Abstract
The morbidity and toxicity associated with current intensive treatment protocols for acute lymphoblastic leukemia in childhood become even more important as the vast majority of children can be cured and become long-term survivors. Osteonecrosis is one of the most common therapy-related and debilitating side effects of anti-leukemic treatment and can adversely affect long-term quality of life. Incidence and risk factors vary substantially between study groups and therapeutic regimens. We therefore analyzed 22 clinical trials of childhood acute lymphoblastic leukemia in terms of osteonecrosis incidence and risk factors. Adolescent age is the most significant risk factor, with patients >10 years old at the highest risk. Uncritical modification or even significant reduction of glucocorticoid dosage cannot be recommended at this stage. A novel and innovative approach to reduce osteonecrosis-associated morbidity might be systematic early screening for osteonecrosis by serial magnetic resonance images. However, discriminating patients at risk of functional impairment and debilitating progressive joint disease from asymptomatic patients still remains challenging.
Background
Survival of children with acute lymphoblastic leukemia (ALL) has dramatically improved over the last decades due to the progressive intensification of multi-agent chemotherapy. Currently, more than 90% of children and adolescents can be cured and become long-term survivors.1,2 Thus, the long-term adverse effects of treatment become increasingly important. Osteonecrosis is one of the most common and debilitating therapy-related side effects of anti-leukemic treatment and can adversely affect long-term quality of life.3 Incidence (1.6–17.6%) and risk factors for the development of osteonecrosis have been investigated in many studies, but results vary substantially between study groups and therapeutic regimens.4–9 Adolescence is the most consistently identified and most significant risk factor, with patients >10 years old at the highest risk.7–11 As this dominates all other therapy-related and patient-specific risk factors, it suggests that the underlying pathophysiology for the development of osteonecrosis likely has to be attributed to age-specific factors ultimately affecting bone morphology, metabolism, and/or nourishment. This may be due, at least in part, to increased end-organ susceptibility caused by a markedly increased growth rate and specific hormonal changes in this period of life.12
Current concepts of osteonecrosis pathogenesis
The early events leading to osteonecrosis are poorly understood. Multiple factors for the development of osteonecrosis are discussed, which probably act synergistically in the context of anti-leukemic treatment. All contributing mechanisms finally lead to an imbalance between the actual and the required bone perfusion, which may be related to intravascular clotting/embolism (intraluminal obliteration), increased marrow pressure (extraluminal obliteration), and direct blood vessel injury. In addition, the direct toxic effects of chemotherapy on bone marrow and bone cells may disturb bone integrity and contribute to osteonecrosis.13
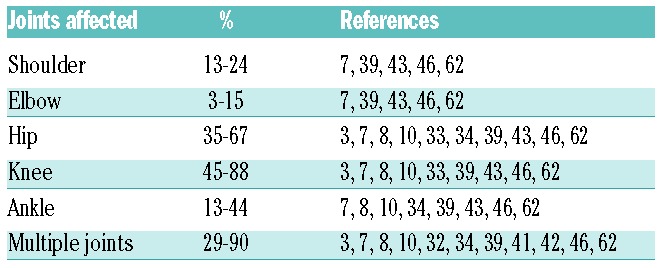
Although the underlying disease and the exposure to damaging agents, such as glucocorticoids (GCs), are of a systemic nature, osteonecrosis predominantly develops in vulnerable areas such as long bone epiphysis and metaphysis (Table 1).
Table 1.
Distribution pattern of osteonecrosis in children and adolescents with ALL (acute lymphoblastic leukemia) according to published data.
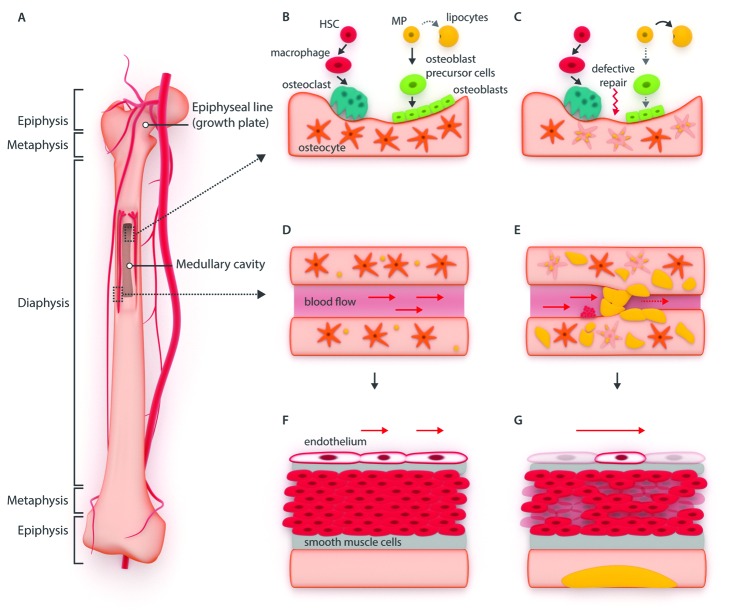
Disrupted blood supply to the bone
Bone is a highly perfused tissue. The blood supply to the endosteal cavity is delivered by the nutrient artery, which enters through the diaphysis and branches into marrow sinusoids, and finally ramifies into small vessels in the cortex. The epiphyseal and metaphyseal vascular zones of prepubertal children are separated by the growth plate, which receives its blood supply only from dia- and epiphyseal vessels and anastomoses in the perichondrium, respectively (Figure 1). Neural, humoral, and hormonal factors contribute to the regulation of vascular resistance, and, thus, influence the blood supply to the bone.
Figure 1.
Schematic illustration of osteonecrosis pathogenesis. (A) Blood supply of bone is delivered by the nutrient arteries, which enter in the dia- and epiphysis and branch into marrow sinusoids. The growth plate receives its blood supply from dia- and epiphyseal vessels and anastomoses in the perichondrium, respectively. (B–C) Bone growth occurs by endochondral bone formation and bone modeling. The bone tissue is continuously turning over, with osteoclasts and osteoblasts being fundamentally involved in this process. In the context of osteonecrosis development, osteoblast differentiation from mesenchymal progenitor cells is disturbed by gradual lipid accumulation within osteoblasts and osteocytes and increased cell death, both mainly induced by GCs (glucocorticosteroids), and results in defective bone repair. (D–E) Bone perfusion is disturbed by intraluminal obliteration induced by lipid emboli and intravascular coagulation and extraluminal obliteration induced by intramedullary lipocyte proliferation and lipid hypertrophy. Intraosseous compartment syndrome may develop, increasingly reducing intramedullary blood flow and predisposing for coagulation in the intraosseous blood vessels. (F–G) Direct blood vessel injury and disruption of the vascular supply to the bone is mainly mediated by damaging effects on the endothelial and smooth muscle cells of nutrient arteries and venous vessels. HSC: hematopoietic stem cell; MP: mesenchymal progenitor cell.
Intraluminal obliteration
Liver-to-bone marrow lipid emboli trigger thrombotic and/or embolic ischemia, resulting in cell damage and subsequent bone marrow edema (BME). This leads to ischemic necrosis of metabolically active/vulnerable regions such as the epiphyses.14,15 By triggering intravascular coagulation in the intraosseous microcirculation (capillaries and venous sinusoids), increased prothrombotic factors (e.g., thrombin, cholesterol) contribute to the development of osteonecrosis.16
Extraluminal obliteration
Intramedullary lipocyte proliferation (compromising the sinusoidal circulation) and osteocyte lipid hypertrophy (e.g., related to GCs or dyslipidemia), proliferation of histiocytes in storage disorders (e.g., Gaucher disease), or bleeding within the bone marrow cause increased intramedullary pressure. Because of the inelasticity of the bone, intraosseous compartment syndrome develops, further reducing intramedullary blood flow and predisposing for hemostasis in the intraosseous blood vessels.17–19
The epiphyseal plate of the immature bone during childhood growth provides elasticity to compensate for the increasing intraosseous pressure, while with epiphyseal closure during adolescence, the intramedullary pressure increases and can be passed through to the epiphyseal part of the bone.
