Abstract
Introduction: Neonatal diabetes is a rare and surprising diagnosis, with many complications and difficult management by the medical team.
Objectives: Management of the diabetes mellitus new-born in our maternity.
Matherial and methods:Analysis of one of the rare cases of diagnosed neonatal diabetes.
Conclusions:Given the rarity of such cases, this event can guide the medical care team consisting of obstetricians, neonatologist and diabetes doctor to effective collaboration by protocol management of new-born with diabetes mellitus suspicion.
Keywords:newborn, diabetes mellitus, neonatal outcome
INTRODUCTION
Neonatal diabetes mellitus (NDM) is a monogenic form of diabetes, rare disease, one to 100.000 to 500.000 live births, which can occur in the first 6 months of life. Infants with NDM do not produce enough insulin, leading to an increase blood glucose (1).
In about half of those with NDM, the condition is lifelong and is called permanent neonatal diabetes mellitus (PNDM). In the rest, the condition is transient and disappears during infancy but can reappear later in life - transient neonatal diabetes mellitus (TNDM). Specific genes that can cause NDM have been identified (1).
Neonatal diabetes mellitus (NDM) is a rare (1:300,000–400,000 newborns) metabolic disorder characterized by hyperglycemia with low levels of insulin (2), affects all races and ethnic groups (3).
Neonatal diabetes is now understood to arise from mutations in genes that play critical roles in the development of the pancreas, of β-cell apoptosis and insulin processing and the regulation of insulin release (3).
The majority of the cases present intrauterine growth retardation (IUGR), failure to thrive, decreased subcutaneous fat, and low or undetectable C-peptide levels (4).
Diagnosis of “early-onset” diabetes can occur within the first days or months of life with hyperglycemia, in rare cases there are neural complications with a potential diagnostic problem witch is the differention of a monogenic cause vs. autoimmune type 1 diabetes in these children with early-onset diabetes (3). The combined data from the cases indicate that over half (~57%) of NDM are transient, require insulin treatment initially, and spontaneously resolve in less than 18 months, only to relapse in later years (3).
TNDM represents 50% to 60% of cases of neonatal diabetes, is a disorder of insulin production that resolves postnatally and there are no clinical features that can predict whether a neonate with diabetes (but no other dysmorphic features) will eventually have permanent or transient disease (2). In nonsyndromic permanent neonatal diabetes mellitus (PNDM) hyperglycemia appears within the first six months of life that and does not resolve over time. Clinical manifestations at the time of diagnosis include intrauterine growth retardation (IUGR), hyperglycemia, glycosuria, osmotic polyuria, severe dehydration, and failure to thrive (6).
CASE REPORT
AnWe report the case of a male new-born, from twin-born, delivered by c-section, cranial presentation, at the gestational age of 35 weeks, weighing 1500 g (intrauterine growth retardation, p<10%), from pregnancy obtained by in vitro fertilization, second twin.
At birth: Apgar Score 7, features of down syndrome - epicanthic eye-fold, hypertelorism, protruding tongue, small ears, cutis laxa, ogive palate, simian crease, gap between 1st and 2nd toes. It required initial care in neonatal intensive unit, with favorable evolution and paraclinical markers (laboratory, radiography, ultrasound transfontanelar) normal for gestational age, except blood glucose levels over 400 mg/ dl in repeated tests. The nutrition was initiated since the first hours of life with preterm formula and breast milk, but poor weight gain over time.
Diabetologist indicate the treatment with insulin at one month of life, under careful follow- up of glucose in blood and urine and clinical course. Genetic screening has decided on a karyotype.
Down’s syndrome is one of the common chromosomal disorders and the most common cause of mental retardation. It is well-known that this patients have an increased prevalence of autoimmune disorders affecting both endocrine and non-endocrine organs (15). Although cases of Down Syndrome associated with diabetes mellitus have been reported in the past, most of the cases were associated with type 1 diabetes mellitus, rarely with type 2 (16).
According to the neonatal protocols, although it started enteral nutrition with brest milk and parenteral nutrition in the first hours of life, in the absence of specific pathologies, weight gain was installed after a month of life, after the introduction of insulin treatment.
DISCUSSION
The role of insulin in fetal growth, especially during the last trimester of pregnancy is important in the high rate of IUGR. Insulin production is inadequate, requiring exogenous insulin therapy. Hyperglycemia, failure to thrive and, in some cases, dehydration occur after birth.
A defect in cell maturation has been suggested (7) with exocrine pancreatic insufficiency present in only a few patients (8).
