The UK National Service Framework for Diabetes recommends nationwide screening of people with diabetes for development of sight-threatening retinopathy.1 All health workers who provide diabetes care require an understanding of the common ophthalmic treatments that can be offered for such disease. The principal conditions to consider are diabetic maculopathy and proliferative retinopathy.
In diabetic maculopathy, central vision may be compromised by macular (central retinal) oedema with varying degrees of ischaemia. The oedema may respond to laser therapy, ischaemia does not. Therapy takes the form of ‘focal’ (Figure 1) or ‘grid’ (Figure 2) macular laser, consisting of up to 200 small (e.g. 100 μm) gently applied burns to areas of central retinal thickening. This tends to encourage resolution of thickening.
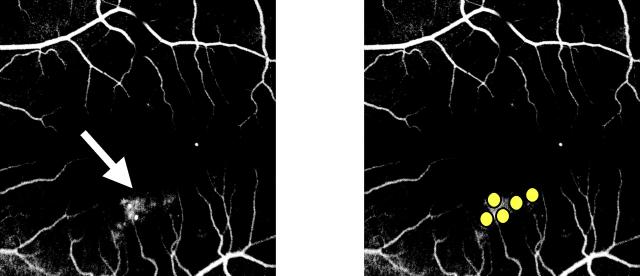
Figure 1.
Focal macular laser therapy for focal macular oedema. Fluorescein angiography reveals focal leakage from diabetic microvascular abnormalities (white arrow). Laser burns (white spots) are placed on the area of thickened retina. Colour version available on [www.jrsm.org]
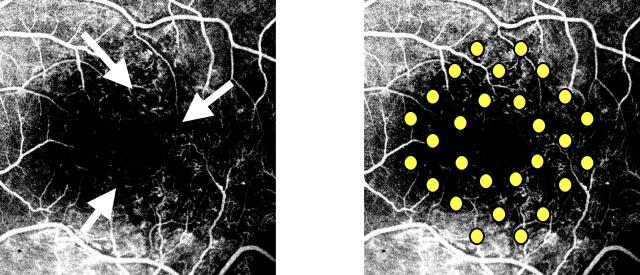
Figure 2.
Grid macular laser therapy for diffuse macular oedema. Fluorescein angiography reveals diffuse leakage from diabetic microvascular abnormalities (white arrows). Laser burns (spots) are placed on the area of thickened retina. Colour version available on [www.jrsm.org]
In proliferative retinopathy, central and peripheral vision may be compromised by bleeding from new vessels arising on the optic disc (NVD) or elsewhere in the retina (NVE). These vessels typically bleed because of the tendency of the overlying vitreous gel, to which the new vessels are attached, to retract, stretching vessels between vitreous and retina. Therapy takes the form of panretinal photocoagulation, in which perhaps 2000 large (e.g. 500 μm) burns, of greater intensity than employed in macular laser, are applied to retina outside the central thirty-degree zones (Figure 3a3b). This tends to encourage a reduction in the calibre of new vessels.
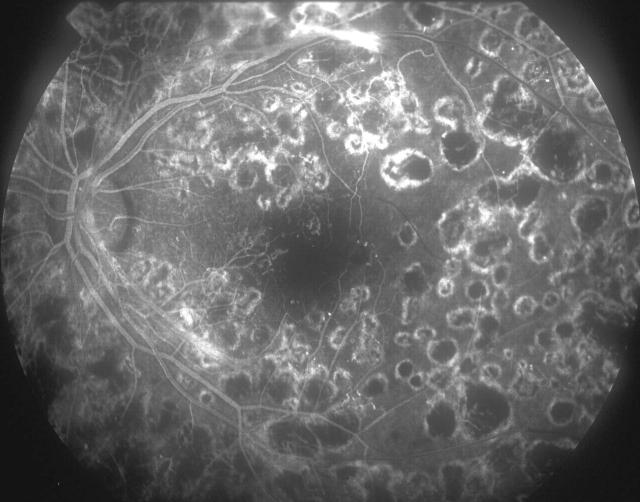
Figure 3a.