Direct blood vessel injury
Disruption of the vascular supply to the bone is a preceding event to glucocorticoid-induced osteonecrosis in a murine model.20 This is mainly mediated by damaging effects on the endothelial and smooth muscle cells of nutrient arteries and venous vessels, which promote further vascular stasis, ischemia, and arteriopathy.21
Altered integrity of bone structure
Longitudinal bone growth occurs by endochondral bone formation, particularly in the growth plates at the proximal and distal ends of long bones, whereas bone growth in width occurs by bone modeling. During remodeling, the bone tissue is continuously turned over. Both osteoclasts and osteoblasts are fundamentally involved in this process and influence bone development during childhood and adolescence.22,23 During the pubertal growth spurt, particularly, the bone length increases. Furthermore, sexual hormones impact bone (re)modeling and, thus, affect bone strength and mass.22
Direct cell toxicity
GCs are reported to induce gradual lipid accumulation within osteocytes, osteocyte death, increased osteocyte apoptosis, suppression of osteoblastic differentiation of marrow stem cells, decreased cell division of osteoblasts near osteonecrosis lesions, and increased mesenchymal stem cell differentiation into lipocytes at the expense of osteogenesis.14,20,24–29
Defective bone repair
During revascularization following ischemia, changes occur in the hematopoietic marrow, fatty marrow, and vascular structures. The surrounding bony architecture within the area of infarction becomes weakened by resorption of subchondral dead bone along the reactive interface. The repair process at least temporarily compromises bone mass integrity. Continued cellular stress, mechanical load/weight-bearing stress fractures, collapse of the chondral bony support system, cartilage disintegration, and deformity of articular surfaces may ultimately lead to progressive joint collapse and degenerative joint disease.30,31
Osteonecrosis in the context of anti-leukemic treatment
Osteonecrosis has only recently been recognized as one of the most significant toxicities of anti-leukemic treatment (see Tables 2 and 3). This is in stark contrast to historical experience in which osteonecrosis was considered a rare complication of ALL therapy. In 2000, Mattano et al. reported on a large retrospective multi-center survey on symptomatic osteonecrosis in children with high-risk ALL treated according to the CCG-1882 protocol between 1989 and 1995.7 With a cumulative osteonecrosis incidence of 9.3% and orthopedic interventions in 24% of the affected children, this report highlighted, for the first time, osteonecrosis as a serious problem of modern chemotherapy. A trend to better outcome after occurrence of osteonecrosis further emphasized the challenge of treating these children with therapy that maximizes cure rates but is associated with unanticipated and – to a certain extent – unacceptable toxicity. Notably, this was chronologically associated with the introduction of dexamethasone for delayed intensification with improved survival rates, particularly in the most affected group of adolescents. A retrospective study on two consecutive DFCI trials reported a slightly lower osteonecrosis incidence (7%) but an even higher rate (30%) of orthopedic interventions,32 the former speculatively owed to the fact that dexamethasone was only given in DFCI trial 91-01. A magnetic resonance imaging (MRI) screening based prospective study determined a significantly higher osteonecrosis incidence (15.5%) without the impact of steroid dose or dexamethasone administration (see Table 4).33 This was even exceeded by a prospective study analyzing the Nordic ALL protocols, which reported an osteonecrosis incidence as high as 24%, identified by MRI screening at the end of treatment.8 As the earlier reports were based on retrospective data collection, the true osteonecrosis incidence was most likely underestimated. However, 6 of the 17 affected patients reported by Ribeiro et al.33 and 16 of the 23 patients reported by Niinimäki et al.8 were only detected by MRI, and the patients remained asymptomatic until the end of the study. Two independent retrospective reports on Berlin-Frankfurt-Muenster (BFM)-based trials with quite similar therapy (AIEOP-ALL 95,34 ALL-BFM 9510) from the late 90s determined a much lower, but almost identical, osteonecrosis incidence of 1.6–1.8%. However, in patients aged ≥10 years, the osteonecrosis incidence was reported to be 8.9% and even higher in those ≥15 years (16.7%).10 Thus, when comparing these studies, one has to keep in mind that appropriate age groups must be compared, and that there might be a significant difference in the patients’ age distribution in each study, which certainly influences the overall incidence of osteonecrosis. In line with this, Mattano et al.7 only evaluated high-risk patients, but young patients usually make up only about one third of the high-risk group. However, the osteonecrosis incidence in these retrospective studies was probably underestimated as this toxicity was unanticipated, and therefore not listed as a reportable event on the case report forms. Furthermore, the treating physicians in those days were not aware of this toxicity, and a standardized diagnostic approach was lacking. However, if one assumes that osteonecrosis was underreported in these trials, and exposure to dexamethasone increases the risk of osteonecrosis, particularly during delayed intensification, one would expect a much higher incidence of osteonecrosis in the subsequent trial ALL-BFM 2000. Notwithstanding that the overall incidence of osteonecrosis was substantially higher (4.7%)35 and exceeded that reported in the trial NOPHO ALL-2008 (3.1%),36 and EORTC-CLG 58951 (2.5%),37 it still remained lower than that of CCG,38,39 DFCI,40,41 DCOG,42,43 and UK44,45 trials. Even when comparing only the group of older patients, the incidence (in prospective studies on symptomatic osteonecrosis) is much higher but still varies substantially between the trials (CCG-196139 9.9% 10–15 years, 20% 16–21 years; UKALL 200345 16% 10–15 years, 15% >16 years; NOPHO ALL200836 11% 10–14 years, 6.5% 15–17 years; ALL-BFM 200035 14.5% 10–15 years; DFCI-ALL 00-0141 14% 10–18 years). However, a factor which remained consistent throughout all the studies was that older children and adolescents are at a much higher risk of developing osteonecrosis.
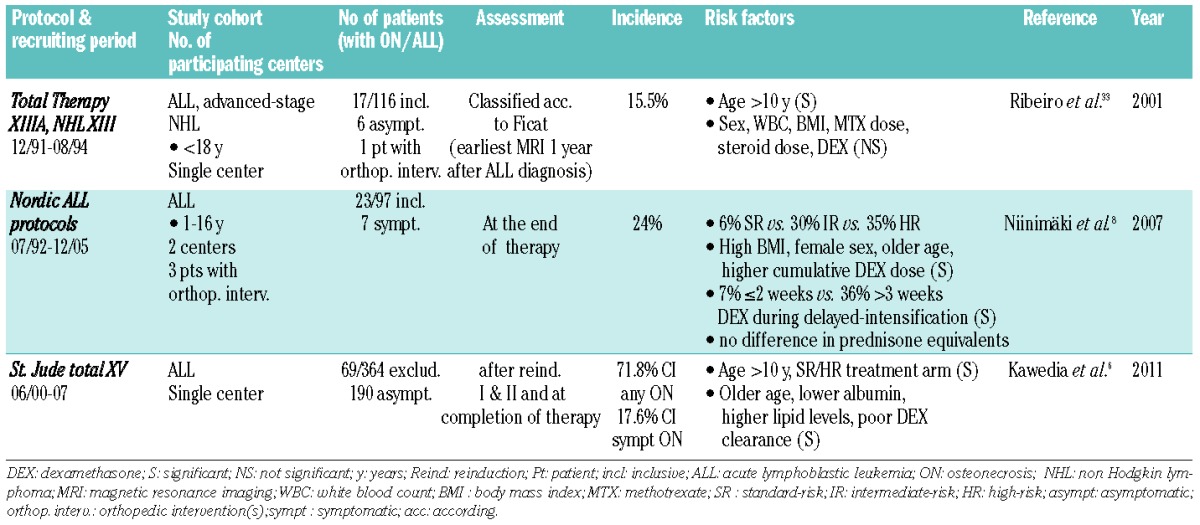
Table 2.
Overview of retrospective studies reporting incidences and risk factors for symptomatic osteonecrosis in children and adolescents with ALL.
