Abstract
Migraine is a common, but often underdiagnosed complaint in children and the lack of studies regarding its treatment in this particularly population makes it harder to enlarge the choices of treatment. However, recent trials made it easier to utilize newer compounds that improve the outcome of the disease. We reviewed the treatment of pediatric migraine and divided therapeutic methods into two broad areas: treatment of the acute attack – used both in the emergency room and as home options and prophylactic agents. Not to be forgotten when talking about treating migraine in children and adolescents is the support therapies offered alongside the classical approach by teams formed by the pediatric neurologist, pediatrician, psychologist, support groups and the families of the patients.
Keywords:migraine, acute treatment, preventive treatment, child
INTRODUCTION
Migraine is a common complaint in the pediatric population. It is a hereditary disorder with a multifactorial inheritance pattern: when interviewing both parents of a child, at least one of them gives a history of migraine in over 90% of cases. 10% of children aged 5-15 years have migraine and migraine also accounts for 75% of headaches in young children referred for neurological consultation. The prevalence of this condition is 2.5% under the age of 7 (both genders equally affected), 5% from age 7 to puberty (female-tomale ratio of 3:2), 5% in post-pubertal boys and 10% in post-pubertal girls. The higher incidence in pubertal girls is probably related to the triggering effect of the menstrual cycle on migraine attacks (1).
Approximately 25% of children will be migraine- free by the age of 25, boys in a significantly higher percentage than girls and more than half will still have headaches at the age of 50. The most common symptoms include episodic attacks of moderate to very severe headache (typically throbbing, unilateral, and exacerbated by physical activity), accompanied by nausea, photophobia and phonophobia. Attacks are heterogeneous in symptomatology, severity and disability, both between different individuals and separate attacks in the same individual sufferer. Migraine is a highly disabling condition that leads to reduced quality of life among children.
Clinical manifestations may vary depending on the age of the child: infants younger than 12 months may have episodes of “head banging” only. Toddlers often look ill, they have abdominal pain, vomiting, and the urge to go to sleep in a dark room; they express their pain by being irritable, rocking or crying without having any apparent reason. School aged children (age 5-10 years) have bifrontal, bitemporal, or retroorbital headache; abdominal pains, nausea, vomiting, phonophobia, photophobia, the need to sleep, typical migraine facies, tearing, swollen nasal passages, thirst, excessive sweating, edema, increased urination, or diarrhea. In older children the intensity of the headache is severe and it lasts longer. It has a pulsating or a throbbing character and the distribution is unilateral with a temporal location.
Migraine, in pediatric population as well as in adults, is underdiagnosed. The diagnosis of migraine is not supported by laboratory or i maging findings and it is based only on the history information and the thorough physical e xamination.
TREATMENT
Migraine treatment is divided into two broad areas: acute and preventive therapies.
GENERAL MEASURES
The education of the family and child regarding migraine headache is an important issue. Children who experience migraine, as well as their families, may benefit from creating a migraine journal where they can mark each episode, describing the attack in order to find a pattern and to identify the potential triggering factors and the response they have after administrating different therapies.
The first step in avoiding migraine attacks is recognizing and eliminating the triggering factors such as:
dietary: alcoholic beverages, caffeine excess, artificial sweeteners, tyramine (aged cheeses, smoked fish, cured meats), nitrates and nitrites, monosodium glutamate
environmental: media abuse, odors
medication: cimetidine, estrogen, histamine, hydralazine, nifedipine, nitroglycerin, ranitidine, reserpine, long-term use of nonsteroidal anti-inflammatory drugs
psychological and physical triggers: stress, anxiety, worry, depression, fatigue, fever, illness, poor sleep habits, irregular meals, fasting, hypoglycemia, dehydration.
When a migraine episode starts the child should rest or sleep in a dark and quite room, with a cool cloth applied on his forehead. Medications for the acute treatment should be given early in the course of the migraine.
ACUTE TREATMENT
The goals of acute treatment are to treat each attack as it occurs and allow the return to normal activities. This type of treatment is needed by all patients. A time limit of two hours has been suggested for these effects to occur. Parents should be given a guide of acute medications to treat attacks depending on the level of severity and they should have rescue medication if the initial therapy does not have the expected effect.
On the other hand, the exhaustion of home treatment options may lead the family to the emergency room.
