Abstract
Objective:
To identify factors that influence Saskatchewan women’s choice between breast conserving therapy (BCT) and mastectomy in early-stage breast cancer (ESBC) and to compare and contrast underlying reasons behind choice of BCT versus mastectomy.
Methods:
Interpretive description methods guided this practice-based qualitative study. Data were analyzed using thematic analysis and presented in thematic maps.
Results:
Women who chose mastectomy described 1 of the 3 main themes: worry about cancer recurrence, perceived consequences of BCT treatment, or breast-tumor size perception. In contrast, women chose BCT because of 3 different themes: mastectomy being too radical, surgeon influence, and feminine identity.
Conclusions:
Although individual reasons for choosing mastectomy versus BCT have been discussed in the literature before, different rationale underlying each choice has not been previously described. These results are novel in identifying interdependent subthemes and secondary reasons for each choice. This is important for increased understanding of factors influencing a complicated decision-making process.
Keywords: cancer, oncology, decision-making, breast conservation therapy, mastectomy, early-stage breast cancer
Introduction
Breast cancer is the most commonly diagnosed cancer and the second most common cause of cancer death in women in North America.1 For early-stage breast cancer (ESBC), it is well established that breast conserving therapy (BCT) and mastectomy offer equivalent survival.2–5 Treatment of ESBC can therefore be viewed as preference-sensitive care, where decision-making between treatment options should vary according to patient preferences and values, but could potentially vary for other reasons.6
There are quantitative studies examining factors that influence therapy choice, but this literature is limited to mostly chart or database reviews, largely retrospective, and mostly conducted outside of Canada.7–9 Common demographic factors examined in such studies include age, education, and ethnicity. Age has shown many discrepant results, with the most consistent finding being an increased likelihood of undergoing mastectomy in younger age groups under 40 or 50.7 The middle age groups generally do not show significant findings. The older age groups above 70 or 80 have shown mixed results, with some studies noting increased mastectomy rates, whereas others showed decreased rates.10,11 Furthermore, some studies have not found any association with age on mastectomy rates.12,13 With respect to ethnicity, African American, Hispanic, and Asian/Pacific Islander women have independently been associated with increased rates of mastectomy.7,14
Travel-related factors, such as distance to a radiation treatment center, have shown varying effects on rates of BCT versus mastectomy. Although several studies have demonstrated a decreasing rate of BCT as distance to radiation center increases,15–17 others have found no difference.18,19
Individual values and preferences may be the most important subset of factors influencing choice of mastectomy versus BCT, but are the least well studied. The complex nature of decision-making in ESBC makes fully understanding the spectrum and significance of these factors difficult. Most of this research has been through simple stand-alone questionnaires or descriptive qualitative studies. Important personal beliefs and preferences previously noted in the literature include equivalent survival between BCT and mastectomy, fear of cancer recurrence, cosmetic appearance, and feminine identity.11,20–22
Mastectomy rates across Canada have varied greatly over the past decade, with the latest reports from 2008 to 2013 showing interprovincial differences from 25.3% to 68.3%.23 This geographical variation raises many unanswered questions. Are differences related to quality or appropriateness of care? Are attitudes and beliefs of clinicians influencing procedure rates? Are treatment choices related to local patient factors such as belief patterns or geography? This study takes place in the province of Saskatchewan, which had the second highest mastectomy rate of 63.4% compared with the nation’s average of 39%.23 To better understand this variation and what informs women’s treatment options, further research beginning with patient decision-making at the regional level is necessary. The objective of this study was to identify factors that influence Saskatchewan women’s choice between BCT and mastectomy in ESBC and to compare and contrast underlying reasons behind choice of BCT versus mastectomy.
Methods
Methodology
Interpretive Description was the qualitative methodology used to guide this research.24 This methodology is often used in complex clinical phenomena for applied qualitative research within health disciplines, such as nursing, psychiatry, and medicine.24–27 The philosophical basis aligns well with the researchers’ perspectives, and provides congruency between the methodology, objectives, and methods in this project.26 The choice between mastectomy and BCT can be viewed as a planned behavior. The Theory of Planned Behavior is a conceptual framework that links beliefs and behavior.28 This framework has been used to study ESBC decision-making in the past29 and helped guide this study’s framework and analysis.