Permanent hyperglycemia requiring insulin therapy developed in five of the seven TNDM patients who were older than 8 years of age in a French cohort (9). The "transient" form of the disease is probably a permanent β-cell defect with variable expression during growth and development. A major factor in the onset of recurrent diabetes is probably puberty, which is associated with significant insulin resistance.
We concluded that the majority of children with TNDM in remission have no evidence of β-cell dysfunction or insulin resistance in the fasting state. Measures of insulin response to intravenous glucose loading are often normal but suggestive of future recurrence if profoundly abnormal (10). Permanent neonatal diabetes mellitus is less common than the transient form, develops in the neonatal period and does not go into remission.
In an Italian study conducted in infants developing diabetes before the age of one year, a clear difference was demonstrated between those infants developing diabetes before the age of 180 days and those after. The children developing early diabetes had a very high presence of “protective” HLA alleles against classical type 1 diabetes (76% with 0 or 1 susceptibility heterodimers), compared to only 12% in the late (>180 days) onset group (11). In addition, autoimmune markers were far less prevalent in the early onset group of children compared to children with late onset diabetes (15% vs 65% if onset after 180 days) (2).
What we know so far about TNDM vs. PNDM: 1) Patients with TNDM are more likely to have intrauterine growth restriction than ketoacidosis; 2) TNDM patients are younger at the age of diagnosis of diabetes and have lower initial insulin requirements; 3) Cannot be distinguished based on clinical features; 4) Very early onset diabetes mellitus seems to be unrelated to autoimmunity 5) Recurrent diabetes is common in patients with “transient” neonatal diabetes mellitus and, consequently, prolonged follow-up is imperative; 6) Molecular analysis of chromosome 6 anomalies, the KCNJ11 and ABCC8 genes (encoding Kir6.2 and SUR1 respectively) provide a tool for identifying transient from permanent neonatal diabetes mellitus in the neonatal period; 7) About 50% of the PNDM cases are linked to potassium channel mutation which has potentially important therapeutic consequences leading to transfer some patients from insulin therapy to sulfonylureas (2).
Follow-up: Lifelong monitoring of blood glucose concentrations at least four times a day, periodic developmental evaluations and after age ten years, annual screening for chronic complications of diabetes mellitus including urinalysis for microalbuminuria and ophthalmologic examination for retinopathy (6).
There is a hypothesis according to which heterozygous activating mutations in the gene encoding Kir6.2 cause permanent neonatal diabetes and may also be associated with developmental delay, muscle weakness, and epilepsy. Identification of the genetic cause of permanent neonatal diabetes may facilitate the treatment of this disease with sulfonylureas (12). Oral sulfonylurea therapy is safe and effective in the short term in most patients with diabetes due to SUR1 mutations and may successfully replace treatment with insulin injections (13).
Insulin therapy and high caloric intake is important to obtain weight gain and growth in newborns with intra-uterine growth restriction. Although pediatricians face numerous difficulties in managing insulin therapy in the newborn period, very few data are available on the methods of insulin delivery in neonatal diabetes. In infants with transient neonatal diabetes mellitus, ultralente insulin treatment should be given (14). Insulin pump may offer an therapeutic tool in this age group only in experienced hands.
Realizing how difficult it is to take care of a child of this age with diabetes mellitus should prompt clinicians to transfer these children to specialized centers (2).
Genetic counselling should be considered in all the cases of infants with diabetes mellitus. The risk of recurrence is different according to the “transient” or permanent form of the disease and to the different molecular mechanisms identified (2).
In the neonatal period, the prognosis is linked to the severity of the disease, the degree of dehydration and acidosis, as well the rapidity with which the disease is recognized and treated; in the following period, the prognosis is determined by the associated malformations and lesions. Finally, the prognosis rely on the metabolic control, as in all the forms of diabetes mellitus, which will determine the timing of appearance of the long standing diabetes complications (2).
The particularity of the case is a rare occurrence of diabetes in pregnancy monitored (IVF). The clinical presentation of diabetes is the specific form described in the literature. The low birth weight and catch-up growth in NDM of genetic origin might increase insulin resistance and contribute to the later relapse in these children (3).
After birth, some ot this infants fail to thrive and do not grow as rapidly as other infants of the same age and sex, so appropriate therapy improves and may normalize growth and development (1). The pancreatic dysfunction may be maintained throughout life, with relapse initiated at times of metabolic stress such as puberty or pregnancy (5).