There are two categories in which children suffering from migraine attacks fall into: those who are brought to the emergency room during their first acute migraine attack and those who were given a certain migraine diagnosis, but, at that particular moment, suffer from a more severe headache despite their treatment. Both categories should be thoroughly examined in order to establish or confirm the diagnosis of migraine.
General methods
Usually, upon the arrival at the emergency room, the child has already used the first line therapy (i.e. acetaminophen or ibuprofen) without any significant result.The approach of the acute migraine attack in the pediatric emergency room begins with the isolation of the child in a silent, dark compartment and the encouragement to go to sleep. The physician must identify any red flags that can show a potential intracranial pathology and continue the investigations with imaging if any abnormalities are shown during the neurological examination.
If the migraine diagnosis is certain, then the next important step would be intravenous rehydration.
Before arriving to the emergency room, the child has been vomiting and/or has had a poor oral intake due to nausea and severe headache, so it is important that the patient is well hydrated. Also, this measure prevents the possible acute renal failure caused by non-steroidal anti-inflammatory drugs, such as Ketorolac and orthostatic hypotension caused by phenothiazine (chlorpromazine).
Antiemetics
Patients who experience nausea associated or not with vomiting benefit from the placement of an intravenous line in order to receive antiemetic treatment. The use of phenothiazines – prochlorperazine and chlorpromazine or metoclopramide has been proven efficacious, keeping in focus the risk of extrapyramidal signs (dystonia, akathisia) and sedation as adverse effects (2).
Prochlorperazine may be administered after an intravenous line is secured in the emergency room. The used dosage begins at 0.15 mg/kg, without exceeding a maximum of 10 mg/dose.
Metoclopramide may be used in an oral compound at home or intravenous in the emergency room. The recommended dosage is between 0.13-0.15 mg/kg with a maximum of 10 mg/dose (3). In order to avoid sedation and akathisia without influencing the benefits regarding headache and nausea, the infusion of metoclopramide may be slowed down to involve more than 15 minutes (4).
In previous reports, metoclopramide was the most used agent in the emergency department to reduce nausea and vomiting associated with migraine attacks, but recent observational studies showed that prochlorperazine is used with equal frequency, and it appears to be superior to metoclopramide in preventing a repeat emergency department visit (5).
Analgesics – NSAIDs and nonspecific analgesics
Acetaminophen and ibuprofen are the most commonly used over-the-counter treatments for pain relief and antipyretics in children. For acute migraine treatment, acetaminophen is used in doses of 15 mg/kg, and ibuprofen in doses of 7.5 – 10 mg/kg. Both are effective and well tolerated, but ibuprofen is an overall better alternative for pain relief. Our experience with pediatric migraineurs has shown that when given at the beginning of the attack, a combination of acetaminophen and a caffeine compound relieves the headache faster and it diminishes its intensity with greater efficacy than either agent alone.
Ketorolac is another NSAID used mostly in the emergency department. At this time we only have one study regarding the use of ketorolac in pediatric patients suffering from migraine at the emergency room. It was used an intravenous formula, starting from 0.5 mg/kg to a maximum of 30 mg/dose. Ketorolac was effective in 55.2 % of the patients in one hour. An oral formula is also available for home treatment with a dosage of 0.75 mg/kg (6).
When administrated daily, these types of treatments can lead to analgesic-rebound headache. This problem is often under-recognized and very hard to treat. The patient enters a vicious circle, and headaches can become self-perpetuating. Analgesic rebound headache answers well to amitriptyline (10 mg) given for a short period of time (2 months) with minimal sedation effects.
Ergot-based therapies
Children can also benefit from ergot-based therapies (dihydroergotamine, ergotamine associated with caffeine) during the migraine attack, but they should be used based on a strict usage guideline in order to minimize the potential side effects given by their vasoconstrictive properties. Dihydroergotamine’s recommended dosage varies between 0.1-0.2 mg/ dose. An angio-MRI must be considered before prescribing a caffeine based agent. Also, their association with triptans and the use in complicated migraine is contraindicated. Intravenous dihydroergotamine can result in nausea, making necessary pretreatment with an oral antiemetic such as promethazine.
Triptans
One of the mechanisms incriminated in the genesis of the migraine involves the trigeminovascular system and activation of vasoactive structure in cranial and dural vessels, which causes the release of vasoactive neuropeptides. Serotonin (5-hydroxytriptamine) presynaptic receptors control the release of these neuropeptides, and postsynaptic receptors constrict vessel walls. The mechanisms through which serotonin is involved as a mediator of migraine pain are still unknown.
