When important decisions are to be made, the patient must receive detailed information on the illness, treatment options and prognosis. The shortening of hospital stays and the trend towards outpatient care enhance the need of patients and their families for specific information.1 Practitioners are responding to these demands, yet the amount of information correctly recalled by patients is strikingly small.2 In this review I examine empirical evidence concerning the obstacles to memory for medical information and offer some suggestions for overcoming them.
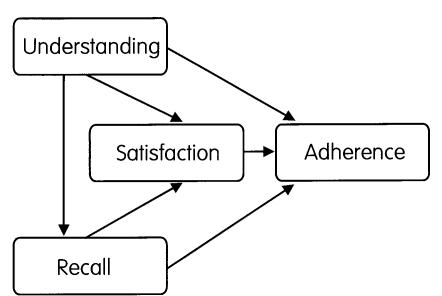
Clearly, memory for medical information is a prerequisite for good adherence to recommended treatment. Ley's3 model on effective communication in medical practice (see Figure 1) stresses the importance of memory next to factors such as the understanding of information and satisfaction with the treatment. 40-80% of medical information provided by healthcare practitioners is forgotten immediately. The greater the amount of information presented, the lower the proportion correctly recalled;4 furthermore, almost half of the information that is remembered is incorrect.5 For the forgetting of information there are three basic types of explanation—first, factors related to the clinician, such as use of difficult medical terminology; second, the mode of information (e.g. spoken versus written); and, third, factors related to the patient, such as low education or specific expectations.6 Here, I discuss only the second and third, since the communication skills of clinicians have been thoroughly reviewed elsewhere.7,8
Figure 1.
Overview of Ley's model on the interactions between patient-related factors and therapy adherence (see Ref. 3)
AGE-RELATED MEMORY FUNCTION
There is a general assumption that people in later life have poorer information recall than younger persons. However, not all aspects of memory are equally susceptible to age-related impairment and certain forms of memory remain intact over the lifespan. For example, memory for specific events or facts (so-called episodic information, which includes what the doctor tells you) is subject to age-related loss,9 whereas memory for skills (such as driving a car) or for general semantic information (knowing that Berlin is the capital of Germany) is relatively spared. There is reason to believe that age-related memory impairments arise from defects in encoding and storage rather than retrieval.10 With respect to medical information, a moderate inverse relation has been reported between age and amount of information recalled correctly.6 Also, when Morrow et al.11 investigated the effects of ageing on memory for appointment-related information through an automated telephone messaging system, the older adults answered fewer questions correctly (though there were no differences between young and old with respect to message repetition).
Why should older adults recall less medical information than young? Although this can be the consequence of age-related cognitive impairments (e.g. in working memory), another possible explanation is an impaired capacity to deal with unstructured information. That is, older people might have difficulty structuring the information for recollection at a later time. This hypothesis was examined by showing young and old adults videos about osteoarthritis, a condition that can affect both age groups.4 Two kinds of presentation were tested—either organized (i.e. in a logical order from test results to treatment consequences) or non-organized. Non-organized presentation of medical information is probably more in line with everyday clinical practice, in which the diagnosis and treatment options tend to emerge from a series of investigations reported to the patient at various times. The results of the study were intriguing: although the young adults outperformed the old immediately after the presentation, no group differences were found in amount of information remembered at one week or one month; moreover, the mode of presentation, organized or unorganized, made no difference to memory performance.
Others12 have suggested that it is not the organization of the material that is crucial in age-related memory function, but the extent to which the information is consistent with previously acquired knowledge and beliefs. There is indeed evidence for this—Rice and Okun13 found that, among older readers, medical information that confirmed existing beliefs was better remembered than information contradicting these beliefs. The acquisition of totally new information tends to be easier than correction of preexisting knowledge, a phenomenon that is explicable in terms of cognitive schemas. A schema is a ‘personal theory’ formed by the individual over the years about a disease or disorder, and in many cases it will embrace misconceptions. New information that is inconsistent with the schema tends to be misinterpreted or forgotten; and patients with chronic medical conditions often have elaborate schemas about their illness. Evidence for the influence of schemas comes from a study by Okun and Rice:14 they found that, both in a group with osteoarthritis and in healthy controls, ‘disconfirming’ information was recalled less accurately than ‘confirming’ information; furthermore, recall was worse when the medical information was related to the participant's own illness and thus had personal relevance.