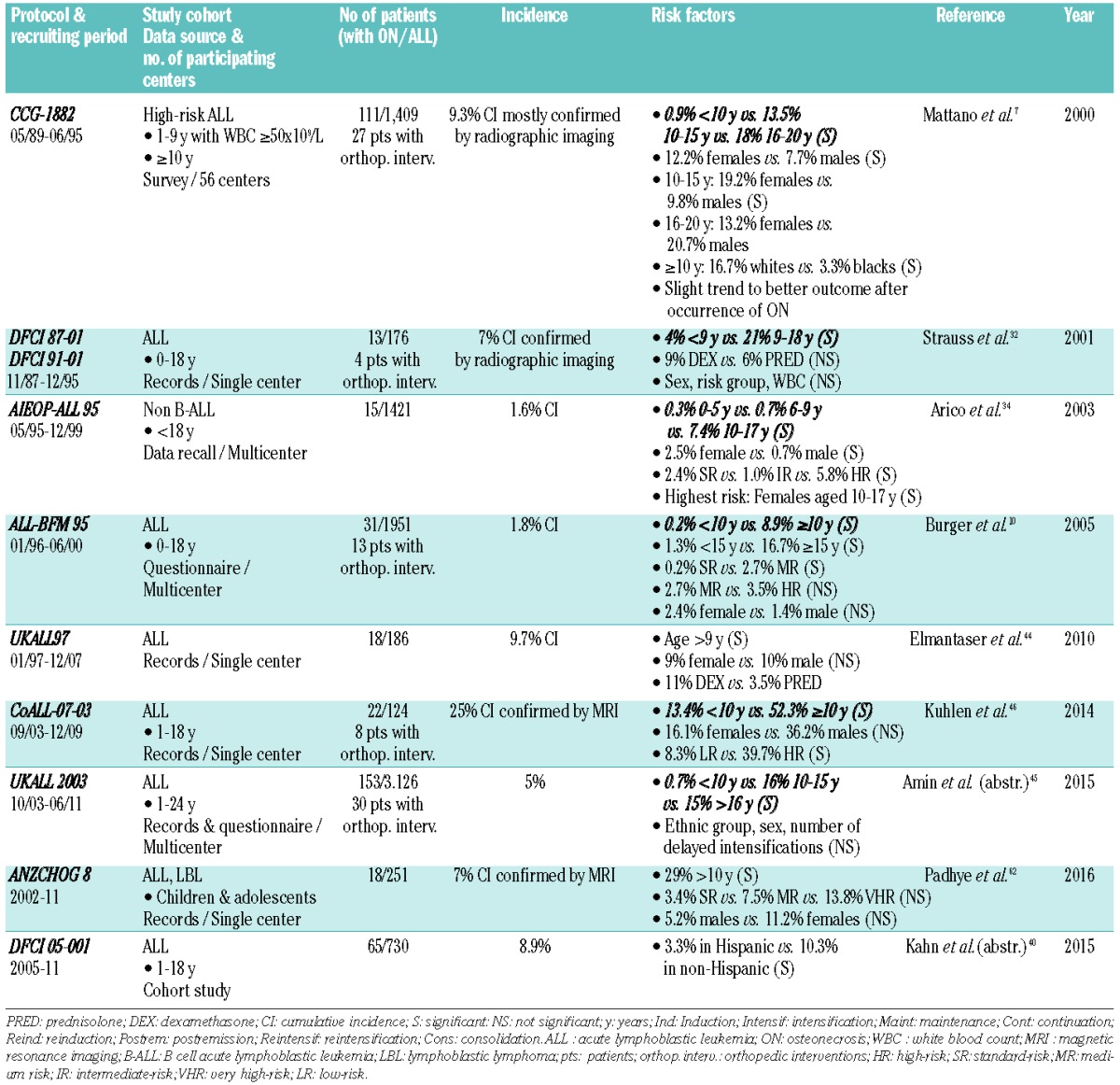
Table 3.
Overview of prospective studies reporting incidences and risk factors for symptomatic osteonecrosis in children and adolescents with ALL.
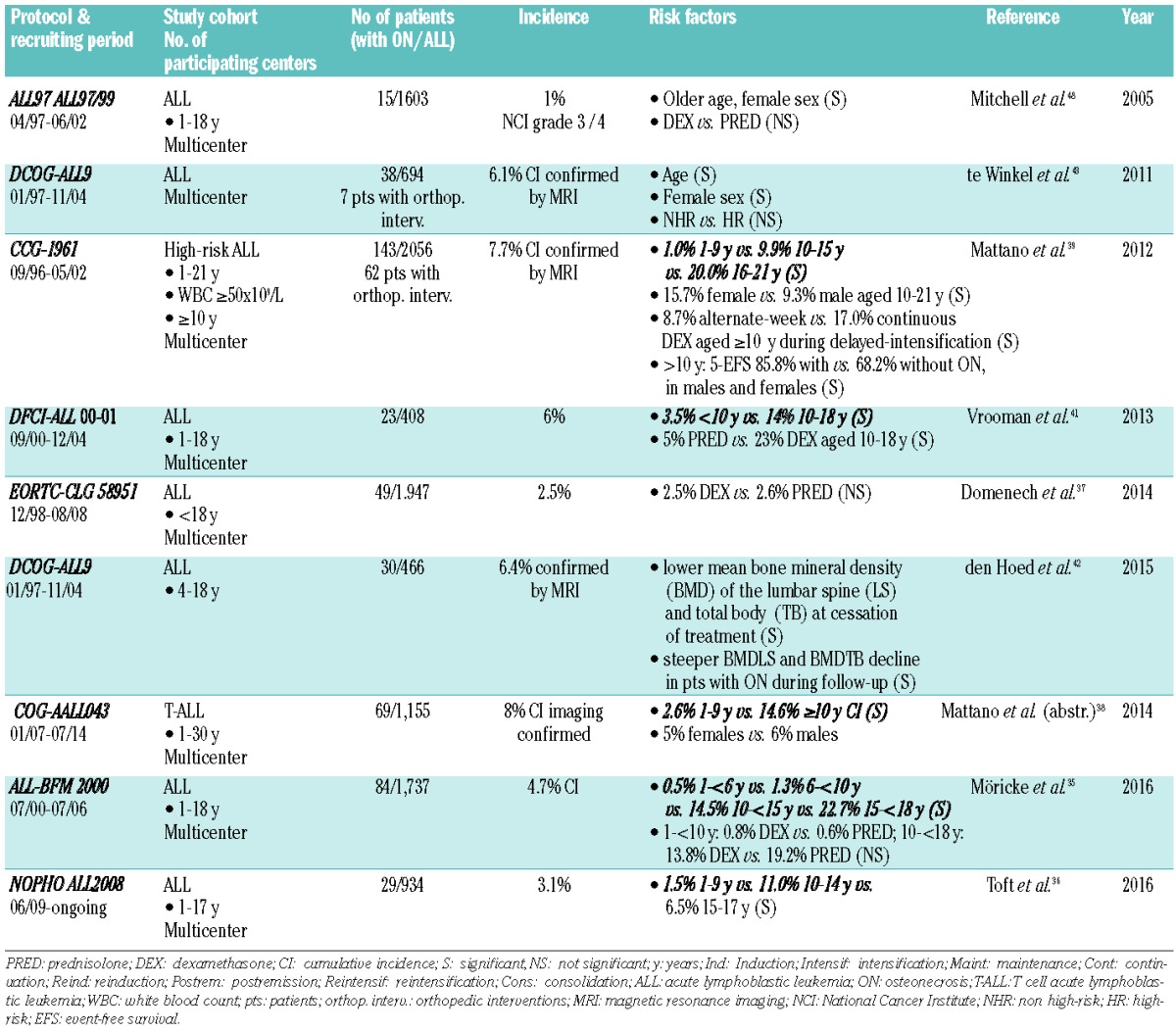
Table 4.
Overview of MRI screening studies for osteonecrosis in children and adolescents with ALL.
It may be speculated that these differences in osteonecrosis incidence may be due to reporting bias, incompleteness of data, and different methods of analysis, and might further be substantially influenced by treatment related or non-treatment related risk factors.