Triptans are a class of tryptamine-based pharmacological agents which act as serotonin agonists, helping reduce cerebral blood flow and neuropeptide release. Sumatriptan is considered to be the reference standard and it is available with different preparations including oral, intranasal, and subcutaneous forms. In the pediatric population the effect of oral sumatriptan showed no significant pain relief (7).
On the other hand, intranasal sumatriptan showed significant effectiveness in headache relief without having any important side effects. Another advantage in using intranasal preparations is the easier way of administration. Intranasal sumatriptan’s recommended dosage may fluctuate between 5, 10 or 20 mg in one nostril. Oral sumatritpan may administered in doses of 25, 50, 100 mg.
Other triptans approved by the FDA for treating migraine attacks in pediatric population, children above the age of 6 and adolescents, are almotriptan, zolmitriptan and rizatriptan. Although limited, studies among the children suffering from migraine attacks show that rizatriptan provided statistically significant pain relief at 2 hours while also reducing associated nausea and vomiting.
Zolmitriptan, in both nasal and oral administration, has proved to be effective in the adolescent population. Also, forvatriptan might have the same effect in adolescents as in adults, using comparable doses (7,8).
Only 2.2% of the children presenting to the emergency room during a migraine attack receive triptans as home treatment for their attacks. The question is if this percentage shows that triptans are used less than other agents or if children using them are less likely to need emergency room treatments than those receiving other agents (9).
Calcitonin gene–related peptide (CGRP)- receptor antagonist - BIBN 4096 BS
CGRP is a 37-amino-acid neuropeptide which is potent vasodilatator present in perivascular trigeminal-nerve fibers that supply the pial arteries, the meningeal arteries and the extracranial cephalic arteries. Therefore, BIBN4096 BS, a calcitonin gene–related peptide- receptor antagonist might be effective in acute migraine treatment.
In recent clinical trials BIBN4096 BS was administered in a dose of 2.5 mg IV over a period of 10 minutes and the rate of response to pain, two hours after treatment was good. Nausea, photophobia, phonophobia and functional capacity all improved in parallel with the extent of response to treatment. Also, the rate of use of rescue medication was lower among patients who received BIBN 4096 BS than among those who received placebo.
At the moment, CGRP receptor antagonist therapy undergoes phase III of clinical studies (10).
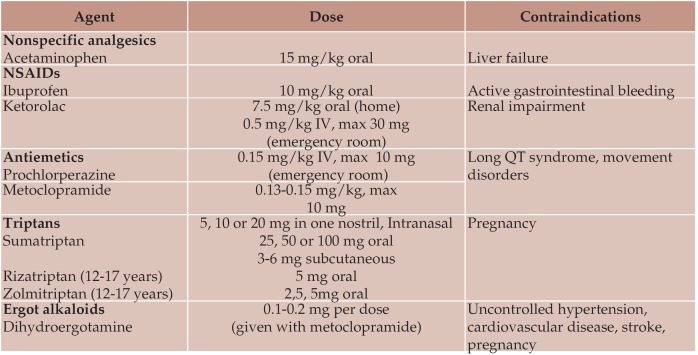
The most frequent agents used in treating acute migraine attacks, their doses,as well as one of their most important contraindications are summarized in Table 1.
Recommendations for the acute treatment of migraine in children and adolescents (8).
Ibuprofen is effective and should be considered for the acute treatment of migraine in children (Level A).
Acetaminophen is probably effective and should be considered for the acute treatment of migraine in children (Level B).
Sumatriptan nasal spray is effective and should be considered for the acute treatment of migraine in adolescents (Level A).
There are no data to support or refute use of any oral triptan preparations in children or adolescents (Level U).
There are inadequate data to make a judgment on the efficacy of subcutaneous sumatriptan (Level U) (8).
PROPHYLACTIC TREATMENT
For children who, despite submitting to nonpharmacological treatments, still experience frequent migraine attacks, often disabling and a major cause of school absence and lower quality of life, prophylactic treatment is required.
β-blockers
In adult population, ƒÒ-blockers (especially propranolol) have shown some efficacy, but in children there have been inconsistent results. When introducing propranolol, heart rate and orthostatic pressure should be monitored every three months and each time the dose is increased. Usually, the starting dose is 1mg/kg divided in three doses without exceeding 4 mg/ kg per day. Propranolol should not be administrated in children with asthma and should be used with caution in patients with diabetes, orthostatic hypotension and depression.
