Abstract
Objective
To evaluate established opioid addiction treatment programs that use traditional healing in combination with buprenorphine-naloxone maintenance treatment in 6 First Nations communities in the Sioux Lookout region of northwestern Ontario.
Design
Retrospective cohort study.
Setting
Six First Nations communities in northwestern Ontario.
Participants
A total of 526 First Nations participants in opioid-dependence treatment programs.
Intervention
Buprenorphine-naloxone substitution therapy and First Nations healing programming.
Main outcome measures
Retention rates and urine drug screening (UDS) results.
Results
Treatment retention rates at 6, 12, and 18 months were 84%, 78%, and 72%, respectively. We estimate that the rate at 24 months will also be more than 70%. The UDS programming varied and was implemented in only 1 community. Initially urine testing was voluntary and it then became mandatory. Screening with either method found the proportion of urine samples with negative results for illicit opioids ranged between 84% and 95%.
Conclusion
The program’s treatment retention rates and negative UDS results were higher than those reported for most methadone and buprenorphine-naloxone programs, despite a patient population where severe posttraumatic stress disorder is endemic, and despite the programs’ lack of resources and addiction expertise. Community-based programs like these overcome the initial challenge of cultural competence. First Nations communities in other provinces should establish their own buprenorphinenaloxone programs, using local primary care physicians as prescribers. Sustainable core funding is needed for programming, long-term aftercare, and trauma recovery for such initiatives.
Résumé
Objectif
Évaluer les programmes de traitement de la dépendance aux opiacés qui combinent médecine traditionnelle et traitement de soutien à la buprénorphine-naxolone instaurés dans 6 collectivités des Premières Nations de la région Sioux Lookout du nord-ouest de l’Ontario.
Type d’étude
Étude de cohorte rétrospective.
Contexte
Six collectivités des Premières Nations du nord-ouest de l’Ontario.
Participants
Un total de 526 membres des Premières Nations participant aux programmes de traitement de la dépendance aux opiacés.
Intervention
Instauration d’un programme de traitement combinant médecine traditionnelle autochtone et traitement de substitution avec buprénorphine-naxolone.
Principaux paramètres à l’étude
Taux de rétention et résultats de la recherche de drogues dans l’urine (RDU).
Résultats
Après 6, 12 et 18 mois de traitement, les taux de rétention étaient de 84 %, 78 % et 72 %, respectivement. Nous prévoyons qu’à 24 mois, le taux sera encore de plus de 70 %. La RDU a été effectuée de façon irrégulière et seulement dans une communauté. Au début, ce test d’urine était optionnel, mais il est ensuite devenu obligatoire. La proportion de résultats négatifs à ce dépistage variait entre 84 % et 95 %, quelle que soit la méthode utilisée.
Conclusion
Les taux de rétention pour ces programmes et la proportion de résultats négatifs aux RDU sont plus élevés que ceux qui ont été rapportés pour la plupart des programmes de méthadone et de buprénorphine-naxolone, et ce, malgré une population de patients où les cas de stress post-traumatique grave sont endémiques et en l’absence des ressources et de l’expertise nécessaires pour traiter la dépendance. Des programmes communautaires de ce type évitent l’obstacle initial de la compétence culturelle. Il serait opportun que les collectivités des Premières Nations des autres provinces établissent leurs propres programmes de buprénorphine-naloxone, leurs médecins de première ligne se chargeant alors des prescriptions. Ces initiatives exigeront aussi un financement soutenu pour la création des programmes, pour le suivi à long terme des patients et pour leur période de rétablissement.
Since the opioid crisis began in the late 1990s, remote northwestern Ontario First Nations communities have experienced a massive surge in the prevalence of opioid addiction.1,2 The Nishnawbe Aski Nation, in a news release in 2012, estimated that 9000 community members of a population of 25 000 in the Sioux Lookout region of northwestern Ontario were opioid dependent.3 A recent study of one community north of Sioux Lookout estimated that 41% of the adults aged 20 to 50 were opioid dependent.1 First Nations band councils and addiction workers report that opioid-related overdoses, crime, social dysfunction, and addiction are common in their communities.4
Until recently, treatment options have been limited. Abstinence-based programs have high relapse rates and have involved traveling out of the community to an urban treatment centre.5 Methadone treatment is not feasible in many isolated First Nations communities, as they lack a methadone prescriber, a pharmacy open 7 days per week, and emergency services.