In sum, the ageing process engenders difficulty in encoding and subsequently remembering medical information, especially that which contradicts preexisting beliefs. Memory also fades more rapidly. A practical implication is that, especially in old people, clinicians should not leave a long gap between providing information and seeking the patient's decision.4
ANXIETY AND DISTRESS
The information given by the doctor often has profound implications for the patient. Moreover, the stress engendered by news of a life-threatening condition may be enhanced by information about prognosis and treatment. What are the effects of stress and anxiety on memory performance? From the results of cognitive-psychological experiments two phenomena are especially relevant in clinical settings—namely, attentional narrowing and state-dependent learning. Attentional narrowing15 occurs if events are perceived as stressful or emotional. For example, when a doctor says, ‘you have X disease, and this will affect everyday activities for the rest of your life’, this central message can become the primary focus, limiting attentional resources for peripheral information. The peripheral information, perhaps about therapy adherence or follow-up appointments, is not processed and stored into memory and therefore cannot be recalled.6
State dependency refers to the phenomenon whereby the amount of information recalled depends on congruity between the physical or psychological state during the learning phase and the state during the recall phase. Thus, if information is given while the patient is highly stressed, with stress-related physiological phenomena such as tachycardia, the memory performance will be best if he or she is in the same state during the recall phase.16 The fact that advice on treatment is commonly given in the stressful environment of a clinic yet is applicable in the more relaxed home environment, may partly explain why patients forget how many pills to take or the date of their next appointment.
Research on the recall of medical information supports this notion. For example, women at risk for breast cancer remembered less information if the physician made a worried impression (thus increasing the level of distress).17 Furthermore, in a group of outpatients anxiety and recall were related in an inversely U-shaped curvilinear manner: both very high and very low anxiety hamper eventual memory performance, moderate anxiety being best.6 Clinicians must therefore take account of the distressing features of the information to be given. If this cannot be mitigated—for example, in the case of a bad-news interview—provision of an audiotape of the interview will enable the patient to go over the information at home, when anxiety and distress have lessened, and absorb it properly.18,19
PERCEIVED IMPORTANCE OF THE INFORMATION
Another factor affecting memory for medical information is its perceived importance. Statements about the diagnosis tend to be viewed as highly important, those related to treatment less so. In addition, the amount of correctly recalled information is closely related to the subjective importance of the material. An effective strategy is to put instructions first in the message, emphasizing their importance—i.e. making use of the ‘primary effect’ commonly observed in memory research. Medical advice is also perceived as being more important if it is expressed in specific rather than general terms. Thus, ‘You need to get some rest’ will be remembered less accurately than ‘You must take the next two weeks off’.20 However, accurate recall also depends on the complexity of the message: statements in simple language will be recalled better than complex formulations.
The organization or categorization of the statements is another influence on memory performance. Information can be categorized in two ways—implicitly or explicitly. As mentioned earlier, implicit categorization—i.e. merely presenting the statements in a logical order—does not improve recall. By contrast, explicit categorization does increase recall of medical information. The difference is that categories of information are specified in advance. 6 A standard five-category set begins by telling the patient what is wrong, then what tests will be performed, then what is expected to happen, then which treatment will be needed and finally what the patient can do to help himself or herself.
SPOKEN, WRITTEN OR NON-VERBAL?
The form or mode of information is also highly relevant. In most instances, medical advice is spoken, but this is not a very successful method. 21 Written information is better remembered and leads to better treatment adherence. 22 However, written instructions do present difficulties to patients with low education or literacy and to non-native speakers, so other options have been investigated. For example, cartoons have been used to improve adherence to wound-care advice in patients just released from the emergency department: those who received the cartoon instructions displayed better compliance and answered more questions correctly. Patients with low education benefited more from the cartoon method than did patients with high education. 23 Others 1,24 have used pictographs— picture-writing—in cancer and HIV/AIDS. With spoken medical instructions only 14% of the information was remembered correctly, compared with over 80% when pictographs were used. 1 Simple pictographs, with a clear and direct link between the picture and its meaning, are most effective. 24 Further studies should focus on the clinical applicability of pictographs and their cost-benefit ratio.
In addition to verbal or visual communication methods technological aids are available, such as videotaped instructions or computer-aided information systems. Research on these new methods has so far yielded mixed results. A study in dental practice indicated that multi-media information had only a slightly better short-term effect than written information, 25 and patients receiving chemotherapy preferred direct communication with a clinician to watching a videotape. 26 Technological aids should be examined in more detail, but on existing evidence a combination of spoken and written or visual information is best. 21
CONCLUSION
Memory for medical information is often poor and inaccurate, especially when the patient is old or anxious. Patients tend to focus on diagnosis-related information and fail to register instructions on treatment. Simple and specific instructions are better recalled than general statements. Patients can be helped to remember medical information by use of explicit categorization techniques. In addition, spoken information should be supported with written or visual material. Visual communication aids are especially effective in low-literacy patients, but video or multimedia techniques do not improve memory performance or adherence to therapy.
Acknowledgments
I thank Dennis Schutter for helpful comments.
