Abstract
Chorea is a rare manifestation of poisoning. We report an index case of a young woman who developed generalized chorea following propiconazole toxin ingestion. As large series on neurological complications of toxic compounds are difficult to be compiled, it is of interest to report our experience. This report adds one more compound to the increasing list of toxic chorea.
KEY WORDS: Chorea, fungicide, propiconazole
Introduction
Chorea may be the manifestation of a wide variety of degenerative, vascular, metabolic, or toxic disorders involving the central nervous system, in which dysfunction of the basal ganglia, particularly of the striatum, is generally assumed to be responsible.[1] We report an index case of generalized chorea secondary to the ingestion of propiconazole toxin (fungicide) in a young female. In this case, generalized chorea is an uncommon clinical entity recognized in a case of poisoning.
Case Report
The patient was a 35-year-old lady who was a known case of primary juvenile myoclonic epilepsy, on treatment with valproate (800 mg/day) for 7 years. She was found in unconscious state at home by the family, who then took her to the emergency department of another facility. In view of prior history of epilepsy, she was treated with anti-epileptic drugs but with no improvement. She developed respiratory failure and was subsequently intubated and mechanically ventilated. Her routine laboratory investigations were normal. Three days later, due to persistent unresponsive neurological condition, she was referred to our tertiary care hospital for further management.
At admission, her Glasgow Coma Scale was E2M5V1, with bilateral small-sized pupils (2 mm, reacting), heart rate of 64/min, blood pressure 90/60 mmHg on inotropic support with norepinephrine 2 μg/kg/min and dopamine 8 μg/kg/min. She was drowsy but localizing painful stimulus. She was extensively reevaluated for persistent altered state of consciousness. Blood biochemistry and metabolic profile were normal with total leukocyte count-12,000/mm3, RBS-85 mg/dl, blood and urine culture were sterile. Chest X-ray and echocardiography were normal. Electroencephalogram was done to rule out status epilepticus while the patient was on valproate (blood level-80) and no sedatives. It revealed 3–5 Hz, 30–40 microvolt delta activity. Magnetic resonance imaging (MRI) brain with contrast, and cytological and biochemical analysis of cerebrospinal fluid were normal.
On day 3 of her illness when inotropes had been tapered, her heart rate was in the range of 50–58/min. Bradycardia (even with inotropic support) along with small-sized pupils raised the suspicion of intoxication. Serum cholinesterase, opioids, and amphetamine levels were sent. Furthermore, relatives were redirected to look for any evidence of suspicious compound at home. Cholinesterase levels were very low (134) along with an empty bottle of propiconazole toxin (fungicide) found at home, confirming the diagnosis of intoxication. She was managed with infusion of atropine. She was tracheostomized and weaned from the ventilator. Over next 2 days, she became alert and was hemodynamically stable. However, on the 9th day of her illness, she developed irregular random flowing movements from one part of the body to another, suggesting generalized chorea [Video 1]. A detailed family history was not positive for any chorea/choreiform movements suggestive of inherited degenerative disorders. The patient was extensively evaluated for other acquired cause of chorea, but her hematological investigations including peripheral blood film, biochemical, thyroid function, serum valproate levels, and vasculitic workup were negative and repeat MRI brain and computed tomography CT abdomen were also normal. She was treated with clonazepam (2 mg), tetrabenazine (75 mg), and risperidone (2 mg) with partial improvement in chorea.
Discussion
Our case depicts initial diagnostic dilemma, which is frequent problem in intoxication as history is often concealed. Our referral area, Northern Province of India, largely has an agriculture background. Hence, insecticide poisonings are relatively a common occurrence with wide spectrum of neurological presentations which may affect the function of the central and peripheral nervous system. Clinical manifestations vary greatly, and include movement disorders such as secondary parkinsonism and a wide range of hyperkinetic disorders and even delayed neuropathy.[2]
Propiconazole is the triazole class of fungicide and is available as an emulsifiable concentrate ready-to-use liquid [Figure 1]. It is also known as DMI or demethylation-inhibiting fungicide, due to its binding with and inhibition of 14-alpha-demethylase enzyme.[3] To the best of our knowledge, this is the index case of generalized chorea following intoxication with propiconazole (fungicide). The probable mechanism may be excessive acetylcholine activity in the nigrostriatal system due to inactivation of acetylcholinesterase by propiconazole. Within the nigrostriatal network, caudate nucleus and globus pallidus are particularly rich in cholinergic neurons causing less inhibition of pallidothalamic fibers and generalized choreiform movements.
Figure 1.
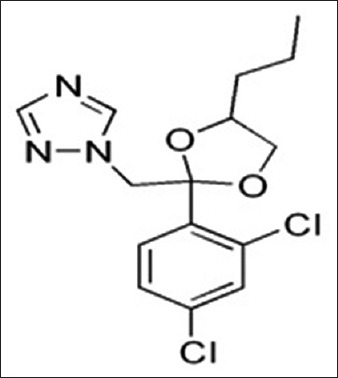
Chemical structure of propiconazole (C15H17Cl2N3O2)
The neurological manifestation with propiconazole intoxication is not reported in literature. Only few cases of extrapyramidal manifestations following cholinergic intoxication secondary to organophosphate poisoning (OPC) have been described. In the three cases described by Joubert et al., the extrapyramidal manifestations were limited to choreiform movements.[2] Bhatt et al. and Kumar and Subrahmanyam also report acute and reversible parkinsonism following intoxication with OPCs.[4,5]
Conclusion
Although exact mechanism of action of propiconazole is not clear, but circumstantial evidence, low cholinesterase levels, and response to anticholinergic treatment sufficiently support our diagnosis. With delayed development of generalized chorea as neurological sequelae, propiconazole may be added as another compound in the causal list of toxic chorea widening the spectrum of acquired toxic causes of chorea still further. In a country like ours, where poisonings are frequent exposure to toxic agents should be considered as a differential in the cause of hyperkinetic movement disorders.
Video available on: www.jpgmonline.com
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Miyasaki JM. Chorea caused by toxins. Handb Clin Neurol. 2011;100:335–46. doi: 10.1016/B978-0-444-52014-2.00026-4. [DOI] [PubMed] [Google Scholar]
- 2.Joubert J, Joubert PH, van der Spuy M, van Graan E. Acute organophosphate poisoning presenting with choreo-athetosis. J Toxicol Clin Toxicol. 1984;22:187–91. doi: 10.3109/15563658408992554. [DOI] [PubMed] [Google Scholar]
- 3.Tahir YF, Nour SM. Oral toxicity of agro-fungicides: Tilt (propiconazole), bayleton (triadimefon) and their mixture to Nubian goats. Sudan JMS. 2009;3:213–21. [Google Scholar]
- 4.Bhatt MH, Elias MA, Mankodi AK. Acute and reversible parkinsonism due to organophosphate pesticide intoxication: Five cases. Neurology. 1999;52:1467–71. doi: 10.1212/wnl.52.7.1467. [DOI] [PubMed] [Google Scholar]
- 5.Kumar AP, Subrahmanyam D. Acute reversible parkinsonism following accidental exposure to organophosphate insecticides. Int Nutr Pharmacol Neurol Dis. 2013;3:70–2. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