In 2012, the Ontario provincial drug plan added buprenorphine-naloxone to its formulary, and the Non-Insured Health Benefits program (which provides drug coverage for First Nations communities) followed suit. The College of Physicians and Surgeons of Ontario permits all physicians to prescribe buprenorphine-naloxone, even if they do not have a methadone licence. This has allowed community leaders and physicians in Ontario First Nations communities to design and implement their own buprenorphine-naloxone maintenance treatment programs. Buprenorphine-naloxone is a partial opioid agonist with a long duration of action. It has a much lower risk of overdose than methadone does, but also has lower treatment retention rates.6–8 Buprenorphine-naloxone is a combination medication that includes buprenorphine, a long-acting opioid with strong opioid-receptor affinity, and naloxone, an opioid antagonist. When used sublingually, very little naloxone is absorbed, but if the drug is diverted to intravenous use, withdrawal symptoms ensue—hence it has a builtin diversion deterrent.
The Sioux Lookout catchment area consists of 32 remote First Nations communities with a land mass of 385 000 km2 and a total population of 25 000.9 Twenty-two of the northern communities have started their own buprenorphine-naloxone programs, with a total of 1399 participants. Buprenorphine-naloxone treatment is initiated either by the community physician, who visits each community 1 week a month, or by urban addiction physicians who act as fly-in locums. Follow-up is in person or by telemedicine. The community physician continues treatment, including dose changes, weaning, and other addiction and general medical needs.
A recent study documented remarkable results from a buprenorphine-naloxone program in one regional community, with dramatically reduced rates of crime and increased rates of school attendance.1 The study measured only community outcomes. This current study is the first to report on treatment retention rates and urine drug screening (UDS) results for buprenorphine-naloxone maintenance programs in the Sioux Lookout region.
METHODS
Treatment setting
We conducted a retrospective cohort study. Six First Nations communities who requested program evaluation (with a total population of 4388) participated in the study. All are located north of the town of Sioux Lookout, where the Sioux Lookout Meno Ya Win Health Centre serves as their regional medical hub for primary and hospital care.9 The population, medication use, and laboratory values were calculated from the physician-based electronic medical records (EMRs), which recorded buprenorphine-naloxone prescriptions. Population estimates were based on all patients covered by Ontario health insurance within each community, as listed in the EMR.
Program description
Administration and staffing
All 6 communities began providing buprenorphine-naloxone substitution in the summer or fall of 2012 and into 2013. Each community designed its own program and complement of staff and consultants. Communities provide a facility for the program, often in an unused or refurbished building. The programs are overseen by the band chief and council, the Health Director, and community leaders. The service delivery team consists of the local program coordinator, medication dispensers, consultant counselors, nurses, and physicians. Community nurses initiate bloodwork on admission to the program. Participants are self-referred. The local capacity to provide direct, observed therapy was often a limiting factor for inductions. Patients were admitted to the program on a first-come, first-served basis if they met the diagnostic criteria for opioid use disorder.10
Buprenorphine-naloxone prescriptions
Patients were often started on buprenorphine-naloxone in group inductions of 10 to 25 patients at a time, depending on funding and the availability of clinical personnel. Often inductions were initiated by visiting community physicians; if available, addiction physicians from urban centres assisted during group inductions. The physician completes a comprehensive assessment of all patients, and those who meet the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, criteria for opioid use disorder10 begin taking buprenorphine-naloxone when they have provided informed consent. Community physicians, who visit each community for 1-week periods each month, prescribe follow-up buprenorphine-naloxone doses. The buprenorphine-naloxone is dispensed daily under the supervision of a community nurse or community addiction worker. Take-home doses are prescribed by the addiction physician or the community physician in consultation with other members of the treatment team. A locally developed physician prescribing guideline was developed to assist induction prescribing and maintenance dosing.
Counseling
After induction, the group attends 4 weeks of intensive day treatment and aftercare. All programs provide daily, supervised dispensing of buprenorphine-naloxone. A “Land” aftercare program has been developed in some of the communities, with organized days of fishing, hunting, traditional walks for memorial events, and community gardening programs. Elders and experienced First Nations counselors provide individual and group healing sessions where possible. Some communities hire counselors from outside of the community if resources permit. In many programs, the community physician provides the core clinical support.
