Abstract
Objective
To determine the prevalence of overweight and obese status in children by age, sex, and visit type, using data from EMRALD® (Electronic Medical Record Administrative data Linked Database).
Design
Heights and weights were abstracted for children 0 to 19 years of age who had at least one well-child visit from January 2010 to December 2011. Using the most recent visit, the proportions and 95% CIs of patients defined as overweight and obese were compared by age group, sex, and visit type using the World Health Organization growth reference standards.
Setting
Ontario.
Participants
Children 0 to 19 years of age who were rostered to a primary care physician participating in EMRALD and had at least one well-child visit from January 2010 to December 2011.
Main outcome measures
Proportion and 95% CI of children with overweight and obese status by age group; proportion of children with overweight and obese status by sex (with male sex as the referent) within each age group; and proportion of children with overweight and obese status at the most recent well-child visit type compared with other visit types by age group.
Results
There were 28 083 well-child visits during this period. For children who attended well-child visits, 84.7% of visits had both a height and weight documented. Obesity rates were significantly higher in 1- to 4-year-olds compared with children younger than 1 (6.1% vs 2.3%; P < .001), and in 10- to 14-year-olds compared with 5- to 9-year-olds (12.0% vs 9.0%; P < .05). Both 1- to 4-year-old boys (7.2% vs 4.9%; P < .01) and 10- to 14-year-old boys (14.5% vs 9.6%; P < .05) had higher obesity rates compared with girls. Rates of overweight and obese status were lower using data from well-child visits compared with other visits.
Conclusion
Electronic medical records might be useful to conduct population-based surveillance of overweight or obese status in children. Methodologic standards, however, should be developed.
Résumé
Objectif
Déterminer la prévalence de surpoids et d’obésité chez les enfants en fonction de l’âge, du sexe et du type de visite, et ce, à l’aide des données de la base de données EMRALD (Electronic Medical Record Administrative data Linked Database).
Type d’étude
On a recueilli les données concernant la taille et le poids d’enfants âgés de 0 à 19 ans qui avaient effectué au moins une visite de contrôle pour enfants normaux entre janvier 2010 et décembre 2011. On a comparé, en fonction des différents groupes d’âge, du sexe et du type de visite, la proportion (et les intervalles de confiance à 95 %) des patients qui, lors de la visite la plus récente, présentaient un surpoids ou une obésité selon les normes de l’OMS pour la croissance.
Contexte
L’Ontario.
Participants
Des enfants âgés de 0 à 19 ans suivis par un médecin de première ligne, qui participaient à EMRALD et qui avaient effectué au moins une visite de contrôle pour enfants normaux entre janvier 2010 et décembre 2011.
Principaux paramètres à l’étude
La proportion et les IC à 95 % des enfants présentant un surpoids ou une obésité selon les groupes d’âge; la proportion des enfants présentant un surpoids ou une obésité selon le sexe (le sexe mâle étant utilisé comme référence) dans chacun des groupes d’âge; et la proportion de ceux qui présentaient un surpoids ou une obésité lors de leur plus récente visite de contrôle pour enfants normaux par rapport à d’autres types de visites et selon les groupes d’âge.
Résultats
Il y a eu 28 083 visites de contrôle pour enfants normaux durant la période de l’étude. Le poids et la taille des enfants étaient documentés dans 84,7 % de ces visites. Les taux d’obésité étaient significativement plus élevés chez les enfants de 1 à 4 ans par rapport à ceux qui avaient moins d’un an (6,1 % vs 2,3 %, P < .001) et chez ceux de 10 à 14 ans par rapport à ceux de 5 à 9 ans (12,0 % vs 9,0 %, P < .05). Les garçons de 1 à 4 ans avaient des taux d’obésité plus élevés que les filles (7,2 % vs 4,9 %, P < .01) et on observait la même chose chez ceux de 10 à 14 ans (14,5 % vs 9,6 %, P < .05). Les taux d’obésité ou de surpoids étaient plus bas lorsqu’on utilisait les données des visites de contrôle pour enfants normaux plutôt que d’autres types de visites.
Conclusion
Les dossiers médicaux électroniques pourraient servir à la détection des cas de surpoids et d’obésité chez les enfants. Il serait toutefois opportun d’élaborer des normes méthodologiques pour ce faire.
