When heart failure develops in a patient with myeloma, special imaging techniques may be informative.
CASE HISTORY
A man of 76 was admitted elsewhere with atrial fibrillation and congestive cardiac failure. In the previous 3 years he had received intermittent courses of melphalan and prednisolone for multiple myeloma, though not in the months leading up to this admission. He was initially treated with intravenous diuretics and improved clinically. Three days after admission, an echocardiogram showed a large pericardial effusion with early tamponade and large mass lesions in the left and right atria. He was then transferred to our centre. On arrival there were no signs of heart failure. The electrocardiogram (ECG) showed low voltages, with atrial flutter and a rapid ventricular response rate. On chest X-ray the cardiac silhouette was enlarged, and bilateral small pleural effusions were present. Old healed rib fractures of the left chest wall were noted. Haemoglobin on admission was 12.2 g/dL, creatinine 146 μmol/L, serum globulins raised at 41 g/L.
The patient underwent further assessment with multi-slice CT of the heart. Retrospective ECG gating was used to minimize cardiac motion artifact and maximize image resolution, with 500 ms gantry rotation and 4 × 1.0 mm collimation. The acquisition was adapted directly from a non-invasive coronary angiography protocol. A large intracardiac mass was seen to arise from the interatrial septum, extending into both atria (Figure 1A,B). The tumour encroached into both right upper and lower pulmonary veins and superior vena cava, which was almost totally obstructed. Three-dimensional CT reconstruction with volume rendering techniques allowed clear visualization of all the cardiac structures involved by tumour.
Figure 1.
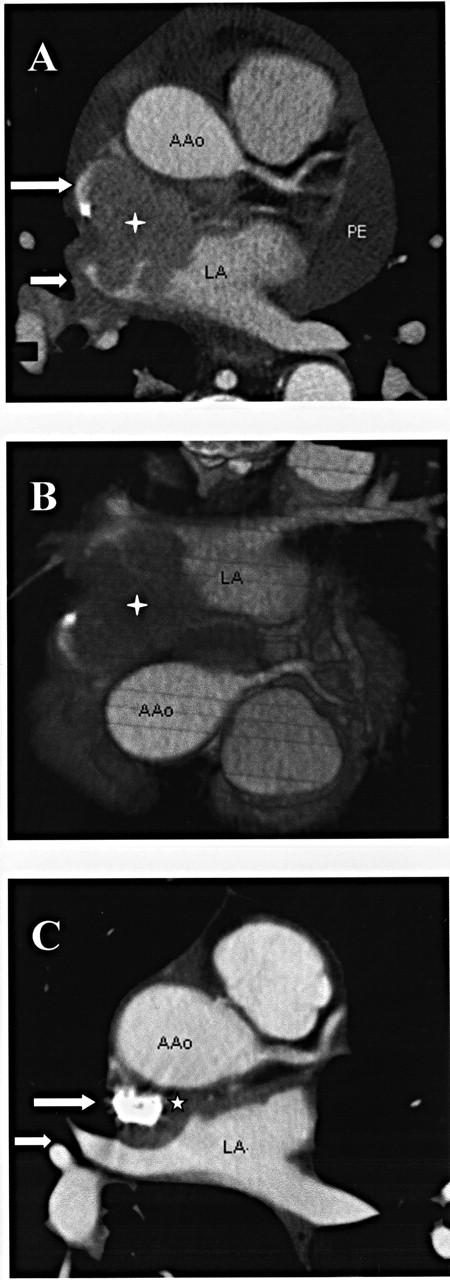
Intracardiac plasmacytoma (A) CT axial cross-section, large arrow showing superior vena cava, small arrow right upper pulmonary vein. Ao=ascending aorta; LA=left atrium; PE=pericardial effusion.
