Abstract
Sweet’s Syndrome also knows as acute febrile neutrophilic dermatosis, is a rare skin’s condition, that can occur either idiopathic or secondary. In the case of the latter, the syndrome can develop after certain malignancies (paraneoplastic syndrome), because of exposure to some medication or post infectious.
It is more frequent in women aged between 30 and 50 years, but concerning children, the disorder is extremely rare (8% of the total number of cases), having equal sex ratio distribution.
We present the case of an 11 year old male, diagnosed with systemic form of SS associated with Myelodysplastic Syndrome. The onset of the hematological condition seemingly occurred at the age of 5, when the diagnosis of chronic immune thrombocytopenic purpura was established. The treatment included repeated cortisone administrations, followed by a splenectomy procedure.
Admitted in our Oncopaediatric department in December 2012, the child is given the diagnosis of MS, to which severe systemical manifestations of SS were added, with partial treatment response (cortisone, cyclosporine, dapsone, indomethacin).
An allogeneic bone marrow transplant was conducted at Fundeni Institute (February 2015) when the SS remission occurred, but the progression was fatal, the child developing graft-versus-host disease.
Keywords:Sweet’s Syndrome, Myelodysplastic Syndrome, Immune Thrombocytopenic Purpura, child
INTRODUCTION
Myelodysplastic Syndrome (MS) is a hematogenous bone marrow dysfunction. It is characterized by inefficient hematopoiesis, with normal or hypercellularity, resulting in various degrees of peripheral cytopenia and a variable risk of acute leukemic transformation most likely in myeloblastic forms (1).
Sweet’s Syndrome (SS) or febrile neutrophilic dermatosis, first described in 1964 by Robert Sweet, is characterized by abrupt onset and recurrent symptoms as: extremely painful and tender nodules or papules, accompanied by high fever, peripheral leukocytosis and neutrophilic infiltrate, with rapid response to topical and systemic corticosteroids. SS can either be idiopathic, pregnancy induced, following certain medication treatments (antibiotics, antiepileptic drugs, cytokines, oral contraceptives, retinoids, granulocyte stimulating factors), associated with infections or with malignancies (paraneoplastic syndrome, frequently in acute myeloblastic leukemia) (2).
In children this condition is very rare, having equal sex ratio distribution, with the youngest diagnosed patient being seven weeks of age (3).
The diagnosis criteria established by Su and Liu in 1986, later modified by Von den Driesch in 1994, include the following:
a. Major criteria:
Sudden onset with extremely painful erythematous or purple papules and nodules.
Neutrophilic dermic infiltrate with the absence of leukocytoclastic vasculitis.
b. Minor criteria:
Fever (t >38°C), recent infections (respiratory, digestive), recent vaccination.
Arthralgia, conjunctivitis or associated malignancies.
Leukocytosis with neutrophilia >70% on the peripheral blood smear, inflammatory systemic syndrome (ESR >20 mm/h, positive CRP).
Positive response to corticosteroids.
The diagnosis of SS is based on the two major criteria and two of the minor (3,4). The elective treatment consists of systemic corticotherapy (oral doses 0.5-1 mg/kg/day with gradual reduction) or intralesional (topic or inhaled) (2).
Other medication includes: dapsone, potassium iodide (tablets or Lugol solution), cyclosporine, colchicine, indomethacin, methotrexate, isotretinoin, cyclophosphamide (2,3).
In some cases antibiotics may be used, partially because of frequent infections of the skin lesions, but also associated with certain inflammatory bowel diseases (Crohn’s disease). Therefore we can add: metronidazole, doxycycline, tetracycline and antistaphylococcal antibiotics (2).
Disease remission occurs within two to four weeks, but with symptom recurrence in 30-50% of cases (4).
CASE REPORT
Male child, aged 11, diagnosed at the age of 5 with immune thrombocytopenic purpura (diagnosis was confirmed at the time through bone marrow aspiration) in Iasi. Insufficient response to corticotherapy lead to the splenectomy procedure (February 2009, at the age of 7). However thrombocytopenia was still present and was later associated with anemia and leucopenia with neutropenia.
Admitted in the Oncopaediatric department of ‘Maria Sklodowska Curie’ Children’s Emergency Hospital, Bucharest, starting December 2012, the child was investigated in the hematological ward, considering the severe and rapid evolution of the pancytopenia.
Hemoglobin electrophoresis (A = 83%, A2 = 0.8%, F = 16.2%) indicated the differential diagnosis with delta-beta thalassemia, this being disproved by the erythrocyte indices (macrocytosis on the peripheral blood smear) and by the genetic exam performed at The National Institute of Transfusional Hematology.
Bone marrow aspiration (October 2013 – showing reduced cellularity, with myeloid series present, granulocytic series 60%, very low erythrocytic series 9%, thrombocytic series with extremely rare megakaryocytes) invalidated the diagnosis of immune thrombocytopenic purpura. We raised the possibility of differential diagnosis between aplastic anemia and myelodisplastic syndrome.