Risk factors
As osteonecrosis seems to be a particularly predominant problem in children and adolescents diagnosed with acute lymphoblastic leukemia, leukemia itself might contribute to the development of osteonecrosis. Lymphoblasts are known to have bone-resorbing effects. However, neither areas of leukemic infiltration of bone26 nor white blood count at diagnosis32,33,46 and immunophenotype (T- versus B-cell leukemia)38,46 are associated with osteonecrosis risk.
Treatment related risk factors
Glucocorticoids
GCs are major contributors to the development of osteonecrosis, with the cumulative dose of received GCs correlating with the risk of osteonecrosis (see Table 5).3,47 In study AALL0232,38 an excess risk of osteonecrosis was found in older patients with dexamethasone at 10 mg/m2/d × 14 days (24%) versus prednisone at 60 mg/m2/d × 28 days (16%). Most studies3,5,32,37,48 report no obviously increased risk of osteonecrosis with the administration of dexamethasone compared to prednisone, even in the risk group of older patients (for example in ALL-BFM 2000,35 the osteonecrosis incidence in patients treated with dexamethasone was 14% versus 19% with prednisone). To make the different trials immediately comparable, many authors calculated the equipotent anti-inflammatory doses of dexamethasone and compared cumulative prednisone-equivalent doses of GCs, showing no significant correlation with the occurrence of osteonecrosis.10,33,46 However, as dexamethasone is known to be more toxic to the skeletal system than prednisone, and low dexamethasone clearance was linked to severe osteonecrosis,6 this approach might conceal differences. On the contrary, the toxic effects of dexamethasone during delayed intensification may be additive or synergistic with those of GCs administered during the induction phase. Reducing the duration of exposure to dexamethasone seems to reduce the risk for symptomatic osteonecrosis and outweighs the cumulative dose as a risk factor for the development of treatment-related osteonecrosis.8,39,49
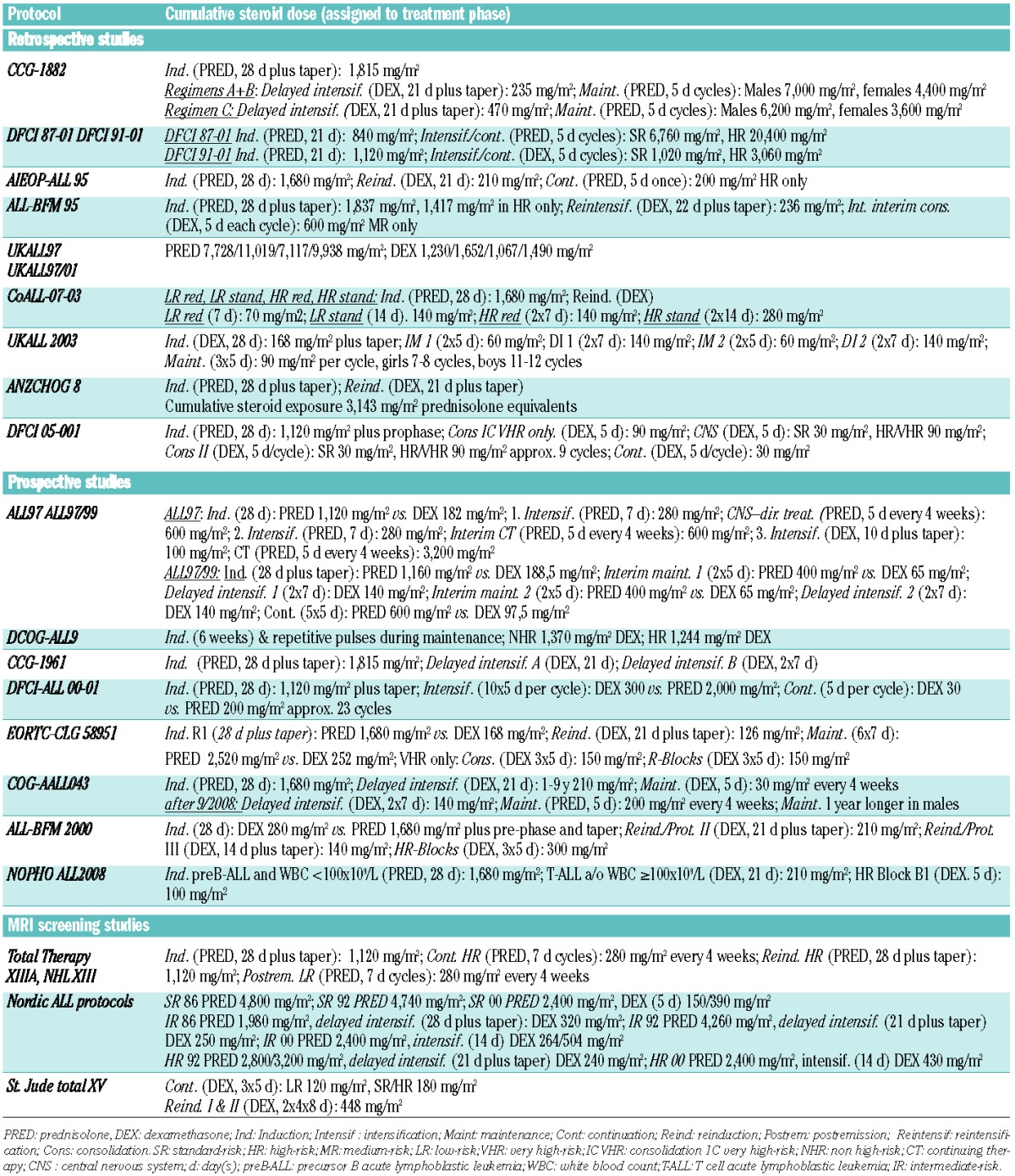
Table 5.
Overview of cumulative corticosteroid doses in pediatric ALL (acute lymphoblastic leukemia) studies.
GCs might affect antithrombin and protein S levels, with the latter further worsened by the additional administration of asparaginase, thus leading to hypercoagulability.50
Nonglucocorticoid drugs
Given the varying frequencies of osteonecrosis in different ALL treatment regimens, nonglucocorticoid drugs such as asparaginase (ASP) and methotrexate (MTX) may additionally modify the risk of osteonecrosis.51 ASP treatment leads to increased plasma concentrations of dexamethasone,6,51,52 whereas ASP allergy is associated with decreased systemic exposure to ASP and with decreased risk of osteonecrosis.53 These effects might further be influenced by the different preparations of ASP used and, to some extent, explain the above-mentioned conflicting results regarding the risk of osteonecrosis in older patients, with the administration of dexamethasone compared to prednisone in trial ALL-BFM 2000 (native asparaginase)35 and AALL0232 (pegylated asparaginase).38
High-dose MTX can damage the growth plate and primary bone, and the long-term use of MTX can reduce primary bone formation, likely due to decreased osteoblast function as well as increased osteoclast formation and function.54,55 Methylenetetrahydrofolate reductase (MTHFR) polymorphisms can lead to mild to moderate increases in plasma homocysteine levels with homocysteinemia, leading to an increased risk of venous thrombosis.56,57 Alkylating agents may harm gonadal function and lead to primary hypogonadism, which compromises bone mineralization if not adequately treated.58 Ifosfamide can induce renal tubulopathy/Fanconi syndrome, and may subsequently manifest as hypophosphatemic rickets, compromising bone structure.59 Due to hypercoagulability, vascular endothelial damage, and disruption of bone formation, purine antimetabolites can impair proliferation of chondrocytes.60
Other treatment related factors
Compared to chemotherapy alone, patients undergoing hematopoietic stem cell transplantation are at an increased risk of developing osteonecrosis.3 Furthermore, total body irradiation (TBI) and chronic graft-versus-host disease correlate with the incidence of osteonecrosis.61
Non-treatment related factors
Osteonecrosis occurs more frequently in white patients than in black patients and in non-Hispanics than in Hispanics.7,9,40 Girls between the ages of 10 and 14 years old are especially affected by osteonecrosis, whereas boys are at the highest risk above the age of 15 years.7,46 There is no clear consensus on a risk difference between males and females. Even in groups that used essentially the same treatment regime, there are disparate results in this regard.7,10,32,34,45,46,62 Inconsistent results have also been reported for the influence of obesity and BMI as risk factors.8,63,64
Genetic risk factors
Various genetic risk factors for the development of osteonecrosis in children with ALL and in steroid-induced osteonecrosis have been identified in numerous studies using candidate gene approaches and large genome-wide association studies (GWAS).6,9,65–68
Polymorphisms in the plasminogen activator inhibitor-1 (PAI-1) gene were initially reported to be associated with an increased risk of osteonecrosis,4,66 but this finding could not be confirmed by subsequent GWAS studies.68 Likewise, findings about polymorphisms involved in lipid homeostasis (acid phosphatase locus 1, ACP1),6 antifolate pharmacodynamics (thymidylate synthetase, TYMS), and steroid hormone response (vitamin D receptor, VDR), have been reported to be associated with osteonecrosis,9 but were not reproducible in GWAS studies.68
According to recent GWAS studies, the glutamate receptor pathway seems to be of crucial importance for the pathogenesis of osteonecrosis in patients with prolonged exposure to corticosteroids. Mechanical load opens mechanosensitive calcium channels in osteocytes, leading to exocytosis of glutamate, which activates osteoblast receptors and impairs endothelial barrier function.67–70 In addition, SNPs in adipogenesis pathways and in enhancers active in mesenchymal stem cells are significantly associated with osteonecrosis development.67 Bone morphogenetic protein (BMP) is toxic to vascular smooth muscle and is released in response to bone damage and mechanical stress.
