Abstract
The feasibility and efficacy of high-dose melphalan followed by autologous hematopoietic stem cell transplantation in newly diagnosed elderly patients with multiple myeloma was analyzed prospectively. Fifty-six multiple myeloma patients, aged 65 years or over, from 6 French centers were studied. The induction therapy was bortezomib-based in combination with dexamethasone and either thalidomide, cyclophosphamide or lenalidomide, for 4–6 cycles. Peripheral blood stem cells were collected after high-dose cyclophosphamide plus G-CSF or G-CSF alone, with plerixafor if needed. The conditioning regimen consisted of melphalan at 140 mg/m2 in 18 patients (36%) and 200 mg/m2 in 32 (64%). Three months post autologous hematopoietic stem cell transplantation, a 2-month consolidation phase with either lenalidomide plus dexamethasone or bortezomib-based combination therapy was allowed, but maintenance treatment was not given. All but 6 patients underwent autologous hematopoietic stem cell transplantation and 3 had tandem transplantations. The treatment-related mortality was 0% at 100 days post transplantation. Sixty-eight percent received consolidation therapy following transplantation. The best response achieved was 40% complete response, 36% very good partial response, and 18% partial response. After a median follow up of 21 months (range 6–31), the estimated progression-free and overall survival rates at two years were 76% [95%CI: (61.6–94.1)] and 88% [95%CI: (76.7–100)], respectively. The higher dose of melphalan (200 mg/m2) afforded superior progression-free and overall survival rates. This prospective study provides evidence for the safety and efficacy of autologous hematopoietic stem cell transplantation as a first-line treatment approach in elderly multiple myeloma patients. (clinicaltrials.gov identifier: 01671826)
Introduction
Two-thirds of multiple myeloma (MM) patients are over 65 years of age at the time of diagnosis. As the general population becomes older, this proportion is destined to increase. Autologous stem cell transplantation (ASCT) is a standard form of treatment for myeloma patients under the age of 65 years1 but is a controversial procedure for patients over this age, mostly because of a suspected increase in toxicity.2–5
In elderly patients, only two randomized studies have compared a transplant versus a no transplant approach. Palumbo et al. first reported a benefit of intermediate-dose (100 mg/m2) melphalan (HDT) plus ASCT for patients aged between 65 and 70 years.6 In contrast, the IFM 99-06 study did not show any benefit of transplantation after melphalan (100 mg/m2) as compared to a combination of melphalan, prednisone and thalidomide.7 However, many subsequent studies, mostly retrospective or registry-based and performed before the latest drugs became available, have shown encouraging results with ASCT in patients over 65 years of age.8–13 Some investigators even reported a successful outcome for patients over the age of 70.14–17 A recent European Society for Blood and Marrow Transplantation (EBMT) study showed that, over the past few years, ASCT was performed more often, especially in the elderly population, and with better outcomes.18
There has been a considerable decrease in toxicity due to better patient selection and improved supportive care. Nowadays, geriatric assessment is routinely performed in the clinic, which helps the treatment decision-making process.19,20 Furthermore, new drugs have emerged, such as the immunomodulatory drugs lenalidomide and pomalidomide and proteasome inhibitors like carfilzomib and ixazomib.21 These, used as single agents or more often in combination, together with the previous standard treatment, are stimulating a new interest in ASCT for elderly patients.22
Therefore, we initiated a multicenter prospective observational study, from 2013 to 2015 in 6 French centers, which included 56 myeloma patients aged 65 years or over, 50 of whom underwent ASCT after bortezomib-based induction.
Methods
Patients
Patients were eligible if they were over 65 years of age and presented with symptomatic, measurable, newly diagnosed multiple myeloma. Between September 2012 and September 2014, a total of 56 newly diagnosed elderly MM patients were treated in 6 institutions in France. The diagnosis, clinical staging and prognostic score of MM were based on the Durie and Salmon staging system and the International Staging System (ISS).23,24 The Seattle group‘s hematopoietic cell transplantation specific comorbidity index (HCT-CI) was used to score the comorbidities.25 Baseline demographics, clinical and laboratory data at diagnosis, and information on treatment and response were collected prospectively and recorded in the EBMT Promise (Med B) database. Patients gave their informed consent to the study. This prospective observational study was approved by the Ethics Committee/Institutional Review Board of Paris Île de France V and registered as clinicaltrials.gov identifier: 01671826.
Treatment
The primary objective was to assess patient outcome and especially any treatment toxicity. In each case, therapy was decided by the physician responsible for the patient. The short-term use of dexamethasone for emergent disease control was not considered as conventional chemotherapy. ASCT was performed as upfront therapy after induction, provided the disease was not progressive.
Induction regimen
The induction regimen was bortezomib-based, either bortezomib plus dexamethasone (VD), bortezomib plus thalidomide plus dexamethasone (VTD), bortezomib plus cyclophosphamide plus dexamethasone (VCD), bortezomib plus lenalidomide plus dexamethasone (VRD), or melphalan plus prednisone plus bortezomib (MPV). Patients received 4–6 21-day cycles according to the local guidelines of each center.