Subsequently, the bone marrow biopsy (June 2014) that indicated granulo-monocytic hyperplasia with left deviation of the formula, high percentage of CD3 positive cells, severe erythroblastopenia and megakaryocytic aplasia, lead to the positive diagnosis of myelodisplastic syndrome. Allogeneic bone marrow transplant from an older brother is suggested (100% HLA compatibility).
During his last admission (January 2014), the child developed clinical systemic manifestation that gradually became more severe; the symptoms are presented in the following table.
Table 1.
Table 1. Clinical manifestations in SS.
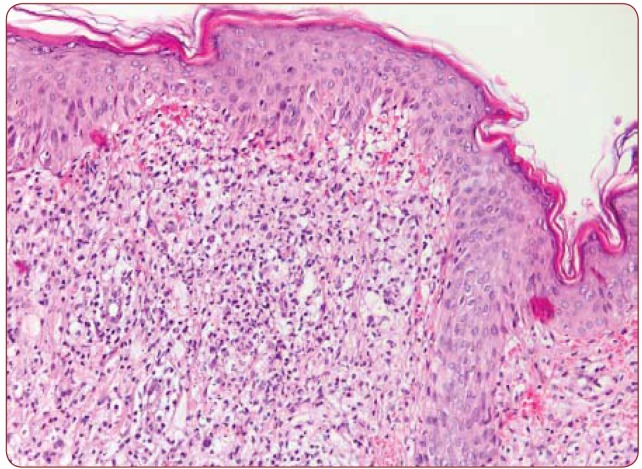
The symptoms were consistent with Sweet’s Syndrome, diagnosis confirmed by two skin biopsies in November 2013 and March 2014. The histopathological specimen of the first biopsy includes a skin fragment with minimal acanthosis and diffuse spongiosis; at dermo-hypodermal level we can observe moderate inflammatory lymphocytic infiltrate with rare neutrophils with perivascular, periadnexal and focal interstitial distribution; turgescent blood vessels with swollen endothelium.
The histopathological paraffin method of the second biopsy shows a skin fragment with important inflammatory infiltrate consisting mainly of neutrophils, but also relatively frequent macrophages and rare lymphocytes, over an extended area, with dense interstitial displacement in the superior dermis; DIF technique used on a different skin fragment was negative (see Figure 2).
Figure 1.
Figure 1. SS – red macules and papules on the back, extremely painful and pruriginous.
Figure 2.
Figure 2. Dense perivascular and interstitial inflammatory infiltrate with band-like distribution throughout the papillary dermis. Endothelial swelling, edema and prominent erythrocyte extravasation are present. HE x 200.
In conclusion, we can confirm the histopathological diagnosis of interstitial dermatitis with prominent neutrophils, consistent with Sweet’s Syndrome. Taking into consideration the references in specialty literature, our patient presented both major diagnosis criteria (abrupt onset with red, painful nodules, as well as dermal infiltrate with neutrophils at skin biopsy) and all the minor criteria (fever, shivering, highly positive inflammatory systemic syndrome, arthralgia, conjunctivitis and a favorable response to both systemic and local corticosteroids).
The patient had a slow evolution towards improvement, under the following medication: corticosteroids (systemic, local and inhaled), oral cyclosporine (150mg/day), oral dapsone and nonsteroidal anti-inflammatory drugs such as indomethacin suppository and later, oral tablets (50 mg/day).
The drug therapy induced an important remission of the SS, but the child continuously presented thrombocytopenia, therefore he was in constant need of thrombocytic mass administration.
In February 2015, as the child reached SS remission, we decided to transfer him to Fundeni Institute for the allogeneic bone marrow transplant procedure (from an older brother with 100% HLA compatibility). Unfortunately, the post-transplant evolution was not a favorable one, the patient developing graft-versushost disease,that eventually leads to his decease.
DISCUSSION
This article brings forward the case of a child with systemic form of Sweet’s syndrome secondary to a malignancy. With an evolution of the disease for over a year, the patient went through almost all clinical manifestations described in literature references, such as: high fever, shivering, rash, red aching nodules, subcutaneous edema, conjunctivitis, arthralgia, arthritis, respiratory symptoms (cough, dyspnoea, pulmonary infiltrates, polyserositis) and encephalitic symptoms (confusion, obnubilation, seizures).
In our case, the malignant affliction started with thrombocytopenia, considered at first to be immune thrombocytopenic purpura. The patient was treated for almost two years (intermittently) with corticosteroids, eventually undergoing a splenectomy procedure.
The presence of anemia and leucopenia, alongside with persistent thrombocytopenia, determined us to repeat the bone marrow aspiration and to extend the evaluation with bone marrow biopsy, thus establishing the positive diagnosis of MS.
The elective treatment in MS is the allogeneic transplant of bone marrow, preferably from a compatible donor, such as a family member.
The severe clinical manifestations regarding paraneoplastic SS delayed this treatment for over a year although we tried almost all the medication indicated for this condition. We have to mention that in specialty literature the longest timeframe of evolution is four to six months.