Obesity is one of the leading contemporary public health problems facing children in Canada and the developed world. According to the World Health Organization (WHO), for children 5 to 19 years of age, the cutoff for overweight body mass index (BMI) is the 85th percentile, and the cutoff for obese BMI is the 97th percentile. For children 0 to 5 years of age, the cutoff for being at risk of overweight BMI is the 85th percentile, overweight BMI is the 97th percentile, and obesity is above the 99.9th percentile.1,2 Children who are obese are at increased risk of becoming obese adults, with increased risk of developing atherosclerotic heart disease, diabetes, and certain cancers.3–5 Complications of childhood obesity, such as hypertension, obstructive sleep apnea, and reduced quality of life, carry substantial morbidity and are increasing in prevalence.6–13 There are minimal prevalence data on overweight or obese status of children in Canada. Results from the 2009 to 2011 Canadian Health Measures Survey showed a prevalence rate of 20% for being overweight and of 12% for being obese, based on direct measurements of 2217 children 5 to 17 years of age, using the WHO growth curves. No recent data are reported for children younger than 5 years of age14,15 and there are no data for children younger than 3 years of age. Data from 8661 children 2 to 17 years of age from the 2004 Canadian Community Health Survey demonstrated a prevalence of 22% for being overweight or obese, and a prevalence of 13% for obesity.16 Abstraction of height and weight data from electronic medical records (EMRs) has been used to estimate the prevalence of childhood obesity in a small number of studies from jurisdictions such as Massachusetts, United States17; Leeds, United Kingdom18; and Västerbotten, Sweden.19 These studies report obesity prevalence in limited age groups and use different obesity cutoffs. However, there is great potential for routinely collected clinical data in EMRs to be used for surveillance of weight status in children, and to assess population-based interventions for obesity. The uptake of EMRs is increasing among child-health providers in Canada20 and elsewhere,21 although there has been very limited primary care research using EMRs.22
In Ontario, it is recommended that children have 9 well-child visits with their primary care physicians in the first 24 months of life and then yearly. The measurement of height and weight at well-child visits has recently been recommended by leading authorities, including the Canadian Task Force on Preventive Health Care,20,23–26 but it remains unknown how consistently this is done. The primary objective of this study is to determine the prevalence of childhood obesity by age and sex using data from the Electronic Medical Record Administrative data Linked Database (EMRALD®) in Ontario.27 The secondary objectives are to determine the frequency of height and weight documentation in the EMR during well-child visits by age group and sex, and to compare overweight and obese status prevalence rates using heights and weights measured in the well-child visit compared with other visit types. Examination by both age and visit type are important, as they might affect the choice of data used for surveillance and to evaluate interventions in primary care.
METHODS
This was a descriptive observational study of children enrolled in EMRALD. At the time of this study, EMRALD housed data from 167 family physicians who used PS Suite EMR and who volunteered to contribute their primary care EMR data. This database is housed at the Institute for Clinical Evaluative Sciences and is used in the evaluation and analysis of the health care system. All data underwent quality and comprehensiveness checks before use.28 All family physicians participating in EMRALD practise under one of the primary care reform models of care in Ontario. The health card numbers of children in EMRALD are replaced with unique identification numbers and anonymously linked to the population-based health administrative databases at the Institute for Clinical Evaluative Sciences. For this study, we abstracted weight and height as recorded in the EMR for children 0 to 19 years of age who were rostered to a primary care physician in EMRALD and had at least one well-child visit from January 2010 to December 2011. Using Ontario Health Insurance Plan (OHIP) data, which contain all fee-for-service and shadow billings for nearly all Ontario physicians, we compared baseline characteristics of our study population to all children in Ontario, using the Registered Persons Database, which contains demographic data for all Ontario residents eligible for OHIP.29
We recorded the frequency of documentation of height and weight during well-child visits. We identified well-child visits using OHIP billing fee codes recorded in the EMR and submitted to OHIP (codes available upon request).30 We then selected the most recent well-child visit with both height and weight documented to calculate obesity prevalence rates. We applied a previously published31 validated set of rules to eliminate biologically implausible values incurred in measurement or data entry: we excluded single height measurements less than 30.5 cm and below the 1st percentile of height for age minus 30.5 cm, and measurements greater than 221 cm or above the 99th percentile of height for age plus 61 cm using the WHO growth curves for height percentiles.
Baseline characteristics of the cohort of children rostered in EMRALD, which was compared with other Ontario children, were reported by age group, sex, median neighbourhood income using postal code, and residence in a rural, suburban, or urban setting. Neighbourhood income quintiles and rurality were defined through linkage of postal codes to census data.32 The number of visits for each child with both documented height and weight was reported by age group. Using the most recent well-child visit with both height and weight documented, the mean (SD) height, weight, and BMI were reported by age group and sex. We reported the proportion and 95% CIs of children defined as overweight and obese using the WHO growth reference standards for BMI z score (zBMI).1,2 The WHO recommends that children whose BMIs are approximately at the 97th percentile (more than 2 SDs above the mean; zBMI > 2) should be considered obese, and children whose BMIs are approximately at the 85th percentile (between 1 and 2 SDs above the mean; zBMI > 1 and ≤ 2) should be considered overweight. The terminology used to characterize being overweight and obese changes with age; children younger than 5 are considered at risk of being overweight if their BMIs are approximately at the 85th percentile (> 1 SD above the mean), overweight if their BMIs are approximately at the 97th percentile (> 2 SDs above the mean), and obese if their BMIs are approximately at the 99th percentile (> 3 SDs above the mean). This change in terminology for children by age can be challenging to apply when performing population- based research. To be consistent regarding definitions of overweight status or obese status we (and others in the field16,33) have defined overweight status as zBMI greater than 1 to less than or equal to 2 and obese status as zBMI greater than 2, using WHO growth curves for all age groups.
Using 2 × 2 contingency tables,
 2 test statistics were used to compare the prevalence of both overweight and obese status in children by age group. Each age group was compared with the adjacent older age category (< 1 year to 1 to 4 years, 1 to 4 years to 5 to 9 years, 5 to 9 years to 10 to 14 years, and 10 to 14 years to 15 to 19 years). We used
2 test statistics were used to compare the prevalence of both overweight and obese status in children by age group. Each age group was compared with the adjacent older age category (< 1 year to 1 to 4 years, 1 to 4 years to 5 to 9 years, 5 to 9 years to 10 to 14 years, and 10 to 14 years to 15 to 19 years). We used
 2 test statistics to compare the prevalence of both overweight and obese status in children by sex (with male sex as the referent) within each age group. We also compared prevalence rates of overweight and obese status using heights and weights measured at the most recent well-child visit compared with other primary care visit types by age group using
2 test statistics to compare the prevalence of both overweight and obese status in children by sex (with male sex as the referent) within each age group. We also compared prevalence rates of overweight and obese status using heights and weights measured at the most recent well-child visit compared with other primary care visit types by age group using
 2 tests. We used SAS, version 9.3, for analysis. This study was approved by the research ethics boards at Sunnybrook Health Sciences Centre and the SickKids Research Institute.