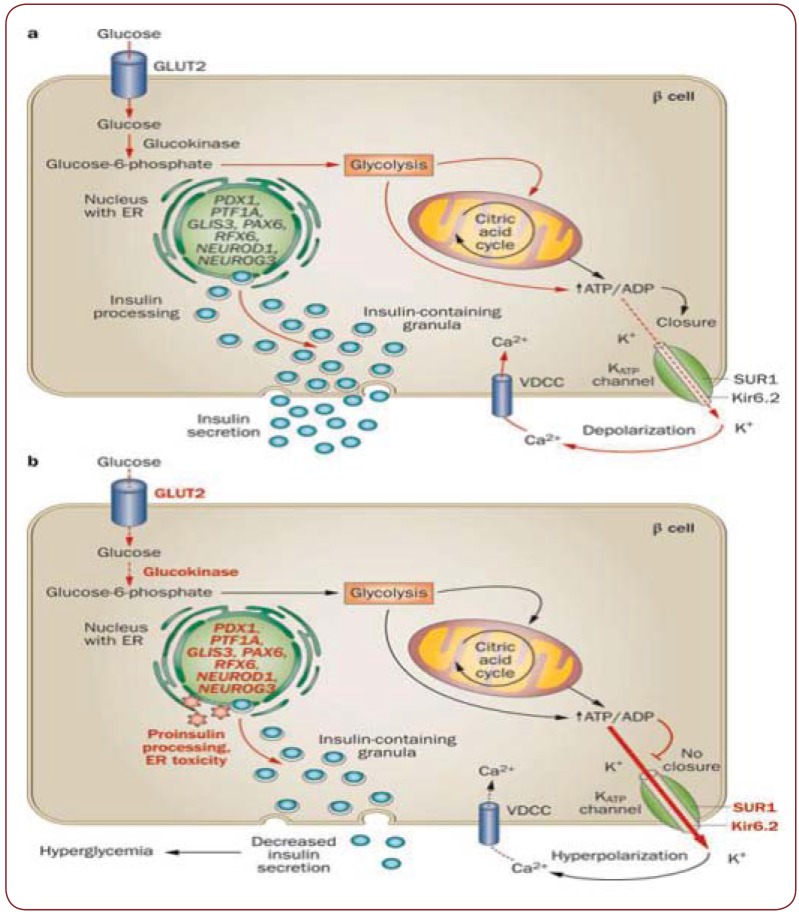
Figure 1.
Figure 1. Management of diabetes mellitus in infants - Beate Karges, Thomas Meissner, Andrea Icks, Thomas Kapellen & Reinhard W. Holl Nature Reviews Endocrinology 8, 201-211 (April 2012) doi:10.1038/nrendo.2011.204. A. Mechanisms of normal insulin secretion. B. Localization of genetic defects within the β cell and their effect on impaired insulin release.
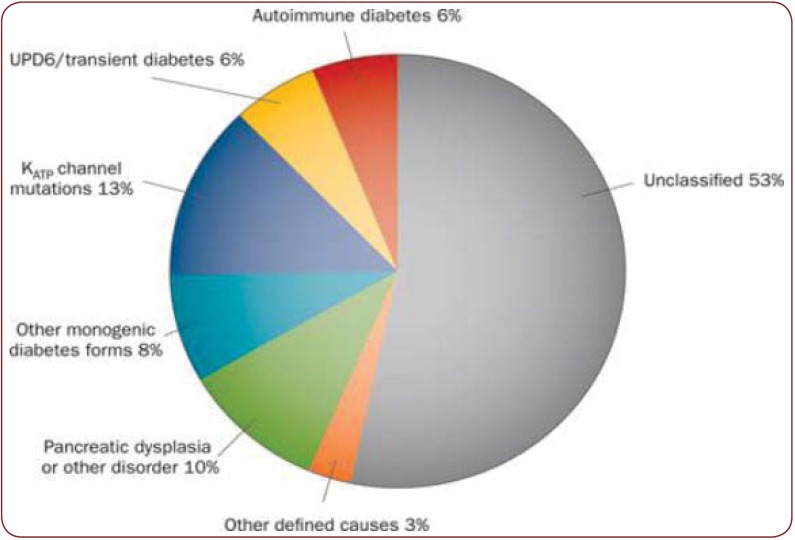
Figure 2.
Figure 2. Causes of neonatal diabetes mellitus with onset „T6 months of age (in percent of total) in 225 infants from the DPV cohort (period of 2000 - 2010). karges, B. et al. (2011) Management of diabetes mellitus in infants Nat. Rev. Endocrinol. doi: 10.1038/ nrendo.2011.204.
CONCLUSION
Neonatal diabetes mellitus require care by a multidisciplinary team (obstetrician, neonatologist, diabetologist, genetician).