Stem cell mobilization and collection
Peripheral blood hematopoietic stem cells were mobilized using the procedure in routine practice at each center. The cells were collected either after administration of high-dose cyclophosphamide plus G-CSF or in the steady state after administration of G-CSF alone, plus plerixafor if needed.
Conditioning regimen and supportive care
To be eligible for transplantation, the patient had to have adequate organ function and no uncontrolled infection. The conditioning regimen consisted of melphalan (140 or 200 mg/m2), given over one or two days, according to the physician’s choice. Tandem ASCT was allowed and supportive care was given according to the current protocol in each institution.
Consolidation/maintenance
A short 2-month consolidation phase three months post ASCT was allowed (lenalidomide-dexamethasone, VD, VTD, VCD or VRD). No maintenance treatment was given.
Engraftment and disease response
The date of neutrophil engraftment was defined as the first of three consecutive days when the absolute neutrophil count was over 0.5×109/L. The date of platelet engraftment was defined as the first of seven consecutive days when the platelet count was over 20×109/L, independent of any platelet transfusions. Response, disease progression and relapse were defined according to the International Myeloma Working Group uniform response criteria.26
Assessment of transplant-related toxicity
Transplant-related mortality (TRM) was defined as the percentage of patients dying without relapse or progression within a given time interval following transplantation. Non-hematologic toxicity was assessed by the local physician. Variables analyzed included bacterial and viral infections, gastro-enteric, renal (serum creatinine) and hepatic (bilirubin, alanine transaminase and aspartate transaminase) function, and cardiotoxicity.
Statistical analysis
Patients’ demographic and clinical characteristics were summarized using the median and range for continuous variables, and counts and percentages for categorical variables.
Progression-free survival (PFS) was defined as the time from the date of starting treatment to the date of disease progression or death from any cause. Overall survival (OS) was defined as the time from the date of starting treatment to death from any cause. PFS and OS curves were calculated using the Kaplan-Meier method. We examined the relationship between outcomes and potential prognostic factors. The differences between the curves were evaluated using the log-rank test. Variables included baseline patient factors, and prognostic and treatment-related factors. The selection rule for multivariate analysis was a threshold of 20%. A multivariate Cox proportional hazards model was used to determine the independent predictors associated with extended OS.
Statistical analysis was performed with a 2-sided α = 0.05 and a 95% confidence interval. Data were analyzed using R software, v.2.15.1, and IBM SPSS statistics v.22.
Results
Patients’ characteristics