2 tests. We used SAS, version 9.3, for analysis. This study was approved by the research ethics boards at Sunnybrook Health Sciences Centre and the SickKids Research Institute.
RESULTS
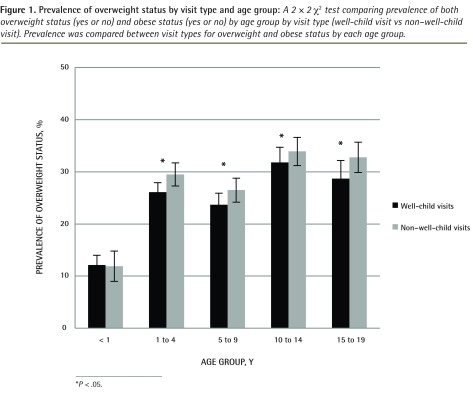
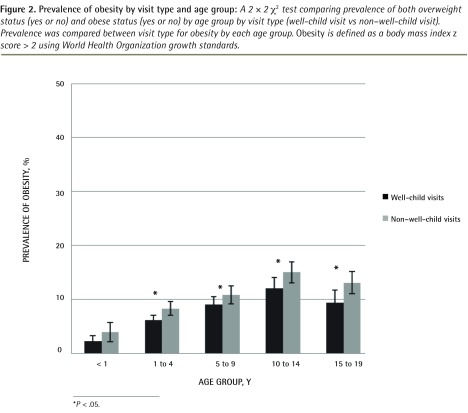
The baseline characteristics of the cohort of children rostered in EMRALD are reported in Table 1. Compared with all children in Ontario, a higher proportion of children rostered in EMRALD live in rural or suburban areas compared with urban areas. Among the 33 343 rostered children, 10 372 (31.1%) children had at least one well-child visit during the study period, with a total of 28 083 well-child visits. The proportion of rostered children who had well-child visits varied by age (Table 2), with much lower rates of well-child visits in the older age groups. For rostered children who attended well-child visits, 84.7% of visits had both height and weight documented, with similar results by age group (Table 2). In those rostered children who had both height and weight documented, the rates of being overweight and obese (Table 3) ranged from 12.1% to 31.8%, and 2.3% to 12.0%, respectively. Rates of being overweight or obese were higher in 1- to 4-year-olds compared with children younger than 1 (P < .001), and in 10- to 14-year-olds compared with 5- to 9-year-olds (P < .05). Obesity rates were higher in 5- to 9-year-olds compared with 1-to 4-year-olds (P < .001). Boys, compared with girls, were statistically significantly more likely to be overweight or obese in the 1- to 4-year-old (P < .01) and 10- to 14-year-old (P < .05) age groups and were more likely to be overweight among those younger than 1 year of age (P < .05). In all age groups, except for children younger than 1, overweight or obese status was more prevalent using height and weight measures from non–well-child visits compared with well-child visits (Figures 1 and 2).
Table 1.
Baseline characteristics of children rostered in EMRALD® and all Ontario children
| CHARACTERISTIC | ALL ROSTERED CHILDREN IN EMRALD* (N = 31 637), N (%) | ALL ONTARIO CHILDREN (N = 3 122 918), N (%) |
|---|---|---|
| Sex† | ||
| • Male | 16 052 (50.7) | 1 601 593 (51.3) |
| • Female | 15 582 (49.3) | 1 521 325 (48.7) |
| Age, y | ||
| • 0–4 | 8218 (26.0) | 727 088 (23.3) |
| • 5–9 | 7928 (25.1) | 747 225 (23.9) |
| • 10–14 | 7772 (24.6) | 779 141 (25.0) |
| • 15–19 | 7719 (24.4) | 869 464 (27.8) |
| Neighborhood income‡ | ||
| • 1—lowest quintile | 4838 (15.3) | 595 712 (19.1) |
| • 2 | 5597 (17.7) | 576 662 (18.5) |
| • 3 | 6480 (20.5) | 625 302 (20.0) |
| • 4 | 7231 (22.9) | 678 401 (21.7) |
| • 5—highest quintile | 7416 (23.4) | 634 259 (20.3) |
| • Unknown or missing | 75 (0.2) | 12 582 (0.4) |
| Rurality‡ | ||
| • Rural | 6058 (19.1) | 149 605 (4.8) |
| • Suburban | 9859 (31.2) | 467 531 (15.0) |
| • Urban | 15 720 (49.7) | 2 505 782 (80.2) |
EMRALD—Electronic Medical Record Administrative data Linked Database.
Administrative data on patient demographic characteristics were available for 31 637 of the 33 343 (94.9%) children in EMRALD.
Sex was not recorded for 3 children.
Neighborhood income quintile and rurality were calculated by linking postal codes from the Registered Persons Database to 2006 Statistics Canada census data.
Table 2.
Rostered patients in EMRALD® with well-child visits and documented height and weight, by age group
| AGE, Y | ALL ROSTERED CHILDREN IN EMRALD | ROSTERED CHILDREN IN EMRALD WITH A WELL-CHILD VISIT, N (%) | WELL-CHILD VISITS WITH HEIGHT AND WEIGHT DOCUMENTED, N (%) |
|---|---|---|---|
| < 1 | 1545 | 1292 (83.6) | 3389 (78.6) |
| 1–4 | 6898 | 4700 (68.1) | 15006 (84.9) |
| 5–9 | 8103 | 2131 (26.3) | 2783 (89.4) |
| 10–14 | 7784 | 1190 (15.3) | 1437 (88.1) |
| 15–19 | 9013 | 1059 (11.7) | 1159 (85.9) |
| Total | 33 343 | 10 372 (31.1) | 23 774 (84.7) |
EMRALD—Electronic Medical Record Administrative data Linked Database.