To summarize, osteonecrosis risk is influenced by germline polymorphisms in genes linked to pharmacodynamics of chemotherapy, bone metabolism, adipogenesis, glutamate signaling pathway, and mesenchymal stem cell differentiation. However, given the lack of a single consistent genetic factor being undoubtedly identified, predictive diagnostic testing that helps to evaluate the risk of osteonecrosis development is not established. Even in the context of genetic variants that increase the risk of osteonecrosis, the occurrence of osteonecrosis remains highly dependent on the patient’s age and the specific therapeutic regimen, and, conversely, genetic risk factors significantly depend on the patient’s age.
Adolescence
Age is the most consistently identified and most significant risk factor, with patients ≥10 years old at the highest risk across treatment regimens and study groups (Table 1).7–11,43,62 In contrast, the incidence is lower in adults undergoing ALL therapy.36 Thus, the pathogenesis of osteonecrosis is likely strongly associated with factors being most prominent in adolescent age, thereby causing the highest vulnerability for osteonecrosis in this age.
There are several adolescent physiological processes that differ fundamentally from younger children and older individuals. These can mainly be attributed to hormonal changes that might lead to increased osteonecrosis susceptibility via interaction with different mechanisms, such as increased local metabolic/perfusion requirements, skeletal maturation (e.g., growth plate structure and development), the coagulation system, or osseous blood vessel supply.
All these processes are induced by the beginning and maturation of sexual hormone production and a physiological peak of growth hormone production during puberty.
Increasing sexual hormone and especially estrogen concentrations during puberty have procoagulatory effects, thus adolescence is associated with the highest risk of the development of venous thromboembolism.71 Additional risk factors, such as thrombophilia or hypofibrinolysis, can further increase the risk of thrombosis.25,72 In experimental settings, testosterone increases nitrogen monoxide release of endothelial cells, and inhibits platelet aggregation.73 Estrogen further promotes intracortical bone remodeling. Bone material is added to the endosteal surface, increasing cortical density and bone mass during puberty.22 These estrogenic effects result in a peak in bone mass gain, and the procoagulatory effects of estrogens predispose adolescents to an imbalance between osseous metabolic/blood supply demands and actual osseous blood supply. This effect might further explain the trend to witness more osteonecrosis in females compared to males.
The growth hormone/IGF1 axis is physiologically stimulated during puberty, 1.5– to 3-fold compared to pre- and postpubertal individuals.74 The IGF1 level peaks in females at an average of 14 years, and in males at 15 years of age.75 Peak growth velocity/pubertal growth spurt can be expected at 12 years of age in females, and at 14 years of age in males.76 This leads to excessive metabolic activity in growth plates and bones, such as increased oxygen consumption with increased hypoxic effects in growth plates.77–79 This helps to explain why areas of bone with late epiphyseal closure and extensive contribution to pubertal length growth, such as long limb bones, are predominantly affected by osteonecrosis.7
Pubertal epiphyseal maturation and ossification progressively reduce mechanically compliant areas in bone architecture, which might then lose their ability to compensate for increased bone marrow pressure.
Concentrations of pro- and anticoagulant factors change crucially during growth.80,81 Major turning points occur after the first six months of life, and between adolescence (11–16 years) and adulthood.82 Coagulant factors (II, V, VII, IX, X, XI, XII, bleeding time), anticoagulant factors (α2M, HCII, Protein C), and the fibrinolytic system (plasminogen, TPA, PAI) are substantially modulated during adolescence and differ significantly from adult levels.80 Both elevated estrogen and testosterone levels further increase the impact of underlying thrombophilia (Factor V Leiden, MTHFR polymorphisms, prothrombinemia, Protein C deficiency, Protein S deficiency hyperhomocysteinemia), and hypofibrinolysis (PAI polymorphisms, increased plasminogen activator inhibitor activity).4,25,66,83 In addition, lifestyle factors, such as smoking, substance abuse, obesity, and use of oral hormonal contraceptives gain importance during adolescence and further contribute to venous thromboembolism (VTE) risk.71 For example, contraceptives with high estrogen content influence the protein C pathway, with subsequently increased activated protein C (APC) resistance84 and platelet aggregation.85 This likely increases the risk of intraluminal obliteration and ischemia in the rapidly growing bone.
Prevention and screening
Long continuous exposure during delayed intensification plays a pivotal role in the development of osteonecrosis. Therefore, this was modified in two trials, either by replacing continuous with alternate-week dexamethasone or by entirely reducing the duration of administration.8,39 osteonecrosis incidence in patients treated according to the altered dexamethasone schedule was significantly reduced. However, high-risk ALL patients with osteonecrosis had a 17.6% better event-free survival than patients without osteonecrosis.39 Hence, modifying treatment must be carefully monitored in future prospective trials.
A different approach to reduce osteonecrosis-associated debilitating long-term effects is early screening for osteonecrosis by MRI to prevent functional impairment. This has been carried out by Ribeiro et al.33 one year after diagnosis of ALL, by Niinimäki et al.86 at the end of therapy, by Kaste et al.87 at 6.5 and 9 months from diagnosis and at completion of therapy, and by Kawedia et al.6 after reinduction I and II and at completion of therapy. The number of patients diagnosed with radiographic osteonecrosis was high (15.5%,33 24%86 and 71.8%,6 respectively) with a substantial proportion of patients remaining asymptomatic until the end of the study (35%, 70%, and 73%, respectively). Kaste et al.87 further distinguished between limited and extensive (involving more than 30% of the head surface) femoral head osteonecrosis, the latter being a crucial predictor of joint infraction. As radiological classification of osteonecrosis was not uniform, comparability of these results is limited. Furthermore, a recent study by Niinimäki et al. identified critical deficiencies in all available radiological osteonecrosis classification systems and recommended a new, joint-specific classification system.88
With a cumulative incidence of 71.8% of any osteonecrosis, the study by Kawedia et al.6 highlights the need for further research, with particular regard to followup, as the course of osteonecrosis may be transient and reversible and some changes may resolve without symptoms. Even when patients present with joint pain and radiographic changes, the clinical course remains unpredictable. Thus, identifying patients at risk of functional impairment and debilitating progressive joint disease still remains challenging.