Data collection
The 6 programs started buprenorphine-naloxone substitution in the summer or fall of 2012 and into 2013. Data were collected from the start of each program until July 2015. Because UDS was only randomly available for that time period, we also included initial UDS results from early 2016, when it became mandatory in 1 community.
Information on buprenorphine-naloxone prescribing was accessed through the regional EMR system. Patients were considered retained in treatment from the date of their first buprenorphine-naloxone prescription until their last prescription ended. Twelve-month retention rates were calculated for patients who started buprenorphine-naloxone 12 months before July 2015. Buprenorphine-naloxone dosing data were available from 1 of the 6 communities and were analyzed for induction dose and the dose at every 6-month follow-up.
Urine drug screening was performed systematically in only 1 of the 6 communities. In 2014 and 2015, random and voluntary monthly testing was performed in the summer months. Urine testing was performed on 4 randomly chosen days during the summer (May to August). In 2016, monthly UDS became mandatory in that community. Point-of-care urine dipsticks were used to test for cocaine, oxycodone, morphine, benzodiazepines, and buprenorphine.
Diabetes prevalence was estimated by review of EMRs for all hemoglobin A1c results above 6.5% in the study period, measured against total community populations. We chose to compare the prevalence of diabetes with that of opioid use disorder, as diabetes is a disease that attracts core funding and programming in federal funding schemes, while opioid use disorder and aftercare programming goes wanting. We chose to compare prevalences in the 20- to 50-year-old age group, as nearly all those receiving opioid agonist therapy with buprenorphine-naloxone were in that age group.
Suicide events were enumerated from internal documents from the Sioux Lookout First Nations Health Authority, as specifically requested by the 6 community Health Directors. Examination of drug involvement in these events was outside the scope of this study. Data were entered using Excel 2013, and analyses were completed using SPSS, version 21.0. Descriptive statistics were obtained in addition to
 2 tests for independence.
2 tests for independence.
Ethics approval
The study was launched in response to a request from 6 communities to evaluate their treatment programs. Ethics approval was granted by the Sioux Lookout Meno Ya Win Health Centre Research Review and Ethics Committee. The evaluation received partial funding from the Northern Ontario Academic Medicine Association. Most of the investigators on this study are also clinicians working in Sioux Lookout or community leaders.
RESULTS
Patient characteristics
In the 6 communities, 526 individuals were treated with buprenorphine-naloxone. The mean (SD) age was 32.3 (8.4) years; 55% were women. Most (96%) program participants were in the 20- to 50-year-old age range (Table 1). The rate of opioid-dependence treatment for adults in this population group was 28% (504 of 1800). We also surveyed the prevalence of type 2 diabetes mellitus in the same age group and found a prevalence of 14%.
Table 1.
Age distribution of community members prescribed buprenorphine-naloxone in 2013 to 2015
| AGE, Y | PARTICIPANTS, N (%) |
|---|---|
| < 20 | 6 (1) |
| 20–29 | 247 (47) |
| 30–39 | 184 (35) |
| 40–49 | 73 (14) |
| 50–59 | 13 (2) |
| ≥ 60 | 3 (1) |
| Total | 526 (100) |
Buprenorphine-naloxone dose
Doses were analyzed in only 1 community. The mean (SD) dose of buprenorphine-naloxone was 15.6 (5.8) mg at the end of the 1-week induction (n = 163), falling to 11.3 (6.8) mg at 6 months, 6.0 (3.6) mg at 18 months, and 6.1 (4.1) mg at 24 months.