Table 3.
Prevalence of overweight and obese status in children by age and sex
| AGE, Y | N | WEIGHT, KG, MEAN (SD) | HEIGHT, CM, MEAN (SD) | BMI, KG/M2, MEAN (SD) | OVERWEIGHT*, % (95% CI) | OBESE*, % (95% CI) |
|---|---|---|---|---|---|---|
| Overall† | ||||||
| • <1 | 1195 | 7.0 (2.0) | 65.3 (7.3) | 16.0 (2.0) | 12.1 (10.2–13.9) | 2.3 (1.4–3.2) |
| • 1–4 | 3426 | 13.2 (3.1) | 89.3 (10.2) | 16.3 (1.6) | 26.1‡ (24.6–27.6) | 6.1‡ (5.2–6.9) |
| • 5–9 | 1445 | 25.2 (7.1) | 122.8 (10.3) | 16.4 (2.5) | 23.7 (21.5–26.0) | 9.0‡ (7.5–10.5) |
| • 10–14 | 977 | 48.5 (14.5) | 154.4 (11.2) | 20.0 (4.3) | 31.8‡ (28.9–34.8) | 12.0§ (9.9–14.1) |
| • 15–19 | 662 | 65.8 (15.1) | 169.1 (8.8) | 22.9 (4.6) | 28.7 (25.2–32.2) | 9.4 (7.1–11.7) |
| Male‖ | ||||||
| • <1 | 614 | 7.4 (2.0) | 66.4 (7.3) | 16.3 (2.0) | 14.2 (11.3–17.0) | 2.9 (1.5–4.3) |
| • 1–4 | 1738 | 6.6 (1.9) | 90.1 (10.2) | 16.5 (1.6) | 27.7 (25.6–29.9) | 7.2 (5.9–8.4) |
| • 5–9 | 703 | 25.3 (6.8) | 123.4 (10.2) | 16.4 (2.3) | 25.6 (22.3–28.9) | 10.1 (7.8–12.4) |
| • 10–14 | 468 | 48.4 (14.6) | 154.7 (12.1) | 19.9 (4.1) | 35.0 (30.6–39.5) | 14.5 (11.2–17.8) |
| • 15–19 | 270 | 70.4 (14.5) | 175.8 (7.2) | 22.7 (4.1) | 30.7 (25.1–36.4) | 8.5 (5.0–12.0) |
| Female | ||||||
| • <1 | 581 | 6.6 (1.9) | 64.2 (7.1) | 15.7 (2.0) | 9.8§ (7.3–12.3) | 1.7 (0.6–2.9) |
| • 1–4 | 1681 | 12.8 (3.0) | 88.6 (10.3) | 16.1 (1.6) | 24.4§ (22.4–26.5) | 4.9¶ (3.8–5.9) |
| • 5–9 | 742 | 25.0 (7.4) | 122.3 (10.3) | 16.4 (2.6) | 22.0 (18.9–25.0) | 8.0 (5.9–10.0) |
| • 10–14 | 509 | 48.6 (14.4) | 154.1 (10.3) | 20.2 (4.5) | 28.9§ (24.8–32.9) | 9.6§ (7.0–12.3) |
| • 15–19 | 392 | 62.6 (14.8) | 164.5 (6.6) | 20.2 (4.5) | 27.3 (22.8–31.8) | 9.9 (6.9–13.0) |
BMI—body mass index, zBMI—body mass index z score.
Being overweight is defined as zBMI > 1 to ≤ 2; being obese is defined as zBMI > 2 using World Health Organization growth standards.
A 2 × 2
 2 test comparing prevalence of both being overweight (yes or no) and being obese (yes or no) by age group. Each age group was compared to the adjacent older age category (< 1 y to 1–4 y, 1–4 y to 5–9 y, 5–9 y to 10–14 y, and 10–14 y to 15–19 y).
2 test comparing prevalence of both being overweight (yes or no) and being obese (yes or no) by age group. Each age group was compared to the adjacent older age category (< 1 y to 1–4 y, 1–4 y to 5–9 y, 5–9 y to 10–14 y, and 10–14 y to 15–19 y).
P < .001.
P < .05.
A 2 × 2
 2 test comparing prevalence of both being overweight (yes or no) and being obese (yes or no) versus sex (female or male) within each age group. Male is the referent.
2 test comparing prevalence of both being overweight (yes or no) and being obese (yes or no) versus sex (female or male) within each age group. Male is the referent.
P < .01.
Figure 1.
Prevalence of overweight status by visit type and age group:
A 2 × 2
 2
test comparing prevalence of both overweight status (yes or no) and obese status (yes or no) by age group by visit type (well-child visit vs non–well-child visit). Prevalence was compared between visit types for overweight and obese status by each age group.
2
test comparing prevalence of both overweight status (yes or no) and obese status (yes or no) by age group by visit type (well-child visit vs non–well-child visit). Prevalence was compared between visit types for overweight and obese status by each age group.
*P < .05.
Figure 2.
Prevalence of obesity by visit type and age group:
A 2 × 2
 2
test comparing prevalence of both overweight status (yes or no) and obese status (yes or no) by age group by visit type (well-child visit vs non–well-child visit). Prevalence was compared between visit type for obesity by each age group. Obesity is defined as a body mass index z score > 2 using World Health Organization growth standards.