Table 1.
Table 1. Treatment of the acute migraine attack in children (adapted after 8,11).
NSAIDs = nonsteroidal anti-inflammatory drug.
Antihistaminic drugs
The antihistamine cyproheptadine has serotonin and calcium-blocking, as well as anticholinergic properties and is well-tolerated by children. The daily dose varies from 2 to 8 mg/kg. The dose may be administered in a single dose at bedtime, in order to avoid daytime sleepiness having the same effect as two or three daytime doses.Increased appetite, weight gain and somnolence may appear and can limit the use of cyproheptadine in older children.
The combination of propranolol and cyproheptadine was proved the most efficacious of either therapies alone compared to placebo (7).
Tricyclic antidepressants
Tricyclic antidepressants have been used to treat analgesic-rebound headache in children, as well as in adults.
Amitriptyline is the most used and efficacious tricyclic antidepressant in children. The clinical experience showed that a single day oral dose of 5 mg, given at bedtime is, in most cases, effective. If the headaches persist with the same frequency, the dose may be increased by 5 mg increments not sooner than two weeks between changes.
Keeping in mind that, at the moment, neither nortriptyline or protriptyline are proved to be effective in the treatment of adult or pediatric headache, nortriptilyne can be used for it’s milder anticholinergic activity and sedative effects, as an alternative to amitriptyline (7).
An electrocardiogram should be performed before beginning the treatment because nonspecific electrocardiographic changes may be observed, as well as chances in atrioventricular conduction.
Anti-epileptic drugs
It was always suspected that there is a strong association between migraine and epilepsy. This is important in elaborating a treatment strategy helpful for patients with both migraine and epilepsy. No controlled pediatric studies are currently available in order to evaluate the co-morbidity of epilepsy and migraine or behavioral disorders and migraine, but there does seem to be higher concurrence in children. Their therapeutic effects in treating migraine are due to their N and T- type calcium channel blocking properties.
Valproic acid was effective in open-label trials in young children and adolescents, but the adverse effects in adolescent females, including weight gain, hair loss, teratogenic effects and liver insufficiency must be considered (12).
Valproate treatment starts with a dose of 10 to 15 mg/kg divided in two daily doses. This dose can be increased with 15 mg/kg increments reaching a maximum of 60 mg/kg/day. The therapeutic dose for treating migraine is not yet established, but the therapeutic range is considered to be 50 to 100 mg/dL. If given a dose that exceeds 150 mg/dL, the patient should be monitored closely.
Newer antiepileptic drugs such as topiramate, gabapentin and levetiracetam have been shown to reduce headache frequency in openlabel, retrospective trials. Topiramate is, generally, a well-tolerated therapy. In migraneur children the treatment starts at 15 mg/day and it is increased during a period of over eight weeks to 2 to 3 mg/kg daily. The maximum tolerated dose may reach a limit of 200 mg/day. Topiramate treatment may cause anorexia, weight loss, gastroenteritis, as well as concentration difficulty, somnolence or even cognitive impairment. Given the low dose administrated in treating migraine, Topiramat can be a good choice for the pediatric population due to its efficacy and the low frequency of side effects (13).
Levetiracetam administrated in a dose of 125 to 250 mg twice a day has been proven to be effective in treating migraine. During the Levetiracetam treatment, patients may experience dizziness, irritability and somnolence (14).
Calcium channel blockers
Cinnarizine is an L-type calcium channel blocker which has a number of different pharmacological effects that may determine its positive results in treating migraine. A double-blind placebo-controlled randomized study showed that at a dose of 1.5 mg/kg/day in children weighing less than 30 kg and 50 mg/day in those weighing more than 30 kg significantly reduces the frequency and intensity of headache in children with migraine. Also, side effects such as weight gain and extrapyramidal signs were minimal (15).