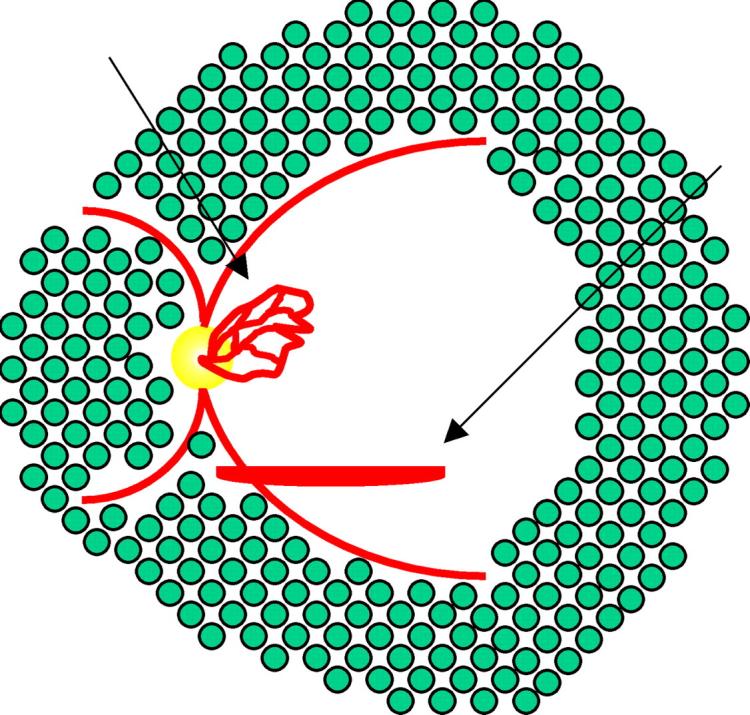
Panretinal photocoagulation for proliferative retinopathy. Laser burns (spots) are placed outside central retina (a) as can be seen in the fluorescein angiogram
Figure 3b.
Panretinal photocoagulation for proliferative retinopathy. Laser burns (spots) are placed outside central retina (b). Colour version available on [www.jrsm.org]
MACULAR LASER THERAPY
Technique
Treatment is an outpatient procedure; admission to hospital is not required. The patient sits at a slit lamp similar to that used in routine ophthalmic examination but modified to accept a laser fibreoptic cable (Figure 4). Proxymetacaine or benoxinate drops are used to anaesthetize the cornea and a therapeutic contact lens is applied. As treatment is started, the patient experiences bright flashes of light but no pain. The eye must be kept as still as possible during treatment to ensure accurate application of the laser and to avoid damage to the fovea; a typical treatment takes about ten minutes. Therefore the patient needs some means of communicating with the ophthalmologist so that the treatment can be safely interrupted. The usual signal is a raised hand or a noise in the throat; if the patient speaks, jaw movement may displace the laser beam. Commonly the patient is very dazzled after the treatment, and sometimes the laser spots are visible to the patient. Typically though not invariably, this effect fades over the next few days. No special precautions need to be taken after the laser, and no additional eye drops or oral therapy are needed.
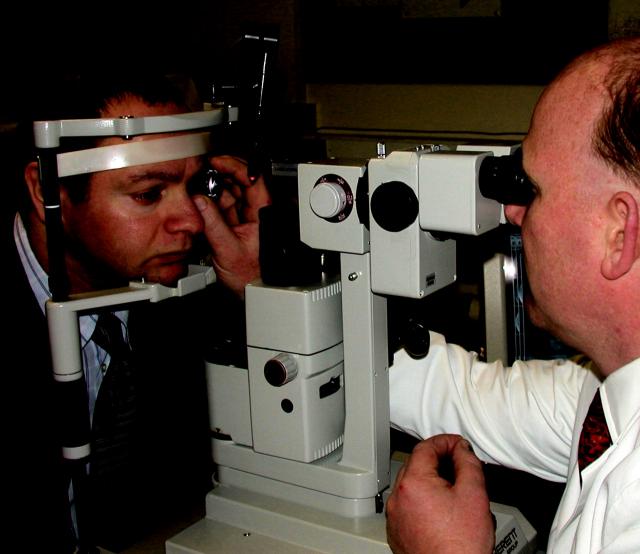
Figure 4.
Laser slit lamp delivery. Colour version available on [www.jrsm.org]
Side-effects
Some reduction in colour vision or small dark spots near the central vision are quite commonly perceived by the patient after treatment. If the patient looks directly at the laser beam during treatment, the fovea can be damaged, with potential for severe visual loss, especially if laser power is at any but a very low setting. This is a rare occurrence. Another rare but serious complication results from application of high power levels over a small area (high fluence), which can rupture Bruch's membrane, which separates choroid from retina. Acutely, this can cause haemorrhage; later, vascular ingrowth can result in macular scarring similar to that in age-related macular degeneration, with loss of central vision.
Effects of treatment
In the Early Treatment Diabetic Retinopathy Study,2 macular laser therapy for clinically significant macular oedema approximately halved the rate of moderate visual loss, defined as doubling of the visual angle, and equating to a change from 6/6 to 6/12 or from 6/12 to 6/24. A modest improvement (one line on the Snellen visual acuity chart) was seen in 40% of treated and 20% of untreated eyes. The number needed to treat to prevent one case of moderate visual loss over 3 years is 8.