In this case, the evolution was similar to other paraneoplastic syndromes (for example nephrotic syndrome secondary to Hodgkin’s lymphoma) which show regression once the primary malignancy responds to treatment and can reappear if there’s a relapse of the disease.
Unlike most cases, this particular one is characterized by the absence of neutrophilia. This is possible because of the association between SS secondary to a hematological malignancy such as MS.
CONCLUSION
Our patient was diagnosed with systemic SS, secondary to a hematological malignancy (MS). He presented almost all clinical symptoms described so far in specialty literature, but with a longer evolution and resistance to treatment, acting like a paraneoplastic syndrome.
Assuming that we discover neutropenia associated with SS (instead of neutrophilia), we might consider searching for a malignancy as the underlying disease.
MS diagnosis was established with difficulty, because of the initial confusion with immune thrombocytopenic purpura.
Conflict of interests: none declared.
Financial support: none declared.
Contributor Information
Doinita Sfrijan, Department of Onco-hematology, “Maria Sklodowska Curie” Children’s Emergency Hospital, Bucharest, Romania; “Carol Davila” University of Medicine, Bucharest, Romania.
Simina-Maria Visan, Department of Onco-hematology, “Maria Sklodowska Curie” Children’s Emergency Hospital, Bucharest, Romania.
Bianca Diaconu, Department of Dermatology, “Maria Sklodowska Curie” Children’s Emergency Hospital, Bucharest, Romania.
Sabina Zurac, Department of Pathology, Colentina Clinical Hospital, Bucharest, Romania.
Cristian Scurtu, Department of Onco-hematology, “Maria Sklodowska Curie” Children’s Emergency Hospital, Bucharest, Romania.
REFERENCES
- Kuhne Th. Myelodisplastic Syndrome. In: Arcei R, Kuhne Th, Imbach P. Pediatric Oncology. A Comprehensive Guide. Berlin: Springer-Verlag. 2006:41–49. [Google Scholar]
- Hönigsmann H, Cohen P, Wolff K. - Acute Febrile Neutrophilic Dermatosis (Sweet’s Syndrome). In: Freedberg IM, Eisen A, Wolff K, et al. Fitzpatrick’s Dermatology In General Medicine. 6th edition. New-York: McGraw-Hill. 2003:1056–1061. [Google Scholar]
- Bayliss Mallory S, Bree A, Chern P. - Illustrated Manual of Pediatric Dermatology. Abingdon, Oxon: Taylor & Francis Group. 2005 [Google Scholar]
- Pires dos Santos T, Gouveia Sales B C, Sigres M. - Sweet Syndrome in childhood. An Bras Dermatol. 2015;90(4):567, 569. doi: 10.1590/abd1806-4841.20153247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouzidi H, Gallouj S, Amraoui N. - Syndrome de Sweet: étude clinique et natomopathologique sur 5 ans. Pan Afr Med J. 2015;20:362. doi: 10.11604/pamj.2015.20.362.4274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto R, Levy Y, Krause JR. - Sweet syndrome and its association with hematopoietic neoplasms. Proc (Bayl Univ Med Cent) 2015;28(1):62–4. doi: 10.1080/08998280.2015.11929190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert Cohen D et al. - Sweet’s syndrome. J Emerg Med. 2015;49:e95. doi: 10.1016/j.jemermed.2015.02.039. [DOI] [PubMed] [Google Scholar]
- Buttgereit F, Burmester GR, Straub RH, et al. - Exogenous and endogenous glucocorticoids in rheumatic diseases. Arthritis Rheum. 2011;63:1. doi: 10.1002/art.30070. [DOI] [PubMed] [Google Scholar]
- Kazmi SM, Pemmaraju N, Patel KP, et al. - Characteristics of Sweet Syndrome in Patients with Acute Myeloid Leukemia. Clin Lymphoma Myeloma Leuk. 2015;15(6):358–63. doi: 10.1016/j.clml.2014.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anzalone CL, Cohen PR. - Acute febrile neutrophilic dermatosis (Sweet’s syndrome). Curr Opin Hematol. 2013;20:26–35. doi: 10.1097/MOH.0b013e32835ad132. [DOI] [PubMed] [Google Scholar]
- Tuerlinchkx D, Bodart E, Despontin K, et al. - Sweet’s syndrome with arthritis in an 8-month-old boy. J Rheumatol. 1999;26:440–2. [PubMed] [Google Scholar]
- Bourke JF, Keohane S, Long CC, et al. - Sweet’s syndrome and malignancy in the U.K. Br J Dermatol. 1997;137:609–13. doi: 10.1111/j.1365-2133.1997.tb03796.x. [DOI] [PubMed] [Google Scholar]
- Sweet RD. - An acute febrile neutrophilic dermatosis. Br J Dermatol. 1964;76:349. doi: 10.1111/j.1365-2133.1964.tb14541.x. [DOI] [PubMed] [Google Scholar]