Treatment retention
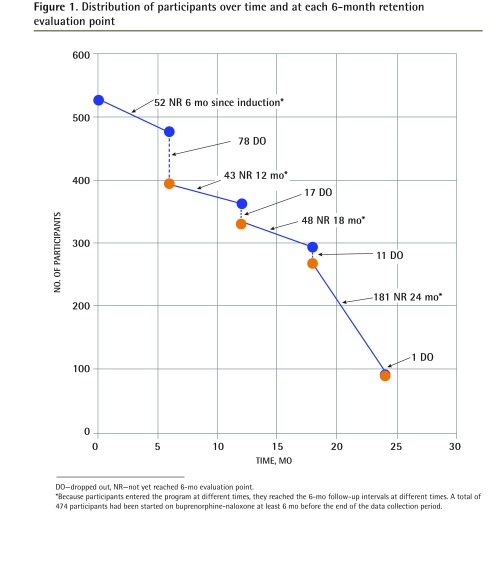
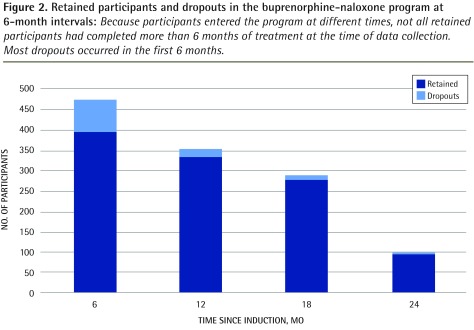
Retention rates were measured at 6, 12, 18, and 24 months (Table 2 and Figures 1 to 3). Of the 526 patients in the total sample, 474 had started buprenorphine-naloxone treatment at least 6 months before the end of the data collection period. Of these 474 patients, 396 were taking buprenorphine-naloxone for at least 6 months, for a retention rate of 84%. Of these 396 patients, 43 had started taking buprenorphine-naloxone less than 12 months before the end of data collection; of the remaining 353 patients, 17 dropped out, for a 12-month retention rate of 78%. Using similar calculations, the 18-month treatment retention rate was 72%, and the 24-month retention rate is estimated to be more than 70%.
Table 2.
Dropouts and retention rates at 6-month intervals since induction
| TIME SINCE INDUCTION, MO | NO. OF PARTICIPANTS (RETAINED AND DROPOUTS)* | RETAINED, N (%) | DROPOUTS, N | CUMULATIVE DROPOUTS |
|---|---|---|---|---|
| ≥ 6 | 474 | 396 (84) | 78 | 78 |
| ≥ 12 | 431 | 336 (78) | 17 | 95 |
| ≥ 18 | 383 | 277 (72) | 11 | 106 |
| ≥ 24 | 202 | 95 (estimated > 70)† | 1 | 107 |
Six months had not yet elapsed since induction for 52 of the 526 total participants at the time of data collection; 43 participants had not yet completed 12 months of treatment, 48 had not yet completed 18 months, and 181 had not yet completed 24 months.
We expect that most of the 181 participants who had not yet completed 24 months of treatment will be retained.
Figure 1.
Distribution of participants over time and at each 6-month retention evaluation point
DO—dropped out, NR—not yet reached 6-mo evaluation point.
*Because participants entered the program at different times, they reached the 6-mo follow-up intervals at different times. A total of 474 participants had been started on buprenorphine-naloxone at least 6 mo before the end of the data collection period.
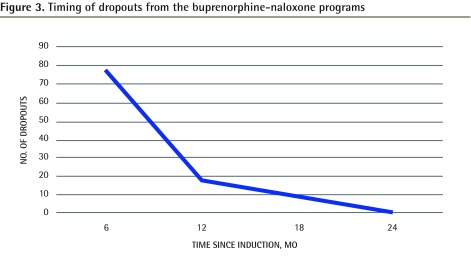
Figure 3.
Timing of dropouts from the buprenorphine-naloxone programs
Urine drug screening
Random, voluntary UDS in the 1 community that initiated it in May to August of 2014 and 2015 captured between 50% and 90% of program participants each month. The results demonstrated that between 84% and 95% of UDS results were positive for buprenorphine and negative for oxycodone, morphine, cocaine, or benzodiazepines.
Mandatory monthly UDS was initiated in January of 2016, after the end of the data collection period, and documented similarly high rates of negative results (Table 3). In January, 16 patients had a combination of urine findings positive for oxycodone (n = 10), morphine (n = 9), and cocaine (n = 4). February included 12 patients with positive urine findings: morphine (n = 10), oxycodone (n = 5), and benzodiazepines (n = 1).
Table 3.
Mandatory UDS results in 1 participating community
| MONTH (2016) | PATIENTS IN THE PROGRAM, N | PATIENTS OUT OF THE COMMUNITY, N | PATIENTS TESTED, N (%) | PATIENTS WITH UDS RESULTS NEGATIVE* FOR ILLICIT DRUGS, N (%) | PATIENTS WITH UDS RESULTS POSITIVE FOR ILLICIT DRUGS, N (%) |
|---|---|---|---|---|---|
| January | 148 | 20 | 128 (100) | 112 (88) | 16 (12) |
| February | 148 | 27 | 121 (100) | 109 (90) | 12 (10) |
UDS—urine drug screening.
A negative UDS result refers to test results positive for buprenorphine alone.