Patients’ demographics and disease characteristics are summarized in Table 1. At the time of diagnosis, median age was 67 years (range 64–74) with 23% of patients over 70 years of age; 30 males and 26 females. The myeloma immunoglobulin subtypes were: IgG (n=29), IgA (n=15), light chain (n=10), other (n=2). The Salmon and Durie stage was III in 89% of cases (n=47) and ISS scores were I (n=18, 35%), II (n=19, 37%), and III (n=14, 27%). High-risk cytogenetic features [t (4;14) and/or del17p] were found in 9 cases (16%). Although 10% of patients had a serum creatinine level of more than 176 micromol/L, none underwent hemodialysis. Twenty-eight patients (5%) received VTD, 9 (17%) VCD, 9 (17%) VD, 4 (7%) MPV and 3 (6%) VRD, with 11 patients (21%) requiring two lines of induction and one three lines.
Table 1.
Patients’ characteristics at diagnosis and transplantation.
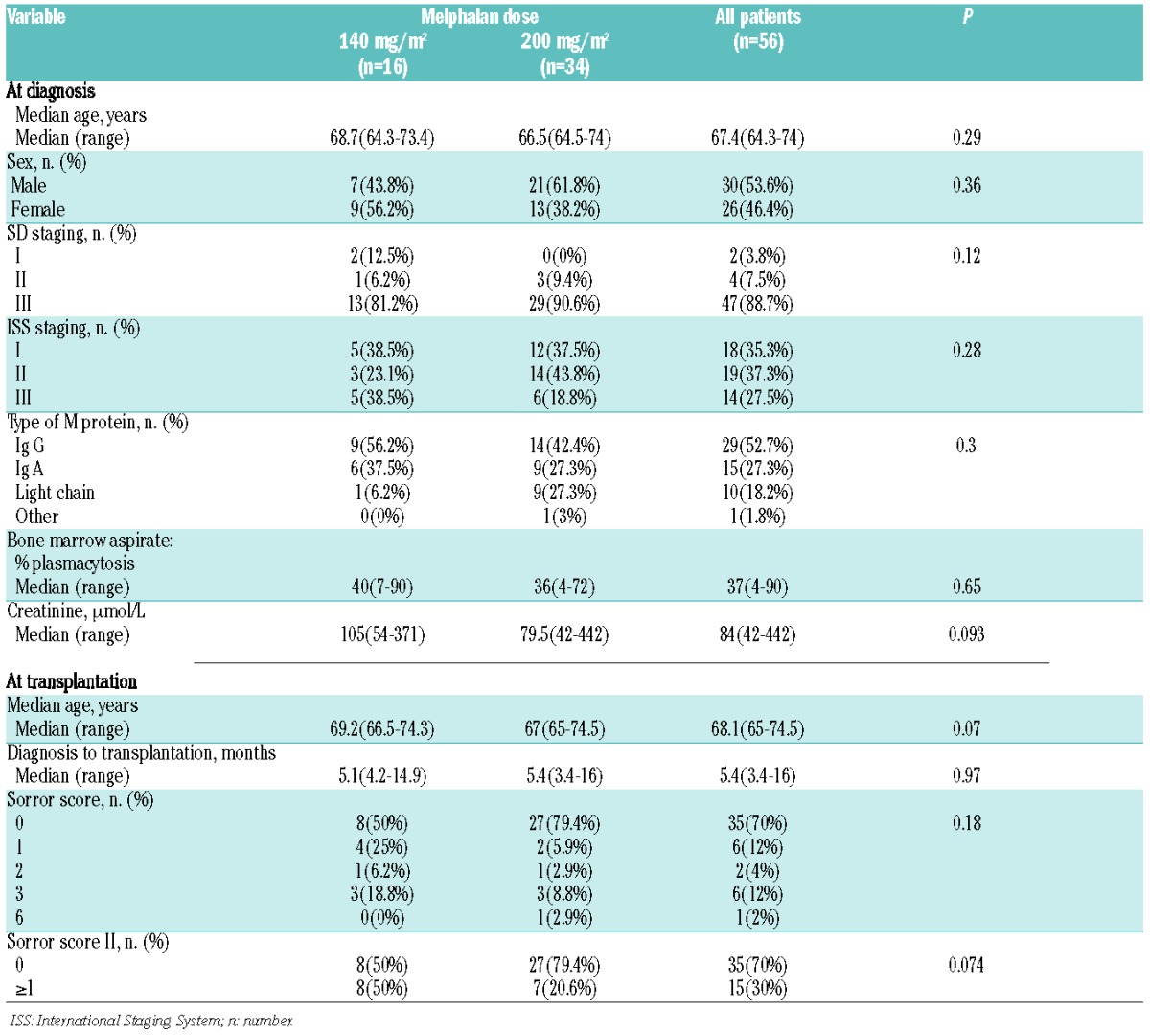
At transplantation, the HCT-CI comorbidity scores were 0 (n=34), 1 (n=6), 2 (n=2), 3 (n=6), 6 (n=1), and unknown (n=1). Median age at the time of ASCT was 68 years and the median time from diagnosis to ASCT was five months. Median follow up was 21 months (range 6–31).
Mobilization
A median of 5.31×106/kg CD34+ cells were collected. Thirty-two patients (57%) were mobilized with cyclophosphamide + G-CSF, 13 (23%) with G-CSF alone, 6 (10%) with G-CSF + plerixafor, and one with cyclophosphamide + G-CSF + plerixafor. The number of mobilization courses was 1 (n=39), 2 (n=10), and unknown (n=2); there were 2 failed mobilizations. There was no ex vivo manipulation of the autologous graft. Median number of CD34+ cells infused was 4.1×106/kg (range 1.7–7.6×106/kg).
Patients unable to proceed to ASCT
In an intention to treat analysis, 6 of the 56 patients could not proceed to ASCT due to an early infectious death (n=1), serious comorbidity (n=2), disease refractoriness to the induction regimen (n=1), or failure to collect an adequate peripheral blood stem cell (PBSC) graft (n=2).
Engraftment
The conditioning regimen consisted of 140 mg/m2 melphalan in 18 patients (36%) and 200 mg/m2 melphalan in 32 (64%). Five patients received bortezomib in combination with melphalan (melphalan 200 mg/m2), while 3 patients (6%) underwent tandem ASCT. Median time to neutrophil and platelet engraftment was 12 days (range 9–56). There was no significant difference in the time to neutrophil or platelet engraftment between the two doses of melphalan.
Consolidation
Consolidation treatment (three months post ASCT) was given in 38 patients (68%). Thirteen (34%) received VTD, 6 (16%) VRD, 6 (16%) VCD, 5 (13%) VD, 4 (10%) RD, 2 (5%) lenalidomide, 1 (3%) MPV, and 1 pomalidomide (3%). In 12 cases, the physician decided to administer no consolidation therapy.
Treatment-related toxicity
The day-100 post ASCT treatment-related mortality (TRM) was 0%. There was no significant difference in TRM between the two doses of melphalan.
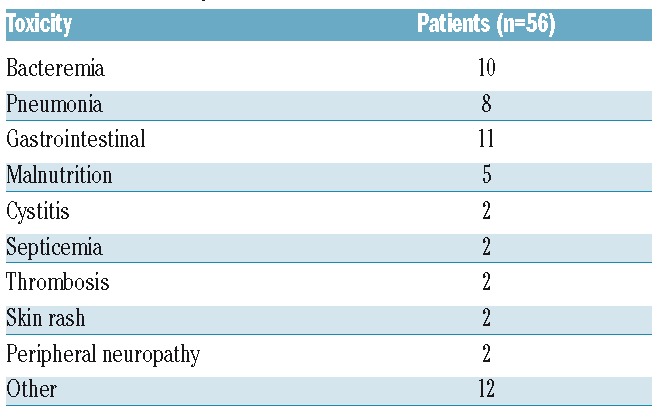
Table 2 summarizes the non-hematologic toxicities appearing after ASCT. Infection within the first 100 days post ASCT occurred in 18 patients (36%) and non-infectious complications in 24 (48%). Gastrointestinal toxicities were frequent, the most common being oral mucositis (n=18, 36%) and diarrhea (n=3, 6%). Pulmonary infection occurred in 7 patients (14%). Malnutrition was noted in 5 patients and thrombosis in 2, while one had a hemorrhage and another a cardiac complication. The incidence of infectious complications post ASCT and the response rate were comparable between the two doses of melphalan (P=0.28).