Sampling and recruitment
Research Ethics Board approval was obtained from the University of Saskatchewan. The Saskatchewan Cancer Agency (SCA) provided recruitment support. Women with ESBC, who had been treated in the calendar year preceding July 2013, were identified. The SCA recruited participants by mailing letters of invitation to potential participants. A purposeful sampling plan was aimed at capturing diversity and variation in the phenomenon under study—specific characteristics identified included different age groups, minority groups, and urban versus rural location of residence. There was no incentive offered for participation. Potential research participants contacted the researchers and face-to-face interviews were arranged at the convenience of the participant.
Data collection was conducted by the lead author, who is a surgical resident and doctoral student (J.G.), and 2 research assistants who were medical students. Supervision was provided by a clinical expert (G.G) and a qualitative expert (A.L.). Interviews of 13 women who chose mastectomy and 12 women who chose BCT were included for analysis. Two mastectomy and 3 BCT interviews were excluded because the patients felt they were not offered treatment options and therefore did not engage in a decision-making process. Semi-structured interviews allowed for in-depth open-ended discussions based on questions formed from factors previously known in literature,7,8,30 as well as other clinically based hypothesized factors. All interviews were audio-recorded and transcribed verbatim.
Analysis
ATLAS.ti software was used for data management and analysis. Thematic analysis following Braun and Clarke31 was conducted. Three members of the research team, 2 interviewers and 1 qualitative expert (J.G., Y.H., A.L.), created a set of codes using sample interviews from the primary data. When appropriate, in vivo codes were created using participant’s language as labels. These codes were then sorted to create, modify, and complete an initial thematic index.
Subsequent analysis was completed by J.G. In-depth, line-by-line coding using the initial thematic index was executed through all interviews. Coding and modification of the thematic index was an iterative process. Once completed, an initial candidate thematic map was created using the Theory of Planned Behavior as a conceptual framework. Separate maps were created for the mastectomy and BCT data sets. Next, all coded data extracts for a theme were individually reviewed and refined to ensure they formed a coherent pattern. Individual themes were subsequently reviewed in relation to other themes, the concept map, as well as the data set as a whole. Reworking the codes, themes, and concepts maps was an iterative process. Constant-comparison techniques were used to confirm and challenge ideas throughout themes.25 This was done in both the mastectomy and BCT analysis, producing final results illustrated in thematic maps (Figure 1 and Figure 2). To increase the validity of findings, the “thoughtful clinician” test as described by Thorne et al25 was used. Expert clinicians with surgical oncology or breast fellowships were consulted to review study results, encouraging them to challenge or confirm the study results.
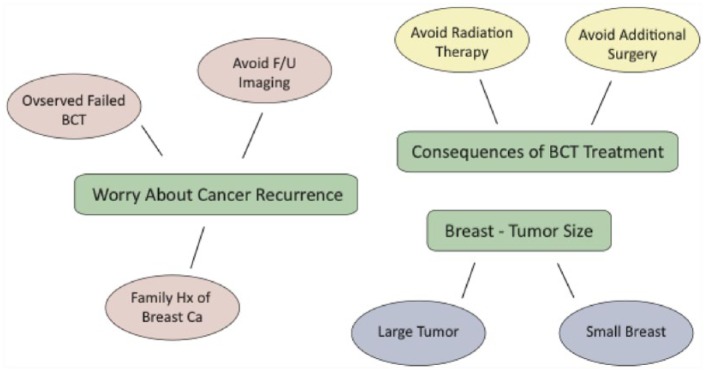
Figure 1.
Thematic map for mastectomy participants. BCT indicates breast conserving therapy; F/U, follow-up; Hx, history.
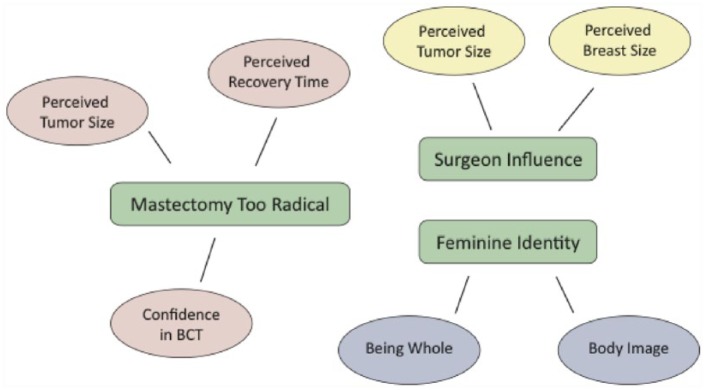
Figure 2.