The principal effect of macular laser therapy is to reduce the rate of visual loss. Patients should be encouraged to hope for stabilization of vision and not to expect visual improvement. Once visual loss occurs, it is unlikely to be reversed. Furthermore, laser treatment does not invariably prevent visual loss. In some patients, oedema persists despite adequate initial treatment to the oedematous area; in others, oedema arises in new areas. In these patients, further laser therapy may be required. Eyes with significant macular ischaemia in association with macular oedema may continue to show visual deterioration despite resolution of oedema. Treatment can take several months to work, and vision may vary during this period. Commonly, as oedema resolves, lipoprotein exudate is deposited in the retina, to be removed ultimately by macrophages.
PANRETINAL LASER THERAPY
Technique
This treatment is likewise usually undertaken in outpatients, although admission to hospital may be required in the few patients unable to cooperate with slit-lamp-delivered laser. In the latter group laser is applied under subtenons local anaesthesia or general anaesthesia, through a binocular indirect ophthalmoscope, with the ophthalmologist standing and the patient supine. The arrangement for outpatient treatment is similar to that for macular laser therapy, although a wide angle contact lens may be required to reach peripheral retina. Treatment consists of a greater number of larger, more intense burns, more rapidly applied than in macular laser therapy. This may cause sharp but transient pain, especially if laser is applied over a nerve or over an old laser burn. For this reason it is particularly important that the patient has some means of communicating with the ophthalmologist, so that treatment can be safely interrupted until the pain fades. The eye must be kept as still as possible during treatment to ensure accurate application of the laser. A typical treatment takes about thirty minutes. Commonly the patient is so dazzled immediately after treatment that he or she cannot see at all from the treated eye. This tends to fade over the next few days to weeks. No special precautions need be taken after laser treatment, but oral nonsteroidal anti-inflammatory agents such as ibuprofen or flurbiprofen are valuable in lessening the dull ache that can follow treatment.
Side-effects
Macular oedema is a material side-effect of treatment, and may be sufficiently severe to reduce visual acuity. It is particularly troublesome in eyes with proliferative retinopathy and pre-existing macular oedema; panretinal photocoagulation may then need to be fractionated over several visits to minimize worsening of macular oedema. The application of laser to peripheral retina also tends to impair peripheral retinal function, and patients may suffer glare and light sensitivity. In addition, visual field may be compromised, in some patients to the extent that they are rendered ineligible to drive. Patient movement or misplaced burns may damage retinal blood vessels.
Effects of treatment
In the Diabetic Retinopathy Study,3 panretinal photo-coagulation for high-risk proliferative retinopathy approximately halved the risk of severe visual loss, defined as the inability to see the top letter on a Snellen chart from 1.56 m. Depending on the pattern of proliferative retinopathy, the number needed to treat to prevent one case of severe visual loss over 2 years is between 3 and 7.
As with macular laser therapy, the principal effect of panretinal photocoagulation is to reduce the rate of visual loss. Again, patients should not expect visual improvement but hope for stabilization of vision. They should be advised that, once visual loss occurs, it is unlikely to be reversed. Growth of new vessels, visual loss and haemorrhage into the vitreous cavity may occur despite well applied treatment. In these patients, further laser therapy may be required, although this may be hampered or prevented by vitreous haemorrhage. Even if the calibre of new vessels is considerably reduced, contraction of the vitreous gel may result in recurrent haemorrhage. If haemorrhage is persistent, preventing laser therapy, or if contraction of the vitreous gel, acting through new vessel stalks, has detached the retina, vitrectomy surgery, involving removal of the vitreous gel, may be required to clear haemorrhage, apply panretinal photocoagulation, or reattach retina.
Panretinal photocoagulation typically takes several months to achieve full effect, although some response can often be seen much sooner. The number of burns required to achieve regression of new vessels varies considerably. In patients with type 1 diabetes and very aggressive disease, many thousands of burns and several sessions of treatment may be required. In patients with type 2 diabetes and less aggressive disease, a thousand burns may suffice.
CONCLUSION
Common laser treatments applied to patients with sight-threatening forms of diabetic retinopathy are effective in preventing but not reversing visual loss. It is therefore imperative that patients with sight-threatening disease are referred before visual loss occurs. This requires an effective retinopathy risk reduction programme and referral chain.
References
- 1.Department of Health. National Service Framework for Diabetes. [http://www.doh.gov.uk/nsf/diabetes/]. Accessed 26 March 2003
- 2.Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol 1985;103: 1796-806 [PubMed] [Google Scholar]
- 3.Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. Ophthalmology 1981;88: 583-600 [PubMed] [Google Scholar]