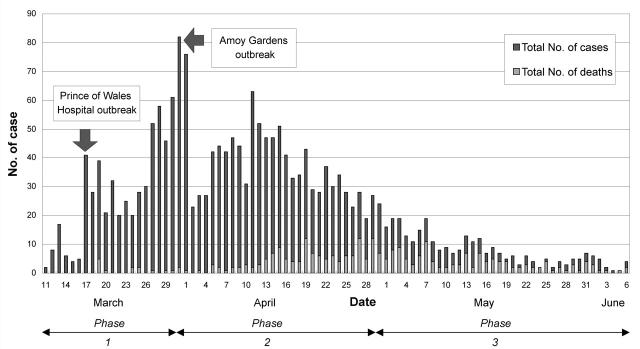
Severe acute respiratory syndrome (SARS) reached Hong Kong in March 2003.1 From 11 March up to 6 June, a total of 1750 cases had been identified (Figure 1), and during the same period 286 people died of the disease. Before the advent of SARS in Hong Kong, the nearby Guangdong Province in Mainland China had experienced an intense outbreak of the atypical pneumonia later termed SARS. This outbreak started in November 2002 and reached its peak in February 2003; up to 5 June 2003, Guangdong had recorded 1511 cases and 57 deaths. Later in April 2003, SARS cases were reported in other provinces and cities of Mainland China including Beijing, Shanxi, Neimonggol, Tianjin and Hebei. Up to 5 June 2003, Mainland China had a total of 5329 cases with 336 reported deaths.2
Figure 1.
Severe acute respiratory syndrome cases, Hong Kong, March-June 2003
From March onwards, SARS was detected in other countries and areas in the Asia-Pacific region. By the beginning of June, Singapore had had 205 cases with 28 deaths, Vietnam 63 cases with 5 deaths and Taiwan 686 cases with 81 deaths.
METHODS
The content of this paper was gathered from personal observations when attending conferences, seminars and video meetings on SARS, from academic staff in the University of Hong Kong, the Chinese University of Hong Kong and the medical school in Guangdong, from clinicians in the Hospital Authority, and from public health professionals in the Department of Health who were either directly involved in the laboratory investigation, diagnosis and management of SARS patients or engaged in efforts to control the disease. Other sources were press reports, personal interviews and websites on SARS provided by the health and hospital authorities, the US Centers for Disease Control and Prevention, the World Health Organization (WHO) and the Centre for Disease Control in Mainland China.
EPIDEMIOLOGY
The SARS epidemic in Hong Kong has gone through three phases. The first was an explosive outbreak in a teaching hospital, affecting a large number of hospital staff and medical students. This phase took place in March 2003. The second phase was an outbreak in the community as a result of the spread of infection from the hospital to the community.3 This reached its peak in early April 2003 when the disease affected a housing estate known as Amoy Gardens; a total of 329 residents in that estate came down with the disease and 33 died. The third phase began in early May, with continuing occurrence of the disease in eight hospitals and more than 170 housing estates throughout the city but with the daily number of new cases declining from double to single digits in mid-June (the time of writing).
The first phase started when a professor from Guangzhou, who had been treating patients with atypical pneumonia in a Guangzhou hospital in Mainland China, visited Hong Kong in February 2003. He stayed at the Metropole Hotel in Kowloon on 21 February. The professor was already unwell when he travelled to Hong Kong and on 22 February he was admitted to the Kwong Wah Hospital in Kowloon. Later he died. From this first index case, 7 other people whose rooms had been on the same floor of the hotel contracted SARS, including 3 visitors from Singapore, 1 visitor from Vietnam, 2 visitors from Canada and 1 local person. Seemingly it was these 7 individuals who, having acquired the infection from the index case, transmitted SARS to Canada, Vietnam, Singapore, and elsewhere in Hong Kong. The local person was admitted to a teaching hospital, the Prince of Wales Hospital, at Shatin on 4 March 2003. From this patient the disease spread through that hospital, ultimately affecting over 100 medical and nursing personnel.