Thematic map for breast conserving therapy (BCT) participants.
Audio recordings, participant transcripts, thematic indexes, concept maps, and early thematic maps are available from the authors on request.
Results
Demographics
Thirteen patients who underwent mastectomy and 12 patients who underwent BCT were interviewed. Averages ages and rural versus urban distribution of participants were comparable. Demographic data appear in Table 1.
Table 1.
Demographics.a
| Characteristic | Mastectomy (N) | BCT (N) |
|---|---|---|
| Median age in years at the time of diagnosis (range) | 64 (33–89) | 60 (46–80) |
| Participant’s home in a rural location | 4 (30.8) | 5 (41.7) |
| Participant’s home in an urban location | 9 (69.2) | 7 (58.3) |
| Participant’s home located in a tertiary center with a radiation center | 7 (53.8) | 6 (58.3) |
| Participants of a visible minority | 1 (7.7) | 1 (8.3) |
Abbreviation: BCT, breast conserving therapy.
Number in parentheses refers to percentages unless otherwise specified.
Mastectomy
Women choosing mastectomy primarily based their decision on 1 of the 3 main themes: worry about cancer recurrence, worry about consequences of BCT treatment, or perceived breast-to-tumor size. The final thematic map indicating why women chose mastectomy is shown in Figure 1.
Worry about cancer recurrence
This theme was the main reason most women chose mastectomy. Participants were concerned about cancer recurrence and wished to do everything they could to minimize this risk. This concept formed by combining 2 earlier themes, minimizing cancer recurrence and obtaining peace of mind. The choice of mastectomy relieved these participants’ concerns about breast cancer and was described as “eliminating risk,” “getting rid of it all,” and obtaining “peace of mind.” This is well exemplified through the following participant response: “And just eliminating the risk, and I am a worrier, and I would probably always be feeling my breast and think ‘oh no’” (Mastectomy participant 2). The source of worry about cancer recurrence was always related to another underlying reason; these are depicted as subthemes: observed failed BCT, avoiding follow-up imaging, and family history.
Observed failed BCT
A common reason behind worry about cancer recurrence was having a close family member or friend fail BCT. Failures were described as requiring re-excisions, having subsequent mastectomy, cancer recurrence, or death from cancer. These negative experiences from close individuals caused significant apprehension and deterred participants from believing, trusting, or pursuing BCT:
I had known always, and I’ve said this for years, but if I ever had breast cancer I would have a mastectomy. I don’t believe in lumpectomy, and I don’t believe in radiation treatments. I’ve had many friends who have had lumpectomy in the past and they’ve all had cancer recurrence. And then had to have more surgery again. So I don’t believe in lumpectomy. (Mastectomy participant 7)
Avoid follow-up imaging
Some participants did not want the continual follow-up imaging required with BCT. The process of repeated imaging tests checking for recurrence caused fear. Participants felt more comfortable having all of the breast tissue removed, knowing they would not have to deal with this source of worry. “I always thought I would always get it all taken care at once. The risk of recurrence, and the fear finding a lump again, and the fear of always checking, I would always be looking for a lump and I didn’t want that” (Mastectomy participant 3).
Familyhistory
A strong family history influenced 2 participants in their decision to choose mastectomy. This increased worry about recurrence was even evident when this 68-year-old participant said, “Even if it was a lumpectomy today, what is the chances I might not get it again . . . The guiding factor was my strong family history of breast cancer” (Mastectomy participant 13)
Consequences of BCT treatment
Some participants held firm opinions that choosing BCT would result in consequences they did not wish to experience. These were either side effects of radiation therapy or the potential of requiring more surgery. Avoidance of radiation was due to individuals observing adverse side effects afflicting someone they knew or from workplace experiences: “I didn’t like the idea of radiation, I work in the OR and I’ve seen surgeons complain of radiated fields so I did not want to have radiation. So that’s the reason I chose mastectomy” (Mastectomy participant 13). Some participants only wanted surgery once, not wanting to risk reoperation. Although wanting to avoid radiation and reoperation risk were often related, only one was central in the decision to have mastectomy.