Suicides
Suicides in these 6 communities declined significantly (P = .035) from 9 cases in the 3-year period of 2009 to 2011 to 2 cases in the subsequent 3-year period during which buprenorphine-naloxone programming began (2012 to 2014).
DISCUSSION
This study confirms the extraordinarily high prevalence of opioid addiction in First Nations communities. Among adults aged 20 to 50 years, 28% were taking buprenorphine-naloxone, double the prevalence of adults in these communities with type 2 diabetes (14%).
This paper is the first, to our knowledge, to report on the effectiveness of buprenorphine-naloxone maintenance programs in rural, aboriginal communities, in Canada or elsewhere. A recent study of an inpatient detoxification program in Sioux Lookout, using a rapid taper of buprenorphine-naloxone, reported relapse rates of 52% after 2 weeks and 70% after 6 months, confirming that tapering and detoxification are of limited usefulness in the treatment of opioid addiction.11
The 6-month treatment retention rate of 84% is higher than rates reported for most methadone and buprenorphine-naloxone programs in the United States and Canada. In a review of 9555 new methadone treatment episodes in Ontario between 1996 and 2001, 2-year treatment retention rates were only 50%.12 Six-month retention rates for buprenorphine-naloxone programs in the United States range from 36% to 78%.13–16 The few studies of buprenorphine-naloxone programs that have reported 12-month outcomes record rates of 25% to 75%.17,18
In these community-based programs, the high retention rates and low rates of illicit opioid use are consistent with the positive community-wide results of an earlier study in 1 of the 6 communities.1 In that report, changes were measured for crime rates, addiction-related medical evacuations, and other outcomes after the introduction of buprenorphine-naloxone programming. One year after the buprenorphine-naloxone program started, criminal charges had fallen by 61.1%, child protection cases had fallen by 58.3%, and school attendance rates had increased by 33.3%.1 Drug-related medical evacuations to hospital fell by 30.0%.1
The 6 communities studied here have experienced a dramatic decline in suicides (P = .035) during the 3-year time period of the initiation of the buprenorphine-naloxone programs compared with the preceding 3-year period. Community Health Directors had requested this statistic be included in the program evaluation, but our mandate did not extend to examining associated individual factors, such as concurrent opioid use or demographic information. We cannot therefore attribute a causal relationship between the reduction in suicides and addiction treatment programming.
The success of the programs runs counter to current knowledge about medication, patient, and treatment factors that affect treatment retention. Systematic reviews have demonstrated that buprenorphine has lower treatment retention rates than methadone does.8 Yet Sioux Lookout patients required rather low buprenorphine-naloxone doses of 6.0 mg at 18 months (the usual therapeutic range is 8 to 16 mg) and have retention rates of 78% at the 1-year mark. In some communities, this could be because participants were not daily users and therefore had a lower degree of physical dependence. Despite this, we know anecdotally that in several of the communities included in this study, there were histories of daily intravenous opioid use for greater than 5 years.
Further, many Sioux Lookout region patients have characteristics that have been associated with poor outcomes. Our clinical impression is that community members use illicit opioids often purchased from drug dealers, rather than oral opioids acquired from physicians’ prescriptions; illicit opioid users have higher rates of treatment dropout than oral prescription opioid users do.19,20
Also, compared with the general population, First Nations individuals have substantially higher rates of depression, posttraumatic stress disorder, and binge drinking.21 These factors are associated with an increased severity of addiction (eg, earlier onset of injection drug use).22
Another factor that would normally have predicted a poor outcome is that the 6 treatment programs lacked the expertise and resources that other methadone or buprenorphine-naloxone programs in Ontario have. Primary care physicians, community nurses, and addiction workers have little or no training in opioid substitution therapy; none of the family physicians has an exemption to prescribe methadone. All health care workers managed buprenorphine-naloxone patients on top of their regular duties, which were already very demanding. The few on-site mental health and addiction workers have little training in opioid substitution therapy.
Given these negative prognostic factors, the high treatment retention rates deserve further study. One possible explanation is that the 6 programs were funded, designed, and implemented by each individual community, and their approach differs radically from that of other opioid substitution programs in North America. In a typical program, the primary relationship is between the individual patient and the physician or counselor. The Sioux Lookout programs, in contrast, are primarily a community-wide “welcoming back” of addicted patients to their families and their previous roles. Groups of 10 to 20 patients start taking buprenorphine-naloxone on the same day. The induction is a community event, where local leaders, friends, and relatives congratulate the inductees. Psychosocial treatment programs lack formal activities such as group therapy; instead they are meeting places where patients can gather and hold healing circles and other traditional events. Families expect patients to resume parenting, work, school, or family obligations. The primary care physician who prescribes buprenorphine-naloxone also provides medical care for the patient’s family and community.
