148. doi: 10.1038/nature03546. [DOI] [PubMed] [Google Scholar]
- Vainchenker W, Constantinescu SN - A unique activating mutation in JAK2 V617F is at the origin of polycythemia vera and allows a new classification of myeloproliferative diseases. Hematology (Am Soc Hematol Educ Progr) 2005;195:200. doi: 10.1182/asheducation-2005.1.195. [DOI] [PubMed] [Google Scholar]
- Baxter EJ, Scott LM, Campbell PJ, et al. - Acquired mutation of the tyrosine kinase in human myeloproliferative disorders. Lancet. 2005;365:1054–1061. doi: 10.1016/S0140-6736(05)71142-9. [DOI] [PubMed] [Google Scholar]
- Michiels JJ, Berneman Z, Van Bockstaele D, et al. - Clinical and laboratory features, pathobiology of platelet-mediated thrombosis and bleeding complications and the molecular etiology of essential thrombocythemia and polycythemia vera: therapeutic implications. Sem Thromb Hemostas. 2006;32:147–207. doi: 10.1055/s-2006-939431. [DOI] [PubMed] [Google Scholar]
- Antonioli E, Guglielmelli P, Pancrazzi A, et al. - Clinical implications of the JAK2 V617F mutation in essential thrombocythemia. Leukemia. 2005;19:1847, 1849. doi: 10.1038/sj.leu.2403902. [DOI] [PubMed] [Google Scholar]
- Vannucchi AM, Antonioli E, Guglielmelli P, et al. - Prospective indentification of high-risk polycythemia vera patients based on JAK2 V617F allele burden. Leukemia. 2007;21:1952–1959. doi: 10.1038/sj.leu.2404854. [DOI] [PubMed] [Google Scholar]
- Passamonti F, Rumi E, Pietra D, et al. - Relation between JAK2 V617F mutation status, granulocyte activation, and constitutive mobilization of CD34+ cells into peripheral blood in myeloproliferative disorders. Blood. 2006;107:3676–3682. doi: 10.1182/blood-2005-09-3826. [DOI] [PubMed] [Google Scholar]
- Scott LM, Scott MA, Campbell PJ, Green AR - Progenitors homozygous for the V617F JAK2 mutation occur in most patients with polycythemia vera, but not essential thrombocythemia. Blood. 2006;108:2435–2437. doi: 10.1182/blood-2006-04-018259. [DOI] [PubMed] [Google Scholar]
- Moliterno AR, Williams DM, Isaacs MA, et al. - Phenotypic variability within the JAK2 V617F-positive MPD: roles of progenitor cell and neutrophil allele burden. Exp Hematol. 2008;36:1480–1486. doi: 10.1016/j.exphem.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale RE, Allen AJR, Nash MJ, et al. - Log-term serial analysis of X-chromosome inactivation patterns and JAK2 V617F mutant levels in patients with essential thrombocythemia show that minor mutant-positive clones can remain stable for many years. Blood. 2007;109:1241–1243. doi: 10.1182/blood-2006-06-029769. [DOI] [PubMed] [Google Scholar]
- Michiels JJ, Ten Kate FWJ, Vuzevski VD, et al. - Histopathology of erythromelalgia in thrombocythemia. Histopathology. 1984;8:669–678. doi: 10.1111/j.1365-2559.1984.tb02379.x. [DOI] [PubMed] [Google Scholar]
- Michiels JJ, Abels J, Steketee J, et al. - Erythromelalgia caused by plateletmediated arteriolar inflammation and thrombosis in thrombocythemia. Ann Intern Med. 1985;102:466–471. doi: 10.7326/0003-4819-102-4-466. [DOI] [PubMed] [Google Scholar]
- Michiels JJ, Bernaman Z, Schroyens W, et al. - Platelet-mediated thrombotic complications in patients with ET: reversal by aspirin, platelet reduction, and not by Coumadin. Blood CellsMol Dis. 2006;36:199–205. doi: 10.1016/j.bcmd.2005.12.021. [DOI] [PubMed] [Google Scholar]
- Delhommeau F, Pisani DF, James C, et al. - Oncogenic mechanism in myeloproliferative disorders. Cell Mol Life Sci. 2006;63:2939–2953. doi: 10.1007/s00018-006-6272-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villeval JL, James C, Pisani DF, et al. - New insights into the pathogenesis of JAK2 V617F-positive myeloproliferative disorders and consequences for the management of patients. Sem Thromb Hemostas. 2006;32:341–351. doi: 10.1055/s-2006-942755. [DOI] [PubMed] [Google Scholar]