Table 2.
Non-hematopoietic toxicities.
Response and survival
Disease status at the time of ASCT was defined as: complete response (CR) (n=12, 24%), very good partial response (VGPR) (n=19, 38%), partial response (PR) (n=17, 34%), or stable disease (SD)/non-responsive (n=2, 4%). The overall response rate on day 100 was 96% (CR: 34%, VGPR: 47%, PR: 15%, and SD/non-responsive: 4%). At three months post ASCT, 68% of the patients were able to receive the planned consolidation treatment. The best responses were: CR (n=20, 40%), VGPR (n=18, 36%), PR (n=9, 18%), progression (n=1, 2%), and unknown (n=2, 4%) (Figure 1).
Figure 1.
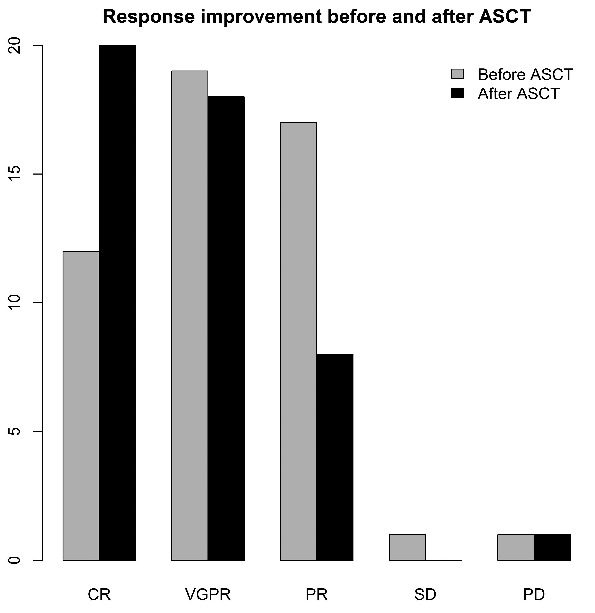
Response rates before and after autologous stem cell transplantation (ASCT). CR: complete response; VGPR: very good partial response; PR: partial response; SD: stable disease; PD: progressive disease.
After a median follow up of 21 months (range 6–31), the PFS and OS rates at two years were 76% [95%CI: (61.6–94.1)] and 88% [95%CI: (76.7–100)], respectively (Figure 2). There was a trend to a better rate of PFS in the 200 mg/m2 melphalan group (Figure 3).
Figure 2.
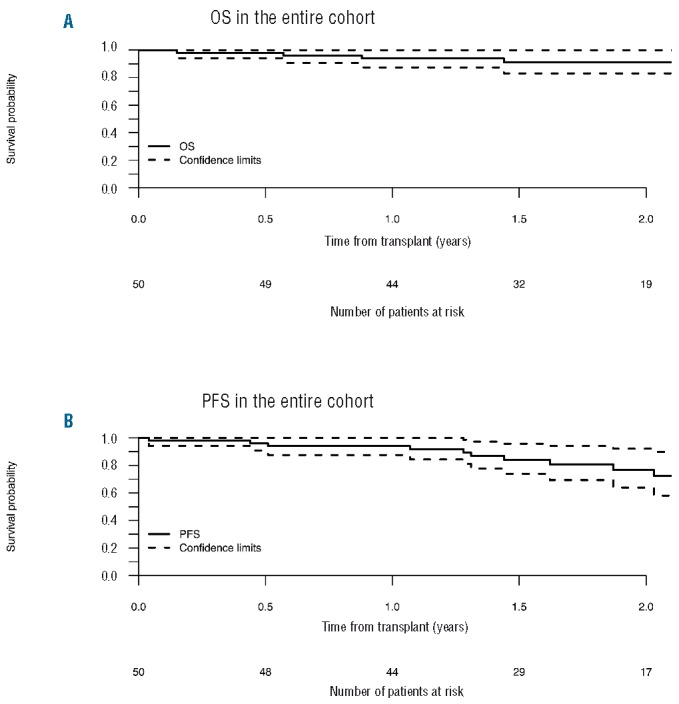
(A) Overall survival and (B) progression-free survival in the entire cohort after autologous stem cell transplantation (ASCT) (n=56). The dotted lines represent confidence intervals.
Figure 3.