Limitations
The study has important limitations. Much of the clinical information for participants was inaccessible, as it was contained in paper charts in 6 remote locations at considerable distance from one another. Results of the baseline patient assessment were not recorded in the EMR, so we do not know the patients’ type, route, or dose of opioids used. Urine toxicology results were not systematically available. Treatment retention rates were calculated over 6-month intervals, so some information will have been lost (for example, data from participants who started taking buprenorphine-naloxone within 6 months of July 2015 were not included). The 24-month evaluation time had not yet occurred for a large cohort of participants (n = 181). Information on the disposition of dropouts is unknown; they might have remained opioid free or returned to illicit drug use. The relationship between the reduction in suicides and program development cannot be determined, because an examination of causality was beyond the scope and mandate of this study.
Other considerations
Despite these limitations, the results are most likely valid because they are consistent with our clinical observations and the observations of other clinicians, as well as the study of community measures described above.1 One community member described the effect of the buprenorphine-naloxone program:
Five years ago, our community was in a mess. No one bought food. No one looked after their children; parents would bring them to grandparents and not come back for many days. Now [3 years after the introduction of the buprenorphine-naloxone program] bills are paid, people buy gas, play bingo, and go to fishing derbies. Children play, go to school, play hockey. We have many celebrations; everyone comes to Traditional Days.
In the Sioux Lookout region, short-term competitions for federal funding have pitted the needs of one community against those of another. Many communities have not been able to initiate programs owing to inadequate resources, and established programs have often suspended accepting new patients. Recently, federal funding competitions support up to 3 years of programming, but what is needed is a regional, and ultimately national, well resourced strategy and sustainable funding that flows to local communities, primary care, and First Nations health authorities for treatment planning, implementation, and evaluation.
Aftercare programming, including mental health and trauma recovery treatment, is particularly vulnerable to inadequate resourcing. Core program funding similar to that for other chronic diseases (eg, diabetes programs) is vital to the development and maintenance of community-based treatment programs.
Unfortunately, the Sioux Lookout success is an anomaly; the situation in other Canadian First Nations communities remains grim. In several provinces, medical regulators do not allow primary care physicians without a methadone exemption to prescribe buprenorphine-naloxone. As very few First Nations communities have methadone prescribers, these communities have no access to either buprenorphine-naloxone or methadone, 2 medications that are on the World Health Organization list of essential medications. This is very disturbing given that the opioid crisis is entering its 20th year, First Nations communities have been devastated by the crisis, and buprenorphine-naloxone is an inexpensive and highly effective intervention.
Now that the federal Non-Insured Health Benefits program has agreed to fund buprenorphine-naloxone, regardless of its provincial funding status, the next step is for medical regulators to remove barriers to primary care prescribing of buprenorphine-naloxone. This would allow other First Nations communities to establish their own programs, perhaps with long-distance training, support, and mentorship from Sioux Lookout community physicians and community leaders.
Conclusion
We have presented the successful outcomes of community-based opioid dependence treatment programs in 6 remote First Nations communities. Despite many obstacles, these community-driven initiatives have creatively begun to address crippling levels of addiction. The addiction rates seen in northwestern Ontario First Nations communities affect the fabric of those communities. Culturally embedded, community-based programs can provide an important starting point for long-term healing. Robust treatment programming and creative, culturally appropriate long-term aftercare are warranted. Medical regulators and provincial and federal governments need to empower such community-based treatment initiatives. Sustainable core resources are needed at the community and primary care levels.
Figure 2.
Retained participants and dropouts in the buprenorphine-naloxone program at 6-month intervals: Because participants entered the program at different times, not all retained participants had completed more than 6 months of treatment at the time of data collection. Most dropouts occurred in the first 6 months.
EDITOR’S KEY POINTS
Remote First Nations communities in northwestern Ontario have a high prevalence of opioid addiction and its consequences, such as crime, violence, and overdose. Communities in the Sioux Lookout region have established treatment programs using traditional healing in combination with buprenorphine-naloxone maintenance treatment. The authors were invited by 6 communities to evaluate their programs.