Precise prospective evaluation of side effects and toxicity in children undergoing treatment for ALL in childhood is therefore an important aspect of modern therapy to reduce compromising outcome after successful treatment. Hence, we initiated the multi-center OPAL trial (Osteonecrosis in Pediatric patients with Acute lymphoblastic Leukemia and lymphoblastic lymphoma [LBL]), which is still ongoing. In this trial, we prospectively evaluate children aged ≥10 years diagnosed with ALL or LBL, who are treated according to the AIEOP-BFM 2009 and the CoALL-08-09 protocol with a combination of MRI screening and symptom-oriented anamnesis and functional examination at defined time points during ALL treatment. The trial aims to define the proportion of children who can be diagnosed with early asymptomatic osteonecrosis by MRI and subsequently develop symptomatic osteonecrosis, to identify critical time points of osteonecrosis development during ALL treatment, and to describe the natural course of asymptomatic osteonecrosis lesions only identified by MRI. These data are still lacking and are mandatory for the subsequent evaluation of interventions aimed at preventing osteonecrosis progression and functional impairment. These aspects strongly underline the need for intensive future research in the field of pediatric osteonecrosis.
Conclusions
Osteonecrosis is the most common therapy-related side effect in children with acute lymphoblastic leukemia. Better understanding of the associated therapy-related and non-therapy-related risk factors is needed to improve prediction, management, and, preferably, prevention of this sequelae.
Supplementary Material
Acknowledgments
This work was supported by the German Childhood Cancer Foundation (DKS 2011.11).
The authors would like to thank Dr. Jessica I. Höll for her critical reading of the manuscript and editorial assistance.
Footnotes
Check the online version for the most updated information on this article, online supplements, and information on authorship & disclosures: www.haematologica.org/content/101/11/1295
References
- 1.Schrappe M, Moricke A, Reiter A, et al. Key treatment questions in childhood acute lymphoblastic leukemia: results in 5 consecutive trials performed by the ALL-BFM study group from 1981 to 2000. Klin Padiatr. 2013;225 Suppl 1:S62–72. [DOI] [PubMed] [Google Scholar]
- 2.Pui CH, Campana D, Pei D, et al. JCO 2015: Childhood Acute Lymphoblastic Leukemia: Progress Through CollaborationTreating. N Engl J Med. 2009;360(26):2730–2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Girard P, Auquier P, Barlogis V, et al. Symptomatic osteonecrosis in childhood leukemia survivors: prevalence, risk factors and impact on quality of life in adulthood. Haematologica. 2013;98(7):1089–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bond J, Adams S, Richards S, Vora A, Mitchell C, Goulden N. Polymorphism in the PAI-1 (SERPINE1) gene and the risk of osteonecrosis in children with acute lymphoblastic leukemia. Blood. 2011;118(9): 2632–2633. [DOI] [PubMed] [Google Scholar]
- 5.Kadan-Lottick NS, Dinu I, Wasilewski-Masker K, et al. Osteonecrosis in adult survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2008;26(18):3038–3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kawedia JD, Kaste SC, Pei D, et al. Pharmacokinetic, pharmacodynamic, and pharmacogenetic determinants of osteonecrosis in children with acute lymphoblastic leukemia. Blood. 2011;117(8): 2340–2347; quiz 2556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mattano LA, Jr, Sather HN, Trigg ME, Nachman JB. Osteonecrosis as a complication of treating acute lymphoblastic leukemia in children: a report from the Children’s Cancer Group. J Clin Oncol. 2000;18(18):3262–3272. [DOI] [PubMed] [Google Scholar]
- 8.Niinimaki RA, Harila-Saari AH, Jartti AE, et al. High body mass index increases the risk for osteonecrosis in children with acute lymphoblastic leukemia. J Clin Oncol. 2007;25(12):1498–1504. [DOI] [PubMed] [Google Scholar]
- 9.Relling MV, Yang W, Das S, et al. Pharmacogenetic risk factors for osteonecrosis of the hip among children with leukemia. J Clin Oncol. 2004;22(19):3930–3936. [DOI] [PubMed] [Google Scholar]
- 10.Burger B, Beier R, Zimmermann M, Beck JD, Reiter A, Schrappe M. Osteonecrosis: a treatment related toxicity in childhood acute lymphoblastic leukemia (ALL)–experiences from trial ALL-BFM 95. Pediatr Blood Cancer. 2005;44(3):220–225. [DOI] [PubMed] [Google Scholar]
- 11.Lackner H, Benesch M, Moser A, et al. Aseptic osteonecrosis in children and adolescents treated for hemato-oncologic diseases: a 13-year longitudinal observational study. J Pediatr Hematol Oncol. 2005;27(5):259–263. [DOI] [PubMed] [Google Scholar]
- 12.Bukowinski AJ, Burns KC, Parsons K, Perentesis JP, O’Brien MM. Toxicity of Cancer Therapy in Adolescents and Young Adults (AYAs). Semin Oncol Nurs. 2015;31(3):216–226. [DOI] [PubMed] [Google Scholar]
- 13.Lafforgue P. Pathophysiology and natural history of avascular necrosis of bone. Joint Bone Spine. 2006;73(5):500–507. [DOI] [PubMed] [Google Scholar]
- 14.Jones JP., Jr Fat embolism, intravascular coagulation, and osteonecrosis. Clin Orthop Relat Res. 1993;(292):294–308. [PubMed] [Google Scholar]
- 15.Laroche M. Intraosseous circulation from physiology to disease. Joint Bone Spine. 2002;69(3):262–269. [DOI] [PubMed] [Google Scholar]
- 16.Jones JP., Jr Coagulopathies and osteonecrosis. Acta Orthop Belg. 1999;65 Suppl 1:5–8. [PubMed] [Google Scholar]
- 17.Kaste SC, Karimova EJ, Neel MD. Osteonecrosis in children after therapy for malignancy. AJR Am J Roentgenol. 2011;196(5):1011–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miyanishi K, Yamamoto T, Irisa T, et al. Bone marrow fat cell enlargement and a rise in intraosseous pressure in steroid-treated rabbits with osteonecrosis. Bone. 2002;30(1):185–190. [DOI] [PubMed] [Google Scholar]
- 19.Motomura G, Yamamoto T, Miyanishi K, Yamashita A, Sueishi K, Iwamoto Y. Bone marrow fat-cell enlargement in early steroid-induced osteonecrosis–a histomorphometric study of autopsy cases. Pathol Res Pract. 2005;200(11–12):807–811. [DOI] [PubMed] [Google Scholar]
- 20.Janke LJ, Liu C, Vogel P, et al. Primary epiphyseal arteriopathy in a mouse model of steroid-induced osteonecrosis. Am J Pathol. 2013;183(1):19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Assouline-Dayan Y, Chang C, Greenspan A, Shoenfeld Y, Gershwin ME. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002;32(2):94–124. [PubMed] [Google Scholar]
- 22.Schoenau E. Bone mass increase in puberty: what makes it happen? Horm Res. 2006;65 Suppl 2:2–10. [DOI] [PubMed] [Google Scholar]
- 23.Schoenau E, Saggese G, Peter F, et al. From bone biology to bone analysis. Horm Res. 2004;61(6):257–269. [DOI] [PubMed] [Google Scholar]
- 24.Weinstein RS, Nicholas RW, Manolagas SC. Apoptosis of osteocytes in glucocorticoid-induced osteonecrosis of the hip. J Clin Endocrinol Metab. 2000;85(8):2907–2912. [DOI] [PubMed] [Google Scholar]
- 25.Glueck CJ, Freiberg RA, Fontaine RN, Tracy T, Wang P. Hypofibrinolysis, thrombophilia, osteonecrosis. Clin Orthop Relat Res. 2001;(386):19–33. [DOI] [PubMed] [Google Scholar]