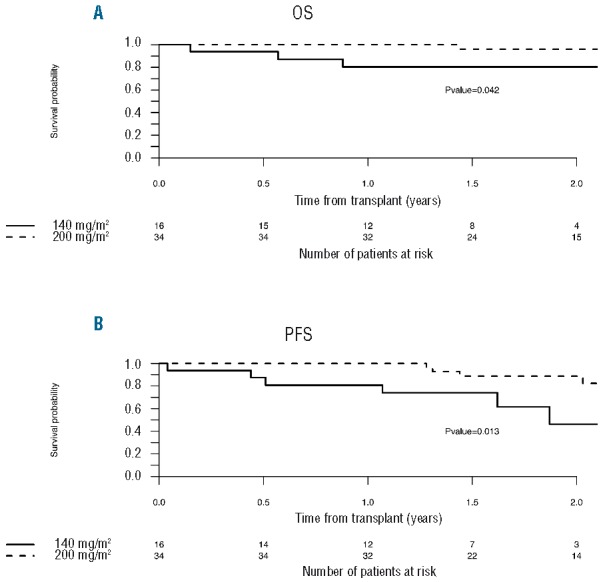
Outcome, overall survival (A) and progression-free survival (B) according to the conditioning regimen: 140 mg/m2 versus 200 mg/m2melphalan.
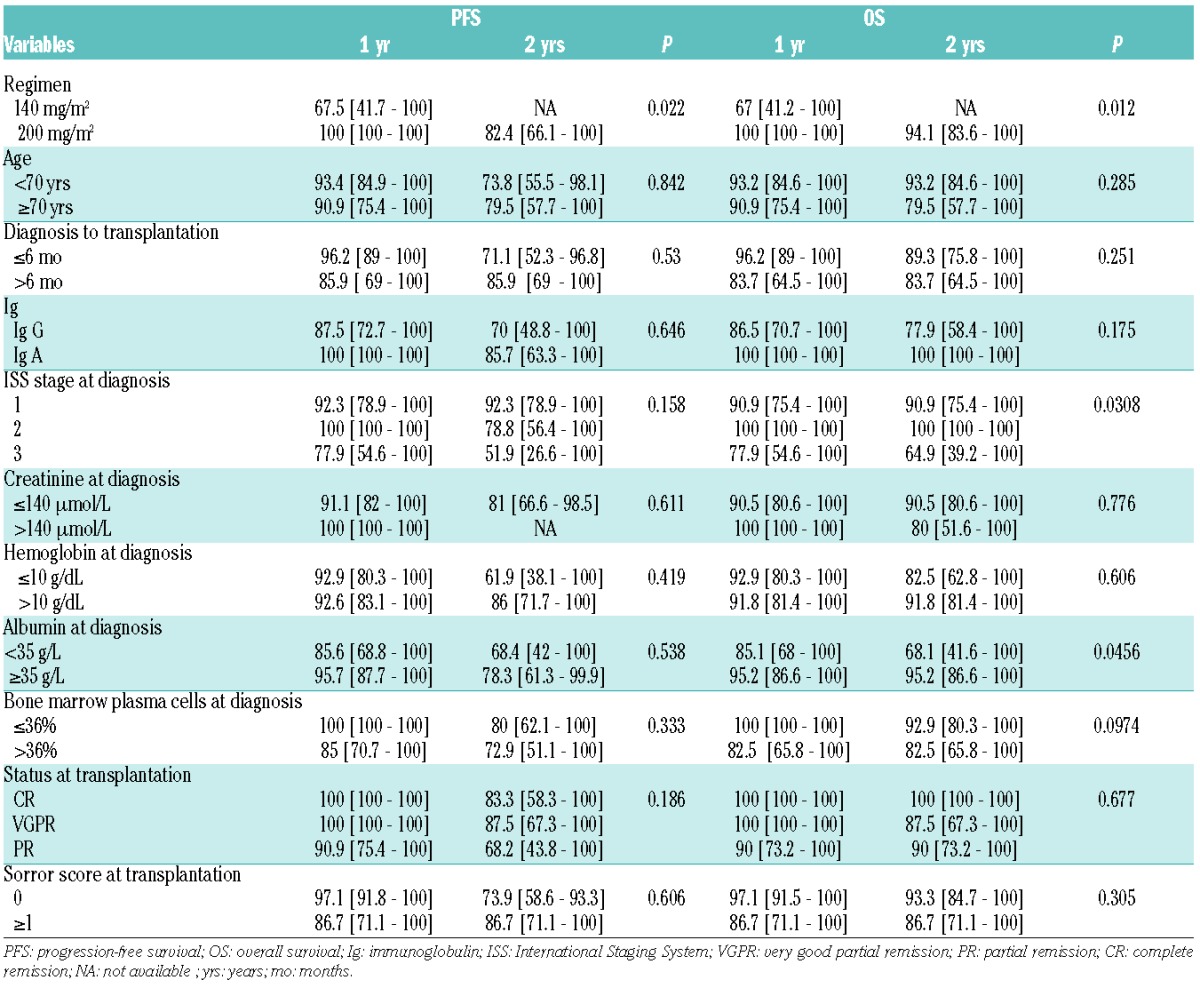
Univariate analysis
We performed a univariate analysis to identify the predictors independently associated with PFS and OS using the Cox proportional hazards model. Variables included in the analysis were: baseline patients’ characteristics (age, sex, type of myeloma protein), prognostic factors (albumin, β2 microglobulin, ISS stage), disease status, and melphalan dose at transplantation. We found the dose of the conditioning regimen to be the only significant prognostic factor for both PFS and OS. ISS stage was only prognostic for OS (Table 3).