The 6-month treatment retention rate of 84% for these programs is higher than that reported for most methadone and buprenorphine-naloxone programs in the United States and Canada, despite these programs lacking the expertise and resources other such programs typically have. In 1 community, the high rates of negative urine drug screening results when screening was voluntary were also demonstrated when screening became mandatory after the study data collection period.
Despite many obstacles, these community-driven initiatives have creatively begun to address crippling levels of addiction. Although a causal relationship could not be determined, the 6 communities studied experienced a dramatic decline in suicides (P = .035) after the initiation of these programs. Culturally embedded, community-based programs can provide an important starting point for long-term healing.
POINTS DE REPÈRE DU RÉDACTEUR
La prévalence de la dépendance aux opiacés est élevée dans les collectivités isolées des Premières Nations du nord-ouest de l’Ontario, avec comme conséquences des crimes, de la violence et des cas d’overdose. Certaines collectivités de la région de Sioux Lookout ont instauré des programmes de traitement qui combinent médecine traditionnelle et traitement de soutien avec la buprénorphine-naloxone. Les auteurs de cet article ont été invités à évaluer les programmes de 6 de ces collectivités.
Avec ces programmes, le taux de rétention après 6 mois est supérieur à ce qui a été rapporté pour la plupart des programmes de méthadone et de buprénorphine-naloxone tant aux États-Unis qu’au Canada, et ce, malgré le fait qu’ils ne profitaient ni de l’expertise ni des ressources dont bénéficient généralement de tels programmes. Dans une de ces collectivités, les taux élevés de résultats négatifs lorsque la recherche de drogues dans l’urine était optionnelle ont également été observés quand ce dépistage est devenu obligatoire, après la période de collecte des données de l’étude.
En dépit de plusieurs obstacles, ces collectivités ont eu l’heureuse initiative de s’attaquer elles-mêmes aux graves problèmes de dépendance qui les accablent. Même s’il n’a pas été possible d’établir une relation de cause à effet, les 6 collectivités concernées ont connu une chute dramatique des suicides (p = .035) à la suite de l’instauration de ces programmes. Parce qu’ils tiennent compte de la culture amérindienne, ces programmes communautaires peuvent constituer un important point de départ pour des résultats durables.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Kanate D, Folk D, Cirone S, Gordon J, Kirlew M, Veale T, et al. Community-wide measures of wellness in a remote First Nations community experiencing opioid dependence. Evaluating outpatient buprenorphine-naloxone substitution therapy in the context of a First Nations healing program. Can Fam Physician. 2015;61:160–5. [PMC free article] [PubMed] [Google Scholar]
- 2.Kelly L, Dooley J, Cromarty H, Minty B, Morgan A, Madden S, et al. Narcotic-exposed neonates in a First Nations population in northwestern Ontario. Incidence and implications. Can Fam Physician. 2011;57:e441–7. Available from: www.cfp.ca/content/57/11/e441.full.pdf+html. Accessed 2017 Jan 4. [PMC free article] [PubMed] [Google Scholar]
- 3.News release. NAN chiefs call for immediate assistance as region braces for major health catastrophe [press release]. Thunder Bay, ON: Nishnawbe Aski Nation; 2012. Feb 16, Available from: www.nan.on.ca/article/region-braces-for-major-health-catastrophe--603.asp. Accessed 2015 Sep 18. [Google Scholar]
- 4.Caverson R. Prescription opioid-related issues in northern Ontario. Toronto, ON: Centre for Addiction and Mental Health; 2010. [Google Scholar]
- 5.Smyth BP, Barry J, Keenan E, Ducray K. Lapse and relapse following inpatient treatment of opiate dependence. Ir Med J. 2010;103(6):176–9. [PubMed] [Google Scholar]
- 6.Auriacombe M, Franques P, Tignol J. Deaths attributable to methadone vs buprenorphine in France. JAMA. 2001;285(1):45. doi: 10.1001/jama.285.1.45. [DOI] [PubMed] [Google Scholar]