2
test comparing prevalence of both overweight status (yes or no) and obese status (yes or no) by age group by visit type (well-child visit vs non–well-child visit). Prevalence was compared between visit type for obesity by each age group. Obesity is defined as a body mass index z score > 2 using World Health Organization growth standards.
*P < .05.
DISCUSSION
We report the frequency of documented height and weight in a large sample of children using EMR data from a sample of primary care (family physician) practices in Ontario. Growth monitoring by primary health care practitioners at all well-child visits through standardized measurement of height and weight is recommended by the leading child health professional organizations nationally and internationally,23–25 and the Canadian Task Force on Preventive Health Care recently recommended growth monitoring at all appropriate primary care visits (including well-child visits and at episodic care and acute illness visits) using the 2014 WHO Growth Charts for Canada.26 A recent study reported frequency of height or weight documentation in children using EMRs in Ontario and found similar results, although different age categories were used.34 In a US study of adults using EMRs, 63% had ever had a height measurement documented, and 91% had a documented weight in the preceding 18 months.35 There are limited recent national data on prevalence of overweight and obese status in children in Canada. Using data from 2123 children measured by the Canadian Health Measures Study from 2009 to 2011, the prevalences of overweight status in 5- to 11-year-olds and in 12- to 17-year-olds were 20% and 12%, respectively, with obese status rates substantially lower in girls (8%) compared with boys (15%).14 Although we cannot directly compare the prevalence rates of overweight and obese status in children owing to contrasting age groups, our prevalence rates of overweight status in children aged 5 to 9 years, 10 to 14 years, and 15 to 19 years are higher—23.7%, 31.8%, and 28.7%, respectively—using the same WHO cutoffs. We also documented lower rates in girls compared with boys in similar age groups. This finding is consistent with other studies in Canada and the United States. It is unknown if these differences by sex might be related to differences in pubertal changes, genetics, or other differences such as dietary patterns. A recent study in Ontario using data from EMRs demonstrated similar rates of obese status in children 5 years of age and older compared with our study, with increased rates in boys compared with girls, but reduced rates of overweight status. For example, in children 10 to 19 years of age, rates of being overweight or obese were 18% and 11%, respectively, compared with 29% and 9% in 15- to 19-year-olds.34
Differences in rates might be related to differences in age groups, differences in definitions across age groups, and different study periods. Biro et al reported rates from measurements from 2004 to 2013.34 Although there is an emphasis on obesity interventions and prevention in the early years in Ontario and elsewhere,36 there are very limited data in Canada (and elsewhere) on obesity rates in young children. In the Canadian Community Health Survey in 2004, the prevalence of obesity using WHO cutoffs in 1341 children 2 to 5 years of age was 11%.16 Similar prevalence rates are reported in preschool children recruited through public health immunization clinics in both Alberta and Newfoundland and Labrador.37,38 Biro et al reported obesity rates in children 0 to 5 years of age of 6% (using weight for length),34 similar to our findings of 6.1% in 1- to 4-year-olds (using BMI). Many methodologic issues, such as sampling strategies, response rate, age group, measurement accuracy, and choice of obesity cutoffs39–41 should be considered when comparing prevalences of overweight and obese status in children from different data sources.
Strengths and limitations
Strengths of our study include the large sample size, the inclusion of young children, and the use of a validated algorithm to eliminate biologically implausible values.31 The EMR might be an important and efficient data source for surveillance for very young children, who have measurements of height and weight taken during their primary health care visits.30 Compared with younger children (ie, those aged < 1 year and 1 to 4 years), a much lower proportion of older children (ie, those aged 5 to 9 years, 10 to 14 years, and 15 to 19 years) rostered in EMRALD attended well-child visits. The findings from this study might therefore reflect rates of overweight and obese status in older children that are not representative of the general population in this age group. We attempted to reduce this potential ascertainment bias by including height and weight measurements that were obtained only from well-child visits and not from all possible visits. For all age groups, except for children younger than 1 year of age, we identified lower prevalence rates of overweight and obese status using data from well-child visits compared with other visit types, as shown for the 18-month visit in a recent study.34 Increased weight in children might lead to an increase in health problems, leading parents to seek additional medical visits. Health care use is increased in children with obesity.42,43 These methodologic issues are important to consider, are not documented in previous studies using EMR data,18,19,44 and require further study.
An important limitation of this analysis relates to the quality of the height and weight measurements themselves. The primary care practices that contribute their data to EMRALD do not have standardized equipment, protocols, or training for measurement of height or length and weight in children. Although we eliminated biologically implausible values according to a previously published study,31 other errors cannot be entirely eliminated.45 However, ALSPAC (Avon Longitudinal Study of Parents and Children) demonstrated that routinely collected height and weight data in children 4 to 43 months of age were accurate compared with standardized research-collected height and weight data, with slight overestimates for height among tall children, and underestimates of height among short children.46 Yin et al demonstrated good reliability between routine and research-collected lengths in young children.47 This lends indirect support to the accuracy and reliability of routinely collected data.
We characterized weight status in our cohort using BMI. Although weight for length for age is the recommended measure to determine weight status in children younger than 2 years of age, other studies have shown strong correlation between weight for length and BMI for age in children (r = 0.83).48 Although we recognize there are slight differences between supine length and standing height measurement, in this study it is unknown which method was used by each physician. Previous research has shown that both measures indirectly reflect body adiposity to a similar extent.17 Although patients in EMRALD have an increased rate of residence in a rural and suburban area, Shields and Tjepkema previously showed no association between rural-urban residence and rates of overweight or obese status in children in Canada.49 Children in this study all received primary care from family physicians. It is unknown how practitioner type (eg, pediatrician, family physician, nurse practitioner) might affect the frequency of measurement of height and weight, or prevalence of being overweight or obese.