Another calcium channel blocker studied for treating pediatric migraine is Flunarizine. The largest placebo-controlled study so far showed that a dose of 5mg/day of flunarizine decreases in a significant way headache frequency and duration compared with placebo in pediatric migraine. Compared with the low frequency of side effects of Cinnarizine, Flunarizine’s adverse effects
OnabotulinumtoxinA
Onabotulinumtoxin A is a drug approved by the Food and Drug Administration (FDA) for chronic migraine in adults. It was shown effective in two phase III placebo controlled trials (PREEMPT 1 and PREEMPT 2). It’s effectiveness was shown in reducing the duration of headache and the improved quality of life. The patients were treated following a protocol. The drug was administered intramuscularly, using 155 units in a total of 31 injection sites, every 12 weeks. The adverse effects included: injection site pain, headache, facial paresis, neck pain and weakness. In the pediatric population onabotutlinumtoxin A was evaluated in two studies. One of them used a dose of 100 units and showed an improvement in headache relief in 4 out of 10 patients and in the second one, half of the patients experienced a 75% reduction in the frequency of their attacks over the long course (7).
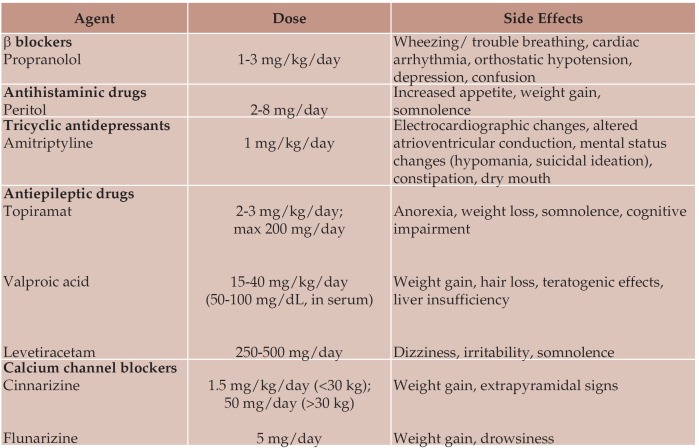
The most used prophylactic therapies in pediatric migraine and the side effects that must be taken into consideration when elaborating a treatment strategy are summarized in Table 2.
Table 2.
Table 2. Prophylactic treatment of the migraineur child (adapted after 7).
Migraine is a chronic disease that can often require long term therapy. The restrictions applied to the migraneur child – a well-organized life style, permanent avoidance of trigger factors –together with the constant pressure of the daily treatment may have a deep impact on the child’s emotional development. Given the well-known fragility of children and adolescents, migraineurs and their families would benefit from the help of a psychotherapist/ psychologist.
Other non-pharmacological measures that have been proven effective in migraine relief include biofeedback programs and relaxation training, aiming to reduce both the frequency and severity of migraine attacks. All children may benefit from these therapies, but they are reserved for those who have disabling headaches.
CONCLUSION
Although considered to be a benign self-limited disorder, migraine in children has proved to surpass the childhood period into adulthood. Recognizing and avoiding trigger factors as well as a suitable therapy strategy may give the migraneur child the chance for a good quality of life. The promptitude and the efficacy of the acute treatment diminishes the time in which the child is exposed to pain and discomfort making it less susceptible to the great amount of psychological stress during attacks.
Prophylactic treatment is necessary after a certain diagnosis is made, but it is mandatory to keep in mind the contraindications of the chosen therapeutic agents as well as their immediate and comprised side effects. Another important aspect is the underlying conditions of the sufferer. They will be thoroughly be taken into consideration when recommending a therapeutical plan.
An important part of the prophylactic treatment in pediatric migraine is the psychological support that should be given to each child in order to have a compliant patient without any further emotional disorders that may arise from both the pressure of the daily treatment as well as the vulnerability and emotional fragility that characterize these particular age categories. It is not to be forgotten the need of a multidisciplinary team (pediatric neurologist, pediatrician, psychologist, support groups, family) when treating a migraineur child.
Conflict of interests: none declared.
Financial support: none declared.
Contributor Information
Raluca Ioana Teleanu, Department of Pediatric Neurology, “Dr. Victor Gomoiu” Children’s Hospital, Bucharest, Romania; “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Oana Vladacenco, Department of Pediatric Neurology, “Dr. Victor Gomoiu” Children’s Hospital, Bucharest, Romania.
Daniel Mihai Teleanu, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Diana Anamaria Epure, Department of Pediatric Neurology, “Dr. Victor Gomoiu” Children’s Hospital, Bucharest, Romania.