- 26.Ojala AE, Paakko E, Lanning FP, Lanning M. Osteonecrosis during the treatment of childhood acute lymphoblastic leukemia: a prospective MRI study. Med Pediatr Oncol. 1999;32(1):11–17. [DOI] [PubMed] [Google Scholar]
- 27.Wang GJ, Sweet DE, Reger SI, Thompson RC. Fat-cell changes as a mechanism of avascular necrosis of the femoral head in cortisone-treated rabbits. J Bone Joint Surg Am. 1977;59(6):729–735. [PubMed] [Google Scholar]
- 28.Kawai K, Tamaki A, Hirohata K. Steroid-induced accumulation of lipid in the osteocytes of the rabbit femoral head. A histochemical and electron microscopic study. J Bone Joint Surg Am. 1985;67(5):755–763. [PubMed] [Google Scholar]
- 29.Yin L, Li YB, Wang YS. Dexamethasone-induced adipogenesis in primary marrow stromal cell cultures: mechanism of steroid-induced osteonecrosis. Chin Med J (Engl). 2006;119(7):581–588. [PubMed] [Google Scholar]
- 30.Mankin HJ. Nontraumatic necrosis of bone (osteonecrosis). N Engl J Med. 1992;326(22): 1473–1479. [DOI] [PubMed] [Google Scholar]
- 31.Sala A, Mattano LA, Jr, Barr RD. Osteonecrosis in children and adolescents with cancer - an adverse effect of systemic therapy. Eur J Cancer. 2007;43(4):683–689. [DOI] [PubMed] [Google Scholar]
- 32.Strauss AJ, Su JT, Dalton VM, Gelber RD, Sallan SE, Silverman LB. Bony morbidity in children treated for acute lymphoblastic leukemia. J Clin Oncol. 2001;19(12):3066–3072. [DOI] [PubMed] [Google Scholar]
- 33.Ribeiro RC, Fletcher BD, Kennedy W, et al. Magnetic resonance imaging detection of avascular necrosis of the bone in children receiving intensive prednisone therapy for acute lymphoblastic leukemia or non-Hodgkin lymphoma. Leukemia. 2001;15(6): 891–897. [DOI] [PubMed] [Google Scholar]
- 34.Arico M, Boccalatte MF, Silvestri D, et al. Osteonecrosis: An emerging complication of intensive chemotherapy for childhood acute lymphoblastic leukemia. Haematologica. 2003;88(7):747–753. [PubMed] [Google Scholar]
- 35.Möricke A, Zimmermann M, Valsecchi MG, et al. Dexamethasone vs. prednisone in induction treatment of pediatric ALL: results of the randomized trial AIEOP-BFM ALL 2000. Blood. 2016;127(17):2101–2112. [DOI] [PubMed] [Google Scholar]
- 36.Toft N, Birgens H, Abrahamsson J, et al. Toxicity profile and treatment delays in NOPHO ALL2008-comparing adults and children with Philadelphia chromosome-negative acute lymphoblastic leukemia. Eur J Haematol. 2016;96(2):160–169. [DOI] [PubMed] [Google Scholar]
- 37.Domenech C, Suciu S, De Moerloose B, et al. Dexamethasone (6 mg/m2/day) and prednisolone (60 mg/m2/day) were equally effective as induction therapy for childhood acute lymphoblastic leukemia in the EORTC CLG 58951 randomized trial. Haematlogica. 2014;99(7):1220–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mattano LA, Devidas M, Chen S, et al. Effect of High-Dose Methotrexate (HD-MTX) Vs Capizzi Methotrexate/Pegaspargase (C-MTX/ASNase) on Osteonecrosis (ON) Incidence in Children and Young Adults with T-Acute Lymphoblastic Leukemia (TALL): Results of Children’s Oncology Group (COG) Study AALL0434. Blood. 2014;124(21):3649–3649. [Google Scholar]
- 39.Mattano LA, Jr, Devidas M, Nachman JB, et al. Effect of alternate-week versus continuous dexamethasone scheduling on the risk of osteonecrosis in paediatric patients with acute lymphoblastic leukaemia: results from the CCG-1961 randomised cohort trial. Lancet Oncol. 2012;13(9):906–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kahn J, Barrera S, Davila R, et al. Higher Incidence of Treatment-Related Toxicities in Non-Hispanic Patients Undergoing Therapy for Newly Diagnosed Pediatric Acute Lymphoblastic Leukemia on Dana-Farber Cancer Institute ALL Consortium Protocol 05-001. Blood. 2015;126(23):248–248. [Google Scholar]
- 41.Vrooman LM, Stevenson KE, Supko JG, et al. Postinduction dexamethasone and individualized dosing of Escherichia Coli L-asparaginase each improve outcome of children and adolescents with newly diagnosed acute lymphoblastic leukemia: results from a randomized study–Dana-Farber Cancer Institute ALL Consortium Protocol 00-01. J Clin Oncol. 2013;31(9):1202–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.den Hoed MA, Pluijm SM, Te Winkel ML, et al. Aggravated bone density decline following symptomatic osteonecrosis in children with acute lymphoblastic leukemia. Haematologica. 2015;100(12):1564–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.te Winkel ML, Pieters R, Hop WC, et al. Prospective study on incidence, risk factors, and long-term outcome of osteonecrosis in pediatric acute lymphoblastic leukemia. J Clin Oncol. 2011;29(31):4143–4150. [DOI] [PubMed] [Google Scholar]
- 44.Elmantaser M, Stewart G, Young D, Duncan R, Gibson B, Ahmed SF. Skeletal morbidity in children receiving chemotherapy for acute lymphoblastic leukaemia. Arch Dis Child. 2010;95(10):805–809. [DOI] [PubMed] [Google Scholar]
- 45.Amin NL, Kinsey S, Feltbower R, et al. Analysis of Long-Term Outcomes, Management and Prevalence of Osteonecrosis in UKALL 2003: 3.5% of Adolescents and Young Adults over 10 Years of Age with Acute Lymphoblastic Leukaemia Required Hip Replacement. Blood. 2015;126(23):2083–2083. [Google Scholar]
- 46.Kuhlen M, Moldovan A, Krull K, Meisel R, Borkhardt A. Osteonecrosis in paediatric patients with acute lymphoblastic leukaemia treated on Co-ALL-07-03 trial: a single centre analysis. Klin Padiatr. 2014;226(3):154–160. [DOI] [PubMed] [Google Scholar]
- 47.McAvoy S, Baker KS, Mulrooney D, et al. Corticosteroid dose as a risk factor for avascular necrosis of the bone after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;16(9):1231–1236. [DOI] [PubMed] [Google Scholar]
- 48.Mitchell CD, Richards SM, Kinsey SE, et al. Benefit of dexamethasone compared with prednisolone for childhood acute lymphoblastic leukaemia: results of the UK Medical Research Council ALL97 randomized trial. Br J Haematol. 2005;129(6):734–745. [DOI] [PubMed] [Google Scholar]
- 49.van den Heuvel-Eibrink MM, Pieters R. Steroids and risk of osteonecrosis in ALL: take a break. Lancet Oncol. 2012;13(9):855–857. [DOI] [PubMed] [Google Scholar]
- 50.te Winkel ML, Appel IM, Pieters R, van den Heuvel-Eibrink MM. Impaired dexamethasone-related increase of anticoagulants is associated with the development of osteonecrosis in childhood acute lymphoblastic leukemia. Haematologica. 2008;93(10):1570–1574. [DOI] [PubMed] [Google Scholar]
- 51.Yang L, Panetta JC, Cai X, et al. Asparaginase may influence dexamethasone pharmacokinetics in acute lymphoblastic leukemia. J Clin Oncol. 2008;26(12):1932–1939. [DOI] [PubMed] [Google Scholar]
- 52.Hanada T, Horigome Y, Inudoh M, Takita H. Osteonecrosis of vertebrae in a child with acute lymphocytic leukaemia during L-asparaginase therapy. Eur J Pediatr. 1989;149(3):162–163. [DOI] [PubMed] [Google Scholar]
- 53.Liu C, Kawedia JD, Cheng C, et al. Clinical utility and implications of asparaginase antibodies in acute lymphoblastic leukemia. Leukemia. 2012;26(11):2303–2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fan C, Cool JC, Scherer MA, et al. Damaging effects of chronic low-dose methotrexate usage on primary bone formation in young rats and potential protective effects of folinic acid supplementary treatment. Bone. 2009;44(1):61–70. [DOI] [PubMed] [Google Scholar]