Conclusion
The prevalence of overweight and obese status in children might be higher in Canada than previously documented. The development of feasible and efficient surveillance systems to measure obesity in children and to assess population-based obesity interventions is recommended.36 Our study demonstrates that almost 85% of well-child visits in EMRALD had a height and weight documented at the most recent well-child visit. This finding was consistent across all age groups, demonstrating that this approach to obesity surveillance in children might be feasible. Studies to determine validity and reliability of EMR data for obesity surveillance should be developed. However, in addition to height and weight data from EMRs, other data such as health behaviour and weight-related behaviour would strengthen the opportunity to use EMR data to inform interventions for children with excess weight. Unfortunately, health behaviour data are not routinely captured in EMRs. Of importance, this study suggests that the EMR, if valid and reliable, scaled up to include a larger sample of primary care practices, could be one potential data source to conduct population-based surveillance of overweight and obese status in children and to evaluate interventions in Ontario and Canada, particularly for young children who attend primary care frequently.
Acknowledgments
This research was made possible by support in part from the SickKids Foundation and the Institute for Clinical Evaluative Sciences, which is a nonprofit organization funded by an annual grant from the Ontario Ministry of Health and Long-Term Care, with provision of population-based data. The opinions, results, and conclusions reported in this paper are those of the authors and are independent from all funding sources. No endorsement by the Institute for Clinical Evaluative Sciences or the Ontario Ministry of Health and Long-Term Care is intended or should be inferred. The funding organizations were not involved in any of the following: study design; collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the manuscript for publication. Dr Guttmann receives salary support through an Applied Research Chair in Child Health Services Research from the Canadian Institutes of Health Research. Dr Tu holds a Research Scholar Award from the Department of Family Community Medicine at the University of Toronto.
EDITOR’S KEY POINTS
Almost 85% of well-child visits in EMRALD® (Electronic Medical Record Administrative data Linked Database) had a height and weight documented consistently across most age groups, demonstrating that this approach to obesity surveillance in children might be feasible.
However, in addition to height and weight data from electronic medical records (EMRs), other data, such as weight-related behaviour, would strengthen the opportunity to use EMR data to inform interventions for children with excess weight.
The EMR, if valid and reliable, scaled up to include a larger sample of primary care practices, could be one potential data source to conduct population-based surveillance of overweight and obese status in children and to evaluate interventions in Ontario and Canada, particularly for young children who attend primary care frequently.
POINTS DE REPÈRE DU RÉDACTEUR
Près de 85 % des visites de contrôle d’enfants normaux consignées dans la base de données EMRALD (Electronic Medical Record Administrative data Linked Database) mentionnent de façon régulière la taille et le poids des enfants de tous les groupes d’âge, ce qui indique qu’on pourrait se servir de ces données pour détecter les cas d’obésité chez les enfants.
Toutefois, en plus des données sur la taille et le poids des enfants inscrites dans les dossiers médicaux électroniques (DME), d’autres données, par exemple sur le comportement alimentaire, accroîtraient les possibilités d’utiliser les données des DME pour mieux intervenir auprès des enfants qui présentent un excès de poids.
Un DME valide et fiable qui inclurait les résultats d’un échantillon plus large d’établissements de soins de première ligne pourrait être une source d’information pour effectuer une surveillance fondée sur la population des cas de surpoids et d’obésité chez les enfants, et pour évaluer les interventions utilisées en Ontario et ailleurs au Canada, notamment celles qui visent les jeunes enfants qui visitent fréquemment les cliniques de soins primaires.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors are responsible for the reported research. All have made contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published.