Family counseling is a priority, considering the fact that it involves a careful follow-up and additional living costs.
After birth, some ot this infants fail to thrive and do not grow as rapidly as other infants of the same age and sex. Appropriate therapy improves and may normalize growth and development (1).
Conflict of interests: none declared.
Financial support: none declared.
Contributor Information
Ramona Mohora, Department of Neonatology, Polizu Maternity, Bucharest, Romania; ”Alfred Rusescu” Institute for Mother and Child Care, Bucharest, Romania.
Silvia-Maria Stoicescu, Department of Neonatology, Polizu Maternity, Bucharest, Romania; ”Alfred Rusescu” Institute for Mother and Child Care, Bucharest, Romania.
REFERENCES
- Monogenic Forms of Diabetes: Neonatal Diabetes Mellitus and Maturity-onset Diabetes of the Young at National Diabetes Information Clearinghouse, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. NIH Publication. 2007;07:6141–93. [Google Scholar]
- Polak M, Cavé H - Neonatal diabetes mellitus: a disease linked to multiple mechanisms. Orphanet J Rare Dis. 2007;2:12. doi: 10.1186/1750-1172-2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguilar-Bryan L, Bryan J - Neonatal Diabetes Mellitus. Endocr Rev. 2008;29:265–291. doi: 10.1210/er.2007-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fosel S - Transient and permanent neonatal diabetes. Eur J Pediatr. 1995;154:944, 948. doi: 10.1007/BF01958635. [DOI] [PubMed] [Google Scholar]
- Polak M - Cyclic vomiting syndrome in adults:clinical features and response to tricyclic antidepressents. http:// www.orpha.net/consor/cgi-bin/OC_ Exp.php?Lng=GB&Expert=224. 2007 doi: 10.1111/j.1572-0241.1999.01428.x. [DOI] [PubMed] [Google Scholar]
- De León D, Stanley C - Permanent Neonatal Diabetes Mellitus, GeneReviews. Internet. 2014;96:684–8. [Google Scholar]
- Ferguson AW, Milner RD - Transient neonatal diabetes mellitus in sibs. Arch Dis Child. 1970;45:80–83. doi: 10.1136/adc.45.239.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fosel S. - Transient and permanent neonatal diabetes. Eur J Pediatr. 1995;154:944–948. doi: 10.1007/BF01958635. [DOI] [PubMed] [Google Scholar]
- Metz C, Cavé H, Bertrand AM, et al. - Neonatal diabetes mellitus: chromosomal analysis in transient and permanent cases. J Pediatr. 2002;141:483–9. doi: 10.1067/mpd.2002.127089. [DOI] [PubMed] [Google Scholar]
- Shield JP, Temple IK, Sabin M, et al. - An assessment of pancreatic endocrine function and insulin sensitivity in patients with transient neonatal diabetes in remission. Arch Dis Child Fetal Neonatal Ed. 2004;89:F341–3. doi: 10.1136/adc.2003.030502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iafusco D, Stazi MA, Cotichini R, et al. - Permanent diabetes mellitus in the first year of life. Diabetologia. 2002;45:798–804. doi: 10.1007/s00125-002-0837-2. [DOI] [PubMed] [Google Scholar]
- Gloyn AL, Pearson ER, Antcliff JF, et al. - Activating mutations in the gene encoding the ATP-sensitive potassiumchannel subunit Kir6.2 and permanent neonatal diabetes. N Engl J Med. 2004;350:1838–49. doi: 10.1056/NEJMoa032922. [DOI] [PubMed] [Google Scholar]
- Rafiq M, Flanagan SE, Patch AM, et al. - Effective treatment with oral sulfonylureas in patients with diabetes due to sulfonylurea receptor 1 (SUR1) mutations. Diabetes Care. 2008;31:204–9. doi: 10.2337/dc07-1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitamura R, Kimura H, Murakami Y, et al. - Ultralente insulin treatment of transient neonatal diabetes mellitus. J Pediatr. 1996;128:268–270. doi: 10.1016/s0022-3476(96)70406-7. [DOI] [PubMed] [Google Scholar]
- Thyroid dysfunction in Down’s syndrome: Relation to age and thyroid autoimmunity. - Permanent diabetes mellitus in the first year of life. Arch Dis Child. 1998;79:242–5. doi: 10.1136/adc.79.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kota SK, Tripathy PR, Kota SK, Jammula S - Type 2 diabetes mellitus: An unusual association with Down’s syndrome. Indian J Hum Genet. 2013;19:358–359. doi: 10.4103/0971-6866.120818. [DOI] [PMC free article] [PubMed] [Google Scholar]