Amoy Gardens
Phase 2 began in early April with the spread of SARS into the community. This was the time when daily new cases reached their peak. The severe outbreak in Amoy Gardens, a housing estate in Kowloon, began at this time. The index patient in this outbreak was a 33-year-old man who lived in Shenzhen and visited his brother in Amoy Gardens regularly. His chronic renal disease was being treated at the Prince of Wales Hospital. SARS symptoms developed on 14 March 2003. On that day and 19 March he visited his brother who owned a flat in Block E of the estate. He had diarrhoea and used the toilet there. His brother, his sister-in-law and 2 nurses who attended to him at Prince of Wales Hospital subsequently developed SARS. By 15 April 2003, there had been 321 SARS cases in Amoy Gardens, with an obvious concentration in Block E (41%).
A thorough local investigation, conducted by the Department of Health in collaboration with eight other government agencies, then indicated that environmental factors had played an important part in this outbreak. Each block at Amoy Gardens has 8 vertical soil stacks collecting effluent from the equivalent section on all floors. The soil stack is connected to the water closets, the basins, the bathtubs and the bathroom floor drains. Each of these sanitary fixtures is fitted with a U-shaped water trap to prevent foul smells and insects getting into the toilets from the soil stack. Clearly, for this to work, the U-traps must contain water. However, because most households were in the habit of cleaning the bathroom floor by mopping rather than flushing with water, the U-traps connected to most floor drains were probably dry and not functioning properly (Figure 2).
Figure 2.
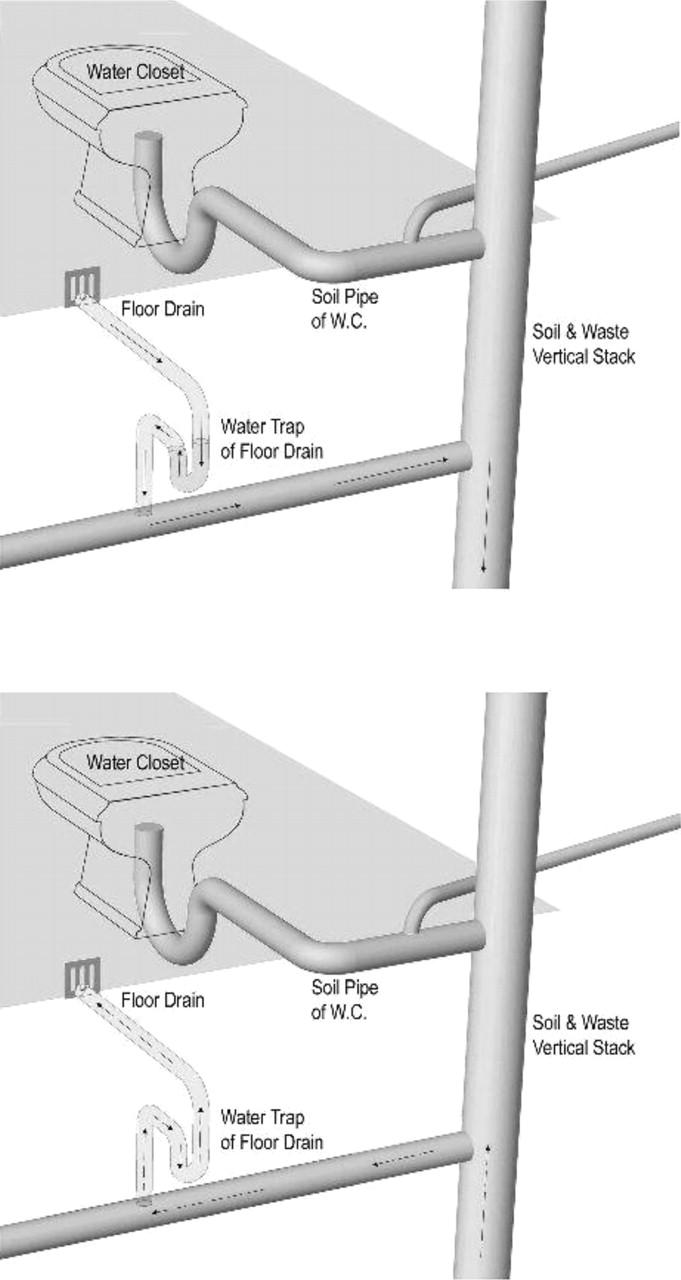
Floor drains at Amoy Gardens
Laboratory studies indicate that many patients with SARS excrete coronavirus in their stools.5 As many as two-thirds of the patients in the Amoy Gardens outbreak had diarrhoea, so a very substantial virus load would have been discharged into the sewerage in Block E. Probably the index patient infected only a small group of Block E residents, with the remainder acquiring the disease via sewage, person-to-person contact and shared communal facilities such as lifts and staircases. These residents subsequently transmitted the disease to others both within and outside Block E through person-to-person contact and environmental contamination.
The bathroom floor drains with dried-up U-traps provided a pathway through which residents came into contact with small droplets containing viruses from the contaminated sewage. These droplets entered the bathroom floor drain through negative pressure generated by exhaust fans when the bathroom was being used with the door closed. Water vapour generated during a shower, and the moist conditions of the bathroom, could also have facilitated the formation of water droplets. The likelihood of exposure was enhanced by the small dimensions of the bathroom units (about 3.5 square metres). Virus-contaminated droplets could readily have been deposited on floor mats, towels, toiletries and other bathroom equipment.
The possibility of disease transmission by other routes—airborne, water-borne, infected dust aerosols—has been examined but there is neither epidemiological nor laboratory support for such mechanisms. A team of environmental experts from the WHO, visiting Amoy Gardens by invitation, agreed with the results of the investigation and also declared the buildings, now cleansed and disinfected, safe for habitation.6
PREVENTION AND CONTROL
The prevention and control measures undertaken in Hong Kong include: (1) preventive education and publicity; (2) tracing the source of infection; (3) introducing five major control measures (compulsory isolation and surveillance of contacts, stopping school and university education sessions, exchange of epidemiological information between Hong Kong and Mainland China, temperature checking of travellers at points of entry and exit, district-wide cleansing campaigns); (4) strengthening collaboration and communication with Mainland China and the WHO; and (5) developing a quick diagnostic test for SARS.
When the first few cases of SARS were identified, the Department of Health of the Hong Kong Special Administrative Region Government passed legislation to make SARS a notifiable infectious disease. Patients with SARS were isolated in the hospitals, and family or close contacts were kept under surveillance, initially at home but later in isolation centres where they were observed for 10 days.
The public health workers undertook the investigations of the source of infection and the tracing of contacts, and promoted application of control measures including the wearing of masks, strict adherence to personal hygiene, and disinfection and cleansing of affected households and housing estates. Incoming and outgoing travellers were screened for fever exceeding 38°C and were required to complete a health declaration form. Apart from their intrinsic value, these measures served to alert the public to the high infectivity of SARS and the need for preventive measures.
In the middle of May 2003, when the epidemic began to slow down, the Government announced further measures. Three committees headed by senior government officials were established—one responsible for the overall cleansing campaigns and environmental improvements in the housing estates; a second for drawing up programmes to revitalize the economy of the city, including tourism, trade and employment; and the third to devise ways to promote community involvement and partnership in improving the physical, social and economic environments of the city. Additional funds were approved to support research on diagnosis, treatment, and vaccine development for SARS. A Centre for Disease Control and Prevention would be developed to strengthen surveillance, research, training and collaboration with other health authorities regionally and internationally.
At the end of May, the Hong Kong Government of the Special Administrative Region appointed a committee of nine experts from the USA, the UK, Australia, Mainland China and Hong Kong to make recommendations on future prevention and control of the disease. I am a member of this team.
Canada
It is pertinent to refer briefly to the SARS outbreak in Canada, the country most severely affected outside Asia.7 As mentioned earlier, 2 visitors from Canada were infected at the Metropole Hotel, in Kowloon. Returning to Toronto they developed symptoms and later gave rise to a cluster of 16 other cases including 4 family members, 2 close contacts and 10 healthcare workers. When the outbreak in Toronto began in March 2003, the WHO issued a warning notice to travellers intending to visit the city—a notice later withdrawn after representations from the Canadian Health Ministry. When no further cases were reported, the outbreak seemed to have been brought under control. However, in mid-May there were further cases. In view of the evidence that more than one generation of cases had occurred, the WHO restored Toronto to the list of infected areas. By 14 June over 90 probable cases had been reported in this resurgence. This Canadian experience highlights the importance of continuing vigilance even when cases begin to decline.
SHORTCOMINGS
The SARS outbreak reached epidemic proportions so quickly and explosively that the health and hospital authorities were unprepared. Initially there was an acute shortage of masks and protective clothing for the medical and health personnel, who were hard hit by the disease. Lack of epidemiological information about the disease hampered the prompt application of effective control measures. Because of inadequate communication, panic developed in the community and weakened cooperation and support from the public. Some contacts did not respond when the Department of Health asked them to attend for surveillance and quarantine. There were difficulties in designating hospitals for the isolation and treatment of SARS patients, because Hong Kong has no infectious-disease hospital as such. Since the wards of the general hospitals were not designed for patients with infectious disease, infection of healthcare staff became a serious issue. By June 2003, 386 medical, nursing and other healthcare workers in the hospitals and clinics had developed SARS and 8 of them (4 doctors, 1 nurse and 3 healthcare assistants) had died. Some hospital wards had to be closed temporarily, and general patients were transferred to other medical institutions to make way for the SARS patients. In the absence of a specific isolation centre for infectious disease, contacts were accommodated in holiday and recreation centres outside the city. Not being designed for the purpose, these were far from ideal. There was much evidence of distress among front-line healthcare workers and members of the public, many of whom were anxious, fearful and depressed. The SARS epidemic damaged not only health but also tourism, international travel and trade, social and business activity, and educational programmes.
Several features of the epidemic rendered control measures difficult in Hong Kong. Initially the cause was unknown, and lack of information on the mode of transmission hampered efforts at control. Because of the large number of cases, patients were admitted into various general hospitals unequipped to handle highly infectious diseases and numerous medical and nursing staff became infected. The lack of isolation facilities allowed infection of patients admitted to the same wards for other reasons. Many patients when admitted to hospital did not have the typical signs of SARS (fever, cough, evidence of chest infection), thus worsening the difficulties of cross-infection control. At one point there was discussion whether a single specially equipped hospital with 600-1000 beds should be designated to cater solely for patients with SARS or with fever on admission. Another issue was whether there should be permanent and proper quarantine facilities for isolation of contacts. Surveillance of contacts at home was not considered effective.
A further controversy arose over the International Health Regulations (IHR). These specify three diseases—namely, cholera, plague and yellow fever—about which the WHO must be notified by the health authorities concerned. The city must then declare itself ‘infected’ with that disease until after twice the incubation period from the last case reported. At the beginning of the SARS epidemic there was doubt whether Hong Kong should declare itself infected with SARS. Although the existing IHR did not include SARS, the WHO had issued a warning notice advising travellers not to visit Hong Kong because of the SARS epidemic—an advisory that drastically reduced the number of international visitors. In May 2003, when the epidemic began to show signs of decline, the WHO set out three conditions for withdrawal of the advisory—no case of SARS spreading to other cities outside Hong Kong; number of new cases less than 5 daily for three days; and number of patients in the hospitals less than 60. At the end of May, the WHO deemed these conditions fulfilled and lifted its advisory on international travellers, though Hong Kong remained on the list of infected areas.5
In some circles the WHO is perceived to have over-reacted to the epidemic,8 causing unnecessary panic on the international scene and putting unjustified barriers in the way of persons from ‘infected’ areas wishing to attend such events as business exhibitions or international sports activities. It is noteworthy that, in May 2003, the World Health Assembly passed a resolution to revise the IHR. This was an appropriate decision since the emergence of new and highly infectious diseases has made the existing regulations out of date.
LESSONS LEARNED
The lessons learned by Hong Kong can be summarized as follows:
SARS differed from previous epidemic infectious diseases in its explosive spread, which caught the health and hospital authorities by surprise and ill-prepared.
Inadequate epidemiological information about the disease hampered the prompt application of effective control measures. Insufficient communication with the public led to panic and thus weakened public cooperation and support.
Because there were no specified infectious disease hospitals, there were difficulties in designating hospitals for the isolation and treatment of SARS patients.
The SARS epidemic in Hong Kong not only affected the health of the people but also had social, economic, and humanitarian repercussions. It unveiled deficiencies in the public health arena and in coordination between the Department of Health and the Hospital Authority—reflected in lack of action between 22 February, when the index patient was admitted to Kwong Wah Hospital, and 4 March when the local contact arrived at the Prince of Wales Hospital. In that interval, the alarm could have been raised and front-line staff could have prepared themselves.
There was also deficient communication between the Secretary (Ministry) level responsible for health policy and the management level responsible for operation of the hospitals. Management inertia at various levels hampered decision-making and delayed implementation of effective measures.
The SARS epidemic also shed light on basic failings of the existing healthcare system in Hong Kong—overcrowded wards; poor ventilation in some hospitals; lack of isolation facilities; inadequate intensive care facilities; staff already working under heavy pressure; difficulty in isolating and cohorting patients with suspected or possible SARS, particularly at the point of admission and immediately thereafter.
The effect of the outbreak on intensive care and nursing personnel was disproportionately high. This worsened the pressures on other branches, particularly during the recovery phase when normal services had to be resumed.
Healthcare workers were put at special risk by certain procedures including use of nebulizers, endotracheal suction and intubation, cardiopulmonary resuscitation, nasogastric feeding, and the use of high flow rates of oxygen.9 The high risk presented by these procedures has implications for medical practice and organization of hospital care in the future.
There is a need to strengthen the exchange of epidemiological information on infectious diseases, especially the emergence of new infections, between the health authorities in Mainland China and Hong Kong. The establishment of a Centre for Disease Control and Prevention in Hong Kong should meet this need.
Hong Kong will continue to face the challenges of infectious disease, because of increasing environmental pollution, population movements, the influx of refugees and immigrants, the emergence of new infections and the changing lifestyle and behaviour of the population.10 There is a great need to set up a Centre for Disease Control and Prevention in Hong Kong so as to strengthen surveillance and exchange of epidemiological information with other health authorities, to undertake research and development on new vaccines and to train medical and scientific personnel on prevention, treatment and control of infectious diseases. On the plus side, the epidemic created an unprecedented sense of unity among all sectors—Government, non-governmental organizations, medical and nursing personnel—in the struggle to contain the epidemic. Various foundations were set up by non-governmental organizations and by public-spirited citizens to provide financial support to victims of SARS and their families. The devotion and self-sacrifice of medical and healthcare staff drew praise and appreciation from all sides, and strengthened the city's resolve to cope better with the challenges of infectious diseases in future. In this way, Hong Kong can be said to have turned the threats of the SARS epidemic into opportunities.
References
- 1.Department of Health, Hong Kong. Severe Acute Respiratory Syndrome (SARS) Statistics, March-May 2003. [http://www.info.gov.hk/dh/]
- 2.Severe Acute Respiratory Syndrome (SARS) Statistics, Mainland China, up to 17 May 2003 [http://www.chinacdc.net.cn/default.asp]
- 3.Donnelly CA, Ghani AC, Leung GM, et al. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet 2003; 361: 1761-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Health, Hong Kong. Outbreak of Severe Acute Respiratory Syndrome (SARS) at Amoy Gardens, Kowloon Bay, Hong Kong. Main Findings of the Investigation, 17 April 2003. Hong Kong: DoH, 2003
- 5.Peiris M, Lai ST, Poon LM, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 2003; 361: 1319-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO Regional Office for the Western Pacific. WHO Environmental Health Team Reports on Amoy Gardens [http://www.who.int/en/]
- 7.WHO Update 78—Situation in Toronto, 11 June 2003 [http://www.who.int/csr/don/2003_06_11a/en]
- 8.SARS: a WHO-induced panic? Far Eastern Econ Rev 22 May 2003
- 9.Tomlinson B, Cockram C. SARS: experience at Prince of Wales Hospital, Hong Kong. Lancet 2003; 361: 1486-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee SH. Prevention and Control of Communicable Diseases in Hong Kong. Hong Kong: Government Printer, 1994