Breast—tumor size
The size in this theme refers to what was perceived by the participant throughout their treatment interactions. The perceptions of having a large tumor, small breast, or a large tumor to small breast ratio were important influences in the choice of mastectomy:
I remember in my mind lumpectomy was never an option. I never was considering it. Because of the size of the tumor I just wanted the whole breast gone. And with lumpectomy I wouldn’t have been left with very much breast tissue anyways. (Mastectomy participant 8)
Breast conserving therapy
The central themes that influenced women to choose BCT were mastectomy being too radical, surgeon influence, and feminine identity. The final thematic map illustrating why women chose BCT is shown in Figure 2.
Mastectomy too radical
Having the entire breast removed with a mastectomy was viewed as being too radical or extreme for the stage of disease the patient felt they had. Mastectomy being too radical was related to some main subthemes: perceived recovery time, perceived tumor size, and confidence in BCT.
Perceived recovery time
The subjective difference in the impact of operation between mastectomy and BCT surgery influenced women’s decision-making. Participants choosing BCT wanted surgery that put less stress on the body, had a shorter recovery time, and less overall effect on their life. This was sometimes due to participant’s older age or comorbid disease:
I wanted the one that took less time, had less impact on my life. I think the mastectomy would have taken more time to recover. A friend of mine has gone through it, she is still off of work and it has been almost three years. She has gone through a lot of struggles and physiotherapy and I felt lucky that we caught it early and I didn’t have to deal with that part. (BCT participant 12)
Perceivedtumor size
A central reason behind many women’s decision for BCT was that mastectomy was viewed as too radical relative to the size of the tumor. Several participants felt that they did not need a drastic surgery to control a small tumor: “Because it had been so small, if it was massive I would say look let’s do something major. It was so small why should I lose a whole breast” (BCT participant 6).
Confidence in BCT
Several women explicitly expressed confidence in BCT treatment and were comfortable with potential consequences from this approach. Furthermore, they acknowledged the possibility of a further surgery, preferring a “staged approach”:
I think because there is less complications if I go that way. Also I have a second chance to go that way if I have to. I have a firm belief that science has come so far over the years. Those things were encouraging for me. (BCT participant 11)
Surgeon influence
Surgeon influence was a common reason that resulted in women choosing BCT. The surgeon was held as an important referent whose opinion was highly valued. In fact, several women completely defaulted their treatment decision to their surgeon’s recommendation. These women expressed strong trust and faith in their surgeon:
And of course he influenced it—he knows more about the area than I do. And when he said if it was his mother he would recommend the lumpectomy. . . even though you are a retired health care provider its different when you are on the other side of the fence. You don’t think logically. It was mostly his recommendation to have the lumpectomy. (BCT participant 5)
Often, the recommendation for BCT was due to the perceived small size of the tumor from the surgeon’s perspective. This idea was repeatedly cited by participants: ‘Whatever the surgeon recommended I was willing to do . . . after she explained to me how small the tumor was and the treatment available I didn’t even have to think about it” (BCT participant 12).
Feminine identity
Feminine identity encompassed the ideas of self-esteem related to body image, retaining one’s own breast, and feeling whole as a woman. Participants felt that breasts were an important part of their body image, which affected their individual and feminine identity. Furthermore, women explained that breasts are an important part of their feminine identity, and keeping them was central to feeling whole as a person: “It is really important for me to maintain that female body form. So the image for me was huge, for my self esteem” (BCT Participant 3).
Discussion
The aim of this study was to explore the decision-making of women in Saskatchewan with ESBC and identify key themes underlying the choice of mastectomy or BCT. The main themes identified by the 2 treatment groups were different, suggesting that women chose to undertake mastectomy or BCT for different reasons. Although the individual reasons found in this study have been seen in previous literature,29,32,33 choice of mastectomy or BCT has not previously been described as having completely different reasons underlying each choice of therapy. Furthermore, the identification of subthemes or secondary reasons for each choice is also a novel observation in this study. The thematic maps created are useful tools for providing visual depictions of decision-making factors for patients and health care workers.
Fear and worry about cancer recurrence have been found in the literature to be an important reason behind women choosing mastectomy32,33 and often the most influential factor for treatment decision-making.11,22,29 This study confirmed the significance of worry and that these feelings were related to an additional underlying reason: observed failed BCT, avoiding follow-up imaging, or family history. A secondary level of connection has never been previously identified in the breast cancer literature and would be an important area of further exploration. The most common subtheme was related to a close family member or friend with ESBC having a negative BCT or positive mastectomy experience, which influenced choice. This has been known to affect decision-making and cancer risk assessment for patients in the past; other studies have suggested patients make choices based on experiential interpretation instead of on statistical probabilities.19,32 Despite clinician’s explanations of equivalent survival, the subjectively perceived risk of each treatment option often supersedes the objective information given.34 A plausible explanation for this theme’s prominence in this study is that Saskatchewan has many smaller communities, both urban and rural, which may contribute to greater communication between residents about cancer experiences. This is an area that requires further research.