- Passamonti F, Rumi E, Pietra D, et al. - Relation between JAK2 V617F mutation status, granulocyte activation, and constitutive mobilization of CD34+ cells into peripheral blood in myeloproliferative disorders. Blood. 2006;107:3676–3682. doi: 10.1182/blood-2005-09-3826. [DOI] [PubMed] [Google Scholar]
- Michiels JJ, Hendrik De Raeve, Berneman Z, et al. - The 2001 world health organization and updated european clinical and pathological criteria fort he diagnosis classification and staging of the Philadelphia-negative chronic myeloproliferative disorders. Sem Thromb Hemostas. 2006;32:307–340. doi: 10.1055/s-2006-942754. [DOI] [PubMed] [Google Scholar]
- Godfrey AL, Chen E, Pagano F, et al. - JAK2 V617F homozygosity arises commonly and recurrently in PV and ET, butPV is characterized by expansion of a dominant homozygous subclone. Blood. 2012;120:2704–2707. doi: 10.1182/blood-2012-05-431791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bench AJ, Nacheva EP, Champion KM, et al. - Molecular genetics and cytogenetics of myeloproliferative disorders. Bailiere’d clin Haematol. 1998;11:819–848. doi: 10.1016/s0950-3536(98)80041-3. [DOI] [PubMed] [Google Scholar]
- Gotlib J - JAK2 inhibition in the myeloproliferative neoplasms: lessons learned from the bench andbedsise. Heamatology ASH Education Book. 2013:529–537. doi: 10.1182/asheducation-2013.1.529. [DOI] [PubMed] [Google Scholar]
- Vannucchi A, Lasho TL, Guglielmelli P, et al. - Muatations and prognosis inprimarymyelofibrosis. Leukemia. 2013;27:1861–1869. doi: 10.1038/leu.2013.119. [DOI] [PubMed] [Google Scholar]
- Guglielmelli P, Lasho TL, Rotunno G, et al. - The number of prognostically detrimental mutations and prognosis in primary myelofibrosis: an international study of 797 patients. Leukemia. 2014;28:1494–1500. doi: 10.1038/leu.2014.76. [DOI] [PubMed] [Google Scholar]
- Lundberg P, Karov A, Nienbold R, et al. - Clonal evolution and clinical correlates of somatic mutations in myeloproliferative neoplasms. Blood. 2014;123:2220–2228. doi: 10.1182/blood-2013-11-537167. [DOI] [PubMed] [Google Scholar]
- James C, Delhommeau F, Marzac C, et al. - Detection of JAK2 V617F as a first intention diagnostic test for erythrocytosis. Leukemia. 2006;20:350–353. doi: 10.1038/sj.leu.2404069. [DOI] [PubMed] [Google Scholar]
- Tefferi A, Pardanani A – Mutation - Mutation screening for JAK2 V617F: when to order the test and how to interpret the results. Leukemia Res. 2006;108:3472–3476. doi: 10.1016/j.leukres.2006.01.004. [DOI] [PubMed] [Google Scholar]
- Scott LM, Tong W, Levine RL, et al. - JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med. 2007;356:459–460. doi: 10.1056/NEJMoa065202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardani A, Lasho TL, Finke C, et al. - Prevalence and clinicopathologic correlates of JAK2 exon 12 mutations in JAK2 V617F-negative polycythemia vera. Leukemia. 2007;21:1960–1963. doi: 10.1038/sj.leu.2404810. [DOI] [PubMed] [Google Scholar]
- Lakey MA, Pardani A, Hoyer JD, et al. - Bone marrow morphologic featuresin polycythemia vera with JAK2 exon 12 mutations. . Am J Clin Pathol. 2010;133:942–948. doi: 10.1309/AJCP3Z2AKUWRGTNM. [DOI] [PubMed] [Google Scholar]
- Klampf T, Gisslinger H, Harutyunyan AS, et al. - Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med. 2013;369:2379–2387. doi: 10.1056/NEJMoa1311347. [DOI] [PubMed] [Google Scholar]
- Rumi E, Pietra D, Ferretti V, et al. - JAK2 or CALR mutation status defines subtypes of essential thrombocythemia with substantially different clinical course and outcome. Blood. 2014;123:1552–1515. doi: 10.1182/blood-2013-11-539098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nangalia J, Massie CE, Baxter J, et al. - Somatic CALR Mutations in Myeloproliferative Neoplasms with Nonmutated JAK2. N Engl J Med. 2013;369:2391–2405. doi: 10.1056/NEJMoa1312542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tefferi A, Lasho TL, Finke CM, et al. - CALR vs JAK2 vs MPL-mutated or triple-negative myelofibrosis: clinical, cytogenetic and molecular comparisons. Leukemia. 2014;28:1472–1477. doi: 10.1038/leu.2014.3. [DOI] [PubMed] [Google Scholar]