Table 3.
Univariate analysis of prognostic factors.
Discussion
Over the past decade, the use of HDT followed by ASCT in combination with new drugs has substantially improved the outcome of younger patients with MM. However, the safety and efficacy of HDT in patients over 65 years of age remain uncertain. In this prospective study, the relatively low toxicity of the ASCT procedure for this patient population is very encouraging, with 0% TRM at 100 days post transplantation. In comparison, patients under 65 years of age have a 100-day TRM of approximately 1%. This is particularly striking considering that 10% of the patients had renal impairment at diagnosis with serum creatinine levels of more than 176 micromol/L, while 16% had high-risk cytogenetic features. It is also important to note that two-thirds of the patients received melphalan at a dose of 200 mg/m2. In this setting, patient selection is important.27,28 Six of the 56 patients (10%) could not proceed to ASCT; these frail individuals were nevertheless not excluded from the post-transplant analysis, which was performed on the basis of the intention-to-treat. Moreover, the comorbidity as measured by the Sorror score was low: 40 in 50 patients (80%) had no or only one comorbidity factor at transplantation. This patient selection could partly explain the low TRM. An improvement in post-transplant care may also have contributed to the lack of early toxicity following transplantation. In this study, an adequate number of stem cells to support ASCT was obtained in all but 2 patients (3.5%). There was no difference in the numbers of stem cells mobilized compared to those collected in younger patients, in accordance with previously published results.14
We confirmed that the inclusion of novel drugs, namely a bortezomib-based induction regimen, improved both response and outcome, and should be incorporated into the HDT approach for elderly patients. In terms of response, 34% CR on day 100 post ASCT is similar to results published in the literature. Palumbo et al. reported that bortezomib-based induction plus ASCT led to 38% CR in patients aged 65–75 years.29 Similarly, Mertz et al. obtained 43% CR + near CR after ASCT.22 The results are even better following post ASCT consolidation, reaching 40% CR in our study. Palumbo et al. even reported a CR rate of up to 66% with lenalidomide plus dexamethasone consolidation and post ASCT maintenance.29 Post ASCT maintenance is, however, still a controversial issue in young patients, and more data will be needed before it can be implemented in an older patient population.
The relationship between melphalan dose and outcome has been demonstrated previously. In a report from the Mayo Clinic, in which 33 patients aged 70 years or older undergoing high-dose therapy were compared with a cohort of matched patients aged 65 years old or under, toxicity and survival were comparable.15 Although a dose reduction to 140 mg/m2 was required for 10 patients in the elderly group, the majority received conditioning with 200 mg/m2 melphalan, and the response rate was similar in the two groups. On the other hand, in a report from the University of Arkansas, 200 mg/m2 melphalan was associated with excessive early mortality (16%) in patients aged aged 70 years or older.14 In the latter study, all subsequent patients were treated with 140 mg/m2 melphalan, which resulted in a TRM of 2%. In our work, there was a better outcome using 200 mg/m2 melphalan compared to 140 mg/m2. Considering that there was no increased toxicity, 200 mg/m2 melphalan could be an appropriate regimen for patients aged 65–70 years.
Our results should also be compared to those of non-transplant approaches, and in particular to the data obtained using new drugs. In the past, for patients aged 65–75 years, a combination of melphalan plus prednisone and thalidomide yielded a median PFS of 27.5 months and a median OS of 51.6 months, which was superior to the PFS of 19.4 months achieved using VAD plus double ASCT (IFM 99-06).7 A combination of thalidomide plus doxorubicine and dexamethasone (Thal DD) plus thalidomide maintenance was not inferior to Thal DD plus high-dose therapy and ASCT in elderly patients with de novo MM.30 After a median follow up of 36 months, there was no significant difference in the median time to progression (TTP) between the group of patients who underwent ASCT and those patients receiving Thal DD plus maintenance (32 vs. 31 months, P=0.962; 32 vs. 29 months, P=0.726, respectively). The 5-year OS was 49% in the first group and 46% in the second (P=0.404). In the Velcade as Initial Standard Therapy in Multiple Myeloma (Vista) study, the TTP among patients receiving bortezomib plus melphalan–prednisone was 24.0 months.31 In the Frontline Investigation of Revlimid and Dexamethasone versus Standard Thalidomide (First) trial, the median PFS was 25.5 months under continuous lenalidomide plus dexamethasone and the OS at 4 years was 59%.19 In our study, the estimated PFS and OS rates at two years were 76% and 88%, respectively, which is encouraging. Moreover, these data are almost superimposable on those of Palumbo et al. using PAD induction followed by ASCT with lenalidomide consolidation and maintenance: after a median follow up of 21 months, their 2-year PFS and OS rates were 69% and 86%, respectively.29 In the younger myeloma patients (aged <65 years), the combination of bortezomib and lenalidomide and dexamethasone as induction and consolidation post ASCT along with a 1-year lenalidomide maintenance gave even better results; with a median follow up of 39 months, estimated 3-year PFS and OS were 77% and 100%, respectively.32 Nevertheless, cross trial comparisons should be viewed with caution on account of the patient selection bias. This implies that selected elderly patients could benefit from auto-SCT, which might be superior to chemotherapy or new drug combinations.