Competing interests
None declared
References
- 1.De Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull. 2004;25(1 Suppl):S15–26. doi: 10.1177/15648265040251S103. [DOI] [PubMed] [Google Scholar]
- 2.De Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–7. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freedman DS, Khan LK, Mei Z, Dietz WH, Srinivasan SR, Berenson GS. Relation of childhood height to obesity among adults: the Bogalusa Heart Study. Pediatrics. 2002;109(2):E23. doi: 10.1542/peds.109.2.e23. [DOI] [PubMed] [Google Scholar]
- 4.Duval S, Vazquez G, Baker WL, Jacobs DR, Jr, CODA study group The Collaborative Study of Obesity and Diabetes in Adults (CODA) project: meta-analysis design and description of participating studies. Obes Rev. 2007;8(3):263–76. doi: 10.1111/j.1467-789X.2006.00263.x. [DOI] [PubMed] [Google Scholar]
- 5.Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357(23):2329–37. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study. Int J Obes Relat Metab Disord. 2004;28(1):10–6. doi: 10.1038/sj.ijo.0802544. [DOI] [PubMed] [Google Scholar]
- 7.Sabin MA, Ford AL, Holly JM, Hunt LP, Crowne EC, Shield JP. Characterisation of morbidity in a UK, hospital based, obesity clinic. Arch Dis Child. 2006;91(2):126–30. doi: 10.1136/adc.2005.083485. Epub 2005 Oct 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sorof J, Daniels S. Obesity hypertension in children: a problem of epidemic proportions. Hypertension. 2002;40(4):441–7. doi: 10.1161/01.hyp.0000032940.33466.12. [DOI] [PubMed] [Google Scholar]
- 9.Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA. 2005;293(4):455–62. doi: 10.1001/jama.293.4.455. [DOI] [PubMed] [Google Scholar]
- 10.Taylor RW, Grant AM, Goulding A, Williams SM. Early adiposity rebound: review of papers linking this to subsequent obesity in children and adults. Curr Opin Clin Nutr Metab Care. 2005;8(6):607–12. doi: 10.1097/01.mco.0000168391.60884.93. [DOI] [PubMed] [Google Scholar]
- 11.Verhulst SL, Schrauwen N, Haentjens D, Rooman RP, Van Gaal L, De Backer WA, et al. Sleep-disordered breathing and the metabolic syndrome in overweight and obese children and adolescents. J Pediatr. 2007;150(6):608–12. doi: 10.1016/j.jpeds.2007.01.051. [DOI] [PubMed] [Google Scholar]
- 12.Verhulst SL, Schrauwen N, Haentjens D, Suys B, Rooman RP, Van Gaal L, et al. Sleep-disordered breathing in overweight and obese children and adolescents: prevalence, characteristics and the role of fat distribution. Arch Dis Child. 2007;92(3):205–8. doi: 10.1136/adc.2006.101089. Epub 2006 Oct 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams J, Wake M, Hesketh K, Maher E, Waters E. Health-related quality of life of overweight and obese children. JAMA. 2005;293(1):70–6. doi: 10.1001/jama.293.1.70. [DOI] [PubMed] [Google Scholar]
- 14.Roberts KC, Shields M, de Groh M, Aziz A, Gilbert JA. Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. Health Rep. 2012;23(3):37–41. [PubMed] [Google Scholar]
- 15.Shields M. Overweight and obesity among children and youth. Health Rep. 2006;17(3):27–42. [PubMed] [Google Scholar]
- 16.Shields M, Tremblay MS. Canadian childhood obesity estimates based on WHO, IOTF and CDC cut-points. Int J Pediatr Obes. 2010;5(3):265–73. doi: 10.3109/17477160903268282. [DOI] [PubMed] [Google Scholar]
- 17.Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012;129(5):823–31. doi: 10.1542/peds.2011-1833. Epub 2012 Apr 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edwards KL, Clarke GP, Ransley JK, Cade JE. Serial cross-sectional analysis of prevalence of overweight and obese children between 1998 and 2003 in Leeds, UK, using routinely measured data. Public Health Nutr. 2011;14(1):56–61. doi: 10.1017/S1368980010001849. Epub 2010 Jun 25. [DOI] [PubMed] [Google Scholar]
- 19.Bergström E, Blomquist HK. Is the prevalence of overweight and obesity declining among 4-year-old Swedish children? Acta Paediatr. 2009;98(12):1956–8. doi: 10.1111/j.1651-2227.2009.01490.x. Epub 2009 Sep 7. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization . Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Geneva, Switz: World Health Organization; 2000. [PubMed] [Google Scholar]
- 21.Schoen C, Osborn R, Squires D, Doty M, Rasmussen P, Pierson R, et al. A survey of primary care doctors in ten countries shows progress in use of health information technology, less in other areas. Health Aff (Millwood) 2012;31(12):2805–16. doi: 10.1377/hlthaff.2012.0884. Epub 2012 Nov 15. [DOI] [PubMed] [Google Scholar]
- 22.Terry AL, Stewart M, Fortin M, Wong ST, Kennedy M, Burge F, et al. How does Canada stack up? A bibliometric analysis of the primary healthcare electronic medical record literature. Inform Prim Care. 2012;20(4):233–40. doi: 10.14236/jhi.v20i4.2. [DOI] [PubMed] [Google Scholar]
- 23.Dietitians of Canada. Canadian Paediatric Society. College of Family Physicians of Canada. Community Health Nurses of Canada. Secker D. Promoting optimal monitoring of child growth in Canada: using the new WHO growth charts. Can J Diet Pract Res. 2010;71(1):e1–3. doi: 10.3148/71.1.2010.54. [DOI] [PubMed] [Google Scholar]
- 24.Koplan JP, Liverman CT, Kraak VI, Committee on Prevention of Obesity in Children and Youth Preventing childhood obesity: health in the balance: executive summary. J Am Diet Assoc. 2005;105(1):131–8. doi: 10.1016/j.jada.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 25.US Preventive Services Task Force. Barton M. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125(2):361–7. doi: 10.1542/peds.2009-2037. Epub 2010 Jan 18. [DOI] [PubMed] [Google Scholar]