Smaller breast and larger tumor size are well-known factors to increase the likelihood of undergoing mastectomy.16,30 This study confirms these findings qualitatively and increases the depth of understanding of previously observed data. Two participants felt that BCT was never an option due to the perceived breast or tumor size and were therefore excluded from the study. This is likely explained because a large tumor to breast ratio is a relative contraindication to BCT.35
A proportion of women chose mastectomy to avoid consequences of BCT treatment: length of treatment required for radiation, side effects specific to radiation, and risk of re-excision due to a positive margin. Other studies have identified similar trends.19,21 These may be due to poor communication or understanding of side effects specific to breast radiation. Further investigations into these specific factors are required.
Mastectomy being considered too radical was an important reason women chose BCT in this study; choice was related to recovery time from surgery, perceived tumor size, and confidence in the BCT approach. Choosing BCT to avoid extensive surgery has been previously discussed in the literature, especially for older age groups.11,36 Prior studies using surveys have commonly reported equivalent survival between BCT and mastectomy as a main reason for choosing BCT, listing “equivalent survival” as a selection item.11,21 In contrast, our study used open-ended questions, which resulted in mastectomy being too radical as the emerging central theme. These results suggest that it is not only the knowledge that survival between treatments is equal, but given the early-stage of disease, mastectomy is viewed as an extreme treatment option. A perception that the tumor size was small also influenced patient views of mastectomy being radical. Although quantitative data have consistently associated smaller tumor size with higher BCT rates,7–9 this study provides an explanation behind this finding.
There have been varying results in the literature as to whether distance to radiation center affects rates of BCT. Although several studies show a decreasing rate of BCT as distance to radiation center increases,15 there are numerous studies that show no difference.15,18,19 Despite Saskatchewan’s large rural population, this study did not find that travel distance to a radiation treatment center deterred choice of BCT. Regional investigation on a larger scale may be important to confirm this finding.
Surgeon influence was a primary reason underlying many women’s choice of BCT. Those who had difficulty choosing between therapies would often default to the surgeon’s recommendation. Literature has previously shown surgeon influence and recommendations to be an important factor in treatment decision-making.11,29,37 A unique finding in this study, differing from the previous literature, was that surgeon influence was only an important theme underlying women’s choice of BCT and was not a significant theme affecting those who chose mastectomy. This is an important distinction that should be considered for future research.
The theme of feminine identity was an important reason many women chose BCT. In our study, this theme encompassed the ideas of body image, feeling whole as a female, and keeping one’s own breast tissue. The influences of these ideas have individually been identified previously as important factors influencing women choosing BC.21,22,29
Limitations
This study was retrospective, which presents potential limitations including recall bias and post-treatment experiences. It is possible patients reported their decisions based on post hoc justification instead of the reasons that were important at the time of decision-making. Patients were recruited based on chart review clinical criteria for ESBC. However, whether explicit choice of therapy was offered versus a lapse in memory during the encounter was unclear in some circumstances, which may lead to unnecessary exclusion from this study. Other studies have identified that patient recall of events surrounding cancer diagnosis may be problematic.38,39 In addition, the type, amount, and style of information presented from physicians may have varied. Our sampling plan included diversity in minority groups, but unfortunately this was not achieved due to lack of recruitment response. A targeted recruitment strategy may be required in future studies to capture these groups.
Implications for practice and research
This article has added understanding to reasons behind choice of therapy for women with ESBC. This insight, along with the thematic maps, will help guide clinicians and allied health care workers counsel and care for patients going through this complicated decision-making process. Some of the novel findings, including separate reasons for choosing mastectomy versus BCT, should be further explored in future research. Generalizability of these results should be established in large-scale survey research and research across different areas of the country.
Acknowledgments
The authors would like to thank Saskatchewan Cancer Agency, Anne Leis, Yasmine Halat, Ricarda Bentham, and SCA nurses for their contribution in this study.