(B)three-dimensional CT reconstruction; (C) CT axial cross-section after radiotherapy, arrows as in (A)
Intracardiac plasmacytoma was diagnosed. The pericardial effusion was drained (800 mL) and the fluid showed a monoclonal band identical to that found in serum (IgA lambda). After drainage of the effusion there was spontaneous reversion to sinus rhythm. On oncological advice he then received radiotherapy to the heart—30 Gy (mid plane dose) in ten fractions over two weeks with 6 MV photons—during which time he was anticoagulated. When electively readmitted six weeks after completion of the initial radiotherapy he was clinically well. Repeat multi-slice CT scan showed almost complete tumour regression, with abnormal signals now confined to a rim along the interatrial septum (see Figure 1C). There was no evidence of pulmonary vein involvement and the contrast-filled superior vena cava was widely patent. The patient was discharged for haematology follow-up at his local hospital. Six weeks later he was admitted with a scrotal swelling with biopsy consistent with plasmacytoma This was managed by orchidectomy.
COMMENT
The development of a plasmacytoma during treatment of myeloma is a bad prognostic feature suggesting resistance to chemotherapeutic agents. There are a few previous case reports of intracardiac plasmacytomas, identified after surgical resection, 1,2,3 or by transvenous biopsy, 4 or at necropsy. 5 Palliative radiotherapy successfully reduced tumour size in one patient6 and radiotherapy plus chemotherapy in another. 5 Plasmacytomas are very sensitive to local radiotherapy, and a proportion of local tumours are curable by this means. 7 In patients less ill than ours, the hazards of mediastinal irradiation would have required more consideration. There is a modest late excess incidence of coronary artery stenosis, 8 and of pericardial constriction after treatment. 9
The clinical presentation of intracardiac tumours depends on the anatomical structures involved. The multi-slice CT images obtained here allowed accurate anatomical localization. The nature of the mass as intracardiac, rather than invading from the vena cava, was not discernible on transthoracic or transoesophageal echocardiography. Multi-slice CT scan was also the modality of choice for confirming the treatment response.
References
- 1.Tak T, Rashtian M, De-Tar M, Chandraratna PA, Gill P. An unusual case of metastatic intracardiac plasmacytoma. Can J Cardiol 1994;10: 857-60 [PubMed] [Google Scholar]
- 2.Carrel T, Linka A, Turina MI. Tricuspid valve obstruction caused by a plasmacytoma metastasis. Ann Thorac Surg 1992;54: 352-4 [DOI] [PubMed] [Google Scholar]
- 3.Torstveit JR, Bennett WA, Hinchcliffe WA, Cornell WP. Primary plasmacytoma of the atrium. Report of a case with successful surgical management. J Thorac Cardiovasc Surg 1977;74: 563-6 [PubMed] [Google Scholar]
- 4.Wan X, Tarantolo S, Orton DF, Greiner TC. Primary extramedullary plasmacytoma in the atria of the heart. Cardiovasc Pathol 2001;10: 137-9 [DOI] [PubMed] [Google Scholar]
- 5.Champeaux AI, Blaser JL, Myers JB, Schachter DT. Multiple myeloma involving the myocardium and coronary vessels. Arch Pathol Lab Med 2000;124: 910-12 [DOI] [PubMed] [Google Scholar]
- 6.Kurzidim K, Gnad M, Hartmann A, Held P, Riegger G, Elsner D. Kardiale Metastasierung eines Plasmozytoms mit der klinischen Manifestation einer ausgedehnten Lungenembolie. Dtsch Med Wochenschr 1998;123: 1372-7 [DOI] [PubMed] [Google Scholar]
- 7.Callender S, Mason DY. Paraproteinaemia. In: Weatherall DJ, Ledingham JGG, Warrell DA, eds. The Oxford Textbook of Medicine. Oxford: Oxford University Press, 1983
- 8.Boivin JF, Hutchinson GB, Lubin JH, et al. Coronary artery disease mortality in patients treated for Hodgkin's disease. Cancer 1992;69: 1241-7 [DOI] [PubMed] [Google Scholar]
- 9.Zinzani PL, Gherlinzoni F, Piovaccari G, et al. Cardiac injury as late toxicity of mediastinal radiation therapy for Hodgkin's disease patients. Haematologica 1996;81: 132-7 [PubMed] [Google Scholar]