References
- 1.Houts PS, Bachrach R, Witmer JT, et al. Using pictographs to enhance recall of spoken medical instructions. Patient Educ Couns 1998;35: 83-8 [DOI] [PubMed] [Google Scholar]
- 2.Godwin Y. Do they listen? A review of information retained by patients following consent for reduction mammoplasty. Br J Plast Surg 2000;53: 121-5 [DOI] [PubMed] [Google Scholar]
- 3.Ley P. Communicating with Patients: Improving Communication, Satisfaction and Compliance. New York: Croom Helm, 1988
- 4.McGuire LC. Remembering what the doctor said: organization and older adults' memory for medical information. Exp Aging Res 1996;22: 403-28 [DOI] [PubMed] [Google Scholar]
- 5.Anderson JL, Dodman S, Kopelman M, Fleming A. Patient information recall in a rheumatology clinic. Rheumatol Rehabil 1979;18: 245-55 [DOI] [PubMed] [Google Scholar]
- 6.Ley P. Memory for medical information. Br J Soc Clin Psychol 1979;18: 245-55 [DOI] [PubMed] [Google Scholar]
- 7.Robinson G. Effective doctor-patient communication: building bridges and bridging barriers. Can J Neurol Sci 2002;29(suppl 2): S30-2 [DOI] [PubMed] [Google Scholar]
- 8.Cegala DJ, Lenzmeier Broz S. Physician communication skills training: a review of theoretical backgrounds, objectives and skills. Med Educ 2002;36: 1044-16 [DOI] [PubMed] [Google Scholar]
- 9.Kessels RPC, De Haan EHF. Mnemonic strategies in older people: a comparison of errorless and errorful learning. Age Ageing (in press) [DOI] [PubMed]
- 10.Glisky EL, Rubin SR, Davidson PS. Source memory in older adults: an encoding or retrieval problem? J Exp Psychol Learn Mem Cogn 2001;27: 1131-46 [DOI] [PubMed] [Google Scholar]
- 11.Morrow DG, Leirer VO, Carver LM, Tanke ED, McNally AD. Effects of aging, message repetition, and note-taking on memory for health information. J Geront B Psychol Sci Soc Sci 1999;54: P369-79 [DOI] [PubMed] [Google Scholar]
- 12.Hess TM, Tate CS. Adult age differences in explanations and memory for behavioral information. Psychol Aging 1991;6: 86-92 [DOI] [PubMed] [Google Scholar]
- 13.Rice EG, Okun MA. Older readers' processing of medical information that contradicts their beliefs. J Geront Psychol Sci 1994;49: P119-28 [DOI] [PubMed] [Google Scholar]
- 14.Okun MA, Rice GE. The effects of personal relevance of topic and information type on older adults' accurate recall of written medical passages about osteoarthritis. J Aging Health 2001;13: 410-29 [DOI] [PubMed] [Google Scholar]
- 15.Wessel I, Van der Kooy P, Merckelbach H. Differential recall of central and peripheral details of emotional slides is not a stable phenomenon. Memory 2000;8: 95-109 [DOI] [PubMed] [Google Scholar]
- 16.Schramke CJ, Bauer RM. State-dependent learning in older and younger adults. Psychol Aging 1997;12: 255-62 [DOI] [PubMed] [Google Scholar]
- 17.Shapiro DE, Boggs SR, Melamed BG, Graham-Pole J. The effect of varied physician affect on recall, anxiety, and perceptions in women at risk for breast cancer: an analogue study. Health Psychol 1992;11: 61-6 [DOI] [PubMed] [Google Scholar]
- 18.McHugh P, Lewis S, Ford S, et al. The efficacy of audiotapes in promoting psychological well-being in cancer patients: a randomised, controlled trial. Br J Cancer 1995;71: 388-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ford S, Fallowfield L, Hall A, Lewis S. The influence of audiotapes on patient participation in the cancer consultation. Eur J Cancer 1995;31A: 2264-9 [DOI] [PubMed] [Google Scholar]
- 20.Bradshaw PW, Ley P, Kincey JA, Bradshaw J. Recall of medical advice. Br J Soc Clin Psychol 1975;14: 55-62 [DOI] [PubMed] [Google Scholar]
- 21.Thomson AM, Cunningham SJ, Hunt NP. A comparison of information retention at an initial orthodontic consultation. Eur J Orthod 2001;23: 169-78 [DOI] [PubMed] [Google Scholar]
- 22.Blinder D, Rotenberg L, Peleg M, Taicher S. Patient compliance to instructions after oral surgical procedures. Int J Oral Maxillofac Surg 2001;30: 216-19 [DOI] [PubMed] [Google Scholar]
- 23.Delp C, Jones J. Communicating information to patients: the use of cartoon illustrations to improve comprehension of instructions. Acad Emerg Med 1996;3: 264-70 [DOI] [PubMed] [Google Scholar]
- 24.Houts PS, Witmer JT, Egeth HE, Loscalzo MJ, Zabora JR. Using pictographs to enhance recall of spoken medical instructions II. Patient Educ Couns 2001;43: 231-42 [DOI] [PubMed] [Google Scholar]
- 25.Barkhordar A, Pollard D, Hobkirk JA. A comparison of written and multimedia material for informing patients about dental implants. Dent Update 2000;27: 80-4 [DOI] [PubMed] [Google Scholar]
- 26.Bakker DA, Blais D, Reed E, Vaillancourt C, Gervais S, Beaulieu P. Descriptive study to compare patient recall of information: nursetaught versus video supplement. Can Oncol Nurs J 1999;9: 115-20 [DOI] [PubMed] [Google Scholar]