Footnotes
Peer review:Two peer reviewers contributed to the peer review report. Reviewers’ reports totaled 737 words, excluding any confidential comments to the academic editor.
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: GG and JG contributed to the study conception and design. All authors contributed to acquisition and analysis of data, revising the manuscript, and approval of the final version of the manuscript to be published.
References
- 1. Canadian Partnership Against Cancer. Breast Cancer Control in Canada: A System Performance Special Focus Report. Toronto, ON: Canadian Partnership Against Cancer; 2012. [Google Scholar]
- 2. Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–1241. [DOI] [PubMed] [Google Scholar]
- 3. Morrow M, Strom EA, Bassett LW, et al. Standard for breast conservation therapy in the management of invasive breast carcinoma. CA Cancer J Clin. 2002;52:277–300. [DOI] [PubMed] [Google Scholar]
- 4. Arriagada R, Le MG, Rochard F, Contesso G. Conservative treatment versus mastectomy in early breast cancer: patterns of failure with 15 years of follow-up data. Institut Gustave-Roussy Breast Cancer Group. J Clin Oncol. 1996;14:1558–1564. [DOI] [PubMed] [Google Scholar]
- 5. van Dongen JA, Voogd AC, Fentiman IS, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European organization for research and treatment of cancer 10801 trial. J Natl Cancer Inst. 2000;92:1143–1150. [DOI] [PubMed] [Google Scholar]
- 6. Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health Aff. 2002:W96–114. Available at: content.healthaffairs.org/webfirst/index.dtl?year=2002 [DOI] [PubMed] [Google Scholar]
- 7. Mac Bride MB, Neal L, Dilaveri CA, et al. Factors associated with surgical decision making in women with early-stage breast cancer: a literature review. J Womens Health. 2013;22:236–242. [DOI] [PubMed] [Google Scholar]
- 8. Roder D, Zorbas H, Kollias J, et al. Factors predictive of treatment by Australian breast surgeons of invasive female breast cancer by mastectomy rather than breast conserving surgery. Asian Pac J Cancer Prev. 2013;14:539–545. [DOI] [PubMed] [Google Scholar]
- 9. Teh YC, Shaari NE, Taib NA, et al. Determinants of choice of surgery in Asian patients with early breast cancer in a middle income country. Asian Pac J Cancer Prev. 2014;15:3163–3167. [DOI] [PubMed] [Google Scholar]
- 10. Pappo I, Karni T, Sandbank J, et al. Breast cancer in the elderly: histological, hormonal and surgical characteristics. Breast. 2007;16:60–67. [DOI] [PubMed] [Google Scholar]
- 11. Cyran EM, Crane LA, Palmer L. Physician sex and other factors associated with type of breast cancer surgery in older women. Arch Surg. 2001;136:185–191. [DOI] [PubMed] [Google Scholar]
- 12. Caldon LJ, Walters SJ, Reed JA, Murphy A, Worley A, Reed MW. Case-mix fails to explain variation in mastectomy rates: management of screen-detected breast cancer in a UK region 1997-2003. Br J Cancer. 2005;92:55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. White V, Pruden M, Giles G, et al. The management of early breast carcinoma before and after the introduction of clinical practice guidelines. Cancer. 2004;101:476–485. [DOI] [PubMed] [Google Scholar]
- 14. Killoran M, Moyer A. Surgical treatment preferences in Chinese-American women with early-stage breast cancer. Psychooncology. 2006;15:969–984. [DOI] [PubMed] [Google Scholar]
- 15. Sauerzapf VA, Jones AP, Haynes R, Crawford SM, Forman D. Travel time to radiotherapy and uptake of breast-conserving surgery for early stage cancer in Northern England. Health Place. 2008;14:424–433. [DOI] [PubMed] [Google Scholar]
- 16. Celaya MO, Rees JR, Gibson JJ, Riddle BL, Greenberg ER. Travel distance and season of diagnosis affect treatment choices for women with early-stage breast cancer in a predominantly rural population (United States). Cancer Causes Control. 2006;17:851–856. [DOI] [PubMed] [Google Scholar]
- 17. Boscoe FP, Johnson CJ, Henry KA, et al. Geographic proximity to treatment for early stage breast cancer and likelihood of mastectomy. Breast. 2011;20:324–328. [DOI] [PubMed] [Google Scholar]