- 55.Schwartz AM, Leonidas JC. Methotrexate osteopathy. Skeletal Radiol. 1984;11(1):13–16. [DOI] [PubMed] [Google Scholar]
- 56.Refsum H, Wesenberg F, Ueland PM. Plasma homocysteine in children with acute lymphoblastic leukemia: changes during a chemotherapeutic regimen including methotrexate. Cancer Res. 1991;51(3):828–835. [PubMed] [Google Scholar]
- 57.Whayne TF., Jr Methylenetetrahydrofolate reductase C677T polymorphism, venous thrombosis, cardiovascular risk, and other effects. Angiology. 2015;66(5):401–404. [DOI] [PubMed] [Google Scholar]
- 58.Müller HL, Langer T, Schnabel D. Growth and bone metabolism after oncological disease in childhood and adolescence. Monatsschr Kinderheilkd. 2015;163(2):135–141. [Google Scholar]
- 59.Loebstein R, Atanackovic G, Bishai R, et al. Risk factors for long-term outcome of ifosfamide-induced nephrotoxicity in children. J Clin Pharmacol. 1999;39(5):454–461. [PubMed] [Google Scholar]
- 60.Robson H, Anderson E, Eden OB, Isaksson O, Shalet S. Chemotherapeutic agents used in the treatment of childhood malignancies have direct effects on growth plate chondrocyte proliferation. J Endocrinol. 1998;157(2):225–235. [DOI] [PubMed] [Google Scholar]
- 61.Faraci M, Calevo MG, Lanino E, et al. Osteonecrosis after allogeneic stem cell transplantation in childhood. A case-control study in Italy. Haematologica. 2006;91(8):1096–1099. [PubMed] [Google Scholar]
- 62.Padhye B, Dalla-Pozza L, Little D, Munns C. Incidence and outcome of osteonecrosis in children and adolescents after intensive therapy for acute lymphoblastic leukemia (ALL). Cancer Med. 2016;5(5):960–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kaste SC, Shidler TJ, Tong X, et al. Bone mineral density and osteonecrosis in survivors of childhood allogeneic bone marrow transplantation. Bone Marrow Transplant. 2004;33(4):435–441. [DOI] [PubMed] [Google Scholar]
- 64.Sharma S, Yang S, Rochester R, et al. Prevalence of osteonecrosis and associated risk factors in children before allogeneic BMT. Bone Marrow Transplant. 2011;46(6):813–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Asano T, Takahashi KA, Fujioka M, et al. Genetic analysis of steroid-induced osteonecrosis of the femoral head. J Orthop Sci. 2003;8(3):329–333. [DOI] [PubMed] [Google Scholar]
- 66.French D, Hamilton LH, Mattano LA, Jr, et al. A PAI-1 (SERPINE1) polymorphism predicts osteonecrosis in children with acute lymphoblastic leukemia: a report from the Children’s Oncology Group. Blood. 2008;111(9):4496–4499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Karol SE, Mattano LA, Jr, Yang W, et al. Genetic risk factors for the development of osteonecrosis in children under age 10 treated for acute lymphoblastic leukemia. Blood. 2016;127(5):558–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Karol SE, Yang W, Van Driest SL, et al. Genetics of glucocorticoid-associated osteonecrosis in children with acute lymphoblastic leukemia. Blood. 2015;126(15): 1770–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sharp CD, Houghton J, Elrod JW, et al. N-methyl-D-aspartate receptor activation in human cerebral endothelium promotes intracellular oxidant stress. Am J Physiol Heart Circ Physiol. 2005;288(4):H1893–1899. [DOI] [PubMed] [Google Scholar]
- 70.Brakspear KS, Mason DJ. Glutamate signaling in bone. Front Endocrinol (Lausanne). 2012;3:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nowak-Gottl U, Kenet G. Challenging aspects of managing hemostasis in adolescents. Acta Haematol. 2014;132(3-4):326–330. [DOI] [PubMed] [Google Scholar]
- 72.Glueck CJ, Friedman J, Hafeez A, Hassan A, Wang P. Testosterone, thrombophilia, thrombosis. Blood Coagul Fibrinolysis. 2014;25(7):683–687. [DOI] [PubMed] [Google Scholar]
- 73.Campelo AE, Cutini PH, Massheimer VL. Testosterone modulates platelet aggregation and endothelial cell growth through nitric oxide pathway. J Endocrinol. 2012;213(1): 77–87. [DOI] [PubMed] [Google Scholar]
- 74.Rose SR, Municchi G, Barnes KM, et al. Spontaneous growth hormone secretion increases during puberty in normal girls and boys. J Clin Endocrinol Metab. 1991;73(2): 428–435. [DOI] [PubMed] [Google Scholar]
- 75.Brabant G, von zur Muhlen A, Wuster C, et al. Serum insulin-like growth factor I reference values for an automated chemiluminescence immunoassay system: results from a multicenter study. Horm Res. 2003;60(2):53–60. [DOI] [PubMed] [Google Scholar]
- 76.Prader A, Largo RH, Molinari L, Issler C. Physical growth of Swiss children from birth to 20 years of age. First Zurich longitudinal study of growth and development. Helv Paediatr Acta Suppl. 1989;52:1–125. [PubMed] [Google Scholar]
- 77.Shim KS. Pubertal growth and epiphyseal fusion. Ann Pediatr Endocrinol Metab. 2015;20(1):8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stewart AJ, Houston B, Farquharson C. Elevated expression of hypoxia inducible factor-2alpha in terminally differentiating growth plate chondrocytes. J Cell Physiol. 2006;206(2):435–440. [DOI] [PubMed] [Google Scholar]
- 79.Emons J, Chagin AS, Hultenby K, et al. Epiphyseal Fusion in the Human Growth Plate Does not Involve Classical Apoptosis. Pediatr Res. 2009;66(6):654–659. [DOI] [PubMed] [Google Scholar]
- 80.Andrew M, Vegh P, Johnston M, Bowker J, Ofosu F, Mitchell L. Maturation of the hemostatic system during childhood. Blood. 1992;80(8):1998–2005. [PubMed] [Google Scholar]
- 81.Monagle P, Barnes C, Ignjatovic V, et al. Developmental haemostasis. Impact for clinical haemostasis laboratories. Thromb Haemost. 2006;95(2):362–372. [DOI] [PubMed] [Google Scholar]
- 82.Jaffray J, Young G. Developmental hemostatsis: clinical implications from the fetus to the adolescent. Pediatr Clin North Am. 2013;60(6):1407–1417. [DOI] [PubMed] [Google Scholar]
- 83.Sprengers ED, Kluft C. Plasminogen activator inhibitors. Blood. 1987;69(2):381–387. [PubMed] [Google Scholar]
- 84.Tans G, Bouma BN, Buller HR, Rosing J. Changes of hemostatic variables during oral contraceptive use. Semin Vasc Med. 2003;3(1):61–68. [DOI] [PubMed] [Google Scholar]
- 85.Jayachandran M, Miller VM. Ovariectomy upregulates expression of estrogen receptors, NOS, and HSPs in porcine platelets. Am J Physiol Heart Circ Physiol. 2002;283(1):H220–226. [DOI] [PubMed] [Google Scholar]
- 86.Niinimaki RA, Harila-Saari AH, Jartti AE, et al. Osteonecrosis in children treated for lymphoma or solid tumors. J Pediatr Hematol Oncol. 2008;30(11):798–802. [DOI] [PubMed] [Google Scholar]
- 87.Kaste SC, Pei D, Cheng C, et al. Utility of early screening magnetic resonance imaging for extensive hip osteonecrosis in pediatric patients treated with glucocorticoids. J Clin Oncol. 2015;33(6):610–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Niinimaki T, Niinimaki J, Halonen J, Hanninen P, Harila-Saari A, Niinimaki R. The classification of osteonecrosis in patients with cancer: validation of a new radiological classification system. Clin Radiol. 2015;70(12):1439–1444. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.