Although we looked for prognostic factors, the only two significant factors detected in our univariate analysis of OS were the dose of the conditioning regimen and the ISS stage. This could be related to the small number of patients and the relatively short follow up. However, the β2 microglobulin level before transplantation, which is a confirmed prognostic variable in many studies, may lack significance in this elderly population.14 β2 microglobulin levels are higher in the elderly. This probably reflects an age-related decrease in creatinine clearance, rather than a high tumor burden.
The weaknesses of our study lie in the non-randomized nature of the trial and the highly selected patient population included, as reflected by the low Sorror score in most of our patients. Therefore, the data concerning ASCT may not be relevant to all newly diagnosed elderly myeloma patients. We also acknowledge that the induction, conditioning and consolidation regimens were very heterogeneous, which makes it more difficult to draw conclusions. Follow up was also relatively short. Other groups are currently studying the feasibility and efficacy of high-dose melphalan in elderly patients, such as the DSMM group in Germany and the Freiburg team.13 Specifically, the Freiburg team has proposed a revised Myeloma Comorbidity Index for future frailty measurements which could help to identify those patients fit enough to undergo stem cell transplantation.33
In conclusion, these prospective multicenter results indicate that ASCT is a safe and effective mode of treatment for elderly and fit MM patients in the present era of novel induction agents. One may note that patients over 70 years of age did not have a worse prognosis. Thus, age per se should not be used as an exclusion criterion for ASCT. These results provide a framework for a randomized comparison with non-transplant approaches in this patient subgroup.
Supplementary Material
Footnotes
Check the online version for the most updated information on this article, online supplements, and information on authorship & disclosures: www.haematologica.org/content/101/11/1390
Funding
The study was supported by a grant from the “Association for Training, Education and Research in Hematology, Immunology and Transplantation” (ATERHIT, Nantes, France).
References
- 1.Blade J, Rosinol L, Cibeira MT, et al. Hematopoietic stem cell transplantation for multiple myeloma beyond 2010. Blood. 2010;115(18):3655–3663. [DOI] [PubMed] [Google Scholar]
- 2.Jantunen E. Autologous stem cell transplantation beyond 60 years of age. Bone Marrow Transplant. 2006;38(11):715–720. [DOI] [PubMed] [Google Scholar]
- 3.Gertz MA. Too old for transplantation: think again. Blood. 2004;104(10):3000–3001. [Google Scholar]
- 4.Wildes TM, Rosko A, Tuchman SA. Multiple Myeloma in the Older Adult: Better Prospects, More Challenges. J Clin Oncol. 2014;32(24):2531–2540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozaki S, Shimizu K. Autologous stem cell transplantation in elderly patients with multiple myeloma: past, present, and future. Biomed Res Int. 2014;394792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palumbo A, Bringhen S, Petrucci MT, et al. Intermediate-dose melphalan improves survival of myeloma patients aged 50 to 70: results of a randomized controlled trial. Blood. 2004;104(10):3052–3057. [DOI] [PubMed] [Google Scholar]
- 7.Facon T, Mary JY, Hulin C, et al. Melphalan and prednisone plus thalidomide versus melphalan and prednisone alone or reduced-intensity autologous stem cell transplantation in elderly patients with multiple myeloma (IFM 99–06): a randomised trial. Lancet. 2007; 370(9594):1209–1218. [DOI] [PubMed] [Google Scholar]
- 8.Sirohi B, Powles R, Treleaven J, et al. The role of autologous transplantation in patients with multiple myeloma aged 65 years and over. Bone Marrow Transplant. 2000;25(5):533–539. [DOI] [PubMed] [Google Scholar]
- 9.Reece D, Bredeson C, Perez WS, et al. Autologous stem cell transplantation in multiple myeloma patients <60 vs≥ 60 years of age. Bone Marrow Transplant. 2003;32(12):1135–1143. [DOI] [PubMed] [Google Scholar]
- 10.Jantunen E, Kuittinen T, Penttila K, et al. High-dose melphalan (200 mg/m2) supported by autologous stem cell transplantation is safe and effective in elderly (>65 years) myeloma patients: comparison with younger patients treated on the same protocol. Bone Marrow Transplant. 2006; 37(10):917–922. [DOI] [PubMed] [Google Scholar]
- 11.Lenhoff S, Hjorth M, Westin J, et al. Impact of age on survival after intensive therapy for multiple myeloma: a population-based study by the Nordic Myeloma Study Group. Br J Haematol. 2006;133(4):389–396. [DOI] [PubMed] [Google Scholar]
- 12.Muta T, Miyamoto T, Fujisaki T, et al. Evaluation of the Feasibility and Efficacy of Autologous Stem Cell Transplantation in Elderly Patients with Multiple Myeloma. Intern Med. 2013;52(1):63–70. [DOI] [PubMed] [Google Scholar]