- 18. Hall SE, Holman CD, Hendrie DV, Spilsbury K. Unequal access to breast-conserving surgery in Western Australia 1982-2000. ANZ J Surg. 2004;74:413-419. [DOI] [PubMed] [Google Scholar]
- 19. McVea KL, Minier WC, Johnson Palensky JE. Low-income women with early-stage breast cancer: physician and patient decision-making styles. Psychooncology. 2001;10:137–146. [DOI] [PubMed] [Google Scholar]
- 20. Nold RJ, Beamer RL, Helmer SD, McBoyle MF. Factors influencing a woman’s choice to undergo breast-conserving surgery versus modified radical mastectomy. Am J Surg. 2000;180:413–418. [DOI] [PubMed] [Google Scholar]
- 21. Benedict S, Cole DJ, Baron L, Baron P. Factors influencing choice between mastectomy and lumpectomy for women in the Carolinas. J Surg Oncol. 2001;76:6–12. [DOI] [PubMed] [Google Scholar]
- 22. Schou I, Ekeberg Ø, Ruland CM, Kåresen R. Do women newly diagnosed with breast cancer and consulting surgeon assess decision-making equally? Breast. 2002;11:434–441. [DOI] [PubMed] [Google Scholar]
- 23. Canadian Partnership Against Cancer. The 2015 Cancer System Performance Report. Toronto, ON: Canadian Partnership Against Cancer; 2015. [Google Scholar]
- 24. Thorne S, Kirkham SR, MacDonald-Emes J. Interpretive description: a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health. 1997;20:169–177. [DOI] [PubMed] [Google Scholar]
- 25. Thorne S, Reimer Kirkham S, O’Flynn-Magee K. The analytic challenge in interpretive description. Int J Qual Methods. 2004;3:1–11. [Google Scholar]
- 26. Thorne S. Interpretive Description. Walnut Creek, CA: Left Coast Press; 2008. [Google Scholar]
- 27. Hunt MR. Strengths and challenges in the use of interpretive description: reflections arising from a study of the moral experience of health professionals in humanitarian work. Qual Health Res. 2009;19:1284–1292. [DOI] [PubMed] [Google Scholar]
- 28. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 29. Temple WJ, Russell ML, Parsons LL, et al. Conservation surgery for breast cancer as the preferred choice: a prospective analysis. J Clin Oncol. 2006;24:3367–3373. [DOI] [PubMed] [Google Scholar]
- 30. Chagpar AB, Studts JL, Scoggins CR, et al. Factors associated with surgical options for breast carcinoma. Cancer. 2006;106:1462-1466. [DOI] [PubMed] [Google Scholar]
- 31. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 32. Covelli AM, Baxter NN, Fitch MI, McCready DR, Wright FC. “Taking control of cancer”: Understanding women’s choice for mastectomy. Ann Surg Oncol. 2015;22:383–391. [DOI] [PubMed] [Google Scholar]
- 33. Molenaar S, Oort F, Sprangers M, et al. Predictors of patients’ choices for breast-conserving therapy or mastectomy: a prospective study. Br J Cancer. 2004;90:2123–2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zikmund-Fisher BJ, Fagerlin A, Ubel PA. Risky feelings: why a 6% risk of cancer does not always feel like 6%. Patient Educ Couns. 2010;81:S87–S93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. NCCN Breast Cancer Panel Members. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Breast Cancer. Fort Washington, PA: National Comprehensive Cancer Network; 2014. [Google Scholar]
- 36. Newschaffer CJ, Penberthy L, Desch CE, Retchin SM, Whittemore M. The effect of age and comorbidity in the treatment of elderly women with nonmetastatic breast cancer. Arch Intern Med. 1996;156:85–90. [PubMed] [Google Scholar]
- 37. Stafford D, Szczys R, Becker R, Anderson J, Bushfield S. How breast cancer treatment decisions are made by women in North Dakota. Am J Surg. 1998;176:515–519. [DOI] [PubMed] [Google Scholar]
- 38. Meyer BJ, Russo C, Talbot A. Discourse comprehension and problem solving: decisions about the treatment of breast cancer by women across the life span. Psychol Aging. 1995;10:84–103. [DOI] [PubMed] [Google Scholar]
- 39. Shapiro DE, Boggs SR, Melamed BG, Graham-Pole J. The effect of varied physician affect on recall, anxiety, and perceptions in women at risk for breast cancer: an analogue study. Health Psychol. 1992;11:61–66. [DOI] [PubMed] [Google Scholar]