- Al Assaf C, Van Obbergh F, Billiet J, et al. - Analysis of phenotype and outcome in essential thrombocythemia with CALR or JAK2 mutations. Haematologica. 2015;11:893–897. doi: 10.3324/haematol.2014.118299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vannucchi AM, Antonioli E, Guglielmelli P, et al. - Charateristics and clinical correlates of MPL515W >L/K mutation in essential thrombocythemia. Blood. 2008;112:844–847. doi: 10.1182/blood-2008-01-135897. [DOI] [PubMed] [Google Scholar]
- Beer PA, Campbell PJ, Scott LM - MPL mutations in myeloproliferative disorders: analysis of the PT-1 cohort. Blood. 2008;112:141–149. doi: 10.1182/blood-2008-01-131664. [DOI] [PubMed] [Google Scholar]
- Jones AV, Campbell PJ, Beer PA, et al. - The JAK2 46/1 haplotype predisposes to MPL-mutated myeloproliferative neoplasms. Blood. 2010;115:4517–4523. doi: 10.1182/blood-2009-08-236448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elala YC, Lasho TL, Gangat N, et al. - Calreticulin (CALR) variant stratified driver mutational status and prognosis in essential thrombocythemia. Am J Pathol. 2016 doi: 10.1002/ajh.24338. [DOI] [PubMed] [Google Scholar]
- Barbui T, Thiele J, Vannucchi AM, Tefferi A - Rationale for revision and proposed changes of the WHO diagnostic criteria for polycythemia vera, essential thrombocythemia and primary myelofibrosis. Blood Cancer J. 2015;14:e337. doi: 10.1038/bcj.2015.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tefferi A - Myeloproliferative neoplasms: A decade of discoveries and treatment advances. Am J Hematol. 2016;91:50–8. doi: 10.1002/ajh.24221. [DOI] [PubMed] [Google Scholar]
- Michiels JJ, Ten kate FWJ, Koudstaal PJ, et al. - Aspirin responsive platelet thrombophilia in essential thrombocythemia and polycythemia vera. World J Hematol. 2013;2:20–43. [Google Scholar]
- Michiels JJ - Myeloproliferative and thrombotic burden and treatment outcome of thrombocythemia and polycythemia patients. World J Crit Care Med. 2015;4:230–239. doi: 10.5492/wjccm.v4.i3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiladjian JJ, Cassinat B, Turlure P, et al. - High molecular response rate of polycythemia vera treated with peglyated interpheron-alpha-2a. Blood. 2006;108:1281. doi: 10.1182/blood-2006-03-009860. [DOI] [PubMed] [Google Scholar]
- Quintas-Cardama A, Kantarjian H, Manshouri T, et al. - Peglyated interferon alfa-2a yields high rates of hematological and molecular response in patients with advanced essential thrombocthemia and polycythemia vera. J Clin Oncol. 2009;27:5418–5424. doi: 10.1200/JCO.2009.23.6075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larssen TS, Moeller MB, de Striker K, et al. - Minimal residual disease and normalization of the bone marrow after longterm treatment with alfa-interferon2b in polycythemia vera. A report on molecular responses in seven patients in sustained complete hematological remission. Hematology. 2009;14:331–334. doi: 10.1179/102453309X12473408860587. [DOI] [PubMed] [Google Scholar]
- Cassinat B, Verger E, Kiladjian JJ - Interferon alpha therapy in CALRmutated essential thrombocythemia. N Eng J Med. 2014;371:188–189. doi: 10.1056/NEJMc1401255. [DOI] [PubMed] [Google Scholar]
- Verger E, Cassinat B, Chauveau A, et al. - Clinical and moelucular response to interferon-alpha therapy in essential thrombocythemia patients with CALR mutations. Blood. 2015;126:2585–2691. doi: 10.1182/blood-2015-07-659060. [DOI] [PubMed] [Google Scholar]