- 13.Mertz M, Jansen L, Castro FA, et al. Survival of elderly patients with multiple myeloma-effect of upfront autologous stem cell transplantation. Eur J Cancer. 2016;62;1–8. [DOI] [PubMed] [Google Scholar]
- 14.Badros A, Barlogie B, Siegel E, et al. Autologous stem cell transplantation in elderly multiple myeloma patients over the age of 70 years. Br J Haematol. 2001; 114(3):600–607. [DOI] [PubMed] [Google Scholar]
- 15.Kumar SK, Dingli D, Lacy MQ, et al. Autologous stem cell transplantation in patients of 70 years and older with multiple myeloma: Results from a matched pair analysis. Am J Hematol. 2008;83(8):614–617. [DOI] [PubMed] [Google Scholar]
- 16.Bashir Q, Shah N, Parmar S, et al. Feasibility of autologous hematopoietic stem cell transplant in patients aged ≥ 70 years with multiple myeloma. Leuk Lymphoma. 2012;53(1):118–122. [DOI] [PubMed] [Google Scholar]
- 17.Wildes TM, Finney JD, Fiala M, et al. High-dose therapy and autologous stem cell transplant in older adults with multiple myeloma. Bone Marrow Transplant. 2015;50(8):1075–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Auner HW, Szydlo R, Hoek J, et al. Trends in autologous hematopoietic cell transplantation for multiple myeloma in Europe: increased use and improved outcomes in elderly patients in recent years. Bone Marrow Transplant. 2015;50(2):209–215. [DOI] [PubMed] [Google Scholar]
- 19.Palumbo A, Bringhen S, Mateos MV, et al. Geriatric assessment predicts survival and toxicities in elderly myeloma patients: an International Myeloma Working Group report. Blood. 2015;125(13):2068–2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Palumbo A, Sezer O, Kyle R, et al. International Myeloma Working Group guidelines for the management of multiple myeloma patients ineligible for standard high-dose chemotherapy with autologous stem cell transplantation. Leukemia. 2009;23(10):1716–1730. [DOI] [PubMed] [Google Scholar]
- 21.Benboubker L, Dimopoulos MA, Dispenzieri A, et al. Lenalidomide and dexamethasone in transplant-ineligible patients with myeloma. N Engl J Med. 2014;371(10):906–917. [DOI] [PubMed] [Google Scholar]
- 22.Merz M, Neben K, Raab MS, et al. Autologous stem cell transplantation for elderly patients with newly diagnosed multiple myeloma in the era of novel agents. Ann Oncol. 2014;25(1):189–195. [DOI] [PubMed] [Google Scholar]
- 23.Durie BG, Salmon SE. A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment, and survival. Cancer. 1975;36(3):842–854. [DOI] [PubMed] [Google Scholar]
- 24.Greipp PR, San Miguel J, Durie BG, et al. International staging system for multiple myeloma. J Clin Oncol. 2005;23(15):3412–3420. [DOI] [PubMed] [Google Scholar]
- 25.Sorror ML, Maris MB, Storb R, et al. Hematopoietic cell transplantation (HCT)- specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912–2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Durie BG, Harousseau JL, Miguel JS, et al. International uniform response criteria for multiple myeloma. Leukemia. 2006; 20(9):1467–1473. [DOI] [PubMed] [Google Scholar]
- 27.Palumbo A, Bringhen S, Ludwig H, et al. Personalized therapy in multiple myeloma according to patient age and vulnerability: a report of the European Myeloma Network (EMN). Blood. 2011;118(17):4519–4529. [DOI] [PubMed] [Google Scholar]
- 28.Bringhen S, Mateos MV, Zweegman S, et al. Age and organ damage correlate with poor survival in myeloma patients: meta-analysis of 1435 individual patient data from 4 randomized trials. Haematologica. 2013;98(6):980–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Palumbo A, Gay F, Falco P, et al. Bortezomib As Induction Before Autologous Transplantation, Followed by Lenalidomide As Consolidation-Maintenance in Untreated Multiple Myeloma Patients. J Clin Oncol. 2010; 28(5):800–807. [DOI] [PubMed] [Google Scholar]
- 30.Offidani M, Leoni P, Corvatta L, et al. ThaDD plus high dose therapy and autologous stem cell transplantation does not appear superior to ThaDD plus maintenance in elderly patients with de novo multiple myeloma. Eur J Haematol. 2010; 84(6):474–483. [DOI] [PubMed] [Google Scholar]
- 31.San Miguel JF, Schlag R, Nuriet K, et al. Bortezomib plus Melphalan and Prednisone for Initial Treatment of Multiple Myeloma. N Engl J Med. 2008;359(9):906–917. [DOI] [PubMed] [Google Scholar]
- 32.Roussel M, Lauwers-Cances V, Robillard N, et al. Front-Line Transplantation Program With Lenalidomide, Bortezomib, and Dexamethasone Combination As Induction and Consolidation Followed by Lenalidomide Maintenance in Patients With Multiple Myeloma: A Phase II Study by the Intergroupe Francophone du Myelome. J Clin Oncol. 2014;32(25):2712–2717. [DOI] [PubMed] [Google Scholar]
- 33.Engelhardt M, Dold SM, Ihorst G, Zober A, et al. Geriatric assessment in multiple myeloma patients: validation of the International Myeloma Working Group (IMWG) score and comparison with other common comorbidity scores. Haematologica. 2016;101(9):1110–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