- 7.Whelan PJ, Remski K. Buprenorphine vs methadone treatment: a review of evidence in both developed and developing worlds. J Neurosci Rural Pract. 2012;3(1):45–50. doi: 10.4103/0976-3147.91934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor R, et al. Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation. Health Technol Assess. 2007;11(9):1–171. doi: 10.3310/hta11090. [DOI] [PubMed] [Google Scholar]
- 9.Walker R, Cromarty H, Kelly L, St Pierre Hansen N. Achieving cultural safety in aboriginal health services: implementation of a cross-cultural safety model in a hospital setting. Divers Health Care. 2009;6(1):11–22. [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington DC: American Psychiatric Association; 2000. [Google Scholar]
- 11.Kiepek N, Groom B, Toppozini D, Kakekagumick K, Muileboom J, Kelly L. Evaluation of an inpatient medical withdrawal program in rural Ontario: a 1-year prospective study. Can J Rural Med. 2015;20(3):92–7. [PubMed] [Google Scholar]
- 12.Strike CJ, Gnam W, Urbanoski K, Fischer B, Marsh DC, Millson M. Factors predicting 2-year retention in methadone maintenance treatment for opioid dependence. Addict Behav. 2005;30(5):1025–8. doi: 10.1016/j.addbeh.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Fiellin DA, Moore BA, Sullivan LE, Becker WC, Pantalon MV, Chawarski MC, et al. Long-term treatment with buprenorphine/naloxone in primary care: results at 2–5 years. Am J Addict. 2008;17(2):116–20. doi: 10.1080/10550490701860971. [DOI] [PubMed] [Google Scholar]
- 14.Fudala PJ, Bridge TP, Herbert S, Williford WO, Chiang CN, Jones K, et al. Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. N Engl J Med. 2003;349(10):949–58. doi: 10.1056/NEJMoa022164. [DOI] [PubMed] [Google Scholar]
- 15.Neumann AM, Blondell RD, Azadfard M, Nathan G, Homish GG. Primary care patient characteristics associated with completion of 6-month buprenorphine treatment. Addict Behav. 2013;38(11):2724–8. doi: 10.1016/j.addbeh.2013.07.007. Epub 2013 Jul 25. [DOI] [PubMed] [Google Scholar]
- 16.Potter JS, Marino EN, Hillhouse MP, Nielsen S, Wiest K, Canamar CP, et al. Buprenorphine/naloxone and methadone maintenance treatment outcomes for opioid analgesic, heroin, and combined users: findings from Starting Treatment with Agonist Replacement Therapies (START) J Stud Alcohol Drugs. 2013;74(4):605–13. doi: 10.15288/jsad.2013.74.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Apelt SM, Scherbaum N, Golz J, Backmund M, Soyka M. Safety, effectiveness and tolerance of buprenorphine-naloxone in the treatment of opioid dependence: results from a nationwide non-interventional study in routine care. Pharmacopsychiatry. 2013;46(3):94–107. doi: 10.1055/s-0032-1330033. [DOI] [PubMed] [Google Scholar]
- 18.Stancliff S, Joseph H, Fong C, Furst T, Comer SD, Roux P. Opioid maintenance treatment as a harm reduction tool for opioid-dependent individuals in New York City: the need to expand access to buprenorphine/naloxone in marginalized populations. J Addict Dis. 2012;31(3):278–87. doi: 10.1080/10550887.2012.694603. Epub 2013 Jan 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCabe BE, Santisteban DA, Mena MP, Duchene DM, McLean C, Monroe M. Engagement, retention, and abstinence for three types of opioid users in Florida. Subst Use Misuse. 2013;48(8):623–34. doi: 10.3109/10826084.2013.800112. Epub 2013 Jun 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore BA, Fiellin DA, Barry DT, Sullivan LE, Chawarski MC, O’Connor PG, et al. Primary care office-based buprenorphine treatment: comparison of heroin and prescription opioid dependent patients. J Gen Intern Med. 2007;22(4):527–30. doi: 10.1007/s11606-007-0129-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacMillan HL, Jamieson E, Walsh CA, Wong MY, Faries EJ, McCue H, et al. First Nations women’s mental health: results from an Ontario survey. Arch Womens Ment Health. 2008;11(2):109–15. doi: 10.1007/s00737-008-0004-y. Epub 2008 May 21. [DOI] [PubMed] [Google Scholar]
- 22.Taplin C, Saddichha S, Li K, Krausz MR. Family history of alcohol and drug abuse, childhood trauma, and age of first drug injection. Subst Use Misuse. 2014;49(10):1311–6. doi: 10.3109/10826084.2014.901383. Epub 2014 Apr 7. [DOI] [PubMed] [Google Scholar]