REFERENCES
- Cummings E, Wittick L, Cantor R - Evaluation and Management of Headache in the Pediatric Patient. . http://www.obgynnews.com/ view-pdf.html?file=fileadmin/qhi_archive/ ArticlePDF/EM/041110036. 2015 [Google Scholar]
- Damen L, Bruijn JK, Verhagen AP, et al. - Symptomatic treatment of migraine in children: a systematic review of medication trials. Pediatrics. 2005;116:e295–302. doi: 10.1542/peds.2004-2742. [DOI] [PubMed] [Google Scholar]
- Kabbouche MA, Linder SL - Acute treatment of pediatric headache in the emergency department and inpatient settings. Pediatr Ann. 2005;34:466–471. doi: 10.3928/0090-4481-20050601-12. [DOI] [PubMed] [Google Scholar]
- Tura P, Erdur B, Aydin B, Turkcuer I, Parlak I - Slow infusion metoclopramide does not affect the improvement rate of nausea while reducing akathisia and sedation incidence. Emerg Med J. 2012;29:108e12. doi: 10.1136/emj.2010.094367. [DOI] [PubMed] [Google Scholar]
- Bachur RG, Monuteaux MC, Neuman MI - A comparison of acute treatment regimens for migraine in the emergency department. Pediatrics. 2015;135:232–238. doi: 10.1542/peds.2014-2432. [DOI] [PubMed] [Google Scholar]
- Brousseau DC, Duffy SJ, Anderson AC, Linakis JG - Treatment of pediatric migraine headaches: A randomized, double-blind trial of prochlorperazine versus ketorolac. Ann Emerg Med. 2004;43:256e62. doi: 10.1016/s0196-0644(03)00716-9. [DOI] [PubMed] [Google Scholar]
- Freitag FG, Schloemer F, Schumate D - Recent Developments in the Treatment of Migraine in Children and Adolescents; Journal of headache & pain management. 2016;1:9. [Google Scholar]
- Lewis D, Ashwal S, Hershey A et al. - Practice Parameter: Pharmacological treatment of migraine headache in children and adolescents. Report of the American Academy of Neurology Quality Standards Subcommittee and the Practice Committee of the Child Neurology Society. Neurology. 2004;63:2215–2224. doi: 10.1212/01.wnl.0000147332.41993.90. [DOI] [PubMed] [Google Scholar]
- Richer LP, Laycock K, Millar K, et al. - Treatment of children with migraine in emergency departments: National Practice Variation Study. Pediatrics. 2010;126:e150e5. doi: 10.1542/peds.2009-2337. [DOI] [PubMed] [Google Scholar]
- Olesen J, Diener HC - Calcitonin Gene–Related Peptide Receptor Antagonist BIBN 4096 BS for the Acute Treatment of Migraine. New England Journal of Medicine. 2004;350:1104–1110. doi: 10.1056/NEJMoa030505. [DOI] [PubMed] [Google Scholar]
- Gelfand A., Goadsby P - Treatment of Pediatric Migraine in the Emergency Room. Pediatric Neurology. 2012;47:233–241. doi: 10.1016/j.pediatrneurol.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis DW - Pediatric migraine. Neurol Clin. 2009;27:481–501. doi: 10.1016/j.ncl.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Winner P, Pearlman EM, Linder SL, et al. - Topiramate for migraine prevention in children: a randomized, double-blind, placebo-controlled trial. Headache. 2005;45:1304. doi: 10.1111/j.1526-4610.2005.00262.x. [DOI] [PubMed] [Google Scholar]
- Miller GS - Efficacy and safety of Levetiracetam in pediatric migraine. Headache. 2004;44:238. doi: 10.1111/j.1526-4610.2004.04053.x. [DOI] [PubMed] [Google Scholar]
- Mahmoud R, Ashrafi M - Efficacy and Safety of Cinnarizine in the Prophylaxis of Migraine in Children: A Double- Blind Placebo-Controlled Randomized Trial. Pediatric Neurology. 2014;51:503–508. doi: 10.1016/j.pediatrneurol.2014.05.031. [DOI] [PubMed] [Google Scholar]
- Cruse RP, Patterson MC, et al. - Acute treatment of migraine in children. http://www.uptodate.com/contents/ acute-treatment-of-migraine-inchildren? source=search_result&search= migraine+in+children&selectedTitle=4~150. 2016 [Google Scholar]
- Mack K, Patterson MC, et al. - Preventive treatment of migraine in children. http://www.uptodate.com/contents/ preventive-treatment-of-migraine-inchildren? source=search_result&search= migraine+in+children. 2016 [Google Scholar]