- 26.Canadian Task Force on Preventive Health Care. Recommendations for growth monitoring, and prevention and management of overweight and obesity in children and youth in primary care. CMAJ. 2015;187(6):411–21. doi: 10.1503/cmaj.141285. Epub 2015 Mar 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tu K, Mitiku T, Ivers NM, Guo H, Lu H, Jaakkimainen L, et al. Evaluation of Electronic Medical Record Administrative data Linked Database (EMRALD) Am J Manag Care. 2014;20(1):e15–21. [PubMed] [Google Scholar]
- 28.Tu K, Widdifield J, Young J, Oud W, Ivers NM, Butt DA, et al. Are family physicians comprehensively using electronic medical records such that the data can be used for secondary purposes? A Canadian perspective. BMC Med Inform Decis Mak. 2015;15:67. doi: 10.1186/s12911-015-0195-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iron K, Zagorski BM, Sykora K, Manuel DG. Living and dying in Ontario: an opportunity for improved health information. Toronto, ON: Institute for Clinical Evaluative Sciences; 2008. [Google Scholar]
- 30.Guttmann A, Manuel D, Dick PT, To T, Lam K, Stukel TA. Volume matters: physician practice characteristics and immunization coverage among young children insured through a universal health plan. Pediatrics. 2006;117(3):595–602. doi: 10.1542/peds.2004-2784. [DOI] [PubMed] [Google Scholar]
- 31.Smith N, Coleman KJ, Lawrence JM, Quinn VP, Getahun D, Reynolds K, et al. Body weight and height data in electronic medical records of children. Int J Pediatr Obes. 2010;5(3):237–42. doi: 10.3109/17477160903268308. [DOI] [PubMed] [Google Scholar]
- 32.Wilkins R. PCCF+ version 5E user’s guide. Automated geographic coding based on the Statistics Canada postal code conversion files, including postal codes through March 2009. Ottawa, ON: Health Analysis Division, Statistics Canada; 2009. [Google Scholar]
- 33.Koebnick C, Coleman KJ, Black MH, Smith N, Der-Sarkissian JK, Jacobsen SJ, et al. Cohort profile: the KPSC Children’s Health Study, a population-based study of 920 000 children and adolescents in southern California. Int J Epidemiol. 2012;41(3):627–33. doi: 10.1093/ije/dyq252. Epub 2011 Jan 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Biro S, Barber D, Williamson T, Morkem R, Khan S, Janssen I. Prevalence of toddler, child and adolescent overweight and obesity derived from primary care electronic medical records: an observational study. CMAJ Open. 2016;4(3):E538–44. doi: 10.9778/cmajo.20150108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rose SA, Turchin A, Grant RW, Meigs JB. Documentation of body mass index and control of associated risk factors in a large primary care network. BMC Health Serv Res. 2009;9:236. doi: 10.1186/1472-6963-9-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Healthy Kids Panel. No time to wait: the Healthy Kids Strategy. Toronto, ON: Queen’s Printer for Ontario; 2013. [Google Scholar]
- 37.Edwards J, Evans J, Brown AD. Using routine growth data to determine overweight and obesity prevalence estimates in preschool children in the Capital Health Region of Alberta. Can J Public Health. 2008;99(2):91–4. doi: 10.1007/BF03405451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Canning P, Courage ML, Frizzell LM, Seifert T. Obesity in a provincial population of Canadian preschool children: differences between 1984 and 1997 birth cohorts. Int J Pediatr Obes. 2007;2(1):51–7. doi: 10.1080/17477160601124613. [DOI] [PubMed] [Google Scholar]
- 39.Borghi E, de Onis M, Garza C, Van den Broeck J, Frongillo EA, Grummer-Strawn L, et al. Construction of the World Health Organization child growth standards: selection of methods for attained growth curves. Stat Med. 2006;25(2):247–65. doi: 10.1002/sim.2227. Erratum in: Stat Med 2008;27(16):3216. [DOI] [PubMed] [Google Scholar]
- 40.Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284–94. doi: 10.1111/j.2047-6310.2012.00064.x. Epub 2012 Jun 19. [DOI] [PubMed] [Google Scholar]
- 41.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;(246):1–190. [PubMed] [Google Scholar]
- 42.Anis AH, Zhang W, Bansback N, Guh DP, Amarsi Z, Birmingham CL. Obesity and overweight in Canada: an updated cost-of-illness study. Obes Rev. 2010;11(1):31–40. doi: 10.1111/j.1467-789X.2009.00579.x. Epub 2009 Apr 21. [DOI] [PubMed] [Google Scholar]
- 43.Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad Pediatr. 2013;13(1):6–13. doi: 10.1016/j.acap.2012.10.007. Epub 2012 Nov 30. [DOI] [PubMed] [Google Scholar]
- 44.Vuorela N, Saha MT, Salo M. Prevalence of overweight and obesity in 5- and 12-year-old Finnish children in 1986 and 2006. Acta Paediatr. 2009;98(3):507–12. doi: 10.1111/j.1651-2227.2008.01110.x. Epub 2008 Nov 4. Erratum in: Acta Paediatr 2009;98(3):606. [DOI] [PubMed] [Google Scholar]
- 45.Rifas-Shiman SL, Rich-Edwards JW, Scanlon KS, Kleinman KP, Gillman MW. Misdiagnosis of overweight and underweight children younger than 2 years of age due to length measurement bias. MedGenMed. 2005;7(4):56. [PMC free article] [PubMed] [Google Scholar]
- 46.Howe LD, Tilling K, Lawlor DA. Accuracy of height and weight data from child health records. Arch Dis Child. 2009;94(12):950–4. doi: 10.1136/adc.2009.162552. Epub 2009 Aug 17. [DOI] [PubMed] [Google Scholar]
- 47.Yin H, Dai Y, Li H, Xie X, Ren H. The test-re-test reliability of routine infant anthropometry at primary care hospitals in Chongqing, PR China. Ann Hum Biol. 2013;40(4):309–17. doi: 10.3109/03014460.2013.775343. [DOI] [PubMed] [Google Scholar]
- 48.Nash A, Secker D, Corey M, Dunn M, O’Connor DL. Field testing of the 2006 World Health Organization growth charts from birth to 2 years: assessment of hospital undernutrition and overnutrition rates and the usefulness of BMI. JPEN J Parenter Enteral Nutr. 2008;32(2):145–53. doi: 10.1177/0148607108314386. [DOI] [PubMed] [Google Scholar]
- 49.Shields M, Tjepkema M. Regional differences in obesity. Health Rep. 2006;17(3):61–7. [PubMed] [Google Scholar]