Abstract
The UK National Health Service has now specified a maximum interval of two weeks between general practitioner (GP) referral and specialist assessment for patients with suspected cancer. We examined progress through the cancer pathway in 160 patients with potentially curable cancers of the prostate, bladder, kidney and testis before implementation of this rule. Median intervals with interquartile ranges were quantified from the first GP consultation to hospital referral, then to the first hospital consultation, confirmation of diagnosis and definitive surgery.
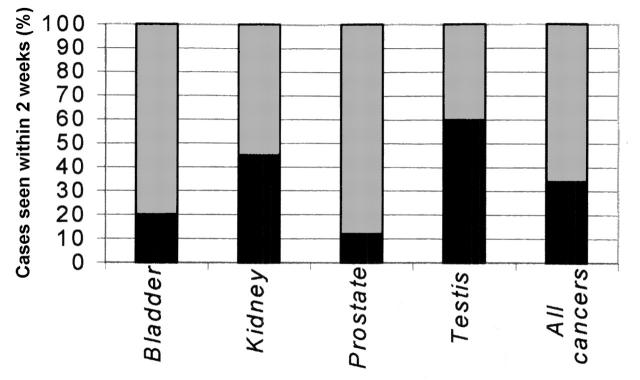
34% of patients were seen at the hospital within two weeks of referral. The overall median interval from GP consultation to radical surgery was 137 days, the longest being for prostate cancer (median 244). For prostate, bladder and renal cancers the principal element of delay was from the time of diagnosis to surgery (76, 73 and 26 days respectively).
These results indicate that, under the two-weeks-wait rule, 2 out of every 3 patients achieve earlier initial assessment. However, the overall delay will not be substantially reduced without concomitant increases in diagnostic facilities, theatre time and human resources.
INTRODUCTION
The journey of a patient with cancer starts with the first consultation with the general practitioner (GP) and finishes with definitive treatment, in many cases removal of the affected organ. The Government White Paper entitled The New NHS—Modern, Dependable declared that ‘Everyone with suspected cancer will be able to see a specialist within 2 weeks of their GP deciding that they need to be seen urgently and requesting an appointment’.1 For urological cancers this was implemented from December 2000. To see how this might affect the cancer care pathway overall we examined the delays at various stages in patients treated before implementation of the rule.
METHODS
The study group consisted of 160 patients—40 each who underwent radical prostatectomy, radical cystectomy, radical nephrectomy or radical orchidectomy before December 2000 for ‘potentially curable’ cancers. The case notes were reviewed to quantify the intervals between the various stages in the patient pathway—namely, from the first GP consultation to hospital referral, then to the first hospital consultation, confirmation of diagnosis and definitive surgery. The statistical package SPSS was used to analyse the data. Median time intervals with interquartile (IQ) ranges were calculated, since the data were not symmetrically distributed.
RESULTS
One-third of the patients were seen at the hospital within two weeks of referral. Figure 1 shows the proportions in each category. The interval from onset of symptoms to radical surgery for the whole series was 137 days (Table 1). The longest delay was for prostate cancer and the shortest for testicular cancer. Patients with prostate cancer had to wait longest at all stages of the pathway—before specialist assessment, before formal diagnosis and before surgical treatment. Some of the prostate cancer patients had several attendances for biopsies before cancer was diagnosed. During the last leg of the journey (diagnosis to radical surgery), the waiting period was the shortest for testicular cancer.
Figure 1.
Percentage of cases seen within two weeks of general practitioner referral
Table 1.
Waiting times from first general practitioner (GP) consultation to radical surgery
|
Median waiting time (interquartile range) in days
|
|||||
|---|---|---|---|---|---|
| Surgical procedure | GP consultation to referral | GP referral to first hospital appointment | First hospital appointment to confirmation of diagnosis | Diagnosis to radical surgery | Overall waiting time |
| Prostatectomy n=40 | 0 (0-1) | 56 (36-84) | 74 (23-292) | 76 (54-103) | 244 (164-382) |
| Cystectomy n=40 | 0 (0-0) | 42 (20-61) | 33 (12-78) | 73 (43-103) | 165 (136-226) |
| Nephrectomy n=40 | 0 (0-31) | 21 (4-44) | 1 (0-36) | 26 (15-42) | 82 (25-179) |
| Orchidectomy n=40 | 0 (0-14) | 9 (5-27) | 0 (0-3) | 4 (2-9) | 30 (16-51) |
| All cases n=160 | 0 (0-11) | 33 (9-60) | 20 (0-73) | 39 (11-76) | 137 (49-226) |
DISCUSSION
Patient delay, clinician delay and most important hospital delays have been recognized as the factors responsible for protracted patient pathways in urological cancers.2-6 Before December 2000 only 34% of patients who eventually had radical cancer surgery were seen in the hospital clinic within two weeks from initial GP referral. Whatever the effect of the two-weeks-wait rule, it will not have improved other steps on the urological cancer care pathway. Patients with prostate and bladder cancer spent much time waiting for staging (imaging) investigations and then for an operating theatre slot.
Do these long waits mean poorer outcomes? This question has been examined particularly for bladder and testicular cancers, but the evidence is conflicting.7,8 For bladder cancer, a recent prospective study suggests that delay is harmful in patients with T1 tumours.9 For testicular cancers some workers report an adverse influence of delay on survival,10,11 others not.12,13 An MRC working party found no effect of delay once stage and marker status were taken into account.14 The matter is hard to resolve because of the mix of patient-related factors (such as co-morbidity) and tumour-related factors. Nevertheless, early diagnosis and treatment will certainly be helpful in alleviating anxiety and reducing absence from work due to symptoms. To this end, cancer services are being reconfigured, and local networks are playing an increasingly important role. Centres and units staffed by experts in all aspects of cancer management are being established, and the resulting improved organization should reduce delay times at various stages. The next Government target is two months from urgent referral to treatment for all cancers by the end of December 2005, and our results indicate that this can be achieved only by broad-based investment in diagnostic and operating facilities.
References
- 1.NHS Executive. Referral Guidelines for Suspected Cancer. London: Department of Health, 2000
- 2.Wallace DM, Harris DL. Delay in treating bladder tumours. Lancet 1965;ii: 332-4 [DOI] [PubMed] [Google Scholar]
- 3.Turner AG, Hendry WF, Williams GB, Wallace DM. A haematuria diagnostic service. BMJ 1977;ii: 29-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacArthur C, Pendleton LL, Smith A. Treatment delay in patients with bladder tumours. J Epidemiol Commun Health 1985;39: 63-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stower MJ. Delays in diagnosing and treating bladder cancer. BMJ 1988;296: 1228-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tocklu C, Ozen H, Sahin A, Rastadoskuoee M, Erdem E. Factors involved in diagnostic delay of testicular cancer. Int Urol Nephrol 1999;31: 383-8 [DOI] [PubMed] [Google Scholar]
- 7.Mommsen S, Aagaard J, Sell A. Presenting symptoms, treatment delay and survival in bladder cancer. Scand J Urol Nephrol 1983;17: 163-7 [DOI] [PubMed] [Google Scholar]
- 8.Gulliford MC, Petruckevitch A, Burney PG. Survival with bladder cancer, evaluation of delay in treatment, type of surgeon, and modality of treatment. BMJ 1991;303: 437-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wallace DM, Bryan RT, Dunn JA, Begum G, Bathers S. Delay and survival in bladder cancer. BJU Int 2002;89: 868-78 [DOI] [PubMed] [Google Scholar]
- 10.Thornhill JA, Fennelly JJ, Kelly DG, Walsh A, Fitzpatrick JM. Patients' delay in the presentation of testis cancer in Ireland. B J Urol 1987;59: 447-51 [DOI] [PubMed] [Google Scholar]
- 11.Oliver RTD. Factors contributing to delay in diagnosis of testicular tumours. BMJ 1985;290: 356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fossa SD, Klepp O, Elgjo RF, et al. The effect of patient's delay and doctor's delay in patients with malignant germ cell tumours. Int J Androl 1981;suppl 4: 134. [DOI] [PubMed]
- 13.Chilvers CED, Saunders M, Bliss JM, Nicholls J, Horwich A. Influence of delay in diagnosis on prognosis in testicular teratoma. Br J Cancer 1989;59: 126-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MRC Working Party on Testicular Tumours. Prognostic factors in advanced non-seminomatous germ cell testicular tumours; results of a multi-centre study. Lancet 1985;i: 8. [PubMed